Abstract
Objectives
This preliminary study examines the efficacy of 12-week home-delivered Problem Adaptation Therapy (PATH) vs. home-delivered Supportive Therapy (ST) in reducing depression and disability in 30 depressed, cognitively impaired, disabled older adults.
Design
A 12-week randomized clinical trial. Research assistants were unaware of the participants' randomization status. Assessments were conducted at baseline, 6 and 12 weeks.
Setting
Weill Cornell - Advanced Center for Interventions and Services Research (ACISR).
Participants
Thirty elders with major depression, cognitive impairment, and disability were recruited through advertisement and the Home-Delivered Meals Program of the Westchester County Department of Senior Programs and Services.
Intervention
PATH is a home-delivered intervention designed to reduce depression and disability in depressed, cognitively impaired, disabled elders. PATH is based on Problem Solving Therapy (PST) and integrates environmental adaptation and caregiver participation. PATH is consistent with Lawton's ecological model of adaptive functioning in aging.
Measurements
Depression and disability were measured with Hamilton Depression Rating Scale – 24 items and Sheehan Disability Scale, respectively. Client Satisfaction Questionnaire was used to assess patient satisfaction with treatment.
Results
Mixed-effects model analyses revealed that PATH was more efficacious than ST in reducing depression and disability at 12 weeks. Participants in both treatment groups were satisfied with treatment.
Conclusions
This preliminary study suggests that PATH is well accepted and efficacious in depressed elders with major depression, cognitive impairment, and disability. Because this population may not adequately respond to antidepressant medication treatment, PATH may provide relief to many patients who would otherwise remain depressed and suffer.
OBJECTIVE
Major depression, cognitive impairment and disability often coexist in the elderly and contribute to increased medical and psychiatric morbidity and mortality (1–3). Currently available treatments have been effective in a minority of depressed, cognitively impaired elders. Antidepressants bring to remission fewer than 40% of depressed elderly patients (4) and have an even lower efficacy in depressed elders with cognitive deficits and especially executive dysfunction (5–8). Furthermore, psychosocial interventions for elders with major depression, cognitive impairment, and disability are understudied.
Most psychosocial interventions in geriatric major depression that have been tested in randomized clinical trials are designed for cognitively intact, ambulatory, depressed elders (9–11). Problem Solving Therapy (PST) (12) and Interpersonal Psychotherapy (IPT) (13) have been adapted for depressed elders with mild cognitive deficits and a behavioral treatment (14) has been designed to treat major depression in demented elders with moderate to severe dementia. Other psychosocial interventions in dementia focus on elders without or with mild depressive symptoms (15). Therefore, elders with major depression and significant, yet not very advanced cognitive impairment have been overlooked. To address the needs of elders with major depression and intermediate cognitive impairment and disability, we developed Problem Adaptation Therapy (PATH), a home-delivered intervention targeting behavioral limitations resulting from depression and disability.
PATH focuses on the patient's ecosystem, which includes the patient, the caregiver, and the home environment, and uses Problem Solving Therapy (PST) as its basic therapeutic framework (16). To minimize the behavioral sequelae of the patients' cognitive deficits, PATH incorporates environmental adaptation tools and invites caregiver participation. Environmental adaptation tools are designed to bypass behavioral and functional limitations in these patients (17). Furthermore, a willing and available caregiver helps the cognitively impaired patient in solving everyday problems, utilizing environmental adaptation tools, and initiating and engaging in pleasurable activities (14). Home-delivered interventions with caregiver participation and environmental manipulations have reduced agitation, and improved mood and quality of life in demented patients (18– 21).
PATH is consistent with Lawton's ecological model of adaptive functioning in aging. According to this model, adaptive behavior is a function of the person's competence and the environmental press to which he or she is exposed (22). Competence is defined as the highest capacity that individuals can achieve given their biological health, cognition, motoric behavior, and sensation-perception (22). For depressed elders with cognitive impairment and disability, the balance between the environmental demands and the patients' competence is disrupted. Because of reduced cognitive and behavioral capacities, due to depression, cognitive impairment, and disability, these patients can not meet the demands of their environment (22–23). Continuous unsuccessful attempts to meet the environmental demands contribute to further depression and disability (24). To restore the disrupted balance and to provide a therapeutic ecosystem, PATH: a) helps the patients reduce their depression through a well-established problem-solving intervention; and b) responds to increased environmental demands by utilizing environmental adaptations and by inviting caregiver participation.
This study examined the efficacy of 12-week home-delivered PATH vs. home-delivered Supportive Therapy (ST) in reducing depression and disability in 30 older adults with major depression, cognitive impairment, and disability. We anticipated that over 12 weeks, participants treated with PATH would have had a greater reduction in depression and disability than those who received home-delivered ST.
METHODS
PARTICIPANTS
Elderly participants (age=65 years or older) were recruited through the Research Network Development Core of Weill-Cornell Advanced Center for Intervention and Services Research (ACISR) located at a University Hospital in Westchester County, NY. Participants were community elders responding to an advertisement for geriatric depression or receiving home delivered meals through the Home-Delivered Meals Program of the Westchester County Department of Senior Programs and Services, a collaborating agency of the ACISR's Research Network Development Core.
Inclusion criteria were (1) diagnosis of unipolar Major Depressive Disorder by SCID interview and SCID-IV criteria; (2) a Hamilton Depression Rating Scale (HAM-D) (25) score of 17 or above; (3) cognitive impairment defined by a score lower than 2 standard deviations of the mean of cognitively intact elderly control subjects without history or presence of psychiatric disorders (26) on the Dementia Rating Scale Initiation/Perseveration subscale (DRS IP) (<=30) (27) or Stroop Color-Word (Stroop CW) (<=18) (28); (4) disability as defined by at least 1 impairment in the performance of Instrumental Activities of Daily Living of the Philadelphia Multilevel Assessment Instrument (MAI) (29); (5) limited mobility to follow-up weekly outpatient treatment program as reported by the participant and assessed by the therapist; (6) a caregiver who had knowledge of the participant's history and condition and might be available to participate; (7) either not taking psychotropic drugs (including antidepressants, cholinesterase inhibitors, or memantine) or taking a stable dosage for at least 8 weeks prior to entry and no medical recommendation for medication change in the near future; (7) residence at a distance within 45-minute from the psychiatric university hospital.
Exclusion criteria included (1) Axis I psychiatric disorder or substance abuse other than unipolar major depression, non-psychotic depression; (2) acute or severe medical illness, i.e., delirium, metastatic cancer, decompensated cardiac, liver or kidney failure, major surgery, stroke or myocardial infarction during the three months prior to entry; or drugs known to cause depression, e.g., reserpine, alpha-methyl-dopa, steroids; (3) current involvement in psychotherapy; (4) moderate to severe dementia as evidenced by a Mini-Mental State Examination MMSE (30) score lower than 19; and (5) aphasia, severe dysarthria, and inability to speak English. Patients with severe medical illness and severe dementia were excluded because their behavioral deficits exceed PATH's ability to address them. After description of the study, written informed consent was obtained from the participants. If there were concerns regarding capacity to consent, the subject was excluded from the study. The participants were, then, randomly assigned to either home-delivered PATH or home-delivered ST. To avoid disproportionate assignment into PATH or ST, randomization was made in blocks of five patient participants.
ASSESSMENTS AND INSTRUMENTS
ACISR trained and certified research assistants unaware of randomization status assessed participants at baseline, 6 and 12 weeks. Depression and disability were rated with the Hamilton Depression Rating Scale – 24 items (HAM-D) (25) and the Sheehan Disability Scale (SDS) (31), respectively. The Sheehan Disability scale is a self-administered scale that measures the degree of disruption (on a scale 0–10; 10=the most) of the participants' social life, family life/home responsibilities, and work (31). Since none of the participants worked, this study used as the SDS total score the sum of two individual scores (i.e. Social Life + Family Life/Home Responsibilities). Cognitive impairment and medical burden were measured at baseline with the Mini Mental State Examination (MMSE) (30) and the Charlson Comorbidity scale (32), respectively. Four participants (3 PATH, 1 Supportive) did not complete all the MMSE items because of eyesight and drawing difficulties and their scores were prorated ([# of correct responses / # of total responses]*30). Executive dysfunction was assessed with the DRS IP and the Stroop Color-Word test and memory was measured with the Hopkins Verbal Learning Test-Revised (33). Intensity of antidepressant medication (AD) treatment was measured with the Composite Antidepressant Score – Revised (CAD) (34; revised 1998). CAD measures intensity of AD treatment on a scale of 0–4 with 0=no medication and 4=the most intense AD (for example: 1 corresponds to Citalopram or Paroxetine<10; 2 corresponds to Citalopram or Paroxetine 10–19; 3 corresponds to Citalopram or Paroxetine 20–30; and 4 corresponds to Citalopram or Paroxetine>30). Finally, to examine patients' satisfaction with treatment, we administered 3 items from the Client Satisfaction Questionnaire (35) at 12 weeks. The three items were: CSQ1: To What Extent Did Service Meet Patient's Needs? (Score range 1–4: 4=Almost all needs have been met, 3=Most needs met, 2=Only a few needs met, 1=No needs met); CSQ2: Overall Satisfaction With Service (Scores range 1–4; 4=Very satisfied 3=Mostly satisfied 2=Indifferent or mildly dissatisfied, 1=Quite dissatisfied); CSQ3: Would Patient Come Back To The Program? (Scores range 1–4; 1=No definitely not, 2=No I don't think so, 3=Yes I think so, 4=Yes definitely).
INTERVENTIONS
Problem Adaptation Therapy (PATH)
PATH is a 12-week home-delivered intervention that focuses on the patients' ecosystem (i.e. the patient, the caregiver, and the home-environment). The goals of PATH are to reduce patients' depression and disability by facilitating problem solving and adaptive functioning. To achieve its goals, PATH imparts problem-solving skills to patients by utilizing Problem Solving Therapy (PST) as its basic framework (12, 16). Because many cognitively impaired patients have difficulty in learning and utilizing the problem-solving steps of PST, PATH integrates environmental adaptation tools (PATH tools) and encourages caregiver participation. PATH tools circumvent the behavioral and functional limitations exacerbated by cognitive impairment (17) and include calendars, checklists, pictures, notebooks, magnetized notepads, alarms, signs, colored tags, diaries, timers, timed pre-recorded messages, voice alarms, customized audiotapes, step by step division of a task, etc. PATH tools, which are provided by the therapist, are selected based on the severity of patients' cognitive impairment; their areas of relative cognitive strength; their physical and behavioral limitations; and the specifics of the targeted problem. Caregivers, when available and willing, participate in the problem-solving process, the use of environmental adaptation tools, and the patients' engagement in pleasurable activities (14). Finally, PATH is administered at the patients' home where patients' experience most of their difficulties. Appropriate problem solving strategies are planned and assessed in the patients' own living environment.
Home Delivered Supportive Therapy (ST)
ST is a 12-week intervention and consists of the nonspecific therapeutic factors present in all therapies such as empathic listening, reflection, emotional processing, and encouragement, but without the main aspects of PST (problem-solving coping skills), IPT (interpersonal conflict resolution), and dynamic therapy (exploration of unconscious material) (39). Therefore, ST is an active treatment rather than a control or placebo condition. Twelve weekly ST sessions focus on: 1. facilitating expression of affect; 2. conveying to the patient that he or she is understood; 3. offering empathy; 4. highlighting success experiences; and 6. imparting therapeutic optimism. To parallel the delivery of PATH, ST was administered at the patient's residence and if the patient agreed, willing caregivers were invited to participate. However, the ST therapists did not offer any tangible items nor did they assign any homework.
THERAPISTS
Two Ph.D. (including DNK) and 1 M.S.W. administered both PATH and ST at the patient's residence according to the PATH (36) and ST manuals (37). All therapists were trained in PATH by DNK but had been previously trained and certified in Problem Solving Therapy and in ST by certified PST and ST trainers. To ensure that the interventions were administered as intended, DNK supervised the therapists in a scheduled weekly group and conducted individual supervision sessions when needed. During supervision, DNK listened to 8 audiotaped sessions (half PATH and half ST) by the other two therapists; all of them met the standards of administration of each treatment. All therapists had longer than 5 years experience administering psychotherapy to depressed elders.
STATISTICAL ANALYSIS
All analyses were performed according to the intent-to-treat principle. Initially, we performed univariate analyses between the PATH (N=15) and the ST (N=15) groups on clinical and demographic variables using the Wilcoxon-Mann-Whitney test for continuous variables and the Fisher's exact for categorical variables. We used a mixed effects model to compare the efficacy of PATH and ST on depression (HAM-D total score) and disability (SDS total score); the time effect was entered as a linear effect. We also present the mean and standard deviation of each item of the Client Satisfaction Questionnaire. A two-tailed alpha level was used for each statistical test. All analyses were performed with SAS 9.1.
RESULTS
A total of 37 potential participants were referred to the study and 30 agreed to participate and were randomized to PATH (N=15) or ST (N=15) (Figure 1). The participants were of advanced age and most had high-school or more education (Table 1). Participants suffered from major depression of mild to moderate severity. Their cognitive impairment ranged from mild cognitive deficits to mild dementia. The participants' executive functioning was significantly impaired as indicated by their DRS IP scores and Stroop CW scores (Table 1); their mean scores were more than 2 SD below the mean of a healthy control group of older adults who did not meet any criteria for psychiatric diagnosis or cognitive impairment. The participants' memory deficits were also significant as indicated by the mean scores of Recall and Delayed Recall of HVLT-Revised (Table 1). In addition to their cognitive impairment, the participants had pronounced disability. The mean score of MAI Instrumental Activities of Daily Living score (Table 1) translates into an average impairment in at least 4 Instrumental Activities of Daily Living (i.e. doing housework and handyman work, doing laundry, using the telephone, shopping for groceries, preparing own meals, managing their money, and taking their medication). Therefore, our sample consisted of mildly to moderately depressed elders with cognitive impairment up to the level of mild dementia and pronounced disability. There were no significant differences in demographic or clinical variables between the two treatment arms (Table 1).
Figure 1.
Flowchart of the Study; (*) six week data were collected from these subjects.
Table 1.
Demographic and Clinical Characteristics of 30 Depressed Elders with Cognitive Impairment and Disability at Baseline.
| PATH (N=15) | ST (N=15) | ||||
|---|---|---|---|---|---|
| N | Perc (%) | N | Perc (%) | Fisher's Exact (p) | |
| Gender | 1.00 | ||||
| Female | 10 | 66.67 | 11 | 73.33 | |
| Race and Ethnicity | 1.00 | ||||
| Caucasian-Non-Hispanic | 11 | 73.33 | 11 | 73.33 | |
| African-American | 4 | 26.67 | 4 | 26.67 | |
| Probable or Definite | 1.00 | ||||
| Dementia | 4 | 26.67 | 3 | 20.00 | |
| On Antidepressants | 12 | 78.7 | 12 | 78.7 | 1.00 |
| Mann-Whitney Wilcoxon |
||||||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Range | Mean | SD | Range | z | p | |
| Age | 80.46 | 8.45 | 66–92 | 78.36 | 8.12 | 69–94 | −0.64 | 0.53 |
| Education (years) | 12.50 | 3.67 | 6–18 | 12.23 | 2.68 | 6–16 | −0.25 | 0.80 |
| BASELINE | ||||||||
| HAM-D-24 Total1 | 22.40 | 3.92 | 17–28 | 21.40 | 2.80 | 17–26 | −0.52 | 0.60 |
| MMSE Total2 | 26.86 | 2.33 | 20–30 | 26.40 | 2.95 | 19–29 | −0.15 | 0.88 |
| Executive Dysfunction | ||||||||
| DRS IP3 | 28.14 | 6.39 | 9–35 | 26.00 | 6.51 | 11–35 | −1.12 | 0.26 |
| Stroop CW4 | 15.91 | 8.93 | 4–30 | 15.14 | 8.76 | 5–35 | 0.22 | 0.83 |
| Memory-HVLT 5 | ||||||||
| Immediate Recall | 3.27 | 1.91 | 0–6 | 3.87 | 1.46 | 1–6 | 0.86 | 0.39 |
| Delayed Recall | 4.40 | 2.72 | 0–10 | 5.40 | 2.38 | 0–9 | 1.33 | 0.18 |
| Charlson Total6 | 2.20 | 2.18 | 0–7 | 3.26 | 3.08 | 0–11 | 1.55 | 0.12 |
| SDS Total7 | 13.73 | 5.64 | 0–20 | 10.43 | 5.02 | 0–20 | −1.76 | 0.08 |
| MAI IADL8 | 17.17 | 4.37 | 10–25 | 17.36 | 4.47 | 11–26 | −0.10 | 0.92 |
| Intensity of Antidepressant | ||||||||
| Medication Treatment9 | 2.46 | 1.55 | 0–4 | 2.71 | 1.54 | 0–4 | 0.43 | 0.66 |
24-item Hamilton Depression Rating Scale
Mini Mental State Exam
Mattis Dementia Rating Scale – Initiation / Perseveration Subscale
Stroop Color-Word Score
Hopkins Verbal Learning Test – Revised
Charlson Commorbity Index
Sheehan Disability Scale Total = Social Life Score + Family Life/Home Responsibilities Score
Philadelphia Multilevel Assessment Instrument – Instrumental Activities of Daily Living (IADL) Subscale
Composite Antidepressant Score (CAD)
Caregivers: Nineteen caregivers participated in PATH and ST treatments. Twelve caregivers participated in PATH (3 spouses, 4 adult children, 1 sibling, 2 aids, 2 neighbors/friends); 6 out of 12 (50%) lived with the patient. Seven caregivers were involved in ST sessions (2 spouses, 3 adult children, and 2 aids; 5 (72%) lived with the patient. The average number of sessions that PATH and ST caregivers participated were 6.75 and 3.86, respectively (z=−1.73, p=0.084).
Efficacy on Depression
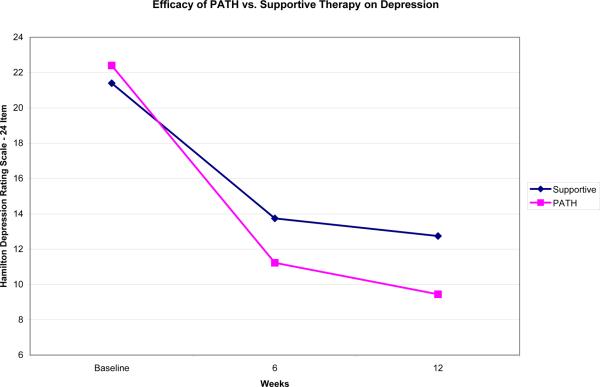
Use of mixed-effects models for repeated measures on HAM-D total scores revealed a significant main effect of time (F=120.88, df=1, 31.8, p<0.0001) and a significant treatment × time interaction (F=5.11, df=1, 31.8, p=0.0307). The treatment × time interaction indicates that participants in PATH had greater decrease in depression over 12 weeks than participants in ST (Figure 2). The mean and standard deviation of the actual HAM-D total scores at the 3 time points were: Baseline: PATH=22.40 (3.92) vs. ST=21.40 (2.80); 6 weeks: PATH=11.07 (4.45) vs. ST=13.75 (4.37); and 12 weeks: PATH=8.92 (4.07) vs. ST=12.75 (5.72). Participants receiving PATH had 51% greater decline in depressive symptomatology than participants treated with ST (HAM-D decline PATH: 13.48 vs. ST: 8.65).
Figure 2.
Depression Scores over 12 weeks of PATH vs. ST in 30 Elders with Major Depression, Cognitive Impairment and Disability Based on the Least Squares Means of the Mixed Effects Model: Time + Treatment + Treatment*Time.
Efficacy on Disability
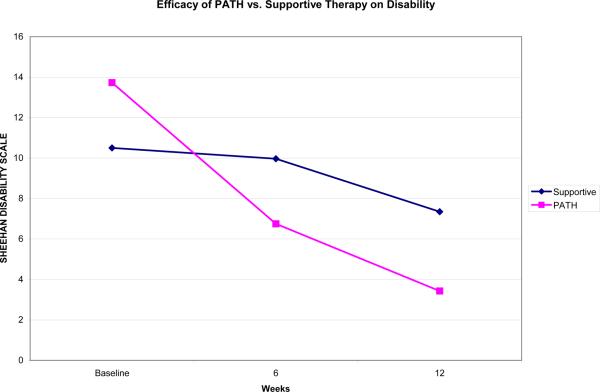
The mixed-effects models on Sheehan Disability Scale (SDS) revealed a significant main effect on time (F=27.57, df=1, 47.1, p<0.0001) and a significant treatment × time interaction (F=7.32, df=1, 47.1, p=0.0095). Similar to the effects on depression, participants in PATH had greater reduction in disability over 12 weeks than participants in ST (Figure 3). The mean and standard deviation of the actual SDS total scores at the 3 time points were: Baseline: PATH=13.73 (5.67) vs. ST=10.43 (5.02); 6 weeks: PATH= 6.57 (5.17) vs. ST=10.42 (4.38); and 12 weeks: PATH= 3.15 (4.65) vs. ST= 7.55 (4.76). Participants receiving PATH had 3.7 times greater decline in disability than participants treated with ST (SDS decline PATH: 10.58 vs. ST: 2.88).
Figure 3.
Disability Scores over 12 weeks of PATH vs. ST in 30 Elders with Major Depression, Cognitive Impairment and Disability Based on the Least Squares Means of the Mixed Effects Model: Time + Treatment + Treatment*Time.
Overall cognitive impairment (MMSE) and executive dysfunction (DRS-IP or Stroop Color-Word) at baseline were not significantly associated with the efficacy of PATH or ST in reducing either depressive symptoms (HAM-D) or disability (SDS). Further, overall cognitive impairment, executive dysfunction and caregiver participation did not moderate treatment effect on depression or disability.
Treatment Satisfaction
Scores from the Client Satisfaction Questionnaire suggest that the patients were satisfied with both treatments (Table 2). Participants reported that their treatment (PATH or ST) met most of their needs and that they would seek a similar service in the future if needed.
Table 2.
Treatment Satisfaction in PATH and ST at the End of 12 Weeks.
| PATH (N=15) | ST (N=15) | Mann-Whitney Wilcoxon |
||
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Z | p | |
| Did Service Meet Patient's Needs* | 3.31 (0.95) | 3.00 (0.85) | −0.92 | 0.36 |
| Would the Patient Come Back To The Program* | 3.31 (0.75) | 3.41 (0.79) | 0.42 | 0.67 |
| Overall Satisfaction With Service* | 3.69 (0.63) | 3.41 (0.79) | −0.96 | 0.34 |
Client Satisfaction Questionnaire
CONCLUSIONS
The principal finding of this study is that home-delivered PATH is more efficacious than home-delivered Supportive Therapy in reducing depression and disability in elders with major depression, cognitive impairment, and disability. Moreover, the comparable rates of treatment satisfaction between PATH and ST participants suggest that these effects were not a by-product of patient enjoyment. Even though the study is preliminary and results need to be confirmed with a large sample, this finding is encouraging since antidepressant drug treatment is often ineffective in this population (5–8).
Our findings are consistent with those of others documenting that Problem Solving Therapy is efficacious in decreasing depression and in reducing disability in depressed older patients with mild executive dysfunction (12) and in depressed patients receiving home healthcare (38). The participants in these two studies, however, had milder cognitive deficits that the participants in this study, and as a result, were able to learn and apply problem solving strategies unassisted (12).
The main innovation of PATH is the systematic integration of environmental adaptations into the problem solving framework and the engagement of caregivers in helping depressed older adults with problems they were unable to face by themselves. These enhancements are necessary as they enable depressed older patients with cognitive impairment up to the level of mild to moderate dementia to utilize and benefit from the problem solving skills imparted by PATH. By inviting caregiver participation and incorporating environmental adaptations, PATH is designed to reduce environmental stress, enhance the patients' coping skills, help to bypass the patients' behavioral and functional limitations, increase the patients' feelings of self-efficacy and improve their adaptive functioning. Caregiver participation and application of behavioral techniques have been used effectively in decreasing depression in elders with advanced dementia (14). Environmental adaptations have also been used successfully in cognitively impaired populations. Compensatory strategies and environmental adaptations have improved functioning and decreased relapse rates in schizophrenics (17) and have promoted adaptive functioning in older adults with dementia (20–21).
PATH was particularly effective on disability, reducing it by 4.3 fold from baseline. We have argued that disability is a distinct dimension of health status with multifactorial etiology and unique prognostic significance (39). Information obtained during a clinical examination, including age, severity of depression, and medical burden, explain only a small part of the variance in disability of elderly patients with major depression. Therefore, improvement of disability by PATH may be a beneficial outcome that is related to improvement of depression, but may extend above and beyond improvement of depression (12).
PATH was efficacious in depressed patients with varying degrees of disability and cognitive impairment, including executive dysfunction. Moreover, PATH was well accepted by patients as evidenced by their responses to the self-administered treatment satisfaction questionnaire. These observations suggest that PATH may benefit a rather large number of depressed elders.
Despite the encouraging results of PATH, future research needs to address dissemination challenges. First, it would require the availability of mental health providers in home care settings. Fewer than 1000 psychologists currently work in these settings (the Bureau of Labor Statistics; National Employment Matrix for Psychologists). Social workers are well represented in home care and can get reimbursed through Medicare but most perform case management functions. Despite dissemination challenges of mental health interventions in home care, recent data support the feasibility of home based PST in the context of routine home care services (38). Cost effectiveness of PATH will also need to be evaluated considering the cost of additional resources (home-delivery, caregiver participation, and environmental adaptations).
The principal limitation of this study is its small sample size. Obtaining statistically significant results on such a small sample is encouraging. However, these results signal the need for a larger efficacy study to examine the acceptance as well as the short-term and long-term impact of PATH on depression and disability. Other limitations include the therapists' allegiance, the differential participation of the caregivers between the two interventions, the absence of assigned homework in the ST arm, and the lack of treatment fidelity measures other than the weekly supervision of therapists. Finally, weekly assessments of depression and disability would provide better information on the course of depression in both PATH and ST.
In summary, this study offers preliminary data that PATH is well-accepted and efficacious in elderly patients with major depression, cognitive impairment reaching the level of mild to moderate dementia, and significant disability. This is the first investigation of PATH and even though our findings are encouraging, they need to be confirmed in a large size efficacy study. Since many depressed, cognitively impaired, disabled elderly patients fail to respond to antidepressant drugs, PATH may be an important part of the therapeutic armamentarium for patients who may otherwise remain depressed and continue to suffer. Furthermore, this study provides preliminary evidence that environmental adaptations and engagement of caregivers can be integrated in problem solving approaches and can reduce the chronic stress experienced by depressed elders unable to manage everyday tasks.
Case Vignette: A Problem Targeted with PATH
Mrs. Y, an 82-year-old woman with history of hypertension and atrial fibrillation, developed major depression following surgery for hip fracture. Her depression was characterized by depressed mood, lack of interest in activities, psychomotor retardation, lack of energy, anhedonia, feelings of worthlessness, and concerns that she would never be herself again. Her executive functioning was significantly impaired whereas she had mild memory and attention deficits. One of the problems targeted in PATH was Mrs. Y's inability to perform exercise. Specifically, Mrs. Y indicated that she was disorganized, did not set a time for her exercises and failed to memorize their sequence. The therapist and Mrs. Y agreed that she should always perform her exercises at the same time (10.30 am) and created a timed schedule of activities (get up, use the bathroom, shower with her aid's assistance if necessary, take analgesics) that would enable her to be ready for her exercises at 10.30 am (i.e. administration of Problem Solving stages). Mrs. Y agreed that a checklist and an alarm might help her to adhere to the schedule (i.e. environmental adaptation tools). Her husband volunteered to keep track of Mrs. Y's scheduled exercises (i.e. caregiver participation). PATH therapist asked Mrs. Y's physical therapist to give Mrs. Y only two exercises initially and to increase the number of exercises progressively. The physical therapist also provided Mrs. Y with written timed instructions and diagrams that were posted in the room where Mrs. Y performed her exercises (i.e. environmental adaptation tools). Within the following 4 weeks, Mrs. Y performed four exercises daily. These successes facilitated her rehabilitation, enhanced her self-esteem, and reduced her hopelessness.
Acknowledgments
This work was supported by NIMH grant K23 MH074659, National Alliance for Research on Schizophrenia and Depression (NARSAD), and MINT Health Foundation.
Footnotes
No disclosures to report.
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Unützer J, Bruce ML, NIMH Affective Disorders Workgroup The elderly. Ment Health Serv Res. 2002;4:245–247. doi: 10.1023/a:1020924901595. [DOI] [PubMed] [Google Scholar]
- 2.Lenze EJ, Sheffrin M, Driscoll HC, Mulsant BH, Pollock BG, Dew MA, Lotrich F, Devlin B, Bies R, Reynolds CF., 3rd Incomplete response in late-life depression: getting to remission. Dialogues Clin Neurosci. 2008;10:419–430. doi: 10.31887/DCNS.2008.10.4/jlenze. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alexopoulos GS. Depression in the elderly. Lancet. 2005;365:1961–1970. doi: 10.1016/S0140-6736(05)66665-2. [DOI] [PubMed] [Google Scholar]
- 4.Thase ME, Entsuah AR, Rudolph RL. Remission rates during treatment with venlafaxine or selective serotonin reuptake inhibitors. Br J Psychiatry. 2001;178:234–241. doi: 10.1192/bjp.178.3.234. [DOI] [PubMed] [Google Scholar]
- 5.Kalayam B, Alexopoulos GS. Prefrontal dysfunction and treatment response in geriatric depression. Arch Gen Psychiatry. 1999;56:713–8. doi: 10.1001/archpsyc.56.8.713. [DOI] [PubMed] [Google Scholar]
- 6.Sneed JR, Roose SP, Keilp JG, Krishnan KR, Alexopoulos GS, Sackeim HA. Response inhibition predicts poor antidepressant treatment response in very old depressed patients. Am J Geriatr Psychiatry. 2007;15:553–563. doi: 10.1097/JGP.0b013e3180302513. [DOI] [PubMed] [Google Scholar]
- 7.Potter GG, Kittinger JD, Wagner HR, Steffens DC, Krishnan KR. Prefrontal neuropsychological predictors of treatment remission in late-life depression. Neuropsychopharmacology. 2004;29:2266–2271. doi: 10.1038/sj.npp.1300551. [DOI] [PubMed] [Google Scholar]
- 8.Alexopoulos GS, Kiosses DN, Murphy C, Heo M. Executive dysfunction, heart disease burden, and remission of geriatric depression. Neuropsychopharmacology. 2004;29:2278–2284. doi: 10.1038/sj.npp.1300557. [DOI] [PubMed] [Google Scholar]
- 9.Areán PA, Alexopoulos G. Psychosocial interventions for mental illness in late-life. Int J Geriatr Psychiatry. 2007;22:99–100. doi: 10.1002/gps.1743. [DOI] [PubMed] [Google Scholar]
- 10.Mackin RS, Areán PA. Evidence-based psychotherapeutic interventions for geriatric depression. Psychiatr Clin North Am. 2005;28:805–20. vii–viii. doi: 10.1016/j.psc.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 11.Cuijpers P, van Straten A, Smit F. Psychological treatment of late-life depression: a meta-analysis of randomized controlled trials. Int J Geriatr Psychiatry. 2006;21:1139–49. doi: 10.1002/gps.1620. [DOI] [PubMed] [Google Scholar]
- 12.Alexopoulos GS, Raue P, Areán P. Problem-solving therapy versus supportive therapy in geriatric major depression with executive dysfunction. Am J Geriatr Psychiatry. 2003;11:46–52. [PubMed] [Google Scholar]
- 13.Miller MD, Reynolds CF., 3rd Expanding the usefulness of Interpersonal Psychotherapy (IPT) for depressed elders with co-morbid cognitive impairment. Int J Geriatr Psychiatry. 2007;22:101–105. doi: 10.1002/gps.1699. [DOI] [PubMed] [Google Scholar]
- 14.Teri L, Logsdon RG, Uomoto J, McCurry SM. Behavioral treatment of depression in dementia patients: a controlled clinical trial. J Gerontol B Psychol Sci Soc Sci. 1997;52:P159–66. doi: 10.1093/geronb/52b.4.p159. [DOI] [PubMed] [Google Scholar]
- 15.Livingston G, Johnston K, Katona C, Paton J, Lyketsos CG. Old Age Task Force of the World Federation of Biological Psychiatry. Systematic review of psychological approaches to the management of neuropsychiatric symptoms of dementia. Am J Psychiatry. 2005;162:1996–2021. doi: 10.1176/appi.ajp.162.11.1996. [DOI] [PubMed] [Google Scholar]
- 16.D'Zurilla TJ, Nezu AM. Problem-solving therapy: a social competence approach to clinical intervention. Singer; New York: 1999. [Google Scholar]
- 17.Velligan DI, Bow-Thomas CC, Huntzinger C, Ritch J, Ledbetter N, Prihoda TJ, Miller AL. Randomized controlled trial of the use of compensatory strategies to enhance adaptive functioning in outpatients with schizophrenia. Am J Psychiatry. 2000;157:1317–23. doi: 10.1176/appi.ajp.157.8.1317. [DOI] [PubMed] [Google Scholar]
- 18.Gitlin LN, Winter L, Dennis MP, Corcoran M, Schinfeld S, Hauck WW. A randomized trial of a multicomponent home intervention to reduce functional difficulties in older adults. J Am Geriatr Soc. 2006;54:809–16. doi: 10.1111/j.1532-5415.2006.00703.x. [DOI] [PubMed] [Google Scholar]
- 19.Gitlin LN, Winter L, Burke J, Chernett N, Dennis MP, Hauck WW. Tailored activities to manage neuropsychiatric behaviors in persons with dementia and reduce caregiver burden: a randomized pilot study. Am J Geriatr Psychiatry. 2008;16:229–39. doi: 10.1097/JGP.0b013e318160da72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Graff MJ, Vernooij-Dassen MJ, Thijssen M, Dekker J, Hoefnagels WH, Olderikkert MG. Effects of community occupational therapy on quality of life, mood, and health status in dementia patients and their caregivers: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2007;62:1002–9. doi: 10.1093/gerona/62.9.1002. [DOI] [PubMed] [Google Scholar]
- 21.Kittur SD, Ruskin R. Environmental modification for treatment of agitation in Alzheimer's patients. Neurorehabilitation. 2001;12:211–214. [Google Scholar]
- 22.Lawton MP. Competence, environmental press, and the adaptation of older people. In: Lawton MP, Windley PG, Byerts TO, editors. Aging and the Environments. Springer, New York; New York: 1982. [Google Scholar]
- 23.Putnam M. Linking aging theory and disability models: Increasing the potential to explore aging with physical environment. The Gerontologist. 2002;42:799–806. doi: 10.1093/geront/42.6.799. [DOI] [PubMed] [Google Scholar]
- 24.Nezu A, Nezu C, Perri M. Psychotherapy for adults within a problem-solving framework: Focus on depression. Journal of Cognitive Psychotherapy. 4(3):247–256. Fal, 1990. Special issue: Problem solving and cognitive therapy. [Google Scholar]
- 25.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alexopoulos GS, Kiosses DN, Klimstra S, Kalayam B, Bruce ML. Clinical presentation of the “depression-executive dysfunction syndrome” of late life. Am J Geriatr Psychiatry. 2002;10:98–106. [PubMed] [Google Scholar]
- 27.Jurica PJ, Leitten CL, Mattis S. Professional Manual. Psychological Assessment Resources, Inc; Lutz, Fl: 2001. DRS-2. Dementia Rating Scale-2. [Google Scholar]
- 28.Golden CJ. The Stroop Color and Word Test (Manual) Stoetling; Chicago: 1978. [Google Scholar]
- 29.Lawton MP, Moss M, Fulcomer M, Kleban MH. A research and service-oriented multilevel assessment instrument. J Gerontol. 1982;37:91–99. doi: 10.1093/geronj/37.1.91. [DOI] [PubMed] [Google Scholar]
- 30.Folstein MF, Folstein SE, McHugh PR. “Mini-Mental State”: A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 31.Leon AC, Olfson M, Portera L, Farber L, Sheehan DV. Assessing psychiatric impairment in primary care with the Sheehan Disability Scale. Int J Psychiatry Med. 1997;27:93–105. doi: 10.2190/T8EM-C8YH-373N-1UWD. [DOI] [PubMed] [Google Scholar]
- 32.Charlson ME, Pompei P, Alex KL, MacKensie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chron Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 33.Brandt J, Benedict RHB. Professional Manual. Psychological Assessment Resources; Lutz. FL: 2001. Hopkins Verbal Learning Test-Revised. [Google Scholar]
- 34.Alexopoulos GS, Meyers BS, Young RC, Kakuma T, Feder M, Einhorn A, Rosendahl E. Recovery in geriatric depression. Arch Gen Psychiatry. 1996;53:305–312. doi: 10.1001/archpsyc.1996.01830040039008. [DOI] [PubMed] [Google Scholar]
- 35.Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD. Assessment of client/patient satisfaction: development of a general scale. Eval Program Plann. 1979;2:197–207. doi: 10.1016/0149-7189(79)90094-6. [DOI] [PubMed] [Google Scholar]
- 36.Kiosses DN, Alexopoulos GS. Problem Adaptation Therapy (PATH) Manual. 2008 rev39. Unpublished manuscript. [Google Scholar]
- 37.Sacks M. Manual for brief supportive psychotherapy. 2002 Unpublished manuscript. [Google Scholar]
- 38.Gellis ZD, McGinty J, Horowitz A, Bruce ML, Misener E. Problem-solving therapy for late-life depression in home care: a randomized field trial. Am J Geriatr Psychiatry. 2007;15:968–78. doi: 10.1097/JGP.0b013e3180cc2bd7. [DOI] [PubMed] [Google Scholar]
- 39.Alexopoulos GS, Vrontou C, Kakuma T, Meyers BS, Young RC, Klausner E, Clarkin J. Disability in geriatric depression. Am J Psychiatry. 1996;153:877–885. doi: 10.1176/ajp.153.7.877. [DOI] [PubMed] [Google Scholar]