Abstract
The presence of elevated levels of glucose in blood during diabetes can lead to the non-enzymatic glycation of serum proteins such as human serum albumin (HSA). This study examined the changes that occur in binding of the sulfonylurea drug tolbutamide to HSA as the level of glycation for this protein was increased. High-performance affinity chromatography was used in this work along with columns containing various preparations of in vitro glycated HSA. It was found in frontal analysis experiments that the binding of tolbutamide with all of the tested preparations of glycated HSA could be described by a two-site model involving both strong and weak affinity interactions. The association equilibrium constants (Ka) for tolbutamide at its high affinity sites on glycated HSA were in the range of 0.8–1.2 × 105 M−1 and increased by 1.4-fold in going from normal HSA to mildly glycated HSA. It was found through competition studies that tolbutamide was binding at both Sudlow sites I and II on the glycated HSA, in agreement with previous studies. The Ka for tolbutamide at Sudlow site II increased by 1.1 to 1.4-fold in going from normal HSA to glycated HSA. At Sudlow site I, the Ka for tolbutamide increased by 1.2 to 1.3-fold in going from normal HSA to the glycated HSA samples. This information demonstrates the effects that glycation can have on drug interactions on HSA and should provide a better quantitative understanding of how the protein binding of tolbutamide in serum may be affected for individuals with diabetes.
Keywords: Tolbutamide, Human serum albumin, Glycation, Drug-protein binding, High-performance affinity chromatography
1. Introduction
It has been estimated that approximately 151 million people worldwide suffer from diabetes [1] and that 23.6 million children and adults have diabetes in the U.S. [2]. Diabetes is a group of disorders that pertain to insulin deficiency, insulin ineffectiveness, or a combination of the two, resulting in glucose intolerance or hypoglycemia [1]. Type I diabetes (i.e., juvenile-onset diabetes) occurs when the immune system destroys the cells that make insulin and control blood glucose levels. Type II diabetes (i.e., non-insulin dependent diabetes) begins with insulin resistance and leads to an eventual decrease in insulin production. Type I and II diabetes occur in 5–10% and 90–95% of patients with diabetes, respectively [2]. Diabetes can lead to complications such as cardiovascular disease, nerve damage, renal failure, and blindness. However, with proper treatment many of these complications can be delayed or prevented. Roughly 57% of people with diabetes take oral medication alone to treat this disease and 13% take both insulin and oral medication for treatment [2].
Sulfonylurea drugs are often used to treat type II diabetes, either alone or in combination with other drugs [3]. Tolbutamide (see Figure 1) was the first drug in this class to be used to treat diabetes and has remained an important agent for this use since its discovery in 1956 [3]. At therapeutic levels, tolbutamide is 90% protein-bound in the circulation. This binding is of interest for tolbutamide and other first-generation sulfonylureas (e.g., chlorpropamide, acetohexamide, and tolazamide) because these agents are thought to be more easily displaced from their carrier proteins than their second-generation counterparts [4]. In addition, even a small change in the free (non-protein bound) fraction of tolbutamide can lead to severe hypoglycemia [5,6].
Figure 1.
Structure of tolbutamide.
Human serum albumin (HSA) is the most abundant protein in human plasma [6–12] and is the main carrier protein for tolbutamide in serum [4]. This protein has a serum concentration of ~40 g/L and is known to have two major binding sites for drugs: Sudlow sites I and II [13]. Sudlow site I, which is found in subdomain IIA of HSA, binds to bulky heterocyclic compounds such as coumarins, sulfonamides, and salicylate [6,8,9,14–16]. Sudlow site II, found in subdomain IIIA, binds to aromatic carboxylic acids and profens [6,8,9,15]. HSA is able to bind and transport both endogenous solutes (e.g., unesterified fatty acids) as well as a wide range of drugs [6]. This binding can have a large affect on the pharmacologic and pharmacokinetic properties of a drug such as tolbutamide by affecting its metabolism, excretion, and bioavailability [6,17].
One process that is believed to affect the binding of drugs to HSA is glycation. Glycation refers to the modification of a protein by a process that begins with the reaction between a reducing sugar and a free amine group on a protein [10,18]. This process can occur for HSA and becomes more pronounced in diabetes when an elevated amount of glucose is present in the bloodstream. While an average individual has 6–13% of HSA in a glycated form, a person with diabetes may have 20–30% or more glycated HSA in the circulation [6,10,11]. It has recently been shown that some of the primary modification sites for glycated HSA are at or near Sudlow sites I and II [11,18,19]. This information, in turn, has created interest in how these modifications may affect the binding of drugs such as tolbutamide to HSA [20].
This study will use high-performance affinity chromatography (HPAC) to examine the binding of tolbutamide to HSA with various levels of glycation. HPAC is a type of HPLC that uses a biological ligand as the stationary phase. HPAC has been used for many years as a selective separation and analysis technique for chemical isolation and analysis, but this approach can also be used as a tool to study various biological interactions (e.g., see recent review in Ref. [21]). This current study will use columns that contain immobilized glycated HSA to examine the binding of tolbutamide with this protein under various experimental conditions. Some benefits of using HPAC over more traditional methods for drug binding studies (e.g., equilibrium dialysis or ultrafiltration) include the good precision and reproducibility of HPAC plus its small sample requirements and ease of automation. The ability to reuse the same protein preparation for many experiments is also an attractive feature of HPAC, as well as its good correlation versus reference methods (e.g., as has been shown in numerous studies for normal HSA; see review in Ref. [21,22]).
This current report will first use frontal analysis to determine how the association equilibrium constants and binding capacities change for columns containing in vitro glycated HSA with increasing levels of glycation [21,22]. Zonal elution studies will then be performed to specifically examine the binding of tolbutamide at Sudlow sites I and II of HSA as the levels of glycation are increased [21,22]. The knowledge gained from these studies should give a better description of how glycation changes the binding of tolbutamide with HSA. This information, in turn, may lead to the development of more effective drug treatment regimes based on personalized medicine for patients with diabetes.
2. Theory
2.1 Frontal Analysis
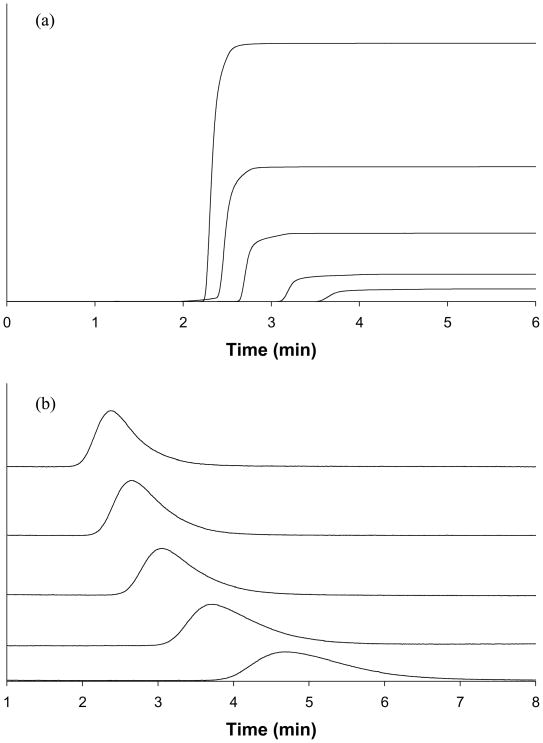
Frontal analysis (or frontal affinity chromatography) was used to determine the association equilibrium constant(s), Ka, and moles of binding sites, mL, for tolbutamide with glycated HSA. An example of this type of experiment is given in Figure 2(a). If a system has single-site binding, Eqns. (1) and (2) in Table 1 can be used with frontal analysis data to provide information on the binding of an applied drug to the immobilized protein [21,22]. In these equations, mLapp is the apparent moles of drug required to reach the central position of the breakthrough curve at a given concentration of the applied drug. According to Eqn. (1), a plot of 1/mLapp vs. 1/[A] should give a linear relationship if the drug binds to only one type of binding site on the protein. In addition, deviations from linearity at high drug concentrations (i.e., low 1/[A] values) can be used to detect multi-site interactions between the drug and protein [22].
Figure 2.
(a) Frontal analysis and (b) zonal elution studies for tolbutamide on the gHSA1 column. The tolbutamide concentrations in (a) were (top-to-bottom) 200, 100, 50, 20, and 10 μM. The results in (b) were obtained using R-warfarin as a probe for Sudlow site II, along with tolbutamide concentrations in the mobile phase (top-to-bottom) of 20, 15, 10, 5, and 1 μM.
Table 1.
Equations used in frontal analysis and zonal elution experiments to obtain binding parameters for a drug with an immobilized protein such as HSAa
| Frontal Analysis | ||||||
Single-site binding
| ||||||
Two-site binding
| ||||||
| Zonal Elution | ||||||
Single-site competition
|
Similar expressions to Eqns. (1)–(2) can be written for a drug-protein system with more than one type of interaction site, as shown in Eqns. (3) and (4) for a two-site binding model [21,22]. In these equations, Ka1 and Ka2 are the association equilibrium constants of the applied analyte A at sites 1 and 2, and mL1 or mL2 are the binding capacities for A at these sites. The term α1 represents the fraction of all binding regions that make up the high affinity binding sites (i.e., α1 = mL1,tot/mLtot). The term β2 is the ratio of the association equilibrium constants for the lower affinity site (Ka2) versus the highest affinity site, where β2 = Ka2/Ka1 and 0 < Ka2 < Ka1. According to Eqn. (3), a non-linear response for a plot of 1/mLapp vs. [A] would be expected throughout a broad range of concentrations for a system with multi-site binding. However, at low concentrations a linear response can still be observed. In this case, Eqn. (3) approaches the linear form shown in Eqn. (5) that can be used to estimate the association equilibrium constant for the highest affinity sites by using data obtained at low analyte concentrations [23].
2.2 Zonal Elution
HPAC and the method of zonal elution were used to examine the binding of tolbutamide to glycated HSA at specific binding sites (see Figure 2(b)). In this approach, the retention time (tR) of injected probe A (i.e., R-warfarin or L-tryptophan in this study) is measured in the presence of various mobile phase concentrations of competing agent I (e.g., tolbutamide) and is used to calculate the retention factor (k) for the injected probe, where k = (tR–tM)/tM) and tM is the elution time of a non-retained solute (e.g., sodium nitrate).
If the injected probe and competing agent have direct competition at a single type of site on an immobilized protein, Eqn. (6) in Table 1 can be used to describe the relationship between the measured retention factor for A and the concentration of I [21,22]. In this equation, KaI and KaA are the association equilibrium constants for the competing agent and site-selective probe, respectively, at their site of competition and VM is the void volume. A plot of 1/k vs. [I] in this case should yield a linear response if A and I follow a model based on direct competition at a single type of binding site. The best-fit line for such a system can then be used to find the association equilibrium constant for I at the site of competition by dividing the slope by the intercept. If multi-site competition or allosteric effects are present, a non-linear response would instead be observed [22].
3. Experimental
3.1 Reagents
The tolbutamide ( ≥ 99.9% pure), R-warfarin (≥ 97%), L-tryptophan (98%), HSA (essentially fatty acid free, ≥ 96%), and commercial glycated HSA (Lot 058K6087) were purchased from Sigma-Aldrich (St. Louis, MO, USA). The Nucleosil Si-300 (7 micron particle diameter, 300 Å pore size) was from Macherey-Nagel (Düren, Germany). Reagents for the bicinchoninic acid (BCA) protein assay were from Pierce (Rockford, IL, USA). The assay kit for fructosamine (used for measuring glycation levels) was from Diazyme Laboratories (San Diego, CA, USA). All aqueous were made using water from a Nanopure system (Barnstead, Dubuque, IA, USA) and filtered with a 0.20 μm GNWP nylon membrane from Millipore (Billerica, MA, USA).
3.2 Apparatus
The HPLC system consisted of a Jasco DG-2080-53 three-solvent degasser (Tokyo, Japan), two Jasco PU-2080 isocratic pumps, a Rheodyne Advantage PF six-port valve (Cotati, CA, USA), a Jasco AS-2055 autosampler, a Jasco CO-2060 column oven, and a Jasco UV-2075 UV/Vis detector. The HPLC system hardware was controlled by EZChrom Elite software v3.2.1 (Scientific Software, Pleasanton, CA, USA) via Jasco LC Net hardware. An in-house version of Labview 5.1 software (National Instruments, Austin, TX, USA) was used to analyze the frontal analysis curves while PeakFit 4.12 (Jandel Scientific Software, San Rafael, CA, USA) was used to determine the central moments of peaks obtained from zonal elution experiments. Linear regression was performed using Excel 2003 (Microsoft Corporation, Redmond, WA, USA) and non-linear regression was performed using DataFit (Oakdale Engineering, PA, USA).
3.3 Methods
3.3.1 Column and Sample Preparation
Diol silica was made using Nucleosil Si-300 silica, and HSA was immobilized to the diol silica by the Schiff base method, both according to previously-published procedures [16]. Control supports were prepared in the same manner but with no HSA being added during the immobilization step. Although both the Schiff base immobilization method and glycation involve the use of free amine groups on a protein, it has been found that these two processes mainly involve different residues on HSA; it has also been shown that the prior glycation of HSA (e.g., under the same conditions as used in this report) does not change the specific activities at Sudlow sites I and II when using warfarin or L-tryptophan as probes for these sites [24].
A BCA assay was performed in triplicate to determine the protein content of each glycated HSA support, using soluble glycated HSA as the standard and the control support as the blank. This report used three batches of HSA for immobilization, with each batch containing a different level of glycation. The first HSA sample was purchased from Sigma (referred to here as “gHSA1”). The second and the third samples (i.e., “gHSA2” and “gHSA3”, respectively) were made in vitro by incubating a 42 g/L HSA solution for one month in sterile pH 7.4 phosphate buffer with 15 mM or 30 mM glucose at 37ºC (Note: Sodium azide was also added to prevent bacterial growth during incubation). The protein was then purified, lyophilized, and stored at −80 °C until further use, according to methods described in Ref. [24]. An enzymatic fructosamine assay from Diazyme Laboratories was used to determine the level of glycation for each sample, as described previously [24], with the results being expressed as mol hexose/mol HSA.
The glycated HSA supports were downward slurry-packed into separate 2.0 cm × 2.1 mm I.D. columns at 3500 psi (24 MPa) using pH 7.4, 0.067 M potassium phosphate buffer as the packing solution. The control supports for each gHSA sample were packed into separate columns under the same conditions. These columns were stored at 4 °C in the packing solution and used over a period of one year and fewer than 500 sample applications per column. The routine washing of these columns with fresh portions of sterile phosphate buffer during the binding studies made it unnecessary to include a preservative in this buffer; this approach also helped maintain conditions that closely corresponded to those seen in vivo in serum during the binding studies. Columns containing normal HSA that have been used in this manner have been found in previous studies to retain good stability for drug-protein binding studies under such conditions [25].
The tolbutamide, R-warfarin, and L-tryptophan solutions were all made in pH 7.4, 0.067 M potassium phosphate buffer. This same buffer was used as the application and elution buffer in the chromatographic studies. All mobile phases were filtered through a 0.2 μM nylon filter and degassed for 10–15 min prior to use. A flow rate of 0.5 ml/min was used for both the frontal analysis and zonal elution studies, with all experiments being carried out at 37°C. This flow rate has been shown in previous studies to give reproducible retention factors and binding capacities for drug binding studies conducted on similar columns containing normal HSA [26,27].
3.3.2 Chromatographic Studies
In the frontal analysis studies, the column was first equilibrated with pH 7.4, 0.067 M potassium phosphate buffer. A switch was then made between the pH 7.4 buffer and a drug solution that was prepared in the same buffer. Once the drug had saturated the column and produced a breakthrough curve, the pH 7.4 buffer was again passed through the column to elute the retained drug. The drug solutions contained 1–200 μM tolbutamide and the elution of tolbutamide was monitored at 250 nm. Although the pKa of sulfonylurea drugs like tolbutamide range from 5.2–6.2, even the solutions containing the highest concentration of tolbutamide in this study gave less than a 0.05 change in pH for the pH 7.4 buffer, and the pH of this solution was found to vary by less than 0.05 units over the course of this study. The frontal analysis experiments were performed in triplicate at each drug concentration. The breakthrough curves were analyzed by using Labview 5.1 and the equal areas method [22]. A correction for non-specific binding to the system was made by subtracting the results for the control column from the data obtained for each glycated HSA column.
Zonal elution competition studies were performed in triplicate using R-warfarin as a probe for Sudlow site I and L-tryptophan as a probe for Sudlow site II [13]. Tolbutamide concentrations of 1–20 μM were placed in the mobile phase while 20 μL injections of 5 μM R-warfarin or L-tryptophan were made. These sample concentrations have been shown to provide linear elution conditions for similar HSA columns [14,28]. The elution of R-warfarin and L-tryptophan was monitored at 308 or 280 nm, respectively. Injections containing 20 μL of 20 μM sodium nitrate were made under the same conditions using only the pH 7.4 buffer as the mobile phase. Sodium nitrate was used as a non-retained solute to determine column void time, with the elution of sodium nitrate being monitored at 205 nm. The resulting peaks were fit to an exponentially-modified Gaussian curve and analyzed using PeakFit v4.12.
4. Results and Discussion
4.1 Preparation of Glycated HSA
Earlier reports examining the binding of tolbutamide with HSA and glycated HSA have examined either changes in the binding capacities of these proteins or the differences in their apparent binding constants [5,20]. These same reports, however, did not consider how the tolbutamide-HSA interactions might change with various levels of glycation for HSA. In addition, these reports measured binding constants at lower temperatures than are present in the body (e.g., 20°C for the fluorescence quenching assay in Ref. [5]) or used higher glucose concentrations for HSA glycation than are found in the body during diabetes [20]. These issues and limitations were overcome in this current investigation by carrying out all binding studies at 37ºC and by using HSA samples that had undergone various known levels of glycation and that were prepared under conditions similar to those found in serum during diabetes.
The glycated HSA samples that were used in this study were the same as employed in recent work examining the changes in the HSA interactions with warfarin and L-tryptophan during glycation [24]. The first sample of glycated HSA (gHSA1) contained 1.31 (± 0.05) mol hexose/mol HSA (Note: the value in parentheses represents ± 1 S.D. for the population of results). This sample was used to represent mildly glycated HSA, as might be found during pre-diabetes or early state diabetes. The second glycated HSA sample (gHSA2) had a glycation level of 2.34 (± 0.13) mol hexose/mol HSA; this sample was made using a glucose concentration and conditions typical of those seen in many diabetic patients [29]. The third sample (gHSA3) had a glycation level of 3.35 (± 0.14) mol hexose/mol HSA, as might be present in uncontrolled or advanced diabetes. After these various preparations of glycated HSA had been immobilized, the resulting supports were determined to have protein contents of 29 (± 4), 47 (± 8), and 40 (± 3) mg protein/g silica, respectively, or ~440–710 nmol HSA/g silica. These protein contents were comparable to those noted in earlier work with normal HSA and comparable supports prepared by the same methods [16].
4.2 Frontal Analysis Studies of Tolbutamide Binding to Glycated HSA
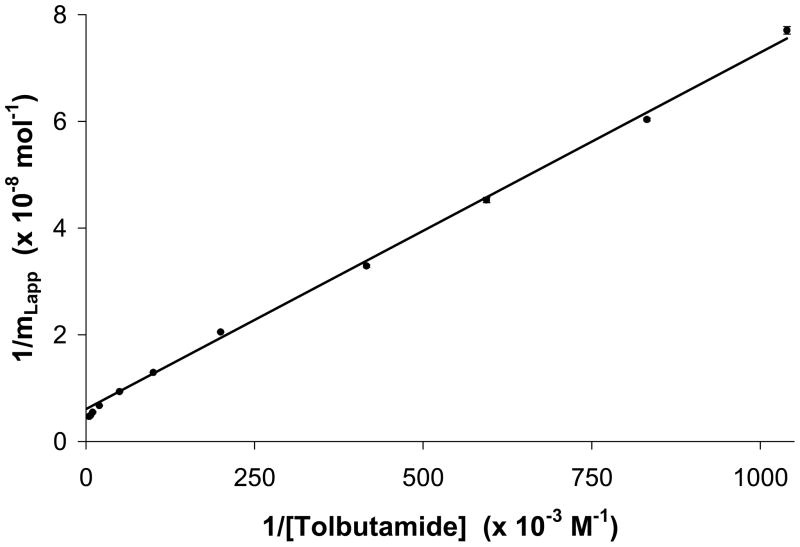
The method of frontal analysis was used to gather information about the overall binding of tolbutamide to glycated HSA. The data that was obtained for each type of glycated HSA column was first plotted using a double-reciprocal plot (see example in Figure 3). When using this type of model and plot, each glycated HSA column gave deviations at high drug concentrations (i.e., low values of 1/[Tolbutamide]) from the expected linear response for a single-site binding model, as described by Eqn. (1). This result indicated that tolbutamide was binding to more than one binding site on each type of glycated HSA. This behavior was consistent with similar studies using normal HSA, which has also been found to have multi-site interactions for tolbutamide [30].
Figure 3.
Double-reciprocal plot of frontal analysis data obtained for tolbutamide on the gHSA1 column. The best-fit line for the upper linear region when analyzed according to Eqn. (5) is y = 670 (± 20) x + [6.1 (± 1.0) × 107], r = 0.999, n = 6. The error bars represent a range of ± 1 SD and are of a comparable size to the data markers in this plot.
Eqn. (5) was next used with the upper linear region of plots like those in Figure 3 to estimate the association equilibrium constant at the high-affinity sites for tolbutamide, according to a method from Ref. [23,24]. This fit was obtained using data at tolbutamide concentrations of 1–10 μM for each of the columns. The resulting Ka values were between 0.9 and 1.1 × 105 M−1 at 37°C and pH 7.4, with correlation coefficients of at least 0.999 (n = 5 or 6) being noted for a linear fit to the given region of the double-reciprocal plots for all glycated HSA columns. These results were similar but slightly higher than a value of 0.82 (± 0.04) × 105 M−1 that was obtained by the sample approach when examining the high affinity sites of tolbutamide on normal HSA [30].
A two-site model was next employed to examine the binding of tolbutamide with the glycated HSA columns (see Figure 4). This was accomplished by analyzing the frontal analysis data through the use of Eqn. (4) and non-linear regression. A two-site model has been shown in earlier work to give the best fit for frontal analysis data acquired for tolbutamide with normal HSA [30]. This model was also found in this current report to give a good fit for the results obtained with tolbutamide on each glycated HSA column, giving correlation coefficients of at least 0.999 (n = 9 to 11). Only random variations in the data about the best-fit lines were observed in these plots, along with a small sum of the square of the residuals (range, 0.8 × 10−19 to 3.8 × 10−19). This overall fit gave much better agreement with the data than a single-site model, which instead exhibited non-random variations of the residuals about the best-fit lines along with correlation coefficients that ranged from 0.965–0.998, and larger values for the sum of the square of the residuals (range, 4.3 × 10−18 to 7.4 × 10−18).
Figure 4.
Plot of mLapp versus [Tolbutamide] for the gHSA1 column, as analyzed according to Eqn. (4) and a two-site model. The best-fit values obtained for the association equilibrium constants and binding capacities are summarized in Table 2. The data used in this plot was the same as in Figure 3. The error bars for the data points (not shown) are comparable in size to the data markers in this plot.
A summary is provided in Table 2 of the association equilibrium constants and amount of each class of binding sites that were noted when using the two-site model for tolbutamide on the glycated HSA columns. In this table, the association equilibrium constants found for the high affinity regions (Ka1) were in good general agreement with the values of 0.9–1.1 × 105 M−1 that were estimated from the linear regions of plots prepared according to Eqn. (5), as described previously in this section. When these results were compared to data that were obtained by the same approach for tolbutamide on a normal HSA column (see entry from Ref. [30] for normal HSA in Table 2), a 1.4-fold increase in affinity was present in going from normal HSA (Ka1 = 0.87 (± 0.06) × 105 M−1) to the gHSA1 sample (Ka1 = 1.2 (± 0.2) × 105 M−1), a change which was significant at the 95% confidence level. The apparent association equilibrium constant for the high affinity regions returned to comparable values versus normal HSA when using the gHSA2 and gHSA3 samples, which had Ka1 values of 0.84 (± 0.16) × 105 M−1 and 0.89 (± 0.06) × 105 M−1, respectively. The corresponding mL1 values for these high-affinity regions were 1.1–2.2 × 10−8 mol and corresponded to specific activities of approximately 0.82–1.0 for all of these high affinity regions, with no apparent change in these values as the level of glycation was varied.
Table 2.
Binding constants obtained for tolbutamide with HSA or glycated HSA at pH 7.4 and 37°C when using frontal analysis and a two-site binding modela
| Tolbutamide | Ka1 (× 105 M−1) | mL1 (× 10−8 mol) | Specific activity | Ka2 (× 103 M−1) | mL2 (× 10−8 mol) | Specific activityb |
|---|---|---|---|---|---|---|
| Normal HSAc | 0.87 (± 0.06) | 2.0 (± 0.1) | 1.1 (± 0.1) | 8.1 (± 1.7) | 1.8 (± 0.1) | 1.0 (± 0.1) |
| gHSA1 | 1.2 (± 0.2) | 1.1 (± 0.2) | 0.82 (± 0.18) | 9.5 (± 3.2) | 1.7 (± 0.1) | 1.2 (± 0.2) |
| gHSA2 | 0.84 (± 0.16) | 2.2 (± 0.4) | 1.0 (± 0.3) | 7.8 (± 5.1) | 1.9 (± 0.2) | 0.87 (± 0.18) |
| gHSA3 | 0.89 (± 0.06) | 1.9 (± 0.1) | 1.1 (± 0.1) | 1.7 (± 1.1) | 3.6 (± 1.4) | 1.9 (± 0.8) |
The values in parenthesis represent a range of ± 1 S.D for the population of results (n = 9–11). These values were determined by using error propagation and the standard deviations of the slopes and intercepts that were obtained from best-fit lines generated according to Eqn. (4).
The specific activity refers to the moles of tolbutamide that were bound per mole of immobilized HSA or glycated HSA.
The results provided for normal HSA are based on previous work described in Ref. [30] and were acquired using experimental conditions identical to those used in this current report for glycated HSA.
The association equilibrium constants calculated for the lower affinity sites were comparable to those obtained for tolbutamide when using similar affinity columns containing normal HSA (for the latter value, see entry for normal HSA in Table 2 from Ref. [30]). The strength of these weak affinity interactions was similar for normal HSA (Ka2 = 8.1 (± 1.7) × 103 M−1) [30] versus gHSA1 or gHSA2, in which these last two samples gave Ka2 values of 9.5 (± 3.2) × 103 M−1 and 7.8 (± 5.1) × 103 M−1, respectively. However, there was an apparent decrease in Ka2 in going from normal HSA to gHSA3, in which this last sample had a Ka2 value of 1.7 (± 1.1) × 103 M−1. The corresponding specific activities for tolbutamide at these low affinity sites ranged from 0.87 to 1.9 for the various glycated samples, which were comparable to a value of 1.0 (± 0.1) that has been noted for tolbutamide with similar columns containing normal HSA [30].
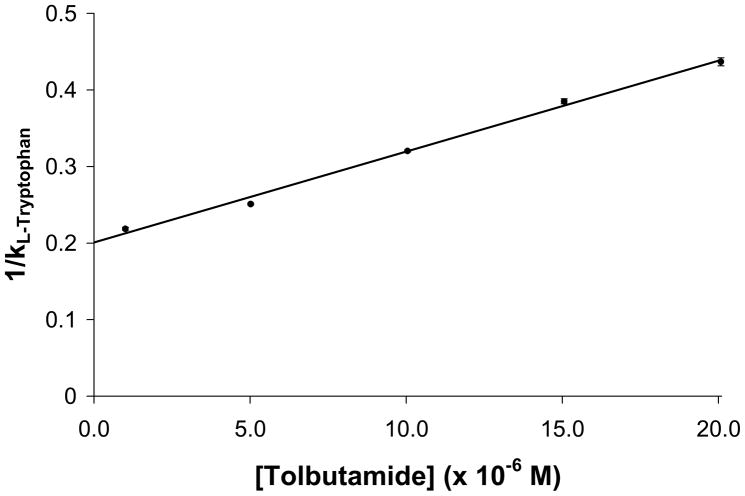
4.3 Site-Specific Interactions of Tolbutamide at Sudlow Site II
Zonal elution competition studies were used to further examine the interactions of tolbutamide with glycated HSA. L-Tryptophan was first used in such work as a site-selective probe to examine the binding of tolbutamide at Sudlow site II [30]. When the data from these experiments were plotted according to Eqn. (6), a linear fit for all the glycated HSA columns was observed (see example of such a plot in Figure 5). Similar linear behavior and correlation coefficients between 0.998 and 0.999 (n = 5) were obtained for each glycated HSA column examined in this study. In each case, only random residuals were noted about the best-fit line. Based on this fit, it was determined that tolbutamide and L-tryptophan had direct competition at a single site. In addition, it was possible to determine that this competition was taking place at Sudlow site II because L-tryptophan is known to bind selectively at this site on both normal HSA and the types of glycated HSA that were examined in this study [24,28]. This result agrees with previous competition studies in which tolbutamide has been found to be displaced by probes for Sudlow site II from both normal HSA and glycated HSA [30].
Figure 5.
Zonal elution studies on the gHSA1 column for the injection of L-tryptophan as a site-selective probe for Sudlow site II in the presence of tolbutamide as a competing agent. The best-fit line obtained when using Eqn. (6) is y = [1.2 (± 0.1) × 104] x + 0.20 (± 0.01), r = 0.998, n = 5. The error bars represent a range ± 1 SD and are comparable in size to the data markers in this plot.
By using the best-fit lines from these plots and Eqn. (6), it was possible to find the association equilibrium constant for tolbutamide at Sudlow site II by taking the ratio of the slope to the intercept for each plot. This method has been used in a previous study with normal HSA to obtain a site-specific association equilibrium constant of 5.3 (± 0.2) × 104 M−1 for tolbutamide at Sudlow site II [30]. The association equilibrium constants values that were obtained at the same site in this study are summarized in Table 3. In going from normal HSA to the mild level of glycation that was present in gHSA1, the size of Ka for tolbutamide at Sudlow site II was found to increase by 1.1-fold to 5.9 (± 0.3) × 104 M−1 (i.e., an increase that was significant at the 90% confidence level). This was followed by higher values of 7.2 (± 0.3) × 104 M−1 for the gHSA2 sample and 6.4 (± 0.3) × 104 M−1 for the gHSA3 sample, or 1.4- to 1.2-fold increases versus normal HSA that were significant at the 95% confidence level. It was also possible from the intercepts of these plots to determine how the specific activity for tolbutamide at Sudlow site II was affected as the level of glycation for HSA was increased. When this was done, no significant change in specific activity was seen at the 95% confidence level for tolbutamide at Sudlow site II in going from normal HSA to any of the glycated HSA columns.
Table 3.
Association equilibrium constants measured for tolbutamide at Sudlow sites I and II at pH 7.4 and 37°Ca
| Tolbutamide | Sudlow Site I (R-warfarin) (× 104 M−1) | Sudlow Site II (L-tryptophan) (× 104 M−1) |
|---|---|---|
| Normal HSAb | 5.5 (± 0.2) | 5.3 (± 0.2) |
| gHSA1 | 6.9 (± 0.2) | 5.9 (± 0.3) |
| gHSA2 | 6.6 (± 0.5) | 7.2 (± 0.3) |
| gHSA3 | 6.5 (± 0.2) | 6.4 (± 0.3) |
The values in parenthesis represent a range of ± 1 S.D for the population of results. These values were determined by using error propagation and the standard deviations of the slopes and intercepts that were obtained from best-fit lines generated according to Eqn. (6).
The results provided for normal HSA are based on previous work described in Ref. [30] and were acquired using experimental conditions identical to those used in this current report for glycated HSA.
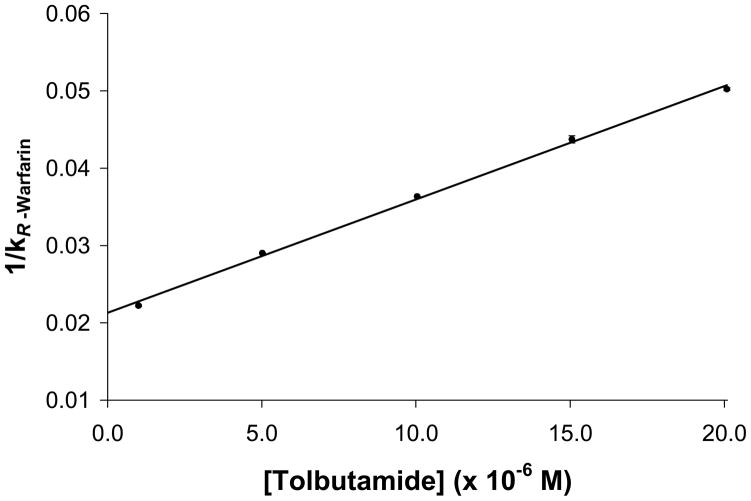
4.4 Site-Specific Interactions of Tolbutamide at Sudlow Site I
Site-specific studies where also carried out using competition studies and R-warfarin as a site-specific probe for Sudlow site I [14,16]. These results were again plotted according to Eqn. (6), with an example being given in Figure 6. All of the glycated HSA columns gave linear behavior for this type of plot, with correlation coefficients that ranged from 0.994 to 0.999 (n = 5) and with only random variations in the residuals being observed about the best-fit line. This type of behavior indicated that tolbutamide and R-warfarin were competing directly at Sudlow site I on HSA. Similar results have been noted in prior competition studies for tolbutamide with probes for Sudlow site I when using both normal HSA and glycated HSA [30].
Figure 6.
Zonal elution studies on the gHSA1 column for the injection of R-warfarin as a site-selective probe for Sudlow site I in the presence of tolbutamide as a competing agent. The best-fit line obtained when using Eqn. (6) is y = 1500 (± 100) x + 0.021 (± 0.001), r = 0.999, n = 5. The error bars represent a range of ± 1 SD and are comparable in size to the data markers in this plot.
The association equilibrium constant for tolbutamide at Sudlow site I on each of the glycated HSA samples was found by using the best-fit lines of plots prepared according to Eqn. (6). The results are summarized in Table 3. The Ka value for tolbutamide at Sudlow site I on the gHSA1 column was roughly 1.3-fold higher than the value of 5.5 (± 0.2) × 104 M−1 that has previously been measured for tolbutamide at this site on normal HSA [30]. A comparable, roughly 1.2-fold increase in affinity versus normal HSA was measured at the same site for the gHSA2 and gHSA3 samples. All of the association equilibrium constants measured at Sudlow site I for tolbutamide with the glycated HSA samples where significantly different at the 95% confidence level when compared to the Ka value reported for tolbutamide at the same site on normal HSA. No significant change at 95% confidence level was seen in the specific activity for tolbutamide at Sudlow site I in going from normal HSA to the glycated HSA columns.
5. Conclusion
This report looked at how the binding of tolbutamide with HSA changes as the level of glycation for HSA is increased. Experiments based on the use of HPAC and frontal analysis indicated that the binding of tolbutamide with glycated HSA followed a two-site model that included a group of high affinity sites and a set of lower affinity interactions. This behavior was in agreement with a previous report that has studied the binding of tolbutamide with normal HSA [30]. The association equilibrium constants for the high affinity interactions were in the general range of 0.8–1.2 × 105 M−1 and increased by 1.4-fold in going from normal HSA to mildly glycated HSA (i.e., the gHSA1 sample), with the overall affinity returning to more normal levels at higher levels of glycation (as noted for the gHSA2 and gHSA3 samples). Competition studies based on zonal elution experiments found that the association equilibrium constant of tolbutamide at Sudlow site I increased by 1.2 to 1.3-fold in going from normal HSA to all of the tested samples of glycated HSA. At Sudlow site II, the association equilibrium constant for tolbutamide increased by 1.1- to 1.4-fold in going from normal HSA to all of the tested samples of glycated HSA. Such an increase in binding affinity to HSA upon glycation could potentially lower the amount of non-bound drug that is available for binding to receptors and may affect the rate of metabolism or extraction and the overall half-life of tolbutamide in the circulation.
As demonstrated in this report, the binding data that can be obtained through this type of research can result in a better understanding of how glycation may change the interactions of drugs such as tolbutamide to HSA during diabetes. This information should aid in the future development of better patient treatments for personalized medicine by allowing physicians to better understand how glycation may affect the activity of such a drug in the circulation and to make appropriate adjustments in the prescribed dose when using tolbutamide and related drugs. Similar binding studies are now being carried out with in vivo glycated HSA. Work with additional pharmaceutical agents, including other sulfonylurea compounds, is also in progress to determine the extent to which the interactions of these drugs may vary during glycation of HSA.
Acknowledgments
This research was supported by National Institutes of Health under grant R01 DK069629 and was conducted in facilities that were renovated under NIH grant RR015468-01.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Unwin N, Whiting D, Gan D, Jacqmain O, Ghyoot G, editors. Diabetes Atlas. International Diabetes Federation; 2009. [Google Scholar]
- 2.National diabetes fact sheet: General information and national estimates on diabetes in the United States. US Centers for Disease Control and Prevention; Atlanta, GA: 2007. 2008. [Google Scholar]
- 3.Skillman TG, Feldman JM. The pharmacology of sulfonylureas. Am J Med. 1981;70:361–372. doi: 10.1016/0002-9343(81)90773-7. [DOI] [PubMed] [Google Scholar]
- 4.Jakoby MG, Covey DF, Cistola DP. Localization of tolbutamide binding sites on human serum albumin using titration calorimetry and heteronuclear 2-D NMR. Biochem. 1995;34:8780–8787. doi: 10.1021/bi00027a029. [DOI] [PubMed] [Google Scholar]
- 5.Koyama H, Sugioka N, Uno A, Mori S, Nakajima K. Effects of glycosylation of hypoglycaemic drug binding to serum albumin. Biopharm Drug Dispos. 1997;18:791–801. doi: 10.1002/(sici)1099-081x(199712)18:9<791::aid-bdd66>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 6.Colmenarejo G. In silico prediction of drug-binding strengths to human serum albumin. Med Res Rev. 2003;23:275–301. doi: 10.1002/med.10039. [DOI] [PubMed] [Google Scholar]
- 7.Abou-Zied OK, Al-Shihi OIK. Characterization of subdomain IIA binding site of human serum albumin in its native, unfolded, and refolded states using small molecular probes. J Am Chem Soc. 2008;130:10793–10801. doi: 10.1021/ja8031289. [DOI] [PubMed] [Google Scholar]
- 8.Ascenzi P, Bocedi A, Notari S, Fanali G, Fesce R, Fasano M. Allosteric modulation of drug binding to human serum albumin. Mini-Rev Med Chem. 2006;6:483–489. doi: 10.2174/138955706776361448. [DOI] [PubMed] [Google Scholar]
- 9.Fasano M, Curry S, Terreno E, Galliano M, Fanali G, Narciso P, Notari S, Ascenzi P. The extraordinary ligand binding properties of human serum albumin. IUBMB Life. 2005;57:787–796. doi: 10.1080/15216540500404093. [DOI] [PubMed] [Google Scholar]
- 10.Mendez DL, Jensen RA, McElroy LA, Pena JM, Esquerra RM. The effect of non-enzymatic glycation on the unfolding of human serum albumin. Arch Biochem Biophys. 2005;444:92–99. doi: 10.1016/j.abb.2005.10.019. [DOI] [PubMed] [Google Scholar]
- 11.Nakajou K, Watanabe H, Kragh-Hansen U, Maruyama T, Otagiri M. The effect of glycation on the structure, function and biological fate of human serum albumin as revealed by recombinant mutants. Biochim Biophys Acta. 2003;1623:88–97. doi: 10.1016/j.bbagen.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 12.Petitpas I, Bhattacharya AA, Twine S, East M, Curry S. Crystal structure analysis of warfarin binding to human serum albumin. J Biol Chem. 2001;276:22804–22809. doi: 10.1074/jbc.M100575200. [DOI] [PubMed] [Google Scholar]
- 13.Sudlow G, Birkett DJ, Wade DN. Further characterization of specific drug binding sites on human serum albumin. Mol Pharmacol. 1976;12:1052–1061. [PubMed] [Google Scholar]
- 14.Moser AC, Kingsbury C, Hage DS. Stability of warfarin solutions for drug-protein binding measurements: Spectroscopic and chromatographic studies. J Pharm Biomed Anal. 2006;41:1101–1109. doi: 10.1016/j.jpba.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 15.Dockal M, Chang M, Carter DC, Ruker F. Five recombinant fragments of human serum albumin--tools for the characterization of the warfarin binding site. Prot Sci. 2000;9:1455–1465. doi: 10.1110/ps.9.8.1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Joseph KS, Moser AC, Basiaga S, Schiel JE, Hage DS. Evaluation of alternatives to warfarin as probes for Sudlow site I of human serum albumin: Characterization by high-performance affinity chromatography. J Chromatogr A. 2009;1216:3492–3500. doi: 10.1016/j.chroma.2008.09.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ascoli GA, Domenici E, Bertucci C. Drug binding to human serum albumin: Abridged review of results obtained with high-performance liquid chromatography and circular dichroism. Chirality. 2006;18:667–679. doi: 10.1002/chir.20301. [DOI] [PubMed] [Google Scholar]
- 18.Garlick RL, Mazer JS. The principal site of nonenzymatic glycosylation of human serum albumin in vivo. J Biol Chem. 1983;258:6142–6146. [PubMed] [Google Scholar]
- 19.Iberg N, Fluckiger R. Nonenzymatic glycosylation of albumin in vivo. J Biol Chem. 1986;261:13542–13545. [PubMed] [Google Scholar]
- 20.Tsuchiya S, Sakurai T, Sekiguchi S-i. Nonenzymatic glucosylation of human serum albumin and its influence on binding capacity of sulfonylureas. Biochem Pharmacol. 1984;33:2967–2971. doi: 10.1016/0006-2952(84)90595-1. [DOI] [PubMed] [Google Scholar]
- 21.Schiel JE, Joseph KS, Hage DS. Biointeraction affinity chromatography. In: Grinsberg N, Grushka E, editors. Adv Chromatogr. Chap 4. Taylor & Francis; New York: 2010. [PubMed] [Google Scholar]
- 22.Hage DS. High-performance affinity chromatography: A powerful tool for studying serum protein binding. J Chromatogr B. 2002;768:3–30. doi: 10.1016/s0378-4347(01)00482-0. [DOI] [PubMed] [Google Scholar]
- 23.Tweed SA, Loun B, Hage DS. Effects of ligand heterogeneity in the characterization of affinity columns by frontal analysis. Anal Chem. 1997;69:4790–4798. doi: 10.1021/ac970565m. [DOI] [PubMed] [Google Scholar]
- 24.Joseph KS, Hage DS. The effects of glycation on the binding of human serum albumin to warfarin and L-tryptophan. J Pharm Biomed Anal. 2010;53:811–818. doi: 10.1016/j.jpba.2010.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang J, Hage DS. Effect of mobile phase composition on the binding kinetics of chiral solutes on a protein-based high-performance liquid chromatography column: Interactions of D- and L- tryptophan with immobilized human serum albumin. J Chromatogr A. 1997;766:15–25. doi: 10.1016/s0021-9673(96)01040-0. [DOI] [PubMed] [Google Scholar]
- 26.Loun B, Hage DS. Chiral separation mechanisms in protein-based HPLC columns. 1. Thermodynamic studies of (R)- and (S)-warfarin binding to immobilized human serum albumin. Anal Chem. 1994;66:3814–3822. doi: 10.1021/ac00093a043. [DOI] [PubMed] [Google Scholar]
- 27.Yang J, Hage DS. Characterization of the binding and chiral separation of D- and L-tryptophan on a high-performance immobilized human serum albumin column. J Chromatogr. 1993;645:241–250. doi: 10.1016/0021-9673(93)83383-4. [DOI] [PubMed] [Google Scholar]
- 28.Conrad ML, Moser AC, Hage DS. Evaluation of indole-based probes for high-throughput screening of drug binding to human serum albumin: Analysis by high-performance affinity chromatography. J Sep Sci. 2009;32:1145–1155. doi: 10.1002/jssc.200800567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Powers AC. Diabetes mellitus. In: Kasper DL, Fauci AS, Longo DL, Braunwald E, Hauser SL, Jameson JL, editors. Harrison's principles of internal medicine. Chap 323 McGraw-Hill; 2005. [Google Scholar]
- 30.Joseph KS, Hage DS. Characterization of the binding of sulfonylurea drugs to HSA by high-performance affinity chromatography. J Chromatogr B. 2010;878:1590–1598. doi: 10.1016/j.jchromb.2010.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]