Abstract
Objective
To examine the association between four aspects of the perceived neighborhood environment (aesthetics, walkability, safety, and social cohesion) and health status outcomes in a cohort of North Carolinians with self-report arthritis, after adjustment for individual and neighborhood SES covariates.
Methods
696 participants self-reported one or more types of arthritis or rheumatic condition in a telephone survey. Outcomes measured were physical and mental functioning (MOS SF-12v2 PCS and MCS); functional disability (HAQ); depressive symptomatology (CES-D scored <16; ≥16). Multivariate regression and multivariate logistic regression analyses were conducted using STATA v11.
Results
Results from separate adjusted models indicate that measures of associations for perceived neighborhood characteristics are statistically significant (p≤0.001 to p=0.017) for each health status outcome (except walkability and MCS) after adjusting for covariates. Final adjusted models included all four perceived neighborhood characteristics simultaneously. A one point increase in perceiving worse neighborhood aesthetics predicted lower mental health (B= −1.81, p=0.034). Individuals had increased odds of depressive symptoms if they perceived lower neighborhood safety (OR: 1.36; CI: 1.04, 1.78, p=0.023) and if they perceived lower neighborhood social cohesion (OR 1.42; CI: 1.03, 1.96, p=0.030).
Conclusions
Study findings indicate that an individual’s perception of neighborhood environment characteristics, especially aesthetics, safety and social cohesion, is predictive of health outcomes among adults with self-report arthritis, even after adjusting for key variables. Future studies interested in examining the role that community characteristics play on disability and mental health in individuals with arthritis might consider further examination of perceived neighborhood.
Gender and race, as well as individual-level socioeconomic status (SES) markers such as education, income and occupation are differentially associated with arthritis (i.e. incidence, disease severity, access to care and health outcomes) (1;2). In efforts to go beyond these individual-level determinants of health and contributors to health disparities, greater attention is now being given to understanding the influence of the neighborhood (or community) environment on health status outcomes and individual health behaviors. Area of residence can be particularly important given the uneven spatial distribution of goods, services, educational facilities, and resources through natural (e.g., geographic landmarks like lakes and mountains) and man-made clustering of individuals (e.g., political, economic or self-imposed segregation). Typically, there are three ways that researchers examine the effect of neighborhood on health: 1) through the use of administrative data (e.g., U.S. Census data), 2) through the use of trained raters who systematically observe and characterize the physical and/or social attributes of neighborhoods; and 3) through the use of self-reported perception of neighborhood conditions (3;4).
While the independent effect of neighborhood socioeconomic status on outcomes like mortality, chronic disease, mental health, and health behaviors has been established in numerous studies of the general population {Kawachi, 2003 17103/id; Morland, 2002 11866/id}, as well as of older adults (7), the relationship between neighborhood SES and arthritis outcomes has only recently been established (8–12). Several studies conducted in the United Kingdom and the United States have examined the relationship of community SES and health outcomes in individuals with rheumatoid arthritis (8), inflammatory polyarthritis (9), systemic lupus erythematosus (SLE) (10), as well as prevalence and health-related quality of life in self-report arthritis (11;12), using aggregate measures like the Carstairs score, Townsend score, Index of Multiple Deprivation and US Census variables as indirect, ‘objective’ proxy for neighborhood characteristics. All have found that living in areas of greater deprivation is related to poorer arthritis-related outcomes (e.g., physical functioning, functional disability, depressive symptoms).
In addition to these objective measures of the neighborhood environment, attention has been given to the significance of perceived neighborhood characteristics. Perceptions can be grounded in observable conditions (13) or there can be incongruities between perceived neighborhood environment and objective reality (14;15). It has been theorized that neighborhood perceptions are important to examine because they can elicit psychosocial or psychological processes (13;16–18), or even a physiological stress response that can affect mental and physical health (19;20).
Current research aimed at better understanding which neighborhood attributes influence health are grounded in the practical and theoretical knowledge generated from decades of social science and public health research (5). Constructs borne out of psychology and sociology, such as social disorder and social cohesion, as well as public health infrastructure features like presence of sidewalks, have been developed as ways to more objectively measure neighborhood characteristics. Typically researchers identify constructs or neighborhood features of relevance to general (e.g., self-rated health) or specific health outcomes (e.g., cardiovascular or asthma outcomes) depending on their research question (3;5;21).
In studies conducted with the general population, perceptions of both physical (e.g., quality, facilities, problems, walkability) and social (e.g., social cohesion, social control) aspects of neighborhood environment have been linked to self-rated health (22–24), physical functioning (25) and mental health outcomes (26–30), as well as health behaviors like smoking, drinking and walking for exercise (29). Among older adults, better self-rated health has been associated with perceiving higher quality of area facilities and neighborliness (31) and physical environment (16). Mobility disability has also been associated with lower perceived neighborhood safety among lower-income, retirement age adults (13).
Neighborhood perceptions have also been shown to influence specific disease outcomes. Mujahid et al found that individuals who self-reported better neighborhood characteristics (e.g., walkability, availability of healthy foods, safety, and social cohesion) were less likely to be hypertensive, even after adjustment for individual-level characteristics of age, gender and SES (education and income) (32). Greater perceptions of neighborhood problems (e.g., traffic, noise, trash, smells, and fires) have been associated with lower quality of life, worse physical functioning and greater depressive symptoms among individuals with asthma, cross-sectionally (21) and prospectively (33). Greater perceptions of neighborhood problems were also associated with smoking and high blood pressure among adults with diabetes (34). To date, no one has examined the role of perceived neighborhood environment on the health outcomes of adults with arthritis. The purpose of this paper is to examine the association between four aspects of the perceived neighborhood environment (aesthetics, walkability, safety, and social cohesion) and self-report health status outcomes in a cohort of North Carolinians with self-report arthritis after adjustment for individual and objective neighborhood SES.
Participants and Methods
Study Design
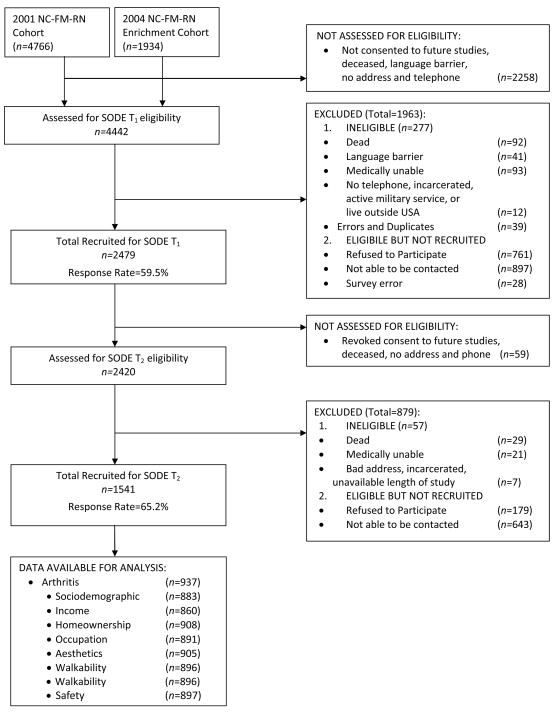
The North Carolina Family Medicine Research Network (NC-FM-RN) was established in 2001 as an ongoing practice-based research network of family medicine practices that were purposively sampled to represent the geographic (urban and rural) and ethnic diversity of North Carolina. This network cohort consists of individuals who visited a participating practice, are 18 years and older, gave consent to participate in the research study and completed a survey about demographics, health conditions and health habits (35). It is frequently enriched with new participants (2004, 2005, 2008) and is used as a source population for a variety of additional research studies. Figure 1 illustrates the flow of participant’s originating from the NC-FM-RN into the current study.
Figure 1.
Participant Recruitment and Participation
In 2006, participants who had agreed to be contacted (N=2420) were mailed a letter inviting them to participate in a follow-up telephone survey for the Individual and Community Social Determinants of Arthritis Outcomes Study. Individuals were eligible to participate in this study if they were 18 years or older, spoke English fluently, and had current contact information (address and telephone number). There was a 65.2% participation rate (N=1541). This follow-up telephone survey assessed demographics, health status, chronic health conditions, health attitudes and beliefs, health behaviors, and perceptions of neighborhood environment, and provides the data for this current study.
Arthritis status was determined using the 2003 arthritis module of the Behavioral Risk Factor Surveillance System (BRFSS) definition of self-reported doctor diagnosis of arthritis. Participants were classified as self-reporting arthritis if they reported any type of doctor diagnosed arthritis, including osteoarthritis, rheumatoid arthritis, or fibromyalgia; all measures were self-reported and questions were closed-ended. Previous research has indicated that this measure is highly reliable in general populations for providing arthritis prevalence estimates, particularly in older populations (36;37). In this study, a total of 937 participants self-reported one or more types of arthritis or rheumatic condition: osteoarthritis (n=484), fibromyalgia (n=118), rheumatoid arthritis (n=219), bursitis or tendonitis (n=439), carpal tunnel syndrome (n=200), gout (n=135), or other arthritis condition (n=111). These respondents are similar in race (76% white vs. 76%) and gender (73% female vs. 71%) when compared to the initial NC-FM-RN cohort in 2001. However, they are more likely to have greater levels of education in the 2006 survey (56% some college or more vs 50%). Finally, after adjustment for age in 2001, this sample is older (24% aged 65+ vs. 18%); this is to be expected as it is reflective of those who visit family practices, as well as an arthritis-only sample. All study materials and methods were approved by the University of North Carolina Biomedical Institutional Review Board.
Health Status Outcomes
Health status outcomes were assessed using the following four established measures:
Physical and mental health functioning
The Medical Outcomes Study’s 12-item Short Form Survey Instrument (SF-12v2) two summary scores, the SF-12v2 Physical Component (PCS), and the SF-12v2 Mental Component (MCS), were used to assess physical and mental health functioning. The SF-12v2 is strongly correlated with the SF-36 and is reliable in general populations (38). In this study, it has high internal consistency (Chronbach’s α =0.90). PCS and MCS scores range from 0 to 100, with higher scores indicating better health; both PCS and MCS were used as continuous variables in this study.
Health Assessment Questionnaire
Self-reported function was assessed using the disability scale of the Health Assessment Questionnaire (HAQ) (39), which includes questions about 20 activities of daily living organized by 8 domains (dressing, arising, eating, walking, hygiene, activities, reach, and grip); scores are adjusted based on the use of assistive devices. Each domain is separately scored, with the total score averaged over the eight domains. Each item is scored from 0 (no disability) to 3 (maximum disability), therefore a higher score represents greater disability.
Depressive Symptoms
The Center for Epidemiologic Studies Depression (CES-D) Scale measures symptoms associated with depression in the general population (40) and is a 20-item, self-report scale yielding scores ranging from 0–60, with higher scores indicating greater levels of depressive symptoms. While a score of 16 or greater has been determined to be a clinically relevant marker of depressive symptoms (41), past research examining depression in cohorts drawn from primary care settings have found low prevalence of depression, suggesting greater sensitivity and specificity to detect depression with the CES-D may come from cutpoints above 16 (42). In this current study, we estimate the prevalence of depression and anxiety from a single self-report question to be 33% (N=1541) and 37% in the sample of arthritis only individuals (N=937). Given this high prevalence of self-report of depression and anxiety, CES-D scores were dichotomized at cutpoint of 16 (< 16 or ≥16) in this study. This scale had high internal consistency in this study (Chronbach’s α = 0.92).
Main Predictors: Perceived Neighborhood Characteristics
During the telephone survey, participants were asked to think about the area of within one mile from their home and report on four perceived neighborhood characteristics: aesthetic environment (7 items), walking/exercise environment (11 items), safety (3 items), and social cohesion (5 items) using a 5-point Likert-response format, with response categories ranging from 1 (strongly agree) to 5 (strongly disagree). Reverse coding was conducted for certain items to standardize the direction of all items. For each scale, responses were summed for each item, and averaged to create an overall scale score that ranged from 1 to 5. For example, a score of 1 would indicate better perception of neighborhood aesthetics and a score of 5 would indicate worse perception of aesthetics. Aesthetic environment, walking environment and safety scales were developed by Echeverria, Diez-Roux and Link (2004) (3) specifically to examine cardiovascular health outcomes; the social cohesion and trust scale was developed by Sampson, Raudenbush and Earls (1997) (43). For clarity and simplicity, these perceived neighborhood characteristics will be referred to as aesthetics, walkability, safety and social cohesion, respectively. We chose these four perceived neighborhood scales because all have previously been determined to be reliable in a sample of participants with cardiovascular disease (3) and we believed these domains may influence physical and mental health outcomes in this sample of participants with arthritis. Items within each neighborhood dimension had good internal consistency in this study (Chronbach’s α: aesthetics= 0.80; walking=0.79; safety=0.78; social cohesion=0.81). See the appendix for each scale, related items, and those items reverse scored.
Appendix.
Perceived Physical and Social Neighborhood Environment Items*.
Aesthetic Environment
|
Walking/exercise environment
|
Safety from crime
|
| Social cohesion |
Response categories were: strongly agree, agree, do not agree or disagree, disagree, strongly disagree
Reverse-coded
Covariates
In this study, covariates included participant socio-demographics (age, race, and gender), health characteristics (body mass index (BMI), and number of comorbid conditions), individual SES measures (education, household income, occupation, and home ownership), and neighborhood SES (block group poverty rate).
Age was calculated using the participant’s self-reported date of birth and date of telephone survey and used as a continuous measure. Race was self-reported and based on the 2000 US Census race and ethnicity categories and trichotomized into non-Hispanic white, non-Hispanic Black, and Other, where Other includes individuals self-reporting Latino/Hispanic ethnicity or more than one race (American Indian/Alaska Native; Asian; Black or African American; Native Hawaiian or Other Pacific Islander; White; Other). BMI (kg/m2) was calculated from self-reported height and weight, and used as a continuous measure. Existing comorbid conditions were assessed by asking participants if a health professional ever told them they had any of 21 different chronic diseases (e.g. diabetes, heart disease, vision problems). For this paper, number of comorbid conditions is a sum of all self-reported conditions excluding back pain, osteoporosis, psoriasis, high blood pressure, high cholesterol, and depression/anxiety. These conditions were excluded either for their association with arthritis and the health outcomes of interest, or because they tend to be asymptomatic.
Because of the close association between individual SES and neighborhood SES, a number of individual-level SES measures were included in the models as covariates. Education was assessed with 7 categories and later dichotomized as a high school education or less and education beyond high school. Household income was queried using a stepped approach, with participants answering “Is your annual family income above or below $45,000”; this dichotomy is retained for this study. Occupation was queried as open text, coded using the 2000 US Census occupation classification categories, and further refined into ‘professional’ (e.g., management, technical, sales and office) and ‘non-professional’ (e.g., farming, fishing, service, construction, production, and labor) categories for use in this study. Home ownership (yes, no) was assessed by asking participants “Do you own your own home?”
Finally, an objective neighborhood SES indicator was assessed. Each participant’s household was geocoded and linked to a US Census 2000 block group, with each participant assigned a block group poverty rate (percentage of households with income below the poverty line). This variable was used as a continuous variable, with higher rates indicating greater neighborhood poverty.
Statistical Analysis
Because these perceived neighborhood scales were created for use among the general population, we conducted factor analysis on the scale items, fitting a four-factor solution with an oblique rotation (assuming correlation between the items) from all participants (n=1541). The scales perform similarly among those with and without self-report arthritis, indicating no difference by arthritis status in the way that individuals interpret and respond to the perceived neighborhood questions. Statistical analyses were conducted on 696 participants who self-reported arthritis (after excluding missing cases on covariates and the main perceived neighborhood environment predictors) using STATA 11.0 (StataCorp, College Station, TX). Univariate analyses were conducted, as well as correlation and bivariate analyses to examine unadjusted and adjusted associations between socio-economic variables, perceived neighborhood characteristics and health status outcomes. Separate multivariate linear regressions were used for physical functioning and mental health, and multivariate logistic regression analysis was used for depressive symptoms. For each health status outcome, separate regression models were conducted to examine perceived physical environment (aesthetics and walkability) and perceived social environment (safety and social cohesion), and adjusted for age, gender, BMI, number of comorbid conditions, race, education, homeownership, occupation, income, and block group poverty rate. Finally, for each health status outcome, a full model included all four perceived neighborhood characteristics as main predictors and adjusted for age, gender, BMI, number of comorbid conditions, race, education, homeownership, occupation, income, and block group poverty rate.
Results
The 696 participants with arthritis were on average 60 years old and had a mean BMI of 30. They tended to be female (73%), white (77%), with median income $45,000 (51% above), educated (66% some college or higher), and worked in occupations considered ‘professional’ (59%) (Table 1). Participants had mean scores of 38.74 and 51.44 for physical functioning and mental health status, respectively, and generally reported low disability (mean score 0.67). The majority of participants, 70%, self-reported depressive symptoms scores of less than 16 (Table 1).
Table 1.
Participant Sociodemographic Characteristics, Neighborhood Characteristics, and Outcomes* (N=696)
| Sociodemographic Characteristics | |
| Age, mean ± SD years; range | 60.41 ± 12.69; 23–94 |
| BMI, mean ± SD kg/m2; range | 29.9 ± 6.8; 15–64 |
| Co-morbid condition count, mean ± condition; range | 3 ± 2; 0–11 |
| Income | |
| <$45,000 Income | 51 |
| Race | |
| non-Hispanic White | 77 |
| non-Hispanic Black | 16 |
| Other | 7 |
| Gender | |
| Women | 73 |
| Education | |
| HS education or less | 44 |
| Homeowner | |
| Yes | 84 |
| Occupation | |
| Professional | 59 |
| Perceived Neighborhood Characteristics | |
| Aesthetics (1–5), mean ± SD; range | 2.23 ± 0.69; 1–5 |
| Walkability (1–5), mean ± SD; range | 2.70 ± 0.67; 1–5 |
| Safety (1–5), mean ± SD; range | 2.26 ± 0.86; 1–5 |
| Social Cohesion (1–5), mean ± SD; range | 2.27 ± 0.72; 1–5 |
| Objective Neighborhood | |
| Block group poverty level, mean ± SD; range | 12.55 ± 8.72; 0–51.37 |
| Health Status Outcomes† | |
| Physical functioning, mean ± SD; range SF12v2 PCS (0–100) | 38.74 ±12.86; 5.68 – 61.57 |
| Mental health, mean ± SD; range SF12v2 MCS (0–100) | 51.44 ±11.08; 8.99 – 75.24 |
| Disability, mean ± SD; range HAQ (0–3) | 0.67 ± 0.64; 0 – 3 |
| Depressive Symptoms, mean ± SD | |
| CES-D | |
| Score <16 | 70 |
| Score ≥16 | 30 |
Values are the percentage unless otherwise indicated, BMI=body mass index
Note N varies for outcomes: PCS & MCS, N=689; HAQ, N=696; CES-D Depressive Symptoms, N=669
Preliminary analyses examined for potential effect modification of race and gender for the four perceived neighborhood characteristic variables on each outcome. No interaction terms were significant at p<0.01 after adjusting the criterion level using a Bonferroni correction for multiple tests, and all likelihood ratio tests were statistically insignificant. Correlation analyses (not shown) indicate the perceived neighborhood scales are moderately correlated with one another (ranging from 0.4 to 0.6; p<0.001), indicating a shared variance. Low correlation (ranging from 0.2–0.3; p<0.001) was also observed for the relationship between each perceived neighborhood characteristic and health status outcome. Bivariate analyses revealed that lower individual-level income, less education, non homeownership, non-professional occupations were significantly associated with worse perception of neighborhood aesthetics, walkability, safety, and social cohesion (with the exception of perceived walkability and homeownership, p=0.547). Examination of block group poverty as an objective measure of community SES shows a modest correlation between aesthetics (0.18, p<0.001), walkability (0.07, p=0.055), safety (0.17, p<0.001) and social cohesion (0.12, p=0.001) (Table 2).
Table 2.
Bivariate Analysis of Individual and Community Level Socioeconomic Status and Perceived Neighborhood Characteristicsa Scores
| Aesthetics | Walkability | Safety | Social Cohesion | |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |
|
Individual SES Measuresb | ||||
| Income | ||||
| ≥$45000 | 2.04 (0.65) | 2.56 (0.66) | 2.04 (0.78) | 2.11 (0.65) |
| <$45000 | 2.40 (0.68) | 2.83 (0.63) | 2.49(0.88) | 2.43 (0.74) |
| p-value | <0.001 | <0.001 | <0.001 | <0.001 |
| Education | ||||
| Beyond HS | 2.13 (0.74) | 2.65 (0.72) | 2.20 (0.88) | 2.23 (0.75) |
| HS or less | 2.37 (0.60) | 2.78 (0.57) | 2.38 (0.84) | 2.36 (0.68) |
| p-value | <0.001 | 0.008 | 0.010 | 0.011 |
| Occupation | ||||
| Professional | 2.12(0.70) | 2.65 (0. 71) | 2.20 (0.84) | 2.19 (0.70) |
| Non-professional | 2.40 (0.64) | 2.79 (0.58) | 2.39(0.89) | 2.42 (0.73) |
| p-value | <0.001 | 0.006 | 0.005 | <0.001 |
| Homeowner | ||||
| Yes | 2.19 (0.70) | 2.70 (0.67) | 2.25 (0.88) | 2.24 (0.72) |
| No | 2.42 (0.64) | 2.74 (0.62) | 2.46(0.79 | 2.52 (0.70) |
| p-value | 0.002 | 0.547 | 0.015 | <0.001 |
| Community SES Measurec | ||||
| Block group poverty | 0.18 | 0.07 | 0.17 | 0.12 |
| p-value | <0.001 | 0.055 | <0.001 | 0.001 |
Higher values of neighborhood characteristic indicates worse perception;
t-test;
correlation
The neighborhood perceptions are measured on a scale of 1–5 with increasing numerical value implying worsening perceptions. In the following presentation of the regression results, all allusions to worse or lower perception will refer to a 1 unit increase in the perception scale. Regression analyses examining the bivariate relationship (not shown) between each perceived neighborhood characteristic and each health status outcome revealed strong relationships; unadjusted models indicate that each perceived neighborhood characteristic is statistically significant (p<0.001) for each health status outcome. These relationships remain, though slightly attenuated (p≤0.001 to p=0.017), in separate models adjusting for age, gender, BMI, number of comorbid conditions, race, and individual and neighborhood SES covariates (Table 3). A one unit increase (worsening) of neighborhood aesthetics, walkability or social cohesion results in a nearly 2 point decline in physical functioning, and a one unit increase of neighborhood aesthetics, safety or social cohesion also results in an average decline of 2 points on mental health functioning. Disability scores were higher for those perceiving worse neighborhood characteristics. A one unit increase in perceived neighborhood aesthetics results in odds 1.79 times higher of reporting greater depressive symptoms (CI: 1.34, 2.38, p<0.001). A one unit increase in perceived neighborhood walkability (OR 1.59, CI: 1.19, 2.12, p=0.002), safety (OR 1.68, CI: 1.35, 2.10, p<0.001) or social cohesion (OR 1.84, CI: 1.42, 2.40, p<0.001) also increased the odds of-reporting greater depressive symptoms.
Table 3.
Adjusted parameter estimates (B), standard error (SE), and Odds Ratio (OR) [95% CI], for Perceived Neighborhood Physical Environment and Social Environment and Health Status Outcome.
| Model | Physical Functioning | Disability | Mental Health | Depressive Symptoms |
|---|---|---|---|---|
| (n=689) | (n=696) | (N=689) | (n=669) | |
| B (SE) | B (SE) | B (SE) | OR [95% CI] | |
| 1. Aesthetics | −2.43 (0.63)*** | 0.15 (0.3)*** | −2.54 (0.61)*** | 1.79[1.34, 2.38]*** |
| 2. Walkability | −2.41 (0.65)*** | 0.12 (0.03)*** | −1.22 (0.63)† | 1.59 [1.19, 2.12]** |
| 3. Safety | −1.19 (0.50)* | 0.09 (0.03)*** | −1.88 (0.48)*** | 1.68 [1.35, 2.10]*** |
| 4. Social Cohesion | −1.92 (0.59)** | 0.13 (0.03)*** | −2.32 (0.57)*** | 1.84 [1.42, 2.40]*** |
Note: Models adjust for age, gender, BMI, number of comorbid conditions, race, education, homeownership, occupation, income, and block group poverty.
p<0.10;
p<0.05;
p≤0.01;
p≤0.001
Multivariate regression and multivariate logistic regression analyses examining the association between all four perceived neighborhood characteristics and health status outcomes are reported in Table 4. No statistically significant association existed between perceived neighborhood characteristics and physical functioning, after adjusting for individual-level covariates and objective neighborhood SES. Perceiving worse neighborhood aesthetics and lower social cohesion was associated with a trend for greater disability. Individuals perceiving worse neighborhood aesthetics scored nearly 2 points lower on mental health even after adjusting for covariates (B= −1.81, p=0.034). A trend for scoring 1.25 points lower on mental health was observed for individuals reporting lower perceived neighborhood social cohesion (B= −1.25, p=0.077). Individuals had 1.36 greater odds of reporting depressive symptoms if they perceived lower neighborhood safety (CI: 1.04, 1.78, p=0.023) and 1.42 times greater odds of reporting depressive symptoms if they perceived lower neighborhood social cohesion (CI: 1.03, 1.96, p=0.030). A trend was observed for individuals perceiving worse neighborhood aesthetics and lower neighborhood social cohesion to score nearly a tenth point higher on the disability scale (B=0.09, p=0.052; B=0.06, p=0.084; respectively). Considering statistically significant covariates in general, poorer outcomes were related to being older, having a higher BMI, greater number of comorbid conditions, less education and income.
Table 4.
Perceived Neighborhood Environment, SES variables, and Health Status Outcomes, Beta (SE) and OR [95% CI]
| Physical Functioning | Disability | Mental Health | Depressive Symptoms | |
|---|---|---|---|---|
| (n=689) | (n=696) | (N=689) | (n=669) | |
| B (SE) | B (SE) | B (SE) | OR (95% CI) | |
| Aesthetics | −1.25 (0.89) | 0.09 (0.04)† | −1.81 (0.85)* | 1.20 [0.81, 1.77] |
| Walkability | −1.29 (0.83) | 0.02 (0.04) | 1.04 (0.80) | 1.03 [0.71, 1.49] |
| Safety | 0.11 (0.61) | 0.03 (0.03) | −0.95 (0.59) | 1.36 [1.04, 1.78]* |
| Social Cohesion | −1.29 (0.73) | 0.06 (0.04)† | −1.25 (0.71)† | 1.42 [1.03, 1.96]* |
| High School or Below | 2.76 (0.95)** | −0.07 (0.05) | 0.97 (0.91) | 0.57 [0.38, 0.89]** |
| Homeowner | 0.031 (1.18) | −0.04 (0.06) | −0.93 (1.13) | 1.05 [0.65, 1.73] |
| Professional Occupation | 1.15 (0.99) | −0.05 (0.05) | 0.78 (0.95) | 0.75 [0.49, 1.16] |
| <$45,000 household income | −2.66 (1.02)** | 0.17(0.05)*** | −2.77 (0.98)** | 2.26 [1.42, 3.59]*** |
| Block group poverty level | 0.04 (0.05) | −0.002 (0.01) | 0.06 (0.05) | 1.00 [0.98, 1.02] |
Note: Models adjust for age, gender, race, BMI, and number of comorbid conditions
p<0.10;
p<0.05;
p<0.01;
p≤0.001
Discussion
Our study revealed that different perceived neighborhood characteristics emerged as significant factors for physical and mental health outcomes in this sample of individuals with arthritis. While nearly all perceived neighborhood characteristics were statistically significant predictors in separate models, these relationships do not remain in the full model with all four perceived neighborhood characteristics and reflect the shared variance among the four perceived neighborhood characteristics to predict health outcomes. Perceiving worse neighborhood aesthetics was independently associated with scoring nearly two points lower on mental health, as well as indicating a trend for having a higher disability score (B=0.09, p=0.052). Individuals who perceived lower neighborhood safety and social cohesion had increased odds of reporting depressive symptoms by 1.36 and 1.42, respectively. There was also a trend for those who perceive worse neighborhood social cohesion to have a lower mental health score (B= −1.25, p=0.077) and a higher disability score (B=0.06, p=0.084). Finally, analyses (not shown) examining the CES-D at a cutpoint of 23 (<23; ≥23) revealed that both the strength and significance of perceived neighborhood safety and perceived social cohesion are attenuated to OR=1.31, p=0.080 and OR=1.41, p=0.062 respectively, indicating a continued trend that neighborhood perceptions may play an important role in major clinical depression beyond individual-level characteristics.
While there is no clear pattern of one or more perceived neighborhood characteristics definitively emerging as predictive of the physical and mental health outcomes examined in this study, perceived aesthetics, safety, and social cohesion do emerge as neighborhood characteristics worthy of additional attention in future studies conducted in an arthritis population. Though findings from studies examining perceived neighborhood environment problems and mental health outcomes have been mixed (7), our study findings are in line with several studies (44–46), including a recent study by Mair et al (30). They found that perception of poor aesthetics, greater violence, and lower social cohesion was associated with greater depressive symptoms (measured with CES-D) in cross-sectional analyses of a large population-based cohort study of healthy adults aged 45–84 (30). These findings, combined with our own in an arthritis-only population, suggest that perceived neighborhood aesthetics, safety, and social cohesion do play a role in health outcomes – particularly mental health, even when controlling for individual-level and neighborhood-level SES variables.
This paper is unique in examining and confirming that these associations exist among individuals with arthritis residing in largely rural areas of North Carolina, a population in which these instruments have not previously been used. Prior studies have generally examined perceived neighborhood environment in more urban areas such as London, United Kingdom (25), Adelaide, Australia (47), and Baltimore, MD; New York, NY; St. Paul, MN; Forsyth County, NC; and Cook County, Illinois (2nd most populous county in USA after LA county) (32). Additionally, previous research indicates that that individual-level socioeconomic status plays a significant role in physical and mental health outcomes among individuals with arthritis, with low income and low education placing individuals at greater risk for poorer health outcomes. Given that neighborhood perceptions (aesthetics, safety, and social cohesion) continue to play a significant role in health outcomes, above and beyond individual-level (e.g., higher income and education) and neighborhood-level socioeconomic status, we conclude that the role of perceived neighborhood environment is an important predictor of physical and mental health. Findings from this research suggest that future researchers consider the importance of the perceived neighborhood environment (aesthetics, safety, and social cohesion) when examining the influence of place on health, particularly mental health, in individuals with arthritis.
Several limitations should be noted, however. This study is cross-sectional and therefore we cannot assert a causal relationship between perceived neighborhood environment and health status outcomes. Additionally, we do not have data on length of residence. Knowledge of how long participants have lived in their particular home and neighborhood would have allowed for adjustment of potential confounders, such as the effect of having established social connections within the neighborhood or being witness to neighborhood environment change over time (e.g., from either good to bad, or bad to good).
Previous research has warned of same-source bias when examining the relationship between individual perceptions and individual health outcomes, indicating that other characteristics may influence one’s perception (3). Because our study aimed to examine whether individual perception of neighborhood environment influenced health outcomes for individuals with arthritis, we obtained both perceived neighborhood characteristics and health status outcomes from the same group of individuals. We cannot adjust for the possibility that those with lower mental health at the time of survey have biased neighborhood perceptions given the cross-sectional nature of our study, though we were able to adjust for physical health (count of comorbid conditions), a theorized cofounder. Additionally, the 937 participants who self-reported arthritis represent 480 block groups (63 individuals not assigned a block group; 293 individuals who are the sole representative for their block group). The remaining 581 participants represent 187 block groups, and the intraclass (or intraneighborhood) correlation coefficient (ICC) reveals very little agreement in the scale scores between block group for each perceived neighborhood: aesthetics 0.079; walkability 0.180; safety 0.089; social cohesion <0.001). We believe that the low ICC is a function of nearly 94% block groups containing fewer than 5 individuals (range 2–12).
In conclusion, our study findings indicate that perceived neighborhood environment, especially characteristics of aesthetics, safety and social cohesion, is predictive of health outcomes in this sample of adults with self-report arthritis, even after adjusting for key variables. Strong feelings of connections and cohesion between neighbors may increase feelings of safety and security in their neighborhood environment, in turn positively influencing mental health. Conversely the lack of positive social interactions and poor perceptions of the neighborhood environment may operate in such a way as to negatively influence mental health. Future studies interested in examining the role that community characteristics play on disability and mental health in individuals with arthritis might consider further examination of perceived neighborhood with constructs of social capital, particularly social cohesion and safety. Additional evidence from prospective studies with community-dwelling adults, especially those from non-urban areas, is needed to shed light on the causal relationship between perceived neighborhood environment and health outcomes.
Acknowledgments
National Institute of Arthritis and Musculoskeletal and Skin Disease Multidisciplinary Clinical Research Center Rheumatic Diseases: P60-AR49465
This project was supported by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases Multidisciplinary Clinical Research Center, Rheumatic Diseases: P60-AR49465-01 and manuscript preparation was supported by the Thurston Arthritis Research Center Training Grant 5T32-AR007416.
We thank the following participating family practices in the North Carolina Family Medicine Research Network (NC-FM-RN) for their assistance: Black River Health Services, Burgaw; Bladen Medical Associates, Elizabethtown; Blair Family Medicine, Wallace; Cabarrus Family Medicine, Concord; Cabarrus Family Medicine, Harrisburg; Cabarrus Family Medicine, Kannapolis; Cabarrus Family Medicine, Mt. Pleasant; Chatham Primary Care, Siler City; CMC-Biddle Point, Charlotte; CMC-North Park, Charlotte; Community Family Practice, Asheville; Cornerstone Medical Center, Burlington; Dayspring Family Medicine, Eden; Family Practice of Summerfield, Summerfield; Goldsboro Family Physicians, Goldsboro; Henderson Family Health Center, Henderson; Orange Family Medical Group, Hillsborough; Person Family Medical Center, Roxboro; Pittsboro Family Medicine, Pittsboro; Prospect Hill Community Health Center, Prospect Hill; Robbins Family Practice, Robbins; and Village Family Medicine, Chapel Hill. Finally, we thank the individuals who willingly participated in the study.
Reference List
- 1.Centers for Disease Control and Prevention (CDC) Racial/ethnic differences in the prevalence and impact of doctor-diagnosed arthritis--United States, 2002. MMWR Morb Mortal Wkly Rep. 2005;54(5):119–23. [PubMed] [Google Scholar]
- 2.Jordan JM, Lawrence R, Kington R, Fraser P, Karlson E, Lorig K, et al. Ethnic health disparities in arthritis and musculoskeletal diseases: report of a scientific conference. Arthritis Rheum. 2002;46(9):2280–6. doi: 10.1002/art.10480. [DOI] [PubMed] [Google Scholar]
- 3.Echeverria SE, Diez-Roux AV, Link BG. Reliability of self-reported neighborhood characteristics. J Urban Health. 2004;81(4):682–701. doi: 10.1093/jurban/jth151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mujahid MS, Diez Roux AV, Morenoff JD, Raghunathan T. Assessing the Measurement Properties of Neighborhood Scales: From Psychometrics to Ecometrics. Am J Epidemiol. 2007;165(8):858–67. doi: 10.1093/aje/kwm040. [DOI] [PubMed] [Google Scholar]
- 5.Kawachi I, Berkman LF. Neighborhoods and Health. New York: Oxford University Press; 2003. [Google Scholar]
- 6.Morland K, Wing S, Diez-Roux A. The contextual effect of the local food environment on residents’ diets: the atherosclerosis risk in communities study. Am J Public Health. 2002;92(11):1761–7. doi: 10.2105/ajph.92.11.1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yen IH, Michael YL, Perdue L. Neighborhood environment in studies of health of older adults: a systematic review. Am J Prev Med. 2009;37(5):455–63. doi: 10.1016/j.amepre.2009.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harrison MJ, Tricker KJ, Davies L, Hassell A, Dawes P, Scott DL, et al. The relationship between social deprivation, disease outcome measures, and response to treatment in patients with stable, long-standing rheumatoid arthritis. J Rheumatol. 2005;32(12):2330–6. [PubMed] [Google Scholar]
- 9.Harrison MJ, Farragher TM, Clarke AM, Manning SC, Bunn DK, Symmons DP. Association of functional outcome with both personal- and area-level socioeconomic inequalities in patients with inflammatory polyarthritis. Arthritis Rheum. 2009;61(10):1297–304. doi: 10.1002/art.24830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Trupin L, Tonner MC, Yazdany J, Julian LJ, Criswell LA, Katz PP, et al. The role of neighborhood and individual socioeconomic status in outcomes of systemic lupus erythematosus. J Rheumatol. 2008;35(9):1782–8. [PMC free article] [PubMed] [Google Scholar]
- 11.Callahan LF, Shreffler J, Mielenz T, Schoster B, Kaufman JS, Xiao C, et al. Arthritis in the Family Practice Setting: Associations with Education and Community Poverty. Arthritis Care Res. 2008;59(7):1002–8. doi: 10.1002/art.23834. [DOI] [PubMed] [Google Scholar]
- 12.Callahan LF, Shreffler J, Mielenz T, Kaufman J, Schoster B, Randolph R, et al. Health-Related Quality of Life in Adults from 17 Family Practice Clinics in North Carolina. Preventing Chronic Disease. 2009;6(1) http://www.cdc.gov/pcd/issues/2009/jan/07_0215.htm. [PMC free article] [PubMed]
- 13.Clark CR, Kawachi I, Ryan L, Ertel K, Fay ME, Berkman LF. Perceived neighborhood safety and incident mobility disability among elders: the hazards of poverty. BMC Public Health. 2009;9:162. doi: 10.1186/1471-2458-9-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Troped PJ, Saunders RP, Pate RR, Reininger B, Ureda JR, Thompson SJ. Associations between self-reported and objective physical environmental factors and use of a community rail-trail. Prev Med. 2001;32(2):191–200. doi: 10.1006/pmed.2000.0788. [DOI] [PubMed] [Google Scholar]
- 15.Kirtland KA, Porter DE, Addy CL, Neet MJ, Williams JE, Sharpe PA, et al. Environmental measures of physical activity supports: perception versus reality. Am J Prev Med. 2003;24(4):323–31. doi: 10.1016/s0749-3797(03)00021-7. [DOI] [PubMed] [Google Scholar]
- 16.Wen M, Hawkley LC, Cacioppo JT. Objective and perceived neighborhood environment, individual SES and psychosocial factors, and self-rated health: an analysis of older adults in Cook County, Illinois. Soc Sci Med. 2006;63(10):2575–90. doi: 10.1016/j.socscimed.2006.06.025. [DOI] [PubMed] [Google Scholar]
- 17.Bowling A, Stafford M. How do objective and subjective assessments of neighbourhood influence social and physical functioning in older age? Findings from a British survey of ageing. Soc Sci Med. 2007;64(12):2533–49. doi: 10.1016/j.socscimed.2007.03.009. [DOI] [PubMed] [Google Scholar]
- 18.Wilson K, Elliott S, Law M, Eyles J, Jerrett M, Keller-Olaman S. Linking perceptions of neighbourhood to health in Hamilton, Canada. J Epidemiol Community Health. 2004;58(3):192–8. doi: 10.1136/jech.2003.014308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Diez Roux AV. Investigating Neighborhood and Area Effects on Health. Am J Public Health. 2001;91(11):1783–9. doi: 10.2105/ajph.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Miller DB, Townsend A. Urban hassles as chronic stressors and adolescent mental health: The Urban Hassles Index. Brief Treatment and Crisis Intervention. 2005;5(1):85. [Google Scholar]
- 21.Yen IH, Yelin EH, Katz P, Eisner MD, Blanc PD. Perceived neighborhood problems and quality of life, physical functioning, and depressive symptoms among adults with asthma. Am J Public Health. 2006;96(5):873–9. doi: 10.2105/AJPH.2004.059253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Collins PA, Hayes MV, Oliver LN. Neighbourhood quality and self-rated health: a survey of eight suburban neighbourhoods in the Vancouver Census Metropolitan Area. Health Place. 2009;15(1):156–64. doi: 10.1016/j.healthplace.2008.03.008. [DOI] [PubMed] [Google Scholar]
- 23.Weden MM, Carpiano RM, Robert SA. Subjective and objective neighborhood characteristics and adult health. Soc Sci Med. 2008;66(6):1256–70. doi: 10.1016/j.socscimed.2007.11.041. [DOI] [PubMed] [Google Scholar]
- 24.Rohrer J, Pierce JR, Jr, Denison A. Walkability and self-rated health in primary care patients. BMC Fam Pract. 2004;5:29. doi: 10.1186/1471-2296-5-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Feldman PJ, Steptoe A. How neighborhoods and physical functioning are related: the roles of neighborhood socioeconomic status, perceived neighborhood strain, and individual health risk factors. Ann Behav Med. 2004;27(2):91–9. doi: 10.1207/s15324796abm2702_3. [DOI] [PubMed] [Google Scholar]
- 26.Kim D. Blues from the neighborhood? Neighborhood characteristics and depression. Epidemiol Rev. 2008;30:101–17. doi: 10.1093/epirev/mxn009. [DOI] [PubMed] [Google Scholar]
- 27.Schaefer-McDaniel N. Neighborhood stressors, perceived neighborhood quality, and child mental health in New York City. Health Place. 2009;15(1):148–55. doi: 10.1016/j.healthplace.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 28.Latkin CA, Curry AD. Stressful neighborhoods and depression: a prospective study of the impact of neighborhood disorder. J Health Soc Behav. 2003;44(1):34–44. [PubMed] [Google Scholar]
- 29.Echeverria S, Diez-Roux AV, Shea S, Borrell LN, Jackson S. Associations of neighborhood problems and neighborhood social cohesion with mental health and health behaviors: the Multi-Ethnic Study of Atherosclerosis. Health Place. 2008;14(4):853–65. doi: 10.1016/j.healthplace.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 30.Mair C, Diez Roux AV, Shen M, Shea S, Seeman T, Echeverria S, et al. Cross-sectional and longitudinal associations of neighborhood cohesion and stressors with depressive symptoms in the multiethnic study of atherosclerosis. Ann Epidemiol. 2009;19(1):49–57. doi: 10.1016/j.annepidem.2008.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bowling A, Barber J, Morris R, Ebrahim S. Do perceptions of neighbourhood environment influence health? Baseline findings from a British survey of aging. J Epidemiol Community Health. 2006;60(6):476–83. doi: 10.1136/jech.2005.039032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mujahid MS, ez Roux AV, Morenoff JD, Raghunathan TE, Cooper RS, Ni H, et al. Neighborhood characteristics and hypertension. Epidemiology. 2008;19(4):590–8. doi: 10.1097/EDE.0b013e3181772cb2. [DOI] [PubMed] [Google Scholar]
- 33.Yen IH, Yelin E, Katz P, Eisner MD, Blanc PD. Impact of perceived neighborhood problems on change in asthma-related health outcomes between baseline and follow-up. Health Place. 2008;14(3):468–77. doi: 10.1016/j.healthplace.2007.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gary TL, Safford MM, Gerzoff RB, Ettner SL, Karter AJ, Beckles GL, et al. Perception of neighborhood problems, health behaviors, and diabetes outcomes among adults with diabetes in managed care: the Translating Research Into Action for Diabetes (TRIAD) study. Diabetes Care. 2008;31(2):273–8. doi: 10.2337/dc07-1111. [DOI] [PubMed] [Google Scholar]
- 35.Sloane PD, Callahan L, Kahwati L, Mitchell CM. Development of a Practice-based Patient Cohort for Primary Care Research. Fam Med. 2006;38(1):50–7. [PubMed] [Google Scholar]
- 36.Sacks JJ, Harrold LR, Helmick CG, Gurwitz JH, Emani S, Yood RA. Validation of a surveillance case definition for arthritis. J Rheumatol. 2005;32(2):340–7. [PubMed] [Google Scholar]
- 37.Bombard JM, Powell KE, Martin LM, Helmick CG, Wilson WH. Validity and reliability of self-reported arthritis: Georgia senior centers, 2000–2001. Am J Prev Med. 2005;28(3):251–8. doi: 10.1016/j.amepre.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 38.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 39.Fries JF, Spitz PW, Young DY. The dimensions of health outcomes: the health assessment questionnaire, disability and pain scales. J Rheumatol. 1982;9(5):789–93. [PubMed] [Google Scholar]
- 40.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 41.Boyd JH, Weissman MM, Thompson WD, Myers JK. Screening for depression in a community sample. Understanding the discrepancies between depression symptom and diagnostic scales. Arch Gen Psychiatry. 1982;39(10):1195–200. doi: 10.1001/archpsyc.1982.04290100059010. [DOI] [PubMed] [Google Scholar]
- 42.McDowell I. Measuring health: a guide to rating scales and questionnaires. 3. Oxford University Press; USA: 2006. [Google Scholar]
- 43.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and Violent Crime: A Multilevel Study of Collective Efficacy. Science. 1997;277(5328):918–24. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 44.Ziersch AM, Baum FE, Macdougall C, Putland C. Neighbourhood life and social capital: the implications for health. Soc Sci Med. 2005;60(1):71–86. doi: 10.1016/j.socscimed.2004.04.027. [DOI] [PubMed] [Google Scholar]
- 45.Mair C, Diez Roux AV, Galea S. Are neighbourhood characteristics associated with depressive symptoms? A review of evidence. J Epidemiol Community Health. 2008;62(11):940–6. 8. doi: 10.1136/jech.2007.066605. [DOI] [PubMed] [Google Scholar]
- 46.Leslie E, Cerin E. Are perceptions of the local environment related to neighbourhood satisfaction and mental health in adults? Prev Med. 2008;47(3):273–8. doi: 10.1016/j.ypmed.2008.01.014. [DOI] [PubMed] [Google Scholar]
- 47.Baum FE, Ziersch AM, Zhang G, Osborne K. Do perceived neighbourhood cohesion and safety contribute to neighbourhood differences in health? Health and Place. 2009;15(4):925–34. doi: 10.1016/j.healthplace.2009.02.013. [DOI] [PubMed] [Google Scholar]