Abstract
Background
Psychological well-being is associated with mortality/survival. Although cardiorespiratory fitness (CRF) is one of the strongest predictors of mortality, studies examining the relationship between well-being and survival seldom account for the possible effects of CRF.
Purpose
This study examined the independent associations of psychological well-being components (low level of negative emotion and high level of positive emotion) and CRF, as well as their combined effects, with survival.
Methods
Participants (N=4888) were examined in 1988–1997 and followed up for a median period of ~15 years (212 deaths, 4.3%). CRF was assessed by a maximal exercise test on a treadmill. Low-level negative emotion was defined as the minimum score of the negative emotion subscale of the CES-D scale, and high-level positive emotion as the maximum score of positive emotion subscale. Results are presented as hazard ratios (95% CIs). Data were analyzed in 2009.
Results
After adjustment for a set of established risk factors, men and women with low levels of negative emotion had lower risk of death than those with higher levels of negative emotion, 0.66 (0.50, 0.87). The association persisted after additional adjustment for CRF and positive emotion. High level of positive emotion was not associated with survival. A high level of CRF independently predicted lower risk of death, 0.54 (0.37, 0.79), compared to a low level of CRF. The risk of death in participants with both a low level of negative emotion and a high level of CRF was 0.37 (0.22, 0.63), compared to their peers with higher levels of negative emotion/low levels of CRF.
Conclusions
Low levels of negative emotion and high levels of CRF are independent predictors of long-term survival in men and women. A strong combined effect was observed, as individuals with both a low level of negative emotion and a high level of CRF had a 63% lower risk of death than those with higher levels of negative emotion and a low level of CRF.
INTRODUCTION
Positive health, as opposed to mere absence of physical illness, has long been ignored scientifically.1 One component of positive health is psychological well-being, which can be defined as a composite of relatively low levels of negative emotion, relatively high levels of positive emotion, and life satisfaction. Psychological studies examining mortality mainly focus on the negative spectrum of the psychological status (e.g., depression, anxiety, distress, and its association with mortality/survival). Recently, an increasing number of studies have focused on positive psychological well-being, supporting that it has a favorable effect on survival in both healthy and diseased populations.2
It has been suggested that a high level of cardiorespiratory fitness (CRF) is associated with better psychological well-being.3 In addition, CRF is one of the strongest predictors of all-cause mortality in healthy and unhealthy men and women,4–8 and should therefore be considered when studying mortality. It is possible that CRF interacts with emotion in the prediction of mortality, such that CRF buffers the adverse effects of negative emotion or enhances positive emotion. The prospective studies analyzing the associations between positive well-being and mortality have been recently reviewed using meta-analytic methods,2 however no studies took into account CRF. The Aerobics Center Longitudinal Study (ACLS) provides an opportunity to comprehensively study both positive psychological well-being and objectively measured CRF in relation to all-cause mortality in a cohort of U.S. men and women, taking into account a complete set of relevant confounders.
Positive and negative emotion are usually independent or weakly correlated, and it is unknown which of them is a stronger predictor of survival, after taking into account a set of established risk factors, including CRF. The current study aimed to examine the independent associations of well-being components (low level of negative emotion and high level of positive emotion) and CRF, as well as their combined effects, with survival.
METHODS
Study Cohort
The ACLS is a prospective epidemiologic investigation of men and women.4, 7, 9 ACLS participants were mostly Caucasian (98%), well-educated, and worked in executive or professional positions.10 All participants completed a detailed questionnaire (including a self-report physical activity measure) and underwent an extensive clinical evaluation, including a physical examination, fasting blood chemistry analyses, personal and family health history, anthropometry, smoking and alcohol use, and a maximal exercise treadmill test. All participants gave written informed consent, and the study protocol was approved annually by the IRB of the Cooper Institute.
A total of 5030 ACLS participants were examined and responded to a mail-back survey from 1988 to 1997. Participants were included in the study if they had complete and valid data for all the main exposures (CRF, positive and negative emotion) and confounders studied: gender, age, smoking, alcohol consumption, BMI, self-reported physical activity, healthy/unhealthy index. The participants not achieving 85% or more of the individual’s age-predicted maximal heart rate during the graded modified Balke treadmill exercise testing were excluded because their test was not considered maximal (n=140). In addition, those participants were excluded who died within 1 year of follow-up (n=2), because a low psychological well-being status might be due to rapidly deteriorating health and be entirely secondary to the disease process. After these exclusions, the final analytic data included 4888 men and women, aged 20–81 years at the time of their clinical examination, and were followed up from the date of the baseline examination until the date of death or 31 December 2003. Mortality surveillance was based on the National Death Index. Participants meeting all the inclusion criteria were younger, heavier, taller, and had higher BMI and CRF level (P<0.05) than those not meeting the criteria.
Baseline Examination
Previous reports have described the baseline examination in detail.4 Briefly, height and weight were measured on a standard scale and stadiometer at the baseline clinic visit. BMI was calculated as weight in kilograms divided by height in meters squared (kg/m2). Cardiorespiratory fitness was defined as the total time of a symptom-limited maximal treadmill exercise test, using a modified Balke protocol.4, 11 Total time of the test on this protocol correlates highly with measured maximal oxygen uptake (VO2max) in both men (r = 0.92) 12 and women (r = 0.94).13 The test endpoint was volitional exhaustion or when the physician stopped it for medical reasons. VO2max was calculated from the final treadmill speed and grade.14 Gender- and age-specific CRF tertiles were computed and used in the analyses. The lower, middle and upper tertiles are hereinafter referred to as low, moderate and high CRF, respectively.
Information on leisure time physical activity (physically inactive or active), smoking (never, ex-smoker, and current smoker), alcohol consumption (≥5 drinks/week or <5 drinks/week), and the presence of any major chronic disease was obtained from a standardized medical history questionnaire. Participants were defined as physically inactive if they reported no leisure-time physical activity in the 3 months before the baseline examination. An unhealthy index (ranging from 0 to 6) was defined as the presence of one or more of the following disease/pathologic conditions: cardiovascular disease, cancer, hypertension, diabetes, respiratory symptoms, or abnormal electrocardiogram at rest or exercise. For certain analyses, this index was dichotomized as the presence or absence of any of the mentioned diseases.
Psychological Well-Being Assessment
The psychological well-being components were ascertained by means of the 20-item version of the Center for Epidemiologic Studies depression (CES-D) scale, included as part of the mail-back survey. The aggregate survey response during the study period in the ACLS is ~65%. Nonresponse bias is a concern in epidemiologic surveillance, and has been investigated in the ACLS. No major source of bias was found.15 Baseline health histories and clinical measures were similar between responders and nonresponders and between early and late responders.
The CES-D scale consists of four subscales, two of which were used in this study. The negative and positive emotion subscales were used to assess negative emotion and positive emotion, respectively. The questions asked about how often the person experienced certain feelings during the previous week. The negative affect subscale included the following 7 items: not able to shake off the blues, depressed, my life had been a failure, fearful, lonely, crying spells and sad. The positive affect subscale included the following 4 items: feeling as good as other people, hopeful, happy, and joy. Response options ranged from 0 to 3, where 0 indicated <1 day, 1 indicated 1–2 days, 2 indicated 3–4 days, and 3 indicated 5–7 days. A negative emotion score was calculated by summing the 7 negative items, with the score ranging from 0 to 21. The same procedure was followed to calculate a positive emotion score (sum of 4 items), ranging from 0 to 12. A person was considered to have low levels of negative emotion if he/she answered 0 to all the negative items (i.e., sum sre=0, called minimum score), and was considered to have high levels of positive emotion if he/she answered 3 to all the positive items (i.e., sum score=12, called maximum score). The four-item positive emotion CES-D subscale has been widely used as a valid measure of positive emotion.16, 17 Factor analyses showed that responses to these four questions are highly correlated with one another and therefore can be treated as additive measures of a single positive emotion score.16, 17 An examination was made of the internal consistency of the negative and positive subscales and the results showed an acceptable consistency among the items composing each subscale, (i.e., Cronbach’s alpha coefficients were 0.80 and 0.70 for the negative and positive subscales, respectively).
Statistical Analysis
Basic descriptive statistics included means and frequencies of key study variables by gender and for the total study population. Cox proportional hazards regression was used to estimate hazard ratios (HRs), 95% CIs, and age-adjusted mortality rates (deaths per 10,000 person-years of follow-up), according to exposure categories.
No significant interaction with gender was found; therefore analyses were performed for all the participants together and gender was included as a covariate in all the models. First, univariate associations of the main exposures (CRF, low-level negative emotion and high-level positive emotion) and confounders were conducted with all-cause mortality, after adjusting for age and gender. Next, a number of multivariate analyses were conducted. Model 1 adjusted for BMI, physical activity, smoking and alcohol consumption. Model 2 additionally adjusted for the healthy/unhealthy index, as mortality can be highly influenced by major chronic diseases. Model 3 adjusted for the other main exposures, in an effort to test whether their association with mortality was independent of the other. Since a significant interaction (P=0.001) was found between CRF and negative emotion in relation to mortality, two more analyses were performed. First, the association between negative emotion and mortality was studied stratifying by levels of CRF. Second, CRF and negative emotion variables were combined to test a possible additive effect on mortality. Survival curves were generated according to categories of the exposures. Two-sided P values were calculated; those <0.05 were considered significant. Analyses were done in 2009 using SPSS statistical software, version 17.0 (SPSS Inc, Chicago).
RESULTS
Over a median follow-up period of 14.8 years (25th and 75th percentiles= 13.6 and 15.4), 212 deaths occurred (4.3%). Baseline characteristics of the participants are shown in Table 1. Forty-one percent of the men and 34% of the women had both low levels of negative emotion and high levels of positive emotion (data not shown). The distribution of the psychological well-being variables was positively skewed for negative emotion and negatively skewed for positive emotion, indicating a healthy mental status for a majority of participants.
Table 1.
Baseline characteristics of the participants.
| Men (n=3901) | Women (n=987) | All (n=4888) | |
|---|---|---|---|
| Age (years) | 49.1 (10.5) | 47.0 (10.8) | 48.7 (10.6) |
| Weight (kg) | 82.3 (12.2) | 61.4 (10.5) | 78.1 (14.6) |
| Height (cm) | 178.5 (6.9) | 164.3 (6.5) | 175.7 (8.9) |
| BMI | 25.8 (3.6) | 22.8 (3.7) | 25.2 (3.8) |
| BMI categories | |||
| < 25 | 1823 (46.7) | 797 (80.7) | 2620 (53.6) |
| 25.0 to 29.9 | 1666 (42.7) | 133 (13.5) | 1799 (36.8) |
| ≥30 | 412 (10.6) | 57 (5.8) | 469 (9.6) |
| VO2max (ml/kg/min) | 44.1 (8.9) | 35.5 (7.9) | 42.4 (9.4) |
| Treadmill time (min) | 19.9 (5.0) | 14.8 (4.8) | 18.8 (5.4) |
| Cardiorespiratory fitness levels | |||
| Low (lower tertile) | 1352 (34.7) | 330 (33.4) | 1682 (34.4) |
| Moderate (middle tertile) | 1266 (32.5) | 330 (33.4) | 1596 (32.7) |
| High (upper tertile) | 1283 (32.9) | 327 (33.1) | 1610 (32.9) |
| Negative emotion | |||
| Any other score | 1384 (35.5) | 473 (47.9) | 1857 (38.0) |
| Minimum score | 2517 (64.5) | 514 (52.1) | 3031 (62.0) |
| Positive emotion | |||
| Any other score | 1925 (49.3) | 504 (51.1) | 2429 (49.7) |
| Maximum score | 1976 (50.7) | 483 (48.9) | 2459 (50.3) |
| Leisure time physical activity | |||
| Inactive | 788 (20.2) | 266 (27.0) | 1054 (21.6) |
| Active | 3113 (79.8) | 721 (73.0) | 3834 (78.4) |
| Smoking | |||
| Never | 2094 (53.7) | 647 (65.6) | 2741 (56.1) |
| Ex-smoker | 1471 (37.7) | 292 (29.6) | 1763 (36.1) |
| Current smoker | 336 (8.6) | 48 (4.9) | 384 (7.9) |
| Alcohol consumption | |||
| <5 drinks/week | 3306 (84.7) | 970 (98.3) | 4276 (87.5) |
| ≥5 drinks/week | 595 (15.3) | 17 (1.7) | 612 (12.5) |
| Dichotomy unhealthy index * | |||
| Absence | 2551 (65.4) | 653 (66.2) | 3204 (65.5) |
| Presence | 1350 (34.6) | 334 (33.8) | 1684 (34.5) |
Data are shown as M(SD) for continuous variables, and as frequency (percentage) for nominal variables. VO2max, maximal oxygen uptake.
The dichotomy unhealthy index was defined as the presence of one or more of the following pathologic conditions: cardiovascular disease, cancer, hypertension, diabetes, respiratory symptoms and abnormal electrocardiogram at rest or exercise.
Association of CRF and Psychological Well-Being with Survival
Univariate associations (HR and 95% CI) of CRF, psychological well-being components (negative and positive emotion) and other potential predictors of all-cause mortality, after adjusting for age and gender, are shown in Table 2.
Table 2.
Univariate association of cardiorespiratory fitness, negative emotion, positive emotion and other factors with all-cause mortality, after adjusting for age and gender.
| Predisposing factors | No. of deaths (n) | Age and gender-adjusted HR (95% CI) |
|---|---|---|
| Cardiorespiratory fitness | ||
| Low | 100 (1682) | 1 (ref) |
| Moderate | 65 (1596) | 0.71 (0.52, 0.97) |
| High | 47 (1610) | 0.52 (0.36, 0.73) |
| Negative emotion | ||
| Any other score | 83 (1857) | 1 (ref) |
| Minimum score | 129 (3031) | 0.64 (0.48, 0.84) |
| Positive emotion | ||
| Any other score | 101 (2429) | 1 (ref) |
| Maximum score | 111 (2459) | 0.88 (0.66, 1.16) |
| Weight status: BMI groups | ||
| < 25 | 100 (2620) | 1 (ref) |
| 25.0 to 29.9 | 85 (1799) | 1.22 (0.91, 1.64) |
| ≥ 30 | 27 (469) | 2.02 (1.31, 3.11) |
| Leisure time physical activity | ||
| Inactive | 38 (1054) | 1 (ref) |
| Active | 174 (3834) | 0.92 (0.65, 1.31) |
| Smoking | ||
| Never | 95 (2741) | 1 (ref) |
| Ex-smoker | 101 (1763) | 1.28 (0.96, 1.69) |
| Current smoker | 16 (384) | 1.43 (0.84, 2.44) |
| Alcohol consumption | ||
| <5 drinks/week | 191 (4276) | 1 (ref) |
| ≥5 drinks/week | 21 (612) | 0.95 (0.60, 1.50) |
| Dichotomy unhealthy index * | ||
| Absence | 100 (3204) | 1 (ref) |
| Presence | 112 (1684) | 1.83 (1.40, 2.40) |
HR, hazard ratio;
Presence of one or more of the pathologic conditions indicated in Table 1
The mortality rates (deaths per 10 000 person-years of follow-up) according to negative emotion categories were calculated stratifying by age (i.e., aged <60 years and aged ≥60 years). The mortality rates did not differ by age group. Mortality rates among those aged <60 years and those aged ≥60 years were 1.5 (20.8/14.2) and 1.5 (143.5/94.9) times greater, respectively, for individuals having low-level negative emotion compared to those with higher levels.
Multivariate associations (HR and 95% CI) of CRF and positive psychological well-being components with all-cause mortality are shown in Table 3. After adjustment for demographic factors (gender and age), BMI, and lifestyle factors such as physical activity, smoking and alcohol consumption (Model 1), participants with high CRF had a lower risk of death compared with low-CRF individuals, 0.54 (0.37 to 0.79). Individuals having low levels of negative emotion had a lower risk of death than those having higher levels of negative emotion, 0.66 (0.50 to 0.87). No association was observed for positive emotion. After additional adjustment for the presence/absence of major pathologic conditions (Model 2), the results were unchanged. When CRF was additionally adjusted for negative emotion and vice versa, the effect on mortality was slightly reduced, but still significant (Model 3). Adjustment for the other main exposures did not affect the results.
Table 3.
Multivariate associations of cardiorespiratory fitness and positive psychological well-being components with all-cause mortality in men and women, after adjustment for demographic factors, lifestyle-related factors, presence of pathologic conditions and main exposures.
| Exposures | Model 1* HR (95% CI) | Model 2† HR (95% CI) | Model 3‡ HR (95% CI) |
|---|---|---|---|
| Cardiorespiratory fitness | |||
| Low | 1 (ref) | 1 (ref) | 1 (ref) |
| Moderate | 0.74 (0.53, 1.02) | 0.77 (0.56, 1.07) | 0.79 (0.57, 1.09) |
| High | 0.54 (0.37, 0.79) | 0.59 (0.40, 0.88) | 0.60 (0.41, 0.89) |
| Negative emotion | |||
| Any other score | 1 (ref) | 1 (ref) | 1 (ref) |
| Minimum score | 0.66 (0.50, 0.87) | 0.69 (0.52, 0.91) | 0.70 (0.53, 0.94) |
| Positive emotion | |||
| Any other score | 1 (ref) | 1 (ref) | 1 (ref) |
| Maximum score | 0.92 (0.70, 1.21) | 0.93 (0.71, 1.22) | 0.94 (0.72, 1.23) |
HR, hazard ratio
Model 1 adjusted for age, gender, BMI, physical activity, smoking (never, ex-smoker, current smoker) and alcohol consumption (≥ 5 drinks/week or <5 drinks/week).
Model 2 adjusted for all the variables in model 1 plus an unhealthy index (i.e., a summary score created from the following pathologic conditions: cardiovascular disease, cancer, hypertension, diabetes, respiratory symptoms and abnormal electrocardiogram at rest or exercise).
Model 3 adjusted for all the variables in model 2 plus psychological well-being indices (negative and positive emotion) for cardiorespiratory fitness, and cardiorespiratory fitness for negative emotion. Adjustment for other main exposures did not affect the results.
Negative Emotion × CRF interactions and combined effects
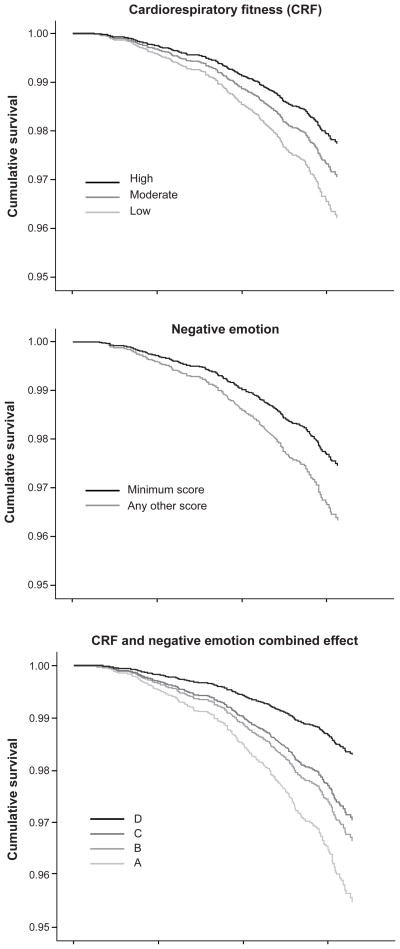
Because an interaction between negative emotion and CRF was found (P=0.001), stratified analyses were performed. Low-level negative emotion was associated with a lower risk of mortality in participants with high CRF (HR=0.51; 95% CI=0.28 to 0.91), whereas this association was not significant in moderate- or low-CRF participants (data not shown). The combined effect of having both high CRF and low levels of negative emotion on mortality was also analyzed (Table 4). The HR of mortality was 0.37 (CI=0.22 to 0.63) in the high-CRF/low-level negative emotion participants (named category “D”), compared with the opposite group (i.e., low CRF/higher levels of negative emotion [named category “A”]). Figure 1 shows survival curves according to levels of CRF, negative emotion and a combination of them, after adjusting for all the variables indicated in Model 2, Table 3.
Table 4.
Combined effect of high cardiorespiratory fitness and low level of negative emotion with mortality in men and women, after adjustment for demographic factors, lifestyle-related factors and presence of pathologic conditions.
| Cardiorespiratory Fitness coding * | Negative emotion Coding † | Combined score ‡ | HR ** (95% CI) | |||
|---|---|---|---|---|---|---|
| 0 | + | 0 | = | 0 | A | 1 (ref) |
| 0 | + | 1 | = | 1 | B | 0.74 (0.50, 1.08) |
| 1 | + | 0 | = | 1 | ||
| 1 | + | 1 | = | 2 | C | 0.65 (0.43, 0.98) |
| 2 | + | 0 | = | 2 | ||
| 2 | + | 1 | = | 3 | D | 0.37 (0.22, 0.63) |
HR, hazard ratio
0, 1 and 2 indicate low, moderate and high levels of cardiorespiratory fitness, respectively.
0 and 1 indicate any other score and minimum score, respectively, in the negative emotion subscale.
The codes 0, 1, 2 and 3, resulting from the sum of the variables cardiorespiratory fitness and negative emotion, were named A, B, C and D, respectively. D is the “best” possible combination between the two exposures (i.e., high level of fitness and low level of negative emotion) and A is the “worst” possible combination (i.e., low level of fitness and higher level of negative emotion).
Model adjusted for all the covariates indicated in Model 2, Table 3.
Figure 1.
Survival curves according to levels of cardiorespiratory fitness, negative emotion and a combination of them, after adjusting for all the variables indicated in Model 2 (Table 3). See A, B, C and D categories’ definitions in Table 4.
CRF, cardiorespiratory fitness
Additional Analyses (data not shown)
All the analyses were run for each single item included in the negative and positive emotion subscales. After adjustment for the confounders, low levels (minimum score) of “lonely feeling” were significantly associated with lower mortality, (0.67; 0.47 to 0.94), compared to higher levels (any other score). No association was found between single positive emotion items and mortality.
When the individuals having major diseases (i.e., CVD and cancer) were excluded from the analyses, the results did not change.
Partial correlations were run adjusted for gender and age, and found rather weak but significant correlations of CRF with positive (r=0.07; P<0.001) and negative (r= −0.05; P<0.001) emotion. Even weaker correlations were found between physical activity and positive (r=0.03; P=0.02) or negative (r= −0.02; P=0.19) emotion.
DISCUSSION
Our results suggest that low-level negative emotion and high CRF are independently associated with survival, after adjustment for important confounders such as age, BMI, physical activity, smoking and alcohol consumption. Accounting for the presence/absence of any major disease/pathologic condition did not affect these findings. To the best of our knowledge this is the first study accounting for the potential effect of CRF in the relationship of positive and negative emotions, as well as their combined effect, with mortality risk. The inclusion of this important predictor of mortality,8 as well as a complete set of other established risk factors strengthens the findings reported in this study.
The interaction analysis suggests that the effect of low-level negative emotion on survival does not persist in participants with low or moderate CRF levels. Finally, an additive effect was observed on survival in those individuals with high levels of CRF and low levels of negative emotion. Compared with the low-CRF/higher level of negative emotion group, individuals with high levels of CRF and low-level negative emotion had a 63% lower risk for all-cause mortality, after controlling for a set of established risk factors, which is considered a large effect. This finding suggest that simultaneous improvements of fitness and avoidance of negative emotion might have a substantial impact on long-term survival. However, additional research is needed to confirm or contrast these findings.
The current data do not allow identification of the causal mechanisms of the association between low-level negative emotion and survival, yet several physiologic pathways can be considered. Low-level negative emotion could alter people’s disease susceptibility by increasing the immune system activity and consequently decreasing the susceptibility to infectious diseases and cancer. This effect can be mediated by the activity of the hypothalamic–adreno–cortical axis leading to lower cortisol levels, preventing insulin resistance, overweight and high blood pressure, among other consequences.18–21 Likewise, it could enhance a variety of capacities, like the ability to concentrate and problem solve or to mobilize social or other resources.18
We examined whether psychological well-being was more strongly associated with survival in older individuals (≥60y), compared with younger individuals(<60y), as has been suggested elsewhere.2 The current results did not show any difference in the associations of low-level negative emotion with survival among younger and older individuals. This finding suggests that interventions that focus on psychological well-being enhancement in younger and older people might be equally successful.
In the current study, additional adjustments for the presence of major diseases did not change the results, suggesting that the main effects observed for the exposures do not substantially differ between healthy and unhealthy people. Because of the small number of people in the current study with chronic disease, it was not possible to run analyses separately for healthy and diseased subgroups. Nevertheless, it was found that after excluding those individuals with major mortality-related diseases from the analysis, the main effect of low-level negative emotion on survival remained rather stable. This suggests that the effect of low-level negative emotion on survival might be independent of the presence or absence of major diseases. It was also hypothesized that lifestyle could explain, at least partially, the observed association between low-level negative emotion and survival. However, the relationship between low-level negative emotion and survival remained significant and was minimally affected when controlling for a set of potentially relevant lifestyle confounders.
Low-level negative emotion was associated with survival independently of positive emotion levels in this study. As expected, there was a modest correlation between positive and negative emotion scores (Spearman’s correlation coefficient = −0.39). This indicates that people reporting high levels of positive emotion do not necessarily have low levels of negative emotion, and vice versa. In this context, Kubzansky et al. reached similar conclusions after comparing optimism and pessimism.22 Positive and negative emotion should therefore be considered as distinctive psychological dimensions that can affect behaviors, physical health indices, and survival in unique ways.
Another major finding of this study is that high levels of positive emotion did not predict survival in the men and women studied. Half of the published studies (48.6%) conducted on healthy people concurred with the results from the present study, while the other half showed a protective effect of measures of positive psychological health on survival.2
Our study must be considered in light of several potential limitations. Fewer women than men were included in this study; however, a formal test was done on the interaction term between gender and main exposures in the models and no significant interaction was observed. This suggests that the associations between the main exposures and survival may not vary between men and women, as previously reported.23 It is possible that there is residual confounding or that some unmeasured variables (e.g., genetic factors) could account for both low-level negative emotion and reduced all-cause mortality risk. Although an established set of risk factors was controlled for, it is possible that other factors such as dietary intake are also relevant. Unfortunately, such data are not available. The current study provides only a single assessment of negative and positive emotion; however, previous research has suggested that measures of psychological well-being attributes are quite stable across years and even decades, regardless of changes in life circumstances.24 Likewise, the CES-D subscales used in this study have shown a high level of stability over time.25 The ACLS participants were mostly Caucasian, well-educated, and from middle to high socioeconomic strata,10 thereby future studies should be conducted in other populations with varying background, ethnicity, or SES. Finally, the distribution of the emotion variables showed that most of the participants were mentally healthy. More heterogeneous study samples might find greater effect sizes in positive psychological health components in relation to survival.
The strengths of the current study include its prospective design with events (deaths) quantified via the National Death Index, which has shown to be an accurate method of ascertaining deaths in observational studies, with high sensitivity (96%) and specificity (100%).26 This study also had a long follow-up (average follow-up period of 15 years) in a relatively large sample of U.S. men and women, with complete and valid data for all the variables included in the study.
Conclusion
The data analyzed indicate that low levels of negative emotion and high levels of CRF are independent predictors of long-term survival in men and women followed up for 15 years, regardless of other established risk factors of mortality. However, no association was found between positive emotion and survival. A strong combined effect was observed, where individuals with both low-level negative emotion and high CRF had a 63% lower risk of death compared to those with higher negative emotion and low CRF.
Findings from this study suggest that it may be beneficial for health professionals to assess their patient’s psychological health levels (i.e., emotion) in addition to performing a physical examination. In addition to encouraging increased levels of physical activity for patients with low CRF, health professionals may also be able to intervene so that improvements in negative emotion (i.e., decrease levels of low negative emotion) can be realized. Improvements in both may lead to the largest reductions in mortality risk.
Acknowledgments
We thank the Cooper Clinic physicians and technicians for collecting the baseline data, and staff at the Cooper Institute for data entry and data management.
This study was supported by NIH grants AG06945 and HL62508, and in part by an unrestricted research grant from The Coca-Cola Company. The study also was supported in part by Robert Wood Johnson Foundation’s Pioneer Portfolio (grant number 63597), the Spanish Ministry of Education (EX-2008-0641, EX-2007-1124), the Swedish Council for Working Life and Social Research, and the Swedish Heart–Lung Foundation (20090635). The funding sources had no role in the collection, analysis, and interpretation of the data or in the decision to submit the manuscript for publication.
Footnotes
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Seligman MEP. Positive Health. Appl Psychol. 2008;57:3–18. [Google Scholar]
- 2.Chida Y, Steptoe A. Positive psychological well-being and mortality: a quantitative review of prospective observational studies. Psychosom Med. 2008;70(7):741–56. doi: 10.1097/PSY.0b013e31818105ba. [DOI] [PubMed] [Google Scholar]
- 3.Galper DI, Trivedi MH, Barlow CE, Dunn AL, Kampert JB. Inverse association between physical inactivity and mental health in men and women. Med Sci Sports Exerc. 2006;38(1):173–8. doi: 10.1249/01.mss.0000180883.32116.28. [DOI] [PubMed] [Google Scholar]
- 4.Blair SN, Kohl HW, 3rd, Paffenbarger RS, Jr, Clark DG, Cooper KH, Gibbons LW. Physical fitness and all-cause mortality. A prospective study of healthy men and women. JAMA. 1989;262(17):2395–401. doi: 10.1001/jama.262.17.2395. [DOI] [PubMed] [Google Scholar]
- 5.Blair SN, Kohl HW, 3rd, Barlow CE, Paffenbarger RS, Jr, Gibbons LW, Macera CA. Changes in physical fitness and all-cause mortality. A prospective study of healthy and unhealthy men. JAMA. 1995;273(14):1093–8. [PubMed] [Google Scholar]
- 6.Erikssen G, Liestol K, Bjornholt J, Thaulow E, Sandvik L, Erikssen J. Changes in physical fitness and changes in mortality. Lancet. 1998;352(9130):759–62. doi: 10.1016/S0140-6736(98)02268-5. [DOI] [PubMed] [Google Scholar]
- 7.Sui X, LaMonte MJ, Laditka JN, et al. Cardiorespiratory fitness and adiposity as mortality predictors in older adults. JAMA. 2007;298(21):2507–16. doi: 10.1001/jama.298.21.2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kodama S, Saito K, Tanaka S, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. Jama. 2009;301(19):2024–35. doi: 10.1001/jama.2009.681. [DOI] [PubMed] [Google Scholar]
- 9.Hooker SP, Sui X, Colabianchi N, et al. Cardiorespiratory fitness as a predictor of fatal and nonfatal stroke in asymptomatic women and men. Stroke. 2008;39(11):2950–7. doi: 10.1161/STROKEAHA.107.495275. [DOI] [PubMed] [Google Scholar]
- 10.Cheng YJ, Macera CA, Addy CL, Sy FS, Wieland D, Blair SN. Effects of physical activity on exercise tests and respiratory function. Br J Sports Med. 2003;37(6):521–8. doi: 10.1136/bjsm.37.6.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Balke B, Ware RW. An experimental study of physical fitness of Air Force personnel. U S Armed Forces Med J. 1959;10(6):675–88. [PubMed] [Google Scholar]
- 12.Pollock ML, Bohannon RL, Cooper KH, et al. A comparative analysis of four protocols for maximal treadmill stress testing. Am Heart J. 1976;92(1):39–46. doi: 10.1016/s0002-8703(76)80401-2. [DOI] [PubMed] [Google Scholar]
- 13.Pollock ML, Foster C, Schmidt D, Hellman C, Linnerud AC, Ward A. Comparative analysis of physiologic responses to three different maximal graded exercise test protocols in healthy women. Am Heart J. 1982;103(3):363–73. doi: 10.1016/0002-8703(82)90275-7. [DOI] [PubMed] [Google Scholar]
- 14.American College of Sports Medicine. ACSM’s Guidelines For Exercise Testing And Prescription. 7. Philadelphia: Lippincott Williams and Wilkins; 2005. [Google Scholar]
- 15.Macera CA, Jackson KL, Davis DR, Kronenfeld JJ, Blair SN. Patterns of non-response to a mail survey. J Clin Epidemiol. 1990;43(12):1427–30. doi: 10.1016/0895-4356(90)90112-3. [DOI] [PubMed] [Google Scholar]
- 16.Fowler JH, Christakis NA. Dynamic spread of happiness in a large social network: longitudinal analysis over 20 years in the Framingham Heart Study. Bmj. 2008;337:a2338. doi: 10.1136/bmj.a2338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Joseph S, Lewis CA. Factor analysis of the Center for Epidemiological Studies Depression Scale. Psychol Rep. 1995;76(1):40–2. doi: 10.2466/pr0.1995.76.1.40. [DOI] [PubMed] [Google Scholar]
- 18.Rozanski A, Kubzansky LD. Psychologic functioning and physical health: a paradigm of flexibility. Psychosom Med. 2005;67 (Suppl 1):S47–53. doi: 10.1097/01.psy.0000164253.69550.49. [DOI] [PubMed] [Google Scholar]
- 19.Kubzansky LD. Sick at heart: the pathophysiology of negative emotions. Cleve Clin J Med. 2007;74 (Suppl 1):S67–72. doi: 10.3949/ccjm.74.suppl_1.s67. [DOI] [PubMed] [Google Scholar]
- 20.Polk DE, Cohen S, Doyle WJ, Skoner DP, Kirschbaum C. State and trait affect as predictors of salivary cortisol in healthy adults. Psychoneuroendocrinology. 2005;30(3):261–72. doi: 10.1016/j.psyneuen.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 21.Bjorntorp P. Do stress reactions cause abdominal obesity and comorbidities? Obes Rev. 2001;2(2):73–86. doi: 10.1046/j.1467-789x.2001.00027.x. [DOI] [PubMed] [Google Scholar]
- 22.Kubzansky LD, Kubzansky PE, Maselko J. Optimism and pessimism in the context of health: bipolar opposites or separate constructs? Pers Soc Psychol Bull. 2004;30(8):943–56. doi: 10.1177/0146167203262086. [DOI] [PubMed] [Google Scholar]
- 23.Kubzansky LD, Thurston RC. Emotional vitality and incident coronary heart disease: benefits of healthy psychological functioning. Arch Gen Psychiatry. 2007;64(12):1393–401. doi: 10.1001/archpsyc.64.12.1393. [DOI] [PubMed] [Google Scholar]
- 24.Charles ST, Reynolds CA, Gatz M. Age-related differences and change in positive and negative affect over 23 years. J Pers Soc Psychol. 2001;80(1):136–51. [PubMed] [Google Scholar]
- 25.Thombs BD, Hudson M, Schieir O, Taillefer SS, Baron M. Reliability and validity of the center for epidemiologic studies depression scale in patients with systemic sclerosis. Arthritis Rheum. 2008;59(3):438–43. doi: 10.1002/art.23329. [DOI] [PubMed] [Google Scholar]
- 26.Stampfer MJ, Willett WC, Speizer FE, et al. Test of the National Death Index. Am J Epidemiol. 1984;119(5):837–9. doi: 10.1093/oxfordjournals.aje.a113804. [DOI] [PubMed] [Google Scholar]