Abstract
Cross sectional/retrospective studies indicate that individuals with body dysmorphic disorder (BDD) have markedly impaired psychosocial functioning. However, no study has prospectively examined functioning in BDD. In this study, which is to our knowledge the first prospective study of the course of BDD, psychosocial functioning was assessed at baseline and over 1 to 3 years (mean = 2.7 ± 0.9 years) of follow-up with the Global Assessment of Functioning Scale (GAF), Social and Occupational Functioning Scale (SOFAS), and LIFE-RIFT (Range of Impaired Functioning Tool). Psychosocial functioning was poor during the follow-up period. Functioning remained stably poor over time on the SOFAS and LIFE-RIFT, although there was a trend for a gradual and slight improvement on the GAF over time. The cumulative probability of attaining functional remission on the GAF (score >70 for at least 2 consecutive months) during the follow-up period was only 5.7%. On the SOFAS, the cumulative probability of attaining functional remission (score >70 for at least 2 consecutive months) was 10.6%. BDD severity significantly predicted functioning on the GAF (p=.0012), SOFAS (p=.0017), and LIFE-RIFT (p=.0015). A trend for a time-by-BDD severity interaction was found on the GAF (p=.033) but not the SOFAS or LIFE-RIFT. More delusional BDD symptoms also predicted poorer functioning on all measures, although this finding was no longer significant when controlling for BDD severity. Functioning was not predicted, however, by age, gender, BDD duration, or a personality disorder. In conclusion, psychosocial functioning was poor over time, and few subjects attained functional remission. Greater BDD severity predicted poorer functioning.
Keywords: body dysmorphic disorder, dysmorphophobia, delusional disorder, functioning, prospective, somatoform disorders
Body dysmorphic disorder, a distressing or impairing preoccupation with an imagined or slight defect in one’s physical appearance (e.g., “scarred” skin or a “deformed” nose), is a relatively common disorder (Bienvenu et al., 2001; Rief et al., 2006). Descriptions of BDD during the past century have emphasized these individuals’ poor psychosocial functioning (Morselli, 1891; Phillips, 1991). However, functioning in BDD has received only limited investigation.
In an early study, 97% of 30 subjects with BDD reported a history of avoiding usual social or occupational activities because of embarrassment over their perceived appearance defects (Phillips et al., 1993). Subsequent studies which used standard functioning measures reported impairment in psychosocial functioning. In a BDD pharmacotherapy study (n=20), Schneier Disability Profile scores reflected moderate functional impairment (Hollander et al., 1999). In a study of 62 patients with BDD (85% of whom participated in a placebo-controlled pharmacotherapy study [Phillips et al., 2002]), scores on the Medical Outcomes Study 36-Item Short Form Health Survey (SF-36) (Ware, 1993) were markedly poor in all mental health domains. For example, on the SF-36 subscale that assesses role limitations due to emotional problems, BDD subjects’ scores were 1.6 standard deviation units poorer than U.S. population norms; on the social functioning subscale, their scores were 2.2 standard deviation units poorer (Phillips, 2000). Similarly poor SF-36 scores were reported in two small open-label pharmacotherapy studies (Phillips, 2006; Phillips & Najjar, 2003). Mental health-related SF-36 subscale scores in all three studies were poorer than norms for clinical depression (Ware, 1993). These studies also found impaired functioning on the Global Assessment of Functioning Scale (GAF), Social and Occupational Functioning Scale (SOFAS), and Longitudinal Interval Follow-up Evaluation (LIFE) (American Psychiatric Association, 1994; Keller et al., 1987). However, these studies are limited by relatively small sample sizes. In addition, studies which used standard functioning measures consisted entirely or largely of pharmacotherapy trial participants, which may have introduced bias.
The present study examined the following aspects of psychosocial functioning in BDD over 1 to 3 years (mean = 2.7 ± 0.9 years) of follow-up: level of psychosocial functioning, stability of functional impairment, the probability of attaining “functional remission,” and predictors of psychosocial functioning. To our knowledge, this is the first report of prospectively assessed psychosocial functioning in BDD. (We have previously reported on this sample’s cross-sectional/retrospectively assessed functioning from the intake interview [Phillips et al., 2005a].) The present study had a larger sample and broader inclusion criteria than previous studies, which may increase the generalizability of the findings. We hypothesized that (1) psychosocial functioning would be poor and remain poor over time; (2) few subjects would “functionally remit” over time; and (3) more severe BDD symptoms would predict poorer functioning over time. We were also interested in whether delusionality of BDD appearance beliefs would predict poorer functioning. In a previous cross-sectional study, delusional BDD beliefs were associated with poorer functioning/quality of life on two of three SF-36 mental health subscales (Phillips, 2000). A report from the present sample found that at the time of intake into the study, greater delusionality was significantly, although modestly, associated with poorer scores on three of seven functioning/quality of life scales/subscales (Phillips et al., 2005a). This question is of clinical interest, as it is useful for clinicians to know whether more delusional patients function more poorly over time. This question also has some relevance for DSM-V. In DSM-IV, nondelusional BDD and delusional BDD are classified separately (BDD as a somatoform disorder and delusional BDD as a psychotic disorder). However, the nature of the relationship between these BDD variants is unclear (Phillips, 2004), and data are needed on delusionality in BDD. In addition, delusionality/insight may be conceptualized as a dimension that characterizes a number of disorders (Eisen et al., 2004; Phillips, 2004), yet little is known about the relationship between delusionality and functional impairment.
METHODS
Subjects
Participants were recruited from a variety of sources into this single-site longitudinal observational study of the course of BDD. All subjects met full criteria for lifetime (i.e., current or past) DSM-IV BDD or its delusional variant. Subjects were required to be age 12 or older and able to be interviewed in person. The only exclusion criterion was the presence of a mental disorder (e.g., an organic mental disorder) that would interfere with the collection of valid interview data. Forty six percent of the subjects were referred by mental health professionals, 38.6% were obtained from advertisements, 10.2% from our program website and brochures, 3.4% from subject friends and relatives, and 1.7% from nonpsychiatrist physicians. (For a detailed description of the full sample of 200 subjects at the time of intake into the study, see Phillips et al., 2005b). The investigation was carried out in accordance with the latest version of the Declaration of Helsinki. The study was approved by the hospital Institutional Review Board, and written informed consent was obtained (assent plus parental consent for adolescents) after the procedures had been fully explained.
The current report is based on the 176 subjects who met full DSM-IV criteria for BDD during the week before the intake interview (the remaining 24 subjects had met full DSM-IV BDD criteria in the past). Of these 176 subjects, 163 (92.6%) completed a one-year follow-up interview. This report also includes all two-year and three-year interview data presently available for analysis (for 141 subjects and 78 subjects, respectively). Two-year and three-year interview data are not available for all subjects because subjects were enrolled over a period of 2.4 years and therefore currently have varying follow-up durations; for example, most subjects had not come due for their year 3 interview at the time these data were analyzed. For all 176 subjects, the mean age at intake was 32.5 ± 12.3 years (range=14–64), 71.0% (n=125) were female, and 76.1% (n=134) were single. At study intake, the mean score on the 48-point Yale-Brown Obsessive Compulsive Scale Modified for BDD [Phillips et al., 1997)], a measure of current BDD severity, was 30.4 ± 6.6.
Assessments
Subjects were interviewed at intake and re-interviewed annually following the intake interview. At each annual interview, psychosocial functioning scores were obtained for the past month and for each month during the preceding year. Interviews were conducted by experienced interviewers who were closely supervised by the first author. Interviewers received careful and rigorous training, as in similar longitudinal studies (e.g., Goisman, et al., 1994). This training includes discussing videotapes, conducting mock interviews with experienced interviewers, and being closely supervised during training sessions and initial interviews. All interviews were thoroughly edited both clinically and clerically by senior staff.
The following measures of psychosocial functioning were administered at the intake interview and annual follow-up interviews. (1) The LIFE-RIFT (Range of Impaired Functioning Tool) is a reliable and valid semi-structured measure of current functioning in the domains of work (including job, school, and household functioning), interpersonal relations, recreation, and satisfaction (Leon et al., 1999). Scores in each individual domain range from 1–5 (1 = no impairment, high level of functioning or very good functioning; 5 = severe impairment or very poor functioning). Subjects who were not working or not in school because of psychopathology were assigned a score of 5. Total LIFE-RIFT scores range from 4 to 20. (2) The DSM-IV Axis V Global Assessment of Functioning Scale (GAF) is a widely used, global measure of psychological, social, and occupational functioning (American Psychiatric Association, 1994). Scores range from 1 to 100, with 100 reflecting the highest level of functioning. (3) The Social and Occupational Functioning Scale (SOFAS) is a global measure of social and occupational functioning. Scores range from 100 (excellent functioning) to 1 (grossly impaired functioning) (American Psychiatric Association, 1994). The SOFAS was added after the study began; SOFAS data are available for 104 subjects at intake. The SOFAS was administered to all subjects at follow-up interviews. GAF, SOFAS, and LIFE-RIFT scores reflect the worst week of functioning during each month.
BDD was diagnosed with the Structured Clinical Interview for DSM-IV—Non-Patient Version (SCID-1/NP) (First et al., 1996). BDD severity during the week before each interview was assessed with the reliable and valid Yale-Brown Obsessive Compulsive Scale Modified for BDD (BDD-YBOCS) (Phillips et al., 1997). This is a 12-item scale with scores that range from 0–48; higher scores reflect greater BDD severity. The Brown Assessment of Beliefs Scale, a reliable and valid measure of delusionality that can be used in various mental disorders, assessed the delusionality of BDD beliefs (e.g., “I look deformed”) during the week before each interview (Eisen et al., 1998). Personality disorders were assessed with the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID–II) (First et al., 1997). The duration of BDD was determined with the BDD Form (Phillips et al., 1993). In this naturalistic study, treatment was not controlled. At intake and each follow-up interview, we recorded whether the subject had received medication or therapy since the last interview. In this report, we focus on receipt of a serotonin-reuptake inhibitor (SRI) or cognitive behavioral therapy (CBT) because there is empirical evidence of their efficacy for BDD (Hollander et al., 1999; Neziroglu & Khemlani-Patel, 2002; Phillips et al., 2002). Treatment data were obtained using: 1) the reliable Psychosocial Treatment Inventory (Steketee et al., 1997), which determined subjects’ perceptions of types of psychotherapy modalities (e.g., cognitive or behavioral) they received, and 2) the Longitudinal Interval Follow-Up Evaluation (LIFE), a semi-structured interview and rating system that records treatment received in longitudinal studies of mental disorders (Keller et al., 1987). Adequacy of SRI trials for BDD were defined as described elsewhere (Phillips et al., 2006b).
Data Analysis
SAS version 9.1 was used for data analysis. First, we computed means and standard deviations for the psychosocial functioning measures at the intake interview and for the 12 months preceding each annual follow-up interview. To determine the stability of psychosocial functioning over time, random effects regression analyses were conducted with annual functioning scores as the outcome variable. The cumulative probability of attaining functional remission on the GAF (score >70) and SOFAS (score >70) for at least 2 consecutive months during follow-up was determined using standard survival analysis methods. The proportion of subjects who were functionally remitted on the GAF or SOFAS (score >70) at each annual interview was also computed. Using random effects regression methods, we examined BDD severity, age, gender, BDD duration, the presence of a personality disorder, and receipt of an SRI or CBT during follow-up as independent predictors of functioning on the GAF, SOFAS, and LIFE-RIFT. These analyses controlled for the other variables as well as baseline score on the psychosocial functioning measure being examined. We first examined delusionality as a predictor of functioning separately because of our interest in this particular variable and because delusionality was fairly highly correlated with BDD severity (r=.44, p<.0001 at intake). We then additionally examined delusionality as a predictor of functioning while controlling for BDD severity. Predictor variables consisted of annual BDD severity and delusionality scores, SRI or CBT treatment received during the follow-up period, and values from the intake interview (for the other predictor variables). Using Cox proportional hazards regression, we also examined whether BDD severity or delusionality predicted attrition from the study; data were available for 88% of the sample. Because we were interested in exploring whether BDD severity had a varying impact on functioning over time, we entered BDD severity and an interaction term between BDD severity and time into each model. Analyses assumed compound symmetry covariance correlations among the time points, the most restrictive assumption available. To reduce potential collinearity, baseline assessments of BDD severity scores were centered by subtracting the sample mean from each score. We selected (a priori) an alpha level of p< 0.01 to determine statistical significance. A p value between 0.01 and 0.05 was considered to constitute a trend.
RESULTS
As shown in Table 1, mean scores on the GAF, SOFAS, and LIFE-RIFT reflect poor psychosocial functioning over the follow-up period. Consistent with our hypothesis, random effects regression analyses indicated that functioning was stably poor over time, with no significant findings for time on the SOFAS (t=−0.65, df=38, p=.517) or LIFE-RIFT (t=−1.28, df=132, p=.201). There was a trend for gradual and slight improvement on the GAF over time (t=2.13, df=133, p=.035).
Table 1.
Psychosocial Functioning for Subjects with Body Dysmorphic Disorder
| Functioning Measure | Mean ± SD score a | |||
|---|---|---|---|---|
| Intake (n=176) | Year 1 (n=163) | Year 2 (n=141) | Year 3 (n=78) | |
| GAF b | 45.4 ± 10.9 | 48.3 ± 9.6 | 50.8 ± 10.8 | 49.9 ± 10.9 |
| SOFAS c,d | 47.7 ± 13.3 | 50.7 ± 12.1 | 53.2 ± 13.0 | 52.5 ± 13.5 |
| LIFE-RIFT total score | 14.4 ± 3.5 | 13.4 ± 3.4 | 12.5 ± 3.8 | 12.6 ± 3.9 |
Mean ± SD scores are based on monthly functioning scores from the previous year (e.g., year 1 scores reflect the mean ± SD for scores from months 1 through 12). At year 1, 70.6% of subjects met full DSM-IV criteria for BDD, and 6.1% were in full remission from BDD. At year 2, 62.7% met full criteria for BDD, and 12.0% were in full remission. At year 3, 60.3% met full criteria, and 7.7% were in full remission.
A GAF score of 41 to 50 reflects serious symptoms (e.g., suicidal ideation, severe obsessional rituals, frequent shoplifting) or any serious impairment in social, occupational, or school functioning (e.g., no friends, unable to keep a job)
A SOFAS score of 41 to 50 reflects serious impairment in social, occupational, or school functioning (e.g., no friends, unable to keep a job); a score of 51 to 60 reflects moderate difficulty in social, occupational, or school functioning (e.g., few friends, conflicts with peers or co-workers)
Because the SOFAS was added to the intake assessment after the study began, n = 104 for this measure at intake
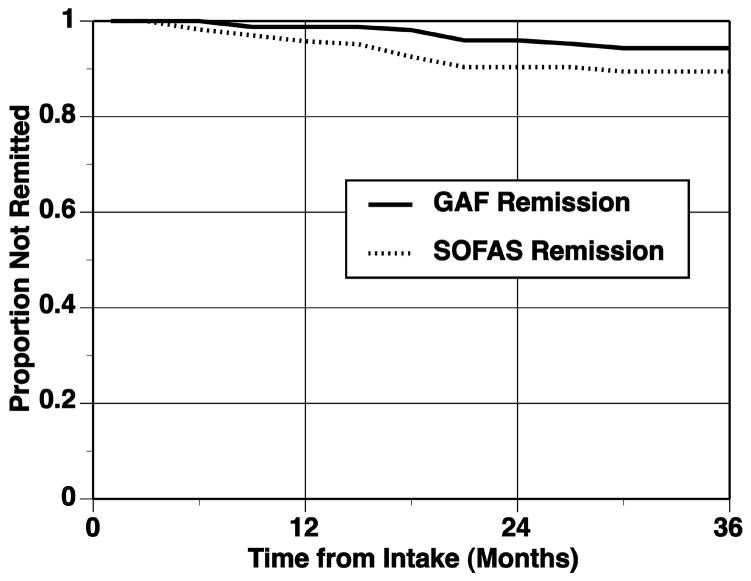
Over 1 to 3 years (mean = 2.7 ± 0.9 years) of follow-up, the cumulative probability of attaining functional remission on the GAF (score >70 for at least 2 consecutive months) was 5.7% (see Figure 1). On the SOFAS, the cumulative probability of attaining functional remission (score >70 for at least 2 consecutive months) during the follow-up period was 10.6% (see Figure 1). After attaining functional remission, some subjects continued to be functionally remitted whereas others subsequently worsened in terms of functioning. The proportion of subjects who were functionally remitted on the GAF at the time of each annual interview was 1.2% (n=2) at year 1, 4.3% (n=6) at year 2, and 3.9% (n=3) at year 3. On the SOFAS, 6.8% (n=11) were functionally remitted at year 1, 9.3% (n=13) at year 2, and 9.0% (n=7) at year 3.
Figure 1. Cumulative Probability of Attaining Functional Remission on the Global Assessment of Functioning Scale or the Social and Occupational Functioning Scale.
GAF = Global Assessment of Functioning Scale; SOFAS = Social and Occupational Functioning Scale
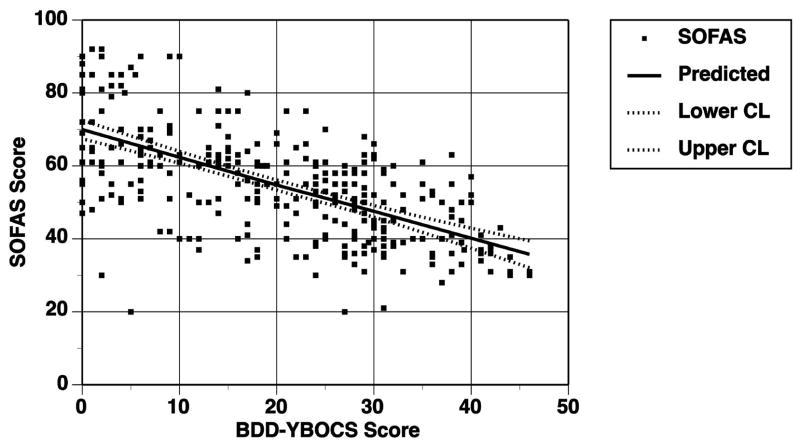
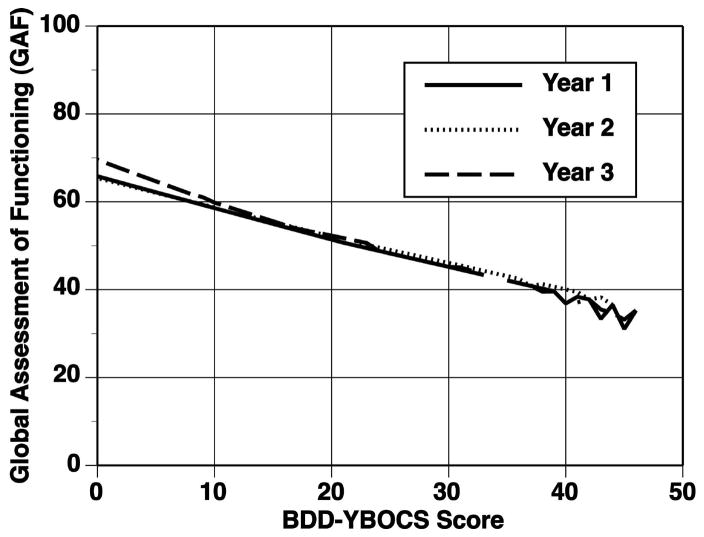
As hypothesized, BDD severity (BDD-YBOCS scores) significantly predicted psychosocial functioning on the GAF (t=−3.30, df=133, p=.0012), SOFAS (t=−3.37, df=38, p=.0017), and LIFE-RIFT (t=3.24, df=132, p=.0015). Figures 2 and 3 graphically illustrate the relationship between BDD-YBOCS scores and SOFAS and GAF scores, showing that more severe BDD symptoms are associated with poorer functioning. A visual inspection of these graphs suggests that the relationship between BDD severity and functioning is fairly linear across the full range of the sample. A time-by-BDD severity interaction was not found for the SOFAS (t=0.82, df=38, p=.419) or LIFE-RIFT (t=1.03, df=132, p=.305). A time-by-BDD severity interaction was found at a trend level for the GAF (t=−2.15, df=133, p=.033); as shown in Figure 3, less severe BDD symptoms were associated with better functioning (i.e., higher GAF scores), but as BDD severity increases, the difference between the years decreases at a trend level.
Figure 2. Relationship between BDD Severity and Level of Functioning on the Social and Occupational Functioning Scale.
BDD-YBOCS = Yale-Brown Obsessive Compulsive Scale Modified for Body Dysmorphic Disorder; SOFAS = Social and Occupational Functioning Scale. More than one data point may appear to constitute only a single point in the graph.
Figure 3. Relationship between BDD Severity and Level of Functioning on the Global Assessment of Functioning Scale.
BDD-YBOCS = Yale-Brown Obsessive Compulsive Scale Modified for Body Dysmorphic Disorder. More than one data point may appear to constitute only a single point in the graph.
Delusionality of BDD beliefs significantly predicted functioning on the GAF (t=−6.84, df=191, p<.0001), SOFAS (t=−5.60, df=94, p<.0001), and LIFE-RIFT (t=6.28, df=190, p<.0001). However, when controlling for BDD severity, delusionality no longer significantly predicted functioning on any measure (GAF: p=.079; SOFAS: p=.679; LIFE-RIFT: p=.454). Conversely, when controlling for delusionality, BDD severity still significantly predicted functioning on all three measures. Neither delusionality nor BDD severity predicted attrition from the study.
Regarding treatment, during the follow-up period 55.8% (n=91) of subjects received an SRI, and 22.7% (n=37) received an SRI trial considered at least minimally adequate for BDD. Twenty percent of subjects whose BDD beliefs were delusional at study intake received an antipsychotic during the follow-up period. During follow-up, 28.0% (n=45) of subjects received both cognitive and behavioral techniques (CBT) that focused on BDD, and 36.0% (n=58) received either cognitive or behavioral techniques that focused on BDD. Only 11.2% (n=18) of subjects received both CBT for BDD and an SRI trial considered at least minimally adequate for BDD (although not necessarily concurrently). Receipt of an SRI or CBT during follow-up did not predict psychosocial functioning on any measure. However, receipt of an SRI trial considered at least minimally adequate for BDD predicted significantly better SOFAS (p=.008) but not GAF or LIFE-RIFT scores. Age, gender, BDD duration, and the presence of a personality disorder did not predict psychosocial functioning on any measure.
DISCUSSION
Individuals with BDD had poor psychosocial functioning, consistent with previous studies (Hollander et al., 1999; Phillips, 2000; Phillips, 2006; Phillips & Najjar, 2003). In addition, prospectively assessed functioning remained stably poor over time. Notably few subjects achieved functional remission during the follow-up period. This was the case even though functional remission was conservatively defined. In survival analyses, subjects were required to have a GAF or SOFAS score >70 for as little as two consecutive months over the entire follow-up period, and they were considered functionally remitted even if functioning was slightly impaired (GAF or SOFAS score of 71–80).
Our study did not directly compare BDD to other disorders, so comparisons must be made with caution. To provide some context for interpreting our results, however, mean LIFE-RIFT scores in the observational NIMH Collaborative Depression Study at various follow-up periods for subjects with major depressive disorder who were “in episode” ranged from 13.56 ± 3.05 to 13.94 ± 3.25 (Leon et al., 1999). Subjects with bipolar I disorder from that study had mean LIFE-RIFT scores of 11.4 (for those subjects with current hypomania), 12.7 (for subjects with current minor depression or dysthymia), 14.0 (subjects with current mania), and 15.0 (subjects with current major depressive disorder) (Judd et al., 2005). GAF scores in our study are poorer than those reported for major depressive disorder and for borderline, schizotypal, avoidant, and obsessive compulsive personality disorders in an observational personality disorder study similar to ours which used the same interviewer trainers and training procedures as our study (Skodol et al., 2005).
Our finding that individuals with more severe BDD symptoms had poorer psychosocial functioning on all three functioning measures is consistent with studies of other disorders, which have demonstrated an association between psychiatric symptom severity and level of psychosocial functioning (e.g., Judd et al., 2005; Judd et al., 2000). Our finding is also largely consistent with a previous BDD study, which found that greater BDD severity (BDD-YBOCS score) was significantly associated with poorer SF-36 mental health (r=−.63, p<.001) and social functioning (r=−.55, p<.001) scores (although in that study BDD severity was not significantly correlated with SF-36 role limitations due to emotional problems [r=−.20, p=.15]) (Phillips, 2000). When interpreting our findings, it should be kept in mind that GAF score reflects both functioning level and symptom severity, and thus may be confounded with BDD severity to some extent. SOFAS scores reflect functioning level independent of symptom severity, however, and only one of the four LIFE-RIFT domains explicitly reflects the influence of psychopathology on functioning. Another consideration is that two of the 12 BDD-YBOCS items measure functional impairment (interference in functioning due to BDD preoccupations and compulsive BDD behaviors). Most BDD-YBOCS items, however, do not measure functional impairment. In addition, all three functioning measures assess functioning more broadly, not just impairment attributed to BDD specifically.
It is interesting that individuals with more delusional BDD beliefs had significantly poorer functioning on all three measures. This finding is consistent with a prior cross-sectional study which found that greater delusionality was significantly correlated with poorer SF-36 mental health (r=−.42, p=.002) and social functioning (r=−.33, p=.02). However, when controlling for BDD severity, delusionality no longer significantly predicted functioning on any measure. This finding is consistent with those in a prior report of the present study’s intake interview. In that report subjects with delusional BDD had significantly poorer scores on several, but not most, functioning measures, although these differences were no longer significant after controlling for BDD severity (Phillips et al., 2006). The relationship between illness severity, delusionality, and functioning is relevant to a number of disorders -- including obsessive compulsive disorder, major depressive disorder, hypochondriasis, and anorexia nervosa -- and needs further study (Eisen et al., 2004; Phillips, 2004; Schatzberg & Rothschild, 1992). In addition, dimensions that cut across psychiatric disorders – such as delusionality/insight -- will be of interest during the development of DSM-V (Kupfer, 2005); a better understanding of important aspects of dimensions, such as their relationship to functional impairment, may potentially be informative.
We found that receipt of an SRI (without considering the adequacy of dose or treatment duration) did not predict psychosocial functioning but that receipt of an at least minimally adequate SRI trial did predict better functioning on the SOFAS although not the GAF or LIFE-RIFT. SRI efficacy trials have consistently found that subjects treated with an SRI have significant improvement in psychosocial functioning (Hollander et al., 1999; Phillips, 2006; Phillips & Najjar, 2003; Phillips & Rasmussen, 2004). In the present study, receipt of CBT did not predict better functioning. To our knowledge, CBT efficacy studies have not examined functioning as an outcome measure (although CBT appears to often be efficacious for BDD symptoms [Neziroglu & Khemlani-Patel, 2002]) However, several caveats must be considered when interpreting these findings. Because the present study is observational, and subjects were not randomly assigned to treatment versus no treatment, definitive conclusions cannot be drawn about the impact of treatment on functioning. More severely ill individuals may be more likely to receive treatment in an observational study (i.e., confounding by severity), which may obscure possible benefits of treatment on symptoms and functioning. In addition, information on treatment was based on subject self-report, treatment compliance is unknown, and subjects may have been more complex than those in efficacy trials. Furthermore, many SRI treatments were not optimal, or even minimally adequate, for BDD, unlike treatment provided in BDD efficacy trials, in which treatment is usually optimized. In this study we did not determine the adequacy of CBT treatment, as it is unclear what constitutes an adequate number of CBT sessions for BDD (the number of sessions reported in the literature varies widely), and we were not able to assess the quality of CBT received for BDD. Future reports will further examine the relationship between treatment and functioning.
We did not find that duration of BDD predicted psychosocial functioning, although we previously reported that duration of BDD significantly predicted remission from BDD (Phillips et al, 2005c). This latter finding is consistent with some reports of other disorders (Keller & Shapiro, 1981; O’Leary et al., 2000). Additional research is needed to examine the relationship between illness duration and psychosocial functioning.
This study’s limitations include the relatively small number of third-year follow-up interviews and more limited power for some SOFAS analyses because this scale was added after the study began. Some potential predictors of functioning (e.g., stressful life events [Pagano et al., 2004]) were not examined. The sample was one of convenience from Southeastern New England, and it is unclear how generalizable the results are to other populations, other regions of the United States, or other countries. Statistical power was not sufficient to examine predictors of functional remission because so few functional remissions occurred. Studies in larger samples, in different settings, and over longer follow-up periods are needed to address these limitations and increase understanding of functional impairment, which is an important aspect of psychopathology (Wells et al., 1989). Studies on the relationship between delusionality and functioning are also needed in BDD and other disorders, as delusionality is an important and understudied dimension of a number of mental illnesses.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 1994. (DSM-IV) [Google Scholar]
- Bienvenu OJ, Samuels JF, Riddle MA, Hoehn-Saric R, Liang KY, Cullen BA, Grados MA, Nestadt G. The relationship of obsessive-compulsive disorder to possible spectrum disorders: results from a family study. Biological Psychiatry. 2000;48:287–293. doi: 10.1016/s0006-3223(00)00831-3. [DOI] [PubMed] [Google Scholar]
- Eisen JL, Phillips KA, Baer L, Beer DA, Atala KD, Rasmussen SA. The Brown Assessment of Beliefs Scale: reliability and validity. American Journal of Psychiatry. 1998;155:102–108. doi: 10.1176/ajp.155.1.102. [DOI] [PubMed] [Google Scholar]
- Eisen JL, Phillips KA, Coles ME, Rasmussen SA. Insight in obsessive compulsive disorder and body dysmorphic disorder. Comprehensive Psychiatry. 2004;45:10–15. doi: 10.1016/j.comppsych.2003.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders: Non-patient edition (SCID-I N/P) New York: NYSPI; 1996. [Google Scholar]
- Goisman RM, Warshaw MG, Peterson LG, Rogers MP, Cuneo P, Tomlin-Albanese JM, Kazin A, Gollan J, Epstein-Kaye T, Reich JH, Keller MB. Panic, agoraphobia, and panic with agoraphobia: data from a multi-center anxiety disorder study. Journal of Nervous and Mental Disease. 1994;182:72–79. doi: 10.1097/00005053-199402000-00002. [DOI] [PubMed] [Google Scholar]
- Hollander E, Allen A, Kwon J, Aronowitz B, Schmeidler J, Wong C, Simeon D. Clomipramine vs desipramine crossover trial in body dysmorphic disorder. Archives of General Psychiatry. 1999;56:1033–1039. doi: 10.1001/archpsyc.56.11.1033. [DOI] [PubMed] [Google Scholar]
- Judd LL, Akiskal HS, Schettler PJ, Endicott J, Leon AC, Solomon DA, Coryell W, Maser JD, Keller MB. Psychosocial disability in the course of bipolar I and II disorders. Arch Gen Psychiatry. 2005;62:1322–1330. doi: 10.1001/archpsyc.62.12.1322. [DOI] [PubMed] [Google Scholar]
- Judd LL, Akiskal HS, Zeller PJ, Paulus M, Leon AC, Maser JD, Endicott J, Coryell W, Kunovac JL, Mueller TI, Rice JP, Keller MG. Psychosocial disability during the long-term course of unipolar major depressive disorder. Archives of General Psychiatry. 2000;57:375–380. doi: 10.1001/archpsyc.57.4.375. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC. The Longitudinal Interval Follow-up Evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Keller MB, Shapiro RW. Major depressive disorder: initial results from a one-year prospective naturalistic follow-up study. The Journal of Nervous and Mental Disease. 1981;169:761–768. [PubMed] [Google Scholar]
- Kupfer DJ. Dimensional models for research and diagnosis: a current dilemma. Journal of Abnormal Psychology. 2005;114:557–559. doi: 10.1037/0021-843X.114.4.557. [DOI] [PubMed] [Google Scholar]
- Leon AC, Solomon DA, Mueller TI, Turvey CL, Endicott J, Keller MB. The Range of Impaired Functioning Tool (LIFE-RIFT): A brief measure of functional impairment. Psychological Medicine. 1999;29:869–878. doi: 10.1017/s0033291799008570. [DOI] [PubMed] [Google Scholar]
- Morselli E. Sulla dismorfofobia e sulla tafefobia. Bolletinno della R accademia di Genova. 1891;6:110–119. (translated by Jerome L., 2001. History of Psychiatry, 103–114) [Google Scholar]
- Neziroglu F, Khemlani-Patel S. A review of cognitive and behavioral treatment for body dysmorphic disorder. CNS Spectrums. 2002;7:464–471. doi: 10.1017/s1092852900017971. [DOI] [PubMed] [Google Scholar]
- O’Leary D, Costello F, Niall G, Webb M. Remission onset and relapse in depression: an 18- month prospective study of course for 100 first admission patients. Journal of Affective Disorders. 2000;57:159–171. doi: 10.1016/s0165-0327(99)00086-5. [DOI] [PubMed] [Google Scholar]
- Pagano ME, Skodol AE, Stout RL, Shea MT, Yen S, Grilo CM, Sanislow CA, Bender DS, McGlashan TH, Zanarini MC, Gunderson JG. Stressful life events as predictors of functioning: findings from the Collaborative Longitudinal Personality Disorders Study. Acta Psychiatrica Scandinavica. 2004;110:421–429. doi: 10.1111/j.1600-0447.2004.00398.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips KA. Body dysmorphic disorder: the distress of imagined ugliness. American Journal of Psychiatry. 1991;148:1138–1149. doi: 10.1176/ajp.148.9.1138. [DOI] [PubMed] [Google Scholar]
- Phillips KA. Quality of life for patients with body dysmorphic disorder. Journal of Nervous and Mental Disease. 2000;188:170–175. doi: 10.1097/00005053-200003000-00007. [DOI] [PubMed] [Google Scholar]
- Phillips KA. Psychosis in body dysmorphic disorder. Journal of Psychiatric Research. 2004;38:63–72. doi: 10.1016/s0022-3956(03)00098-0. [DOI] [PubMed] [Google Scholar]
- Phillips KA. An open-label study of escitalopram in body dysmorphic disorder. International Clinical Psychopharmacology. 2006;21:177–179. doi: 10.1097/01.yic.0000194378.65460.ef. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips KA, Albertini RS, Rasmussen SA. A randomized placebo-controlled trial of fluoxetine in body dysmorphic disorder. Archives of General Psychiatry. 2002;59:381–388. doi: 10.1001/archpsyc.59.4.381. [DOI] [PubMed] [Google Scholar]
- Phillips KA, Hollander E, Rasmussen SA, Aronowitz BR, DeCaria C, Goodman WK. A severity rating scale for body dysmorphic disorder: development, reliability, and validity of a modified version of the Yale-Brown Obsessive Compulsive Scale. Psychopharmacology Bulletin. 1997;33:17–22. [PubMed] [Google Scholar]
- Phillips KA, McElroy SL, Keck PE, Jr, Pope HG, Jr, Hudson JI. Body dysmorphic disorder: 30 cases of imagined ugliness. American Journal of Psychiatry. 1993;150:302–308. doi: 10.1176/ajp.150.2.302. [DOI] [PubMed] [Google Scholar]
- Phillips KA, Menard W, Fay C, Pagano M. Psychosocial functioning and quality of life in body dysmorphic disorder. Comprehensive Psychiatry. 2005a;46:254–260. doi: 10.1016/j.comppsych.2004.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips KA, Menard W, Fay C, Weisberg R. Demographic characteristics, phenomenology, comorbidity, and family history in 200 individuals with BDD. Psychosomatics. 2005b;46:317–332. doi: 10.1176/appi.psy.46.4.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips KA, Menard W, Pagano M, Fay C, Stout RL. Delusional versus nondelusional body dysmorphic disorder: clinical features and course of illness. Journal of Psychiatric Research. 2006a;40:95–104. doi: 10.1016/j.jpsychires.2005.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips KA, Najjar F. An open-label study of citalopram in body dysmorphic disorder. Journal of Clinical Psychiatry. 2003;64:715–720. doi: 10.4088/jcp.v64n0615. [DOI] [PubMed] [Google Scholar]
- Phillips KA, Pagano ME, Menard W. Pharmacotherapy for body dysmorphic disorder: treatment received and illness severity. Annals of Clinical Psychiatry. 2006b;18:251–257. doi: 10.1080/10401230600948464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips KA, Pagano ME, Menard W, Fay C, Stout RL. Predictors of remission from body dysmorphic disorder: a prospective study. Journal of Nervous and Mental Disease. 2005c;193:564–567. doi: 10.1097/01.nmd.0000172681.51661.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips KA, Rasmussen SA. Change in psychosocial functioning and quality of life of patients with body dysmorphic disorder treated with fluoxetine: a placebo-controlled study. Psychosomatics. 2004;45:438–444. doi: 10.1176/appi.psy.45.5.438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rief W, Buhlmann U, Wilhelm S, Borkenhagen A, Brahler E. The prevalence of body dysmorphic disorder: a population-based survey. Psychological Medicine. 2006;36:877–885. doi: 10.1017/S0033291706007264. [DOI] [PubMed] [Google Scholar]
- Schatzberg AF, Rothschild AJ. Psychotic (delusional) major depression: should it be included as a distinct syndrome in DSM-IV? American Journal of Psychiatry. 1992;149:733–745. doi: 10.1176/ajp.149.6.733. [DOI] [PubMed] [Google Scholar]
- Skodol AE, Pagano ME, Bender DS, Shea MT, Gunderson JG, Yen S, Stout RL, Morey LC, Sanislow CA, Grilo CM, Zanarini MC, McGlashan TH. Stability of functional impairment in patients with schizotypal, borderline, avoidant, or obsessive-compulsive personality disorder over two years. Psychological Medicine. 2005;35:443–451. doi: 10.1017/s003329170400354x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steketee G, Perry JC, Goisman RM, Warshaw MG, Massion AO, Peterson LG, Langford L, Weinshenker N, Farreras IG, Keller MB. The Psychosocial Treatments Interview for anxiety disorders: a method for assessing psychotherapeutic procedures in anxiety disorders. Journal of Psychotherapy Practice and Research. 1997;6:45–61. [PMC free article] [PubMed] [Google Scholar]
- Ware JE., Jr . SF-36 Health Survey Manual and Interpretation Guide. Boston: The Health Institute, New England Medical Center; 1993. [Google Scholar]
- Wells KB, Stewart A, Hays RD, Burnam A, Rogers W, Daniels M, Berry S, Greenfield S, Ware J. The functioning and well-being of depressed patients. Journal of the American Medical Association. 1989;262:914–919. [PubMed] [Google Scholar]