Abstract
Background
We previously noted that older adults admitted to surgical ICUs (SICUs) are at high risk for delirium. In the current study, we describe the association between the presence of delirium and complications in older SICU patients, and describe the association between delirium occurring in the SICU and functional ability and discharge placement for older patients.
Methods
Secondary analysis of prospective, observational, cohort study. Subjects were 114 consecutive patients ≥ 65 years old admitted to a surgical critical care service. All subjects underwent daily delirium and sedation/agitation screening during hospitalization. Outcomes prospectively recorded included SICU complication development, discharge location, and functional ability (as measured by the Katz activities of daily living instrument).
Results
Nearly one third of older adults (31.6%) admitted to an SICU had a complication during ICU stay. There was a strong association between SICU delirium and complication occurrence (p = 0.001). Complication occurrence preceded delirium diagnosis for 16 of 20 subjects. Subjects with delirium in the SICU were more likely to be discharged to a place other than home (61.3% vs 20.5%, p < 0.0001) and have greater functional decline (67.7% vs 43.6%, p = 0.023) than nondelirious subjects. After adjusting for covariates including severity of illness and mechanical ventilation use, delirium was found to be strongly and independently associated with greater odds of being discharged to a place other than home (odds ratio, 7.20; 95% confidence interval, 1.93 to 26.82).
Conclusions
Delirium in older surgical ICU patients is associated with complications and an increased likelihood of discharge to a place other than home.
Keywords: aged, complications, critical care, delirium, discharge placement, functional status, intensive care, outcomes, surgery
Delirium is a potentially debilitating disorder experienced by many older adults admitted to ICUs. Often defined as acute cognitive dysfunction,1 as many as 30 to 62%2,3 of older patients have an episode of delirium during ICU stay. The elevated risk for delirium in the older critically ill population is thought to be due to both intrinsic and extrinsic factors, including preexisting cognitive impairment (dementia), depression, impairments in activities of daily living (ADL), severity of illness, outpatient use of benzodiazepines or narcotics, and a variety of physiologic abnormalities.4 Once thought to be an “inconsequential” outcome of ICU care,1 research suggests that delirium in this setting is associated with multiple unfavorable short-term and long-term outcomes including higher ICU and hospital costs,5 longer ICU and hospital length of stay,2,6–8 greater use of continuous sedation and physical restraints,9 increased removal of catheters and self-extubation,10 and higher ICU and hospital mortality rates.6,11,12 Delirium is also an independent predictor of mortality at 6 months after hospital discharge in ICU patients receiving mechanical ventilation.12
Several factors, such as dementia and dependency for the performance of ADLs, are known to contribute to postoperative complications for older adults.13 Older adults are also more likely to have conditions affecting surgical utilization rates and outcomes, such as cancer diagnoses, malnutrition, and social isolation.14 However, no studies to date have specifically examined the effect of delirium on outcomes of older adults admitted to surgical ICUs (SICUs). This is a significant gap, considering people > 65 years old comprise more than one half of the average general surgery practice,14 consume nearly 60% of all ICU days,15 and are one of the fastest-growing segments of the US population.
For this reason, we conducted a secondary analysis of a data set that was designed to examine the course of delirium in a cohort of older adults admitted to SICUs. Our first aim was to describe the association between the presence of delirium and complications in older SICU patients. Our second aim was to describe the association between delirium occurring in the SICU and older adults' posthospital functional ability and discharge placement. We hypothesized that there would be a positive association between delirium and SICU complications and that older adults with an episode of delirium during their SICU stay would have decreased functional ability at hospital discharge and would be more likely to be discharged to a place other than home when compared to older adults with no delirium.
Materials and Methods
Data for the current analyses were derived from a prospective, observational, cohort study that was designed to examine the course of delirium in older SICU patients. While the frequency and trajectory of mental status changes of this sample were described elsewhere,2 none of the outcome data reported in the present study have been previously published. Study participants were recruited from SICUs at the Hospital of the University of Pennsylvania, a 700-bed, urban, teaching hospital. All consecutive patients ≥ 65 years old admitted to the surgical critical care service between August 27, 2004, and December 31, 2004, were considered for study inclusion. The University of Pennsylvania institutional review board approval of the study previously reported2 included the further statistical analysis included in this article. Written informed consent was obtained from all patients, if capable, and their surrogates. In the event where a patient was not capable of providing informed consent, it was obtained from his/her surrogate and then later obtained when decisional capacity returned.
Enrollment criteria included age ≥ 65 years, English speaking, admitted to a SICU, and managed by the surgical critical care service. Participation also required the availability of a surrogate responder who maintained in-person or telephone contact exceeding 4 h/wk with the patient over the previous 5 years. Both the patient and his/her surrogate needed to agree to participate in the study within 24 to 48 h of SICU admission. Exclusion criteria defined a priori were recent (within 1 year) CNS injury (defined as head or spinal cord injury, neurosurgical procedure, or cerebral vascular accident); current or past treatment for specific Diagnosis and Statistical Manual of Mental Disorders IV axis 1 psychotic disorders; legal blindness; deafness; and, because of the frequent postoperative cognitive dysfunction associated with cardiopulmonary bypass, cardiothoracic surgery. Study enrollment flow is illustrated in Figure 1.
Figure 1.
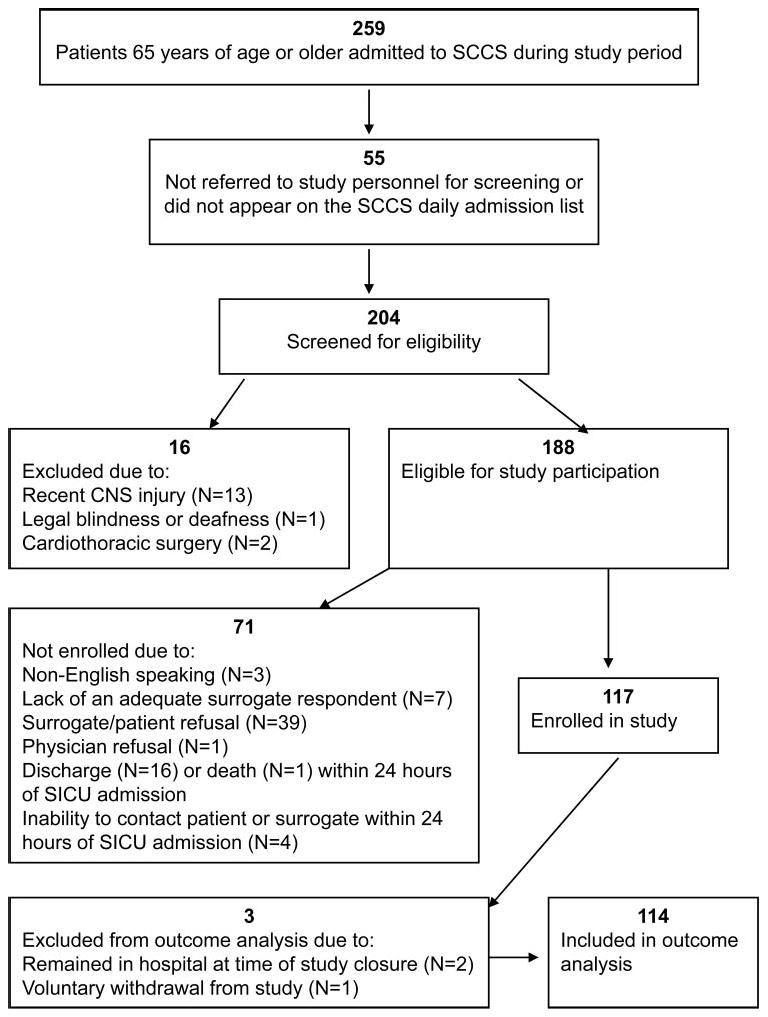
Flow of study enrollment. SCCS = surgical critical care service.
Structured interviews with all of the subjects' surrogates were conducted within 24 to 48 h of SICU admission to obtain information regarding demographic data, psychiatric history, preadmission visual, hearing and health status, and prior living arrangements. The use of home health care (HHC) services or any assistive device use to perform ADL was also recorded. The Katz ADL16 index was used to formally assess the baseline functional ability with a reference point of 1 week prior to current hospitalization. The range of scores for the Katz ADL is 0 to 6, with higher scores reflecting higher levels of function. Subjects were screened for evidence of preexisting dementia with the use of the short form of the Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE).17 The short IQCODE requires informants to recall what their relative/family member's memory/intelligence was like 5 years ago and compare it to their present ability. It consists of 16 questions that are rated on a 5-point scale ranging from 1 (much improved) to 5 (much worse). A cut score of 3.31 achieves a balance of sensitivity (79%) and specificity (82%) for detecting dementia.17
Study personnel recorded the APACHE (acute physiology and chronic health evaluation) II scores,18 admitting service, operative procedures, and also calculated their Charlson comorbidity index (CCI)19 scores from the medical record. Mechanical ventilation use was recorded daily throughout the hospital stay. Complication occurrence in the SICU was detected by daily review of physician progress notes for 15 commonly encountered complications (eg, pneumonia, urinary tract infection, pulmonary emboli). Study personnel recorded if, and how many, complications the subjects' had each day during the SICU stay.
Subjects underwent daily sedation/agitation and delirium screening between the hours of 10:00 am and 7:00 pm from study enrollment to hospital discharge. Interrater agreement for delirium and agitation/sedation status was obtained by having the two study personnel responsible for screenings perform their assessments together until 100% agreement on findings was obtained. Level of arousal was measured using the Richmond Agitation-Sedation Scale,20,21 which rates a patient's level of agitation/sedation on a 10-point scale ranging from − 5 (unarousable, not responsive to voice or physical stimulation) to + 4 (combative). Delirium in the SICU was diagnosed with the Confusion Assessment Method for the ICU (CAM-ICU).23,24 The CAM-ICU assesses four features of delirium: (1) acute onset or fluctuating course, (2) inattention, (3) disorganized thinking, and (4) altered level of consciousness.22,23 To be diagnosed as delirious or CAM-ICU positive, the subject must display features 1 and 2, and either 3 or 4. The CAM-ICU has proven valid and reliable in ICU populations including older adults admitted to medical ICUs.3 Subjects in this study were coded delirious in the SICU if they had a Richmond Agitation-Sedation Scale score ≥ − 3 and scored positive on the CAM-ICU.
Within 24 to 48 h of anticipated hospital discharge, subjects' were administered the Katz ADL. At this time, both subjects and nurses were questioned about where and with whom subjects would be discharged and whether they would receive HHC services.
Data Analysis
Descriptive statistics were used to examine sample characteristics. The baseline characteristics and intrahospital variables between those subjects who were ever rated delirious during their SICU stay and those who never had delirium during this period were compared using Student t test for continuous variables and χ2 test for categorical variables.
Two multivariable logistic regression models were developed to determine if SICU delirium had an effect on the subjects' functional ability and discharge placement. In these models, the presence of SICU delirium and covariates, which were chosen based on clinical judgment and previous research studies,3,4,6–11,14 were the independent and explanatory variables. Covariates included surgical service type, gender, impaired hearing, preadmission Katz ADL score, IQCODE score, mechanical ventilation use, complications, age, and APACHE II and CCI scores. The dependent variable for the functional ability model was a change in the subjects Katz ADL score from hospital admission to discharge (where the probability modeled was 1 (decrease in KATZ ADL score) vs 0 (increase or no change from admission to hospital discharge). Similarly, multivariate logistic regression was used to determine if SICU delirium affected the subject's likelihood of being discharged to a place other than home (where the probability modeled was 1 [any place other than home] vs 0 [home]). In both models, adjusted odds ratios with 95% confidence intervals (CIs) were calculated. Models were assessed for evidence of multicollinearity and goodness of fit. Statistical significance was defined as a p value < 0.05, and all analyses were performed using statistical software (SAS version 9.1; SAS Institute; Cary, NC).
Results
Demographic and preadmission characteristics of the 114 subjects are presented in Tables 1, 2. The subjects were predominantly older (average age, 75 years), white (85%), and male (59.6%). While most subjects had visual impairment (98.3%) or hearing loss (43.9%), the vast majority were living at home (96.5%) prior to hospitalization. Thirty-three subjects (28.9%) used some type of assistive device to perform the ADL. Only 9.1% of those living at home received HHC services prior to hospitalization. Twenty-one subjects (18.4%) scored ≥ 3.31 on the IQCODE (suggesting evidence of preexisting dementia). Severity of illness as measured by APACHE II was 14.5 ± 6.7 on SICU admission. Study subjects had an average CCI score of 4.5 ± 2.9 (± SD). Forty-eight subjects (42.1%) received mechanical ventilation sometime during SICU admission. Thirty-four subjects (29.8%) had delirium sometime during SICU stay. Subjects with SICU delirium were significantly more likely to have preadmission hearing impairment, have an unplanned hospital admission, receive mechanical ventilation, and have higher APACHE II scores than nondelirious subjects (Table 1).
Table 1. Characteristics of SICU Study Sample Grouped by Delirium Status*.
| Characteristics | Overall Sample (n = 114) |
SICU Delirious (n = 34) |
SICU Nondelirious (n = 80) |
p Value |
|---|---|---|---|---|
| Age, yr | 75.4 ± 6.3 | 75.5 ± 6.9 | 75.4 ± 6.0 | 0.931 |
| Male gender | 68 (59.6) | 23 (67.6) | 45 (56.3) | 0.257 |
| Hearing loss | 50 (43.9) | 21 (61.8) | 29 (36.3) | 0.012 |
| Visual impairment | 112 (98.2) | 34 (100) | 78 (97.5) | 1.000 |
| Admission planned | 82 (71.9) | 18 (52.9) | 64 (80.0) | 0.003 |
| Ethnicity (white) | 97 (85.1) | 28 (82.4) | 69 (86.3) | 0.593 |
| Currently married | 76 (66.7) | 21 (61.8) | 55 (68.8) | 0.469 |
| Assistive device use† | 33 (28.9) | 9 (26.5) | 24 (30.0) | 0.703 |
| Katz ADL < 5‡ | 89 (78.1) | 24 (70.6) | 65 (81.3) | 0.208 |
| Admitting service | 0.089 | |||
| General surgery§ | 42 (36.8) | 9 (26.5) | 33 (41.3) | |
| Vascular surgery | 40 (35.1) | 10 (29.4) | 30 (37.5) | |
| Trauma/emergency surgery | 18 (15.8) | 9 (26.5) | 9 (11.3) | |
| Other‖ | 14 (12.3) | 6 (17.6) | 8 (10.0) | |
| IQCODE score ≥ 3.31 | 21 (18.8) | 9 (26.5) | 12 (15.0) | 0.135 |
| APACHE II | 14.5 ± 6.7 | 17.5 ± 6.6 | 13.2 ± 6.3 | 0.001 |
| CCI | 4.5 ± 2.9 | 4.5 ± 2.9 | 4.5 ± 2.9 | 0.894 |
| Mechanical ventilation during SICU stay (yes) | 48 (42.1) | 21 (61.8) | 27 (33.8) | 0.006 |
Data are presented as mean ± SD or No. (%).
Assistive devices included canes/crutches, walkers, wheelchairs, or shower seats.
Katz ADL > 5 means independent in five or more ADL.
General surgery category includes colorectal, surgical oncology, and GI surgical services.
Other category includes otorhinolaryngology, oral/maxillofacial, urology, gynecology/oncology, orthopedics, and plastic surgical services.
Table 2. Functional Ability and Living Arrangements of Study Population*.
| Characteristics | Preadmission (n = 114) |
Discharge (n = 109) |
|---|---|---|
| Residence | ||
| Home | 110 (96.5) | 74 (67.9) |
| Living conditions | ||
| Alone | 19 (17.3)† | 6 (8.1)† |
| Spouse | 75 (68.2)† | 52 (70.3)† |
| Child | 10 (9.1)† | 9 (12.2)† |
| Significant other | 6 (5.5)† | 7 (9.5)† |
| HHC/personal assistant | 10 (9.1)† | 33 (44.6)† |
| Nursing home | 0 (0) | 3 (2.8) |
| Skilled nursing facility | 1 (0.9) | 15 (13.8) |
| Rehabilitation center | 1 (0.9) | 14 (12.8) |
| Other | 2 (1.8) | 3 (2.8) |
| Katz ADL score‡ | ||
| 6 | 89 (78.1) | 46 (42.2) |
| 5 | 15 (13.2) | 22 (20.2) |
| 4 | 3 (2.6) | 8 (7.3) |
| 3 | 1 (0.9) | 8 (7.3) |
| 2 | 1 (0.9) | 11 (10.1) |
| 1 | 5 (4.4) | 8 (7.3) |
| 0 | 0 (0) | 6 (5.5) |
| Katz ADL categories | ||
| Bathing independent | 102 (89.5) | 71 (65.1) |
| Dressing independent | 106 (92.9) | 69 (63.3) |
| Toileting independent | 108 (94.7) | 80 (73.4) |
| Transferring independent | 108 (94.7) | 68 (62.4) |
| Continence independent | 93 (81.6) | 86 (78.9) |
| Feeding independent | 114 (100) | 98 (89.9) |
| Katz ADL score | 5.5 ± 1.2 | 4.3 ± 2.0 |
Data are presented as No. (%) or mean ± SD.
Preadmission living conditions and HHC/personal assistant use calculated on 110 subjects reporting being admitted from home; discharge living conditions and HHC use calculated on 74 subjects reporting being discharged home.
The range of scores for the Katz ADL is 0 (dependent in all ADL) to 6 (independent in all ADL).
Complications
Thirty-six subjects (31.6%) had at least one complication during SICU stay. A total of 73 complications were experienced by the sample. Most of the complications were cardiopulmonary, and included cardiac arrhythmias (n = 19), pneumonia (n = 7), and reintubation (n = 7). Subjects with delirium were significantly more likely than nondelirious subjects to have an SICU complication (20 of 34 subjects [59%] vs 16 of 80 subjects [20%]; p = 0.001). Complications preceded delirium onset in most subjects who experienced delirium (16 of 20 subjects).
Discharge Placement
Of the 109 subjects with postdischarge placement information, most (n = 74; 67.9%) were discharged directly home (Table 2). The majority of these subjects reported they would be living with their spouse on discharge (70.3%; 52 of 74 subjects). Thirty-three patients (44.6%) discharged home reported they would be receiving HHC services. Thirty-five subjects (32.1%) required some form of postdischarge institutional care. Most of these subjects were discharged to either skilled nursing facilities (n = 15) or rehabilitation centers (n = 14). Univariate analysis revealed that in addition to SICU delirium, an unplanned admission, hearing loss, assistive device use, lower preadmission functional status, complications, and surgical service type were all significantly associated with discharge placement (Table 3). After adjusting for these variables, only SICU delirium (p = 0.003) was associated with discharge to a place other than home. Delirium occurring in the SICU increased by 7.2 (CI, 1.93 to 26.82) the odds of being discharged to place other than home (Table 4).
Table 3. Univariate Logistical Analysis of Risk of Discharge to a Place Other than Home and Decrease in Katz ADL Score in 114 Older Adults Admitted to an SICU.
| Variables | Discharged Not Home | Katz ADL Decreased | ||
|---|---|---|---|---|
| Odds Ratio (95% CI) [Unadjusted] | p Value | Odds Ratio (95% CI) [Unadjusted] | p Value | |
| SICU delirium | 6.14 (2.48–15.21) | < 0.0001 | 2.72 (1.13–6.52) | 0.025 |
| Service | 0.009 | 0.014 | ||
| Trauma | 8.00 (2.22–28.83) | 0.002 | 4.21 (1.16–15.23) | 0.029 |
| Vascular | 1.00 (reference) | 1.00 (reference) | ||
| General* | 1.11 (0.40–3.12) | 0.842 | 0.78 (0.32–1.91) | 0.582 |
| Other† | 1.48 (0.37–5.97) | 0.580 | 4.31 (1.03–18.15) | 0.046 |
| Admission planned | 0.23 (0.09–0.57) | 0.002 | 0.30 (0.12–0.77) | 0.012 |
| Nonwhite | 0.96 (0.30–2.99) | 0.937 | 0.98 (0.34–2.82) | 0.968 |
| Female | 2.08 (0.92–4.71) | 0.081 | 3.19 (1.42–7.14) | 0.005 |
| Not married | 2.02 (0.87–4.72) | 0.101 | 1.49 (0.66–4.37) | 0.338 |
| Hearing loss | 2.61 (1.15–5.96) | 0.022 | 1.65 (0.77–3.57) | 0.201 |
| Living alone | 1.34 (0.48–3.77) | 0.580 | 1.14 (0.42–3.06) | 0.801 |
| Assistive device use | 2.95 (1.23–7.09) | 0.016 | 0.98 (0.42–2.26) | 0.953 |
| Pre-Katz ADL < 5 | 3.34 (1.27–8.77) | 0.014 | ||
| IQCODE < 3.31 | 0.60 (0.22–1.66) | 0.323 | 1.54 (0.57–4.19) | 0.399 |
| Mechanical ventilation use | 1.16 (0.52–2.63) | 0.716 | 0.97 (0.45–2.08) | 0.937 |
| Complication, %‡ | 3.72 (1.55–8.89) | 0.003 | 3.59 (1.47–8.79) | 0.005 |
| Age | 1.06 (0.99–1.14) | 0.068 | 1.05 (0.99–1.12) | 0.137 |
| APACHE II | 1.05 (0.99–1.13) | 0.119 | 1.05 (0.99–1.12) | 0.125 |
| CCI | 0.94 (0.81–1.08) | 0.368 | 1.05 (0.92–1.20) | 0.437 |
General surgery category includes colorectal, surgical oncology, and GI surgical services.
Other category includes otorhinolaryngology, oral/maxillofacial, urology, gynecology/oncology, orthopedics, and plastic surgical services.
The type and number of SICU complications in the study population included cardiac arrhythmias (n = 19), pneumonia (n = 7), reintubation (n = 7), urinary tract infection (n = 6), acute renal failure (n = 6), GI bleeding (n = 6), deep vein thrombosis (n = 5), myocardial infarction (n = 4), suspected adverse drug event (n = 4), sepsis (n = 3), pulmonary emboli (n = 3), cerebral vascular accident (n = 2), and cardiopulmonary resuscitation (n = 1).
Table 4. Multivariate Analysis of Risk of Discharge to a Place Other than Home and Decrease in Katz ADL Score in 114 Older Adults Admitted to an SICU*.
| Variables | Discharged Not Home | KATZ ADL Decreased | ||
|---|---|---|---|---|
| Odds Ratio (95% CI) [Adjusted] | p Value | Odds Ratio (95% CI) [Adjusted] | p Value | |
| SICU delirium | 7.20 (1.93–26.82) | 0.003 | 3.41 (0.95–12.19) | 0.059 |
| Service | 0.279 | 0.113 | ||
| Trauma | 4.83 (0.99–23.68) | 0.052 | 2.57 (0.54–12.34) | 0.238 |
| Vascular | ||||
| General† | 1.66 (0.46–6.03) | 0.444 | 0.65 (0.21–1.99) | 0.448 |
| Other‡ | 1.12 (0.15–8.39) | 0.911 | 4.19 (0.63–27.98) | 0.139 |
| Females | 2.97 (0.89–9.78) | 0.074 | 5.81 (1.96–17.20) | 0.002 |
| Hearing loss | 2.47 (0.77–7.89) | 0.128 | 1.63 (0.57–4.61) | 0.360 |
| Pre-Katz ADL < 5 | 1.48 (0.39–5.63) | 0.569 | ||
| IQCODE < 3.31 | 1.02 (0.23–4.59) | 0.971 | 3.78 (0.88–16.15) | 0.073 |
| Mechanical ventilation use | 0.76 (0.20–2.83) | 0.677 | 0.45 (0.14–1.45) | 0.183 |
| Complication§ | 1.73 (0.50–5.94) | 0.387 | 1.44 (0.42–5.01) | 0.559 |
| Age | 1.03 (0.94–1.14) | 0.477 | 1.04 (0.96–1.14) | 0.339 |
| APACHE II | 1.02 (0.92–1.14 | 0.671 | 1.08 (0.97–1.19) | 0.148 |
| CCI | 0.99 (0.80–1.21) | 0.890 | 1.08 (0.89–1.31) | 0.411 |
C statistic for discharge placement model = 0.83; C statistic for functional ability model = 0.81.
General surgery category includes colorectal, surgical oncology, and GI surgical services.
Other category includes otorhinolaryngology, oral/maxillofacial, urology, gynecology/oncology, orthopedics, and plastic surgical services.
The type and number of SICU complications in the study population included cardiac arrhythmias (n = 19), pneumonia (n = 7), reintubation (n = 7), urinary tract infection (n = 6), acute renal failure (n = 6), GI bleeding (n = 6), deep vein thrombosis (n = 5), myocardial infarction (n = 4), suspected adverse drug event (n = 4), sepsis (n = 3), pulmonary emboli (n = 3), cerebral vascular accident (n = 2), cardiopulmonary resuscitation (n = 1).
Functional Ability
While 78.1% (89 of 114 subjects) were functionally independent prior to hospital admission, fewer than half (42.2%; 46 of 109 subjects) were fully independent at discharge (Table 2). The Katz ADL category with the greatest percentage decrease from admission to discharge was transferring, followed by dressing and bathing. A total of 4 subjects had an improvement in Katz ADL score from admission to discharge, 50 subjects had no change, and 55 subjects had a decrease. A total of 21 of 31 delirious subjects (67.7%) had a decrease in Katz ADL scores, vs 34 of 78 nondelirious subjects (43.6%) [p = 0.023]. Univariate analysis revealed in addition to delirium, surgical service type, an unplanned admission, female gender, and complications were all significantly associated with a decrease in Katz ADL score (Table 3). Only gender was found to significantly predict functional decline in the multiple regression model (Table 4). Female subjects were at a 5.8 (95% CI, 1.96 to 17.20) increased odds of having a decrease in Katz ADL score from admission to hospital discharge. Delirium in the SICU approached significance (p = 0.059), increasing the odds of functional decline by 3.4 (95% CI, 0.95 to 12.19).
Discussion
To our knowledge, this is the first study examining the association of delirium and short-term outcomes of older adults admitted to SICUs. We found that nearly one third of older adults admitted to a SICU had a complication during their ICU stay. There was a strong association between SICU delirium and complication occurrence. Unexpectedly, most subjects in this sample had a complication before delirium was diagnosed. This suggests that ICU complications may serve as a risk factor for delirium. Further study of this area is warranted. This is particularly important as the Centers for Medicare and Medicaid Services consider expanding the list of hospital-acquired conditions for nonpayment. The proposed list for 2009 includes delirium and conditions (ie, complications) such as extreme blood sugar derangement, iatrogenic pneumothorax, ventilator-associated pneumonia, and deep vein thrombosis/pulmonary embolism.24
We also found that SICU delirium was associated with a decrease in functional ability at hospital discharge and greater likelihood of being discharged to a place other than home. Even after controlling for a number of important variables including age, severity of illness, and mechanical ventilation use, an older adult with SICU delirium was seven times more likely to be discharged to a place other than home. While not statistically significant, delirium increased the odds of functional decline over threefold. It is likely, that if the sample had been larger, this finding would have reached significance. These results are consistent with prior studies of the effect of delirium on hospitalized (non-ICU) older adults' functional ability and discharge placement.25–28
Our findings have significant clinical and research implications. First, they support the mounting evidence that delirium is an important, independent prognosticator of poor outcomes in the critically ill older adult. We suggest both routine delirium assessment and the judicious use of sedatives and analgesics (as offered in the SCCM guidelines)29 be incorporated into the plan of care of all critically ill older adults. We also suggest that strategies intended to decrease the frequency and severity of delirium in hospitalized older adults (ie, restraint reduction, early device removal, frequent mobilization, hearing and visual aids, and efforts to improve patient communication through assistive strategies) be implemented in the critical care setting. For example, a study30 of older patients with femoral neck fracture demonstrated that the application of comprehensive geriatric assessment, management, and rehabilitation decreased the number of days of postoperative delirium, decreased complications, and shortened length of hospitalization. Similar success has been demonstrated in the Hospitalized Elder Life Program.31
Despite the lack of randomized control trials in the ICU setting, there is clearly a need for evidence-based practices to be rigorously employed during the perioperative period. Practical interventions focused on optimal fluid and electrolyte management, nutrition, sleep, and mobility may help reduce delirium and its impact in the ICU.
Our investigation has several limitations. The inclusion of only older, English-speaking surgical patients recruited from a single institution limits generalizability of study findings. We are unable to establish a true “cause/effect” relationship between delirium and the selected outcomes; however, we do provide evidence of the negative effect of SICU delirium on important outcomes. The Katz ADL instrument was selected because of its wide use in the geriatric research literature; however, this instrument is limited by its relatively coarse measure of function. Using surrogates to obtain information regarding the subjects' preadmission health status, functional and cognitive ability, and living arrangements creates the possibility that the surrogates either overestimated or underestimated the older adults' actual status. As with many clinical research studies, the number of covariates measured and examined was limited. It is possible that other factors may impact older adults' short-term outcomes. For example, delirium is treated in diverse ways (ie, restraint/sedation/analgesic use), and these different methods of managing delirium have the potential to influence the outcome variables that were assessed. Finally, in our multivariable models SICU delirium was handled as a yes/no event. It is possible our results may have differed if delirium severity was measured or the time-varying aspect of this disorder was considered.
The strengths of this study include its prospective design, the frequency of delirium assessment, and the focus on older SICU patients, a population that had not been studied previously. The study is also strengthened by the use of a wide variety of valid and reliable tools to measure delirium, dementia, agitation and sedation, severity of illness, functional ability, and comorbidities.
In this study of older adults admitted to SICUs, complications were associated with increased incidence of delirium. Delirium significantly increased the likelihood that older adults would be discharged to a place providing higher levels of dependent care. The consequences of SICU delirium are costly from a resource, economic, and social perspective. Clinicians should routinely assess for delirium in the ICU and aggressively manage it. Further research is needed on how to better prepare elders for surgery, elucidate risk factors for delirium in the SICU, and prevent/treat delirium in the acute care setting.
Acknowledgments
This research was supported in part by a Building Academic Geriatric Nursing Capacity Hartford-Atlantic Postdoctoral Fellowship.
Abbreviations
- ADL
activities of daily living
- APACHE
acute physiology and chronic health evaluation
- CAM-ICU
Confusion Assessment Method for the ICU
- CCI
Charlson comorbidity index
- CI
confidence interval
- HHC
home health care
- IQCODE
Informant Questionnaire on Cognitive Decline in the Elderly
- SICU
surgical ICU
Footnotes
The study was conducted at the Hospital of the University of Pennsylvania, Philadelphia, PA.
The authors have no conflicts of interest to disclose.
References
- 1.Pandharipande P, Jackson J, Ely EW. Delirium: acute cognitive dysfunction in the critically ill. Curr Opin Crit Care. 2005;11:360–368. doi: 10.1097/01.ccx.0000170503.76528.4b. [DOI] [PubMed] [Google Scholar]
- 2.Balas MC, Deutschman CS, Sullivan-Marx EM, et al. Delirium in older patients in surgical intensive care units. J Nurs Scholar. 2007;39:147–154. doi: 10.1111/j.1547-5069.2007.00160.x. [DOI] [PubMed] [Google Scholar]
- 3.McNicoll L, Pisani MA, Zhang Y, et al. Delirium in the intensive care unit: occurrence and clinical course in older patients. J Am Geriatr Soc. 2003;51:591–598. doi: 10.1034/j.1600-0579.2003.00201.x. [DOI] [PubMed] [Google Scholar]
- 4.Pisani MA, Murphy TE, Van Ness, et al. Characteristics associated with delirium in older patients in a medical intensive care unit. Arch Intern Med. 2007;167:1629–1634. doi: 10.1001/archinte.167.15.1629. [DOI] [PubMed] [Google Scholar]
- 5.Milbrandt EB, Deppen S, Harrison PL, et al. Costs associated with delirium in mechanically ventilated patients. Crit Care Med. 2004;32:955–962. doi: 10.1097/01.ccm.0000119429.16055.92. [DOI] [PubMed] [Google Scholar]
- 6.Ouimet S, Kavanagh BP, Gottfried SB, et al. Incidence, risk factors and consequences of ICU delirium. Intensive Care Med. 2007;33:66–73. doi: 10.1007/s00134-006-0399-8. [DOI] [PubMed] [Google Scholar]
- 7.Thomason JW, Shintani A, Peterson JF, et al. Intensive care unit delirium is an independent predictor of longer hospital stay: a prospective analysis of 261 non-ventilated patients. Crit Care. 2005;9:375–381. doi: 10.1186/cc3729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ely EW, Gautam S, Margolin R, et al. The impact of delirium in the intensive care unit on hospital length of stay. Intensive Care Med. 2001;27:1892–1900. doi: 10.1007/s00134-001-1132-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Micek ST, Anand NJ, Laible BR, et al. Delirium as detected by the CAM-ICU predicts restraint use among mechanically ventilated medical patients. Crit Care Med. 2005;33:1260–1265. doi: 10.1097/01.ccm.0000164540.58515.bf. [DOI] [PubMed] [Google Scholar]
- 10.Dubois MJ, Bergeron N, Dumont M, et al. Delirium in an intensive care unit: a study of risk factors. Intensive Care Med. 2001;27:1297–1304. doi: 10.1007/s001340101017. [DOI] [PubMed] [Google Scholar]
- 11.Lin SM, Liu CY, Wang CH, et al. The impact of delirium on the survival of mechanically ventilated patients. Crit Care Med. 2004;32:2254–2259. doi: 10.1097/01.ccm.0000145587.16421.bb. [DOI] [PubMed] [Google Scholar]
- 12.Ely EW, Shintani A, Truman B, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291:1753–1762. doi: 10.1001/jama.291.14.1753. [DOI] [PubMed] [Google Scholar]
- 13.Fukuse T, Satoda N, Hijiya K, et al. Importance of a comprehensive geriatric assessment in prediction of complications following thoracic surgery in elderly patients. Chest. 2005;127:886–891. doi: 10.1378/chest.127.3.886. [DOI] [PubMed] [Google Scholar]
- 14.Pofahl WE, Pories WJ. Current status and future directions of geriatric general surgery. J Am Geriatr Soc. 2003;51:S351–354. doi: 10.1046/j.1365-2389.2003.51347.x. [DOI] [PubMed] [Google Scholar]
- 15.Angus DC, Kelley MA, Schmitz RJ, et al. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease: can we meet the requirements of an aging population? JAMA. 2000;284:2762–2770. doi: 10.1001/jama.284.21.2762. [DOI] [PubMed] [Google Scholar]
- 16.Katz S, Ford AB, Moskowitz RW. Studies of illness in the aged: the index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 17.Jorm AF. The Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE): a review. Int Psychogeriat. 2004;16:1–19. doi: 10.1017/s1041610204000390. [DOI] [PubMed] [Google Scholar]
- 18.Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–829. [PubMed] [Google Scholar]
- 19.Charlson ME, Pompei P, Ales KL. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 20.Sessler CN, Gosnell MS, Grap MJ, et al. The Richmond Agitation-Sedation Scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med. 2002;166:1338–1344. doi: 10.1164/rccm.2107138. [DOI] [PubMed] [Google Scholar]
- 21.Ely EW, Truman B, Shintani A, et al. Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation-Sedation Scale (RASS) JAMA. 2003;289:2983–2991. doi: 10.1001/jama.289.22.2983. [DOI] [PubMed] [Google Scholar]
- 22.Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU) JAMA. 2001;286:2703–2710. doi: 10.1001/jama.286.21.2703. [DOI] [PubMed] [Google Scholar]
- 23.Ely EW, Margolin R, Francis J, et al. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) Crit Care Med. 2001;29:1370–1379. doi: 10.1097/00003246-200107000-00012. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Medicare and Medicaid Services. [November 5, 2008]; Available at: http://www.cms.hhs.gov/HospitalAcqCond/06_Hospital-Acquired_Conditions.asp.
- 25.Francis J, Kapoor WN. Prognosis after hospital discharge of older medical patients with delirium. J Am Geriatr Soc. 1992;40:601–606. doi: 10.1111/j.1532-5415.1992.tb02111.x. [DOI] [PubMed] [Google Scholar]
- 26.O'Keeffe S, Lavan J. The prognostic significance of delirium in older hospital patients. J Am Geriatr Soc. 1997;45:174–178. doi: 10.1111/j.1532-5415.1997.tb04503.x. [DOI] [PubMed] [Google Scholar]
- 27.Murray AM, Levkoff SE, Wetle TT, et al. Acute delirium and functional decline in the hospitalized elderly patient. J Gerontol. 1993;48:M181–M186. doi: 10.1093/geronj/48.5.m181. [DOI] [PubMed] [Google Scholar]
- 28.Inouye SK, Rushing JT, Foreman MD, et al. Does delirium contribute to poor hospital outcomes? A three-site epidemiologic study. J Gen Intern Med. 1998;13:234–242. doi: 10.1046/j.1525-1497.1998.00073.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jacobi J, Fraser GL, Coursin DB, et al. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med. 2002;30:119–141. doi: 10.1097/00003246-200201000-00020. [DOI] [PubMed] [Google Scholar]
- 30.Lundstrom M, Olofsson B, Stnval M, et al. Postoperative delirium in old patients with femoral neck fracture: a randomized intervention study. Aging Clin Exp Res. 2007;19:178–186. doi: 10.1007/BF03324687. [DOI] [PubMed] [Google Scholar]
- 31.Inouye SK, Bogardus ST, Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340:669–676. doi: 10.1056/NEJM199903043400901. [DOI] [PubMed] [Google Scholar]


