Summary
Residential context has received increased attention as a possible contributing factor to race/ethnic and socioeconomic disparities in birth outcomes in the United States. Utilizing vital statistics birth record data, this study examined the association between neighbourhood deprivation and the risk of a term small-for-gestational-age (SGA) birth among non-Hispanic whites and non-Hispanic blacks in eight geographic areas: Baltimore City, Baltimore County, Montgomery County and Prince Georges County in Maryland, 16 pooled cities in Michigan, Durham County and Wake County in North Carolina, and Philadelphia, Pennsylvania. Multilevel random intercept logistic regression models were employed and statistical tests were performed to examine if the association between neighbourhood deprivation and SGA varied by race/ethnicity and study site. The risk of term SGA was higher among non-Hispanic blacks (range: 10.8%–17.5%) than non-Hispanic whites (range: 5.1%–9.2%) in all areas and it was higher in cities than in suburban locations. In all areas, non-Hispanic blacks lived in more deprived neighbourhoods than non-Hispanic whites. However, the adjusted associations between neighbourhood deprivation and term SGA did not vary significantly by race/ethnicity or study site. The summary fully-adjusted pooled odds ratios, indicating the effect of one standard deviation increase in the deprivation score, were 1.15 [95% CI: 1.08–1.22] for non-Hispanic whites and 1.09 [95% CI: 1.05–1.14] for non-Hispanic blacks. Thus, neighbourhood deprivation was weakly associated with term SGA among both non-Hispanic whites and non-Hispanic blacks.
Introduction
The failure of individual-level demographic, socioeconomic (SES), and behavioural factors to explain SES and race/ethnic disparities in health outcomes has focused increased attention on the possible role of residential context in generating these disparities.1–5 In the United States, residential context may be a particularly salient explanation for black-white differences in health due to large variations in residential environments between blacks and whites. African Americans regardless of their income are more likely than whites to live in neighbourhoods with higher rates of crime and violence, elevated levels of social disorder, and poor public and private services. 6–7 Thus, blacks are more likely to be exposed to stressful life circumstances and lack access to quality health care, opportunities for regular exercise, and healthy foods, factors that have been hypothesized to influence health outcomes.2–3
Recent U.S. studies have explored associations between neighbourhood economic deprivation,8–12 social organization,13–14 residential composition,10, 12–15 crime,8, 14, 16–17 and birthweight and/or preterm birth. In most studies, higher levels of neighbourhood deprivation and crime were associated with a higher risk of preterm birth and lower birthweight,8–14 while measures of neighbourhood level social cohesion were associated with higher birthweight, adjusting for individual-level attributes.13–14 Several authors also found that associations between neighbourhood characteristics and birth outcomes varied by race/ethnicity.9–11, 13, 18
Only a handful of studies have examined the association between neighbourhood context and small-for-gestational age (SGA) births.15, 19–20 These studies found that low neighbourhood-level household income is associated with an elevated risk of SGA in Louisiana19 and Quebec, Canada, 20 after adjustment for maternal characteristics. Additionally, African American women living in U.S. metropolitan statistical areas (MSA) with a higher level of residential segregation were more likely to deliver an SGA infant than other African American women, controlling for individual-level attributes and MSA-educational attainment and population size.15
We extend previous analyses of neighbourhood context and the risk of SGA among non-Hispanic white and non-Hispanic black women in the United States. We hypothesize that a higher level of neighbourhood deprivation would be associated with a higher risk of term SGA and that this association may be mediated by two known risk factors for SGA – maternal smoking and gestational and/or chronic hypertension.21–23 We further speculate that the association between neighbourhood deprivation and SGA may vary by race/ethnicity, and explore if the strength of the association between neighbourhood deprivation and SGA varied in different regions, urban areas, and suburban locations.
Methods
The analysis was conducted as part of the ‘Multilevel Modelling of Disparities to Explain Preterm Delivery (MODE-PTD)’ project, a partnership among four universities and their state or local health departments. Eight geographic areas are represented in the analyses, of which three are large urban centres – Philadelphia, Pennsylvania (PA), Baltimore City, Maryland (MD) and 16 combined cities in Michigan (MI). The other sites include three suburban counties in Maryland (Baltimore County, Montgomery County, and Prince George County) and two counties in North Carolina (Durham County and Wake County). We analyzed the large urban centres and the suburban counties separately to examine whether the association between neighbourhood deprivation and SGA was similar in different geographic regions with substantial variation in levels of poverty and percentage of white residents.24
Individual-level data on birth outcomes and maternal characteristics came from vital records obtained from each site’s governmental partner. The period covered by the analyses varied by site due to data availability and interest of the governmental partner, but in all sites the data covered some years between 1995 and 2001. The birth records were geocoded based on the maternal address given on the birth certificate to identify the mothers’ residential census tract with a minimum of 95% match rate for each area. Maternal age, maternal education, whether the mother smoked during pregnancy, and whether the mother had gestational and/or chronic hypertension were included as individual-level explanatory variables. Less than five percent of the records had missing data on these variables, except in two Maryland sites, Montgomery County and Prince Georges County, where information on smoking was missing for 19% and 8% of non-Hispanic white births and 10% and 28% of non-Hispanic black births, respectively. Births with missing information were excluded.
Small for gestational age (SGA) birth
To identify births as SGA, a newborn weighting less than the 10th percentile of the birthweight distribution for a given gestational week,25 we developed reference curves based on vital statistics data for singleton births born to US resident mothers in the 50 states and the District of Columbia in 1998, 1999, and 2000. Sex-specific reference curves for SGA cut points indicating the 10th percentile in the birthweight distribution for gestational ages 20–44 weeks were developed for first births and second or higher order births. In constructing the SGA cut points, births with extreme deviation from the mean birthweight for a given gestational week were excluded so that the established cut points were not influenced by extreme outliers. We identified outliers as births that fell outside the interquartile range of the birthweight distribution for a given gestational week.26 Approximately 1.5% of births were excluded in the construction of the standard.
The sex- and parity-specific SGA cut points were applied to site-specific birth record data to classify births as SGA. We focus the analyses on singleton term births (37–44 weeks gestation). Because the vast majority of SGA births occur at term27 and black-white differences in SGA are most pronounced among infants delivered at term,28 the removal of preterm births does not affect our conclusions.
Neighbourhood-level deprivation
We used census tracts to define neighbourhoods, a commonly used aerial unit in the neighbourhood effects literature.8, 10, 19, 29 To characterize neighbourhoods by their level of deprivation, we employed a neighbourhood-level deprivation index described elsewhere.30 In brief, this index utilizes data from five domains of social and economic disadvantage available in the 2000 U.S. Census of Population: income/poverty, employment, education, housing, and occupation. The deprivation index was created by principal components analysis utilizing pooled tract-level data from all eight study areas with the first principal component making up the deprivation index. The component loadings were consistent across study sites with the first principal component accounting for 51%–73% of the total variance in all eight areas.30 The standardized index, with a mean zero and a standard deviation of one, was linked to site-specific birth record data by census tract. Smaller values of the deprivation index indicate lower levels of neighbourhood disadvantage.
Statistical methods
To examine the association between neighbourhood-level deprivation and the risk of term SGA, we estimated three race-specific multi-level random-intercept logistic regression models for each study site. Census tracts were used as surrogates for neighbourhoods, so that a unique random effect was estimated for the baseline log-odds of SGA in each tract (Table 1). Our first model included only the neighbourhood deprivation index and described the unadjusted associations between term SGA and neighbourhood deprivation. In Model 2, we included maternal age and education, and in Model, 3 we introduced smoking and gestational and chronic hypertension. Neighbourhood-level deprivation was modelled as a linear term; alternative specifications of the deprivation index (e.g., quadratic, logarithmic transformation) did not improve model fit. Because neighbourhood context has been linked to health behaviours, such as smoking,31–32 and to chronic disease,33 we hypothesized that the effects of neighbourhood deprivation on term SGA operate at least in part through maternal health and health behaviours. Maternal education served as an indicator of individual-level SES. Data on household income are not available on the birth certificate.
Table 1.
Individual-level maternal characteristics, % SGA of term births, and neighbourhood-level deprivation scores for Non-Hispanic White and Non-Hispanic Black women for 8 areas, 1995–2001
| Characteristic | Baltimore City, MD | Baltimore County, MD | Montgomery County, MD | Prince Georges County, MD | 16 Cities, MI | Durham County, NC | Wake County, NC | Philadelphia, PA |
|---|---|---|---|---|---|---|---|---|
| Years | 1999–2001 | 1999–2001 | 1999–2001 | 1999–2001 | 1995–1999 | 1999–2001 | 1999–2001 | 1999–2000 |
| Total term births (no.) | 20,158 | 15,585 | 14,878 | 14,179 | 74,947 | 7,226 | 21,519 | 27,385 |
| Non-Hispanic White (#, %) | 5,131 (25%) | 11,603 (74%) | 10,905 (73%) | 3,609 (25%) | 28,809 (38%) | 3,532 (49%) | 16,236 (75%) | 10,874 (40%) |
| Non-Hispanic Black (#, %) | 15,027 (75%) | 3,982 (26%) | 3,973 (27%) | 10,570 (75%) | 46,138 (62%) | 3,694 (51%) | 5,283 (25%) | 16,511 (60%) |
| INDIVIDUAL LEVEL |
NON-HISPANIC WHITES |
|||||||
| Maternal Age in years (%) | ||||||||
| < 18 | 3.7 | 2.1 | 0.7 | 2.2 | 4.1 | 1.0 | 0.8 | 2.7 |
| 18–19 | 6.9 | 4.3 | 1.5 | 4.5 | 8.3 | 2.6 | 1.9 | 6.0 |
| 20–24 | 22.7 | 15.7 | 6.6 | 19.7 | 27.8 | 11.3 | 10.5 | 20.6 |
| 25–29 | 23.7 | 26.1 | 19.4 | 24.5 | 30.3 | 28.5 | 27.0 | 28.9 |
| 30–34 | 25.9 | 32.1 | 39.7 | 28.4 | 20.1 | 36.3 | 38.2 | 26.6 |
| 35+ | 17.1 | 19.7 | 32.1 | 20.8 | 9.5 | 20.4 | 21.6 | 15.2 |
| Maternal Education (%) | ||||||||
| < 20 years & < High school | 7.5 | 3.1 | 1.0 | 3.0 | 8.6 | 2.4 | 2.7 | 4.8 |
| ≥ 20 years & < High school | 13.5 | 5.3 | 2.4 | 5.4 | 15.6 | 4.2 | 6.6 | 8.1 |
| High school or equiv | 25.0 | 28.9 | 12.1 | 29.3 | 33.2 | 12.6 | 15.1 | 38.6 |
| > High school | 54.0 | 62.7 | 84.5 | 62.3 | 42.7 | 80.8 | 75.6 | 48.4 |
| Mother smoked during pregnancy (%) | 17.5 | 11.4 | 3.6 | 10.8 | 21.2 | 4.9 | 5.2 | 19.9 |
| Mothers with gestational and/or chronic hypertension (%) | 2.5 | 3.6 | 2.4 | 3.2 | 2.9 | 5.3 | 3.9 | 3.5 |
| SGA Term Births (%) | 8.7 | 7.2 | 5.7 | 6.7 | 9.2 | 5.1 | 5.6 | 7.9 |
| NEIGHBOURHOOD LEVEL | ||||||||
| Census tracts (no.) | 168 | 165 | 156 | 136 | 558 | 51 | 105 | 329 |
| Neighbourhood Deprivation Score – | ||||||||
| Median | −0.3 | −0.8 | −1.2 | −0.9 | 0.1 | −1.1 | −1.1 | −0.3 |
| 25% | −0.6 | −1.1 | −1.4 | −1.1 | −0.6 | −1.2 | −1.4 | −0.6 |
| 75% | 0.1 | −0.5 | −0.8 | −0.7 | 0.7 | −0.6 | −0.9 | 0.1 |
| Minimum value | −1.3 | −1.6 | −1.7 | −1.4 | −1.7 | −1.6 | −1.9 | −1.8 |
| Maximum value | 2.6 | 1.6 | 0.7 | 0.7 | 3.7 | 2.5 | 2.6 | 3.7 |
| INDIVIDUAL LEVEL |
NON-HISPANIC BLACKS |
|||||||
| Maternal Age in years (%) | ||||||||
| < 18 | 11.9 | 4.8 | 2.9 | 4.5 | 10.1 | 6.0 | 5.0 | 9.5 |
| 18–19 | 15.4 | 8.1 | 4.6 | 7.5 | 13.2 | 9.8 | 8.2 | 12.1 |
| 20–24 | 33.1 | 26.9 | 17.6 | 23.1 | 32.9 | 30.8 | 29.0 | 32.9 |
| 25–29 | 20.1 | 27.3 | 25.0 | 25.2 | 23.8 | 25.7 | 26.2 | 22.2 |
| 30–34 | 12.1 | 21.1 | 28.2 | 23.8 | 13.2 | 18.8 | 19.9 | 14.4 |
| 35+ | 7.4 | 11.9 | 21.7 | 15.9 | 6.8 | 9.0 | 11.7 | 8.8 |
|
NON-HISPANIC BLACK WOMEN |
||||||||
| Maternal Education (%) | ||||||||
| < 20 years & < High school | 16.5 | 5.2 | 3.1 | 5.3 | 15.6 | 10.5 | 6.4 | 12.5 |
| ≥ 20 years & < High school | 17.3 | 5.4 | 5.1 | 5.3 | 17.9 | 13.4 | 15.3 | 14.3 |
| High school or equiv | 42.2 | 35.4 | 30.8 | 37.5 | 37.3 | 28.7 | 23.1 | 42.9 |
| > High school | 24.1 | 54.1 | 61.0 | 51.9 | 29.3 | 47.5 | 55.2 | 30.4 |
| Mother smoked during pregnancy (%) | 11.9 | 4.5 | 3.3 | 3.4 | 14.5 | 7.7 | 8.0 | 12.0 |
| Mothers with pregnancy related and/or chronic hypertension (%) | 3.2 | 4.5 | 3.8 | 4.0 | 3.0 | 5.6 | 5.0 | 4.7 |
| SGA Term Births (%) | 17.2 | 13.2 | 10.8 | 14.5 | 17.5 | 14.8 | 14.4 | 16.0 |
| NEIGHBOURHOOD LEVEL | ||||||||
| Census tracts (no.) | 91 | 43 | 42 | 68 | 592 | 51 | 103 | 340 |
| Neighbourhood Deprivation Score – | ||||||||
| Median | 0.7 | −0.5 | −0.8 | −0.4 | 0.9 | −0.0 | −0.7 | 0.9 |
| 25% | 0.1 | −0.7 | −1.1 | −0.8 | 0.3 | −0.7 | −1.0 | 0.3 |
| 75% | 1.2 | −0.4 | −0.2 | 0.1 | 1.4 | 0.9 | −0.1 | 1.3 |
| Minimum value | −1.3 | −1.6 | −1.6 | −1.4 | −1.7 | −1.6 | −1.8 | −1.5 |
| Maximum value | 2.6 | 1.2 | 0.7 | 1.1 | 3.7 | 2.5 | 2.6 | 3.7 |
To investigate whether effects of neighbourhood deprivation varied by race/ethnicity, the data were pooled within each site and interaction terms between race/ethnicity and the deprivation index were tested for significant differences. To test whether our findings can be generalized across a wide range of neighbourhood deprivation levels, we took the estimated slope coefficients for neighbourhood deprivation from the eight sites, and calculated a homogeneity test statistic, Cochran’s Q, to test whether the site-specific slope coefficients were homogenous across all sites.34 This random-effects summary estimate of the eight site-specific slope coefficients assumes a “population of populations,” each with its own slope. The statistical model further assumes that these population slopes are normally distributed and that a random sample of these populations was included in our study.34 The models were estimated with STATA35 in three sites (MD, NC & PA) and with Hierarchical Linear and Nonlinear Modelling (HLM)36 in one site (MI).
Results
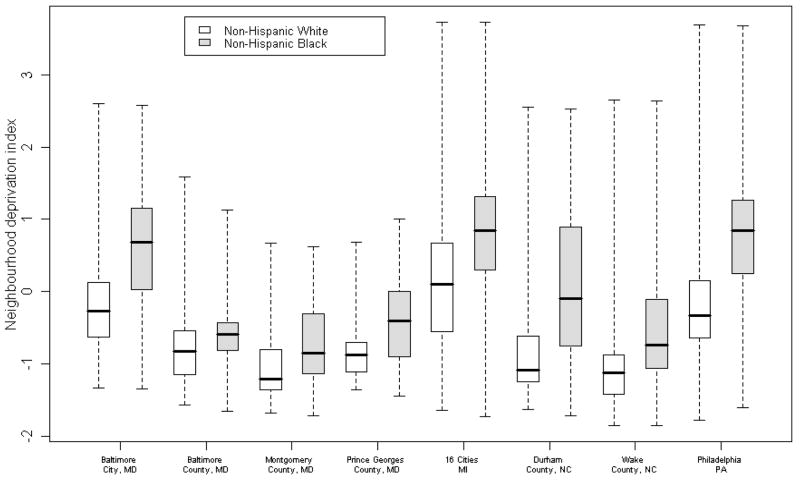
The percentage of non-Hispanic white and non-Hispanic black term births born SGA varied considerably among the study sites as did the level of neighbourhood deprivation (Table 1 and Figure 1). Non-Hispanic black mothers delivering at term lived in more deprived census tracts than their non-Hispanic white counterparts in all study sites , and their infants were close to or more than twice as likely to be born SGA as infants of non-Hispanic white mothers.
Figure 1.
Distribution of neighborhood deprivation scores by race/ethnicity and study site
Table 2 shows the results of the regression analyses, where the odds ratios for neighbourhood deprivation represent the effect of one standard deviation increase in the deprivation score on the risk of term SGA. The unadjusted positive association between neighbourhood deprivation and term SGA was substantially attenuated with adjustment for maternal age and education, with reductions ranging from 40% to 66% for non-Hispanic whites and from 7% to 81% for non-Hispanic blacks. The inclusion of maternal smoking and gestational and/or chronic hypertension resulted in small additional reductions in the odds ratios in most sites. In the fully adjusted model, the odds ratios for neighbourhood deprivation among non-Hispanic whites ranged from 0.92 [95% CI: 0.74, 1.13] in Montgomery County, MD to 1.44 [95% CI: 1.06, 1.96] in Prince Georges County, MD, and for non-Hispanic blacks from 1.00 [95% CI: 0:90, 1.11] in Durham County, NC to 1.16 [95% CI: 1.04, 1.29] in Prince Georges County, MD.
Table 2.
Estimated odds ratios for the effect of neighbourhood deprivation score (and 95% confidence intervals) on SGA term births for Non-Hispanic White and Non-Hispanic Black women for 8 areas, 1995–2001a
| Study Site | Non-Hispanic Whites | Non-Hispanic Blacks | ||||
|---|---|---|---|---|---|---|
| Unadjusted | Adjusted for Maternal Age & Education | Adjusted for Maternal Age, Education, Smoking & Hypertension | Unadjusted | Adjusted for Maternal Age & Education | Adjusted for Maternal Age, Education, Smoking & Hypertension | |
| Baltimore City, MD | 1.45 [1.25–1.70] | 1.24 [1.04–1.47] | 1.15 [0.96–1.38] | 1.16 [1.10–1.23] | 1.09 [1.02–1.15] | 1.06 [1.00–1.12] |
| Baltimore County, MD | 1.68 [1.43–1.98] | 1.23 [1.01–1.48] | 1.08 [0.89–1.30] | 1.15 [0.89–1.47] | 1.11 [0.86–1.43] | 1.07 [0.83–1.38] |
| Montgomery County, MD | 1.04 [0.85–1.28] | 0.94 [0.76–1.16] | 0.92 [0.74–1.13] | 1.19 [0.97–1.46] | 1.14 [0.93–1.40] | 1.15 [0.94–1.42] |
| Prince Georges County, MD | 1.65 [1.24–2.1.9] | 1.39 [1.03–1.88] | 1.44 [1.06–1.96] | 1.30 [1.17–1.44] | 1.17 [1.05–1.30] | 1.16 [1.04–1.29] |
| 16 Cities, MI | 1.42 [1.33–1.51] | 1.24 [1.16–1.33] | 1.20 [1.12–1.28] | 1.24 [1.20–1.29] | 1.18 [1.14–1.22] | 1.15 [1.11–1.19] |
| Durham County, NC | 1.22 [0.92–1.62] | 1.08 [0.80–1.47] | 1.07 [0.80–1.45] | 1.16 [1.06–1.27] | 1.03 [0.93–1.15] | 1.00 [0.90–1.11] |
| Wake County, NC | 1.26 [1.07–1.49] | 1.14 [0.96–1.37] | 1.09 [0.90–1.31] | 1.14 [1.02–1.28] | 1.13 [1.01–1.28] | 1.05 [0.95–1.15] |
| Philadelphia, PA | 1.40 [1.29–1.52] | 1.24 [1.13–1.36] | 1.19 [1.08–1.30] | 1.17 [1.11–1.24] | 1.12 [1.05–1.18] | 1.08 [1.02–1.15] |
| Pooled Estimate | 1.39 [1.28–1.50] | 1.21 [1.15–1.28] | 1.15 [1.08–1.22] | 1.20 [1.16–1.23] | 1.13 [1.09–1.17] | 1.09 [1.05–1.14] |
Note: Years vary by site: Maryland: 1999–2001; Michigan: 1995–1999; North Carolina: 1999–2001; Pennsylvania: 1999–2000.
Based on the homogeneity test statistic, Cochran’s Q, we concluded that the association between neighbourhood deprivation and SGA did not differ significantly among the study areas in all models for non-Hispanic blacks (Model 1: p=0.273; Model 2: p=0.204; Model 3: p=0.078) and in models 2 and 3 for non-Hispanic whites (Model 2: p=0.334; Model 3: p=0.242). Excluding Montgomery County, MD from the test in Model 1, where the association between neighbourhood deprivation and SGA among non-Hispanic whites was weak, the Cochran Q statistic for non-Hispanic whites was no longer statistically significant (p=0.225), indicating homogeneity in the effects of neighbourhood deprivation in all other sites. In the fully adjusted model, the pooled odds ratio, representing the effect of one standard deviation increase in the deprivation score, was 1.15 [95% CI: 1.08, 1.22] for non-Hispanic whites and 1.09 [95% CI: 1.05, 1.14] for non-Hispanic blacks.
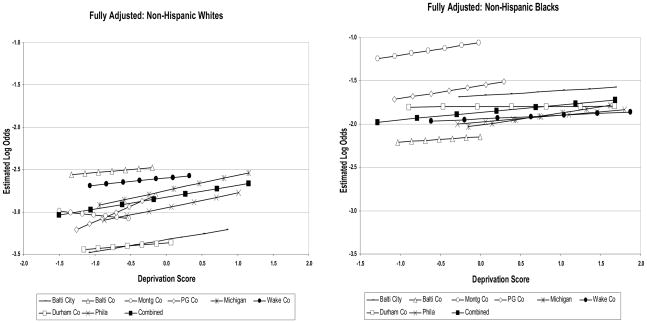
Figure 2 plots the site-specific and pooled fully adjusted estimates of the effect of neighbourhood deprivation on term SGA. Although the slope estimates appear to be somewhat steeper for non-Hispanic whites than non-Hispanic blacks, we found the interaction term between race/ethnicity and neighbourhood deprivation to be insignificant in the adjusted models in all sites. These results are also reflected in the fully adjusted pooled estimates where the confidence intervals for the effect of neighbourhood deprivation overlap for non-Hispanic whites and non-Hispanic blacks. What is also evident is that controlling for neighbourhood deprivation, as measured in this study, does not eliminate the race disparity in term SGA (Figure 2).
Figure 2.
Estimated log-odds of SGA term birth by level of neighbourhood deprivation and study site (adjusted for maternal age, education, smoking and hypertension)
Note: Plotted for reference category: age 20–24, above high school education, non-smoker, and no hypertension.
Discussion
The purpose of this paper was to investigate the association between neighbourhood deprivation and the risk of term SGA among non-Hispanic whites and non-Hispanic blacks in eight geographic areas in the United States. The risk of term SGA varied among study areas with the risk being greatest in cities. Independent of this variability, across all geographic areas, the risk of term SGA was two to two and a half times higher among non-Hispanic blacks than non-Hispanic whites. Neighbourhood deprivation had a positive unadjusted association with term SGA for both non-Hispanic whites and non-Hispanic blacks, but it was substantially reduced with adjustment for maternal age and education, smoking and hypertension. The fully adjusted odds ratios, representing one standard deviation increase in the deprivation score, ranged from 0.92 to 1.44 for non-Hispanic whites and from 1.00 to 1.16 for non-Hispanic blacks. However, the Cochran’s Q homogeneity test revealed that the adjusted associations between neighbourhood deprivation and the risk of term SGA did not differ significantly across the eight areas. When pooled across study sites, the fully adjusted odds ratio for neighbourhood deprivation was 1.15 for non-Hispanic whites and 1.09 for non-Hispanic blacks. These results are similar to findings in Canada and Louisiana where neighbourhood-level household income also predicted fetal growth.19–20
We did not find a significant interaction between race/ethnicity and neighbourhood deprivation on the risk of term SGA. This finding is contradictory to some previously published studies that explored similar interactions on the risk of other adverse birth outcomes.9, 18, 37 These inconsistencies may reflect differences in study designs, including operational definitions of neighbourhood context, outcomes of interest, and adjustment for individual-level characteristics.
The mechanisms through which neighbourhood context have been hypothesized to influence birth outcomes, including SGA, include features of the neighbourhood’s social and service environment, and physical characteristics.2–3, 5 The concentration of adverse neighbourhood conditions along the above dimensions is often closely tied to the clustering of socioeconomic disadvantage. Thus, living in disadvantaged neighbourhoods may expose women to multiple adverse social and physical elements, including crime and violence, weak social networks and limited access to health promoting resources that may contribute to increased risk of poor pregnancy outcomes. Potentially, adverse neighbourhood conditions exert influence on health via increased likelihood of adverse health behaviours, as suggested by findings from prior research.31–32 However, we found that adjustment for smoking during pregnancy and gestational and/or chronic hypertension did not substantially modify the association between neighbourhood deprivation and the risk of term SGA, suggesting that other factors, such as exposure to chronic stress, may play a role. Recent empirical evidence, based on studies of pregnant women of different race/ethnic, SES, and cultural backgrounds, supports the premise that women experiencing high levels of psychological or social stress during pregnancy are at a significantly increased risk for preterm birth, even after adjustment for other biomedical, socio-demographic, and behavioural risk factors.38–41 Less is known about the association between exposure to chronic and acute stress and the risk of SGA, an area that merits further investigation.42
Although neighbourhood deprivation was a significant predictor of the risk of term SGA, we could not explain the higher risk of term SGA among non-Hispanic blacks than non-Hispanic whites by controlling for neighbourhood deprivation. Our measure of neighbourhood conditions was limited to a summary index of neighbourhood-level SES and thus it does not fully capture all neighbourhood-level attributes that may be important. In fact, the relatively small effects and somewhat inconsistent associations between neighbourhood context, race/ethnicity and birth outcomes in multi-level studies published to date are likely to be related to limitations in commonly used measures of neighbourhood context, which most often have been based on census data. Furthermore, neighbourhood context is only one of many social contexts (e.g., family, work) that may influence women’s birth outcomes. The inclusion of multiple social contexts, however, has been limited by lack of available data.
One of the strengths of these analyses is our ability to compare findings across diverse geographic areas. By using identical methodology and a common measure of neighbourhood deprivation, we were able to demonstrate that the association between neighbourhood deprivation and the risk of term SGA was similar across geographic areas with a wide range of socioeconomic profiles. In addition, our classification of term births as SGA was based on newly developed national reference curves.
The findings are also subject to several limitations. First, we are limited by the information available on the birth certificate. In particular, we must rely on maternal education to capture individual-level SES and thus it is possible that our neighbourhood-level deprivation index captures at least a part of the association between maternal income and the risk of term SGA. Adjustment for maternal age and education substantially attenuated the association between neighbourhood deprivation and the risk of term SGA. On the other hand, adjustment for smoking and hypertension resulted only in minor changes in the estimated odds ratios of neighbourhood deprivation. This result needs to be interpreted with some caution because of possible bias in the reporting of smoking and hypertension on the birth certificate. In addition, our estimates are based on cross-sectional data and the birth certificate has no information on the mother’s tenure in the address recorded on the birth certificate. Furthermore, we used census tracts to define neighbourhood boundaries. Some studies of neighbourhood effects have used census block groups9, 17 or alternative neighbourhood boundaries.13–14 A recent study that compared the association between census tract and block group level measures of socioeconomic status and rates of low birthweight, childhood lead poisoning, and mortality concluded that census tract and block group level measures led to similar conclusions, while larger units such as zip code areas, were thought to be less appropriate.43 Finally, we are limited in our interpretation because we cannot assess why some foetuses with growth restriction are delivered at term and others are delivered preterm. Thus, women with growth restricted foetuses that might have gone to term and would therefore have been a part of the analyses are excluded because of a medical decision to deliver early. If these medical decisions are influenced by maternal race/ethnicity and/or other characteristics, our results may be biased.
The findings of our study are consistent with previous research that has documented an inverse association between neighbourhood-level SES and preterm birth, low birthweight, and SGA.8–12, 19–20 That neighbourhood-level economic disadvantage is associated with multiple measures of adverse birth outcomes points to the need to further explore the mechanisms through which neighbourhood deprivation is associated with maternal and infant health. Although better data with more comprehensive measures of maternal characteristics, including SES, are needed before causal inferences can be drawn, this study together with previous literature suggests that residential context may play a role in generating race/ethnic and SES disparities in birth outcomes.
Acknowledgments
The Maternal and Child Health Bureau, Health Resources and Services Administration, Department of Health and Human Services funded this study. We thank Michael Kogan and Mary Kay Kenney for their support and the referees for their helpful comments.
References
- 1.Diez-Roux AV. Multilevel analysis in public health research. Annual Review of Public Health. 2000;21:171–192. doi: 10.1146/annurev.publhealth.21.1.171. [DOI] [PubMed] [Google Scholar]
- 2.Robert SA. Socioeconomic position and health: The independent contribution of community socioeconomic context. Annual Review of Sociology. 1999;25:489–516. [Google Scholar]
- 3.Kawachi I, Berkman LF. Neighbourhoods and health. New York: Oxford University Press; 2003. [Google Scholar]
- 4.Morenoff JD, Lynch JW. What makes a place healthy? Neighbourhood influences on racial/ethnic disparities in health over the life course. In: Anderson NB, Bulatao RA, Cohen B, editors. Critical perspectives on racial and ethnic differences in health in late life. Washington DC: The National Academies Press; 2004. pp. 406–449. [Google Scholar]
- 5.Culhane JF, Elo IT. Neighbourhood context and reproductive health. American Journal of Obstetrics and Gynecology. 2005;192(Supplement 1):S22–S29. doi: 10.1016/j.ajog.2005.01.071. [DOI] [PubMed] [Google Scholar]
- 6.Jargowsky PA. Poverty and place: Ghettos, barrios and the American city. New York: Russell Sage Foundation; 1996. [Google Scholar]
- 7.Massey DS, Denton NA. American apartheid: segregation and the making of the underclass. Boston: Harvard University Press; 1993. [Google Scholar]
- 8.O’Campo P, Xue X, Wang MC, Caughy M. Neighbourhood risk factors for low birthweight in Baltimore: a multilevel analysis. American Journal of Public Health. 1997;87:1113–1118. doi: 10.2105/ajph.87.7.1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pearl M, Braveman P, Abrams B. The relationship of neighbourhood socioeconomic characteristics to birthweight among 5 ethnic groups in California. American Journal of Public Health. 2001;91:1808–1814. doi: 10.2105/ajph.91.11.1808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pickett KE, Ahern JE, Selvin S, Abrams B. Neighbourhood socioeconomic status, maternal race, and preterm delivery: A case-control study. Annals of Epidemiology. 2002;12:410–418. doi: 10.1016/s1047-2797(01)00249-6. [DOI] [PubMed] [Google Scholar]
- 11.Reagan PB, Salsberry PJ. Race and ethnic differences in determinants of preterm birth in the USA: Broadening the social context. Social Science and Medicine. 2005;60:2217–2228. doi: 10.1016/j.socscimed.2004.10.010. [DOI] [PubMed] [Google Scholar]
- 12.Roberts EM. Neighbourhood social environments and the distribution of low birthweight in Chicago. American Journal of Public Health. 1997;87:597–603. doi: 10.2105/ajph.87.4.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buka SL, Brennan RT, Rich-Edwards JW, Raudenbush SW, Earls F. Neighbourhood support and the birthweight of urban infants. American Journal of Epidemiology. 2003;157:1–8. doi: 10.1093/aje/kwf170. [DOI] [PubMed] [Google Scholar]
- 14.Morenoff JD. Neighbourhood mechanisms and the spatial dynamics of birthweight. American Journal of Sociology. 2003;108:976–1017. doi: 10.1086/374405. [DOI] [PubMed] [Google Scholar]
- 15.Bell JF, Zimmerman FJ, Almgren GR, Mayer JD, Huebner CE. Birth outcomes among urban African-American women: A multilevel analysis of the role of racial residential segregation. Social Science and Medicine. 2006;63:3030–3045. doi: 10.1016/j.socscimed.2006.08.011. [DOI] [PubMed] [Google Scholar]
- 16.Collins JW, David RJ. Urban violence and African-American pregnancy outcome: an ecologic study. Ethnicity and Disease. 1997;7:184–190. [PubMed] [Google Scholar]
- 17.Messer LC, Kaufman JS, Dole N, Savitz DA, Laraia BA. Neighbourhood crime, deprivation and preterm birth. Annals of Epidemiology. 2006;16:455–462. doi: 10.1016/j.annepidem.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 18.Gorman BK. Racial and ethnic variation in low birthweight in the United States: individual and contextual determinants. Health and Place. 1999;5:195–207. doi: 10.1016/s1353-8292(99)00009-x. [DOI] [PubMed] [Google Scholar]
- 19.Farley TA, Mason K, Rice J, Habel JD, Scribner R, Cohen DA. The relationship between the neighbourhood environment and adverse birth outcomes. Paediatric and Perinatal Epidemiology. 2006;20:188–200. doi: 10.1111/j.1365-3016.2006.00719.x. [DOI] [PubMed] [Google Scholar]
- 20.Luo Z, Wilkins R, Kramer MS. Effect of neighbourhood income and maternal education on birth outcomes: a population-based study. Canadian Medical Association Journal. 2006;174:1415–1421. doi: 10.1503/cmaj.051096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Frisbie WP, Biegler M, de Turk P, Forbes D, Pullum SG. Racial and ethnic differences in determinants of intrauterine growth retardation and other compromised birth outcomes. American Journal of Public Health. 1997;87:1977–1983. doi: 10.2105/ajph.87.12.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kramer MS. Determinants of low birth weight: methodological assessment and meta-analysis. Bulletin of the World Health Organanization. 1987;65:663–737. [PMC free article] [PubMed] [Google Scholar]
- 23.Savitz DA, Dole N, Terry JW, Jr, Zhou H, Thorp JM., Jr Smoking and pregnancy outcome among African-American and White women in Central North Carolina. Epidemiology. 2001;12:636–642. doi: 10.1097/00001648-200111000-00010. [DOI] [PubMed] [Google Scholar]
- 24.The 2000 Census of Population, Census 2000 Summary File 3 (SF3) – Sample data. http://factfinder.census.gov.
- 25.Alexander GR, Himes JH, Kaufman RB, Mor J, Kogan M. A United States national reference for fetal growth. Obstetrics & Gynecology. 1996;87:163–168. doi: 10.1016/0029-7844(95)00386-X. [DOI] [PubMed] [Google Scholar]
- 26.Tukey JW. Exploratory data analysis. Reading: Addison Wesley; 1977. [Google Scholar]
- 27.Wilcox AJ. On the importance--and the unimportance-- of birthweight. International Journal of Epidemiology. 2001;30:1233–1241. doi: 10.1093/ije/30.6.1233. [DOI] [PubMed] [Google Scholar]
- 28.Salihu HM, Fitzpatrick L, Aliyu MH. Racial disparity in foetal growth inhibition among singletons and multiples. American Journal of Obstetrics and Gynecology. 2005;193:467–474. doi: 10.1016/j.ajog.2004.12.013. [DOI] [PubMed] [Google Scholar]
- 29.Krieger N, Chen JT, Waterman PD, Soobader M, Subramanian SV, Carson R. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: Does the choice of area-based measure and geographic level matter? American Journal of Epidemiology. 2002;156:471–482. doi: 10.1093/aje/kwf068. [DOI] [PubMed] [Google Scholar]
- 30.Messer LC, Laraia BA, Kaufman JS, Eyster J, Holzman C, Culhane J, et al. The development of a standardized neighbourhood deprivation index. Journal of Urban Health. 2006;83:1041–1062. doi: 10.1007/s11524-006-9094-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Duncan C, Jones K, Moon G. Smoking and deprivation: are there neighbourhood effects? Social Science and Medicine. 1999;48:497–505. doi: 10.1016/s0277-9536(98)00360-8. [DOI] [PubMed] [Google Scholar]
- 32.Duncan C, Jones K, Moon G. Health-Related behaviour in context: A multilevel modelling approach. Social Science and Medicine. 1996;42:817–830. doi: 10.1016/0277-9536(95)00181-6. [DOI] [PubMed] [Google Scholar]
- 33.Diez Roux AV, Merkin SS, Arnett D, Chambless L, Massing M, Nieto FJ, et al. Neighbourhood of residence and incidence of coronary heart disease. New England Journal of Medicine. 2001;345:99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- 34.Egger M, Davey Smith G, Altman DG. Systematic reviews in health care: meta-analysis in context. London, United Kingdom: BMJ Books; 2001. Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis; pp. 285–312. [Google Scholar]
- 35.Stata Corporation. Stata. College Station, TX: Stata Corporation; 2006. [Google Scholar]
- 36.Scientific Software International. HLM. Lincolnwood, IL: Scientific Software International; 2006. [Google Scholar]
- 37.Kaufman JS, Dole N, Savitz DA, Herring AH. Modelling community-level effects on preterm birth. Annals of Epidemiology. 2003;13:377–384. doi: 10.1016/s1047-2797(02)00480-5. [DOI] [PubMed] [Google Scholar]
- 38.Hedegaard M, Henriksen TB, Sabroe S, Secher NJ. Psychological distress in pregnancy and preterm delivery. British Medical Journal. 1993;307:234–39. doi: 10.1136/bmj.307.6898.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Copper RL, Goldenberg RL, Das A, Elder N, Swain M, Norman G, et al. The preterm prediction study: maternal stress is associated with spontaneous preterm birth at less than thirty-five weeks gestation. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. American Journal of Obstetrics and Gynecology. 1996;175:1286–92. doi: 10.1016/s0002-9378(96)70042-x. [DOI] [PubMed] [Google Scholar]
- 40.Killingsworth-Rini C, Dunkel-Schetter C, Wadhwa PD, Sandman CA. Psychological adaptation and birth outcomes: the role of personal resources, stress and sociocultural context during pregnancy. Health Psychology. 1999;18:333–45. doi: 10.1037//0278-6133.18.4.333. [DOI] [PubMed] [Google Scholar]
- 41.Wadhwa PD, Culhane JF, Rauh VA, Barve SS, Hogan VK, Sandman CA, et al. Stress, infection and preterm birth: A biobehavioral perspective. Paediatric and Perinatal Epidemiology. 2001;15(Supplement 2):17–29. doi: 10.1046/j.1365-3016.2001.00005.x. [DOI] [PubMed] [Google Scholar]
- 42.Cliver SP, Glodenberg RL, Cutter GR, Hoffman HJ, Copper RL, Gotlieb SJ, et al. The relationships among psychosocial profile, maternal size, and smoking in predicting fetal growth retardation. Obstetrics and Gynecology. 1992;80:262–7. [PubMed] [Google Scholar]
- 43.Krieger N, Chen JT, Waterman PD, Soobader M-J, Subramanian SV, Carson R. Choosing area based socioeconomic measures to monitor social inequalities in low birth weight and childhood lead poisoning: the Public Health Disparities Geocoding Project (US) Journal of Epidemiology and Community Health. 2003;57:186–99. doi: 10.1136/jech.57.3.186. [DOI] [PMC free article] [PubMed] [Google Scholar]