Abstract
This study examined the impact of heat acclimation on improving exercise performance in cool and hot environments. Twelve trained cyclists performed tests of maximal aerobic power (V̇o2max), time-trial performance, and lactate threshold, in both cool [13°C, 30% relative humidity (RH)] and hot (38°C, 30% RH) environments before and after a 10-day heat acclimation (∼50% V̇o2max in 40°C) program. The hot and cool condition V̇o2max and lactate threshold tests were both preceded by either warm (41°C) water or thermoneutral (34°C) water immersion to induce hyperthermia (0.8–1.0°C) or sustain normothermia, respectively. Eight matched control subjects completed the same exercise tests in the same environments before and after 10 days of identical exercise in a cool (13°C) environment. Heat acclimation increased V̇o2max by 5% in cool (66.8 ± 2.1 vs. 70.2 ± 2.3 ml·kg−1·min−1, P = 0.004) and by 8% in hot (55.1 ± 2.5 vs. 59.6 ± 2.0 ml·kg−1·min−1, P = 0.007) conditions. Heat acclimation improved time-trial performance by 6% in cool (879.8 ± 48.5 vs. 934.7 ± 50.9 kJ, P = 0.005) and by 8% in hot (718.7 ± 42.3 vs. 776.2 ± 50.9 kJ, P = 0.014) conditions. Heat acclimation increased power output at lactate threshold by 5% in cool (3.88 ± 0.82 vs. 4.09 ± 0.76 W/kg, P = 0.002) and by 5% in hot (3.45 ± 0.80 vs. 3.60 ± 0.79 W/kg, P < 0.001) conditions. Heat acclimation increased plasma volume (6.5 ± 1.5%) and maximal cardiac output in cool and hot conditions (9.1 ± 3.4% and 4.5 ± 4.6%, respectively). The control group had no changes in V̇o2max, time-trial performance, lactate threshold, or any physiological parameters. These data demonstrate that heat acclimation improves aerobic exercise performance in temperate-cool conditions and provide the scientific basis for employing heat acclimation to augment physical training programs.
Keywords: maximal oxygen uptake, time-trial performance, lactate threshold, plasma volume, cardiac output, hot environment, cool environment
levine and stray-gundersen (22) demonstrated that living at high altitude (hypoxia) while training at sea level can improve aerobic exercise performance beyond levels achieve by living and training at sea level. This “live high-train low” approach was the first to leverage environmental exposure (hypoxia) and associated adaptations to improve aerobic exercise performance outside the adaptation environment. Environmental adaptations to hypoxia and heat stress are primitive and robust; in fact, heat acclimation provides more substantial environmental specific improvements in aerobic performance than altitude acclimation (34). The impact of heat acclimatization on improving exercise performance in cool-temperate conditions has not been well defined. Two studies (24, 36) reported that heat acclimation increased maximal aerobic power (V̇o2max) in temperate conditions, but since neither study employed control groups it is possible the improvements represented a “training effect” (24, 36). Heat acclimation is documented to induce numerous physiological adaptations that theoretically could improve aerobic exercise performance in cool-temperate conditions. These physiological adaptations from heat acclimation include reduced oxygen uptake at a given power output (32, 42), muscle glycogen sparing (7, 42), reduced blood lactate at a given power output (42), increased skeletal muscle force generation (21), plasma volume expansion (2, 38), improved myocardial efficiency (14), and increased ventricular compliance (16). Therefore, it is reasonable to postulate that heat acclimation, similarly to “live high-train low,” might improve exercise performance capabilities in temperate-cool conditions.
The purpose of this study was to determine the impact of heat acclimation on maximal aerobic power, time-trial performance, and lactate threshold, in a cool (13°C) environment. We hypothesized that heat acclimation would improve exercise performance capabilities in cool conditions and therefore provide a relatively convenient means to augment exercise capabilities in trained athletes.
METHODS
Subjects.
Before participation, each volunteer gave written informed consent as set forth by the Declaration of Helsinki. All protocols were approved by the Institutional Review Board of the University of Oregon. Twelve highly trained endurance cyclists (10 men, 2 women), age 24 ± 6 (SD) yr, completed the heat acclimation protocol (height 175 ± 6 cm, weight 67.7 ± 8.1 kg, body mass index 22.1 ± 3.9 kg/m2). Eight subjects (7 men, 1 woman), age 26 ± 4 yr, completed the control protocol (height 174 ± 6 cm, weight 70.2 ± 4.1 kg, body mass index 23.1 ± 3.1 kg/m2). Of these eight controls, four subjects completed the heat acclimation program after completing their control experiments. The heat acclimation group and control group were matched for maximal aerobic power (66.9 and 66.8 ml·kg−1·min−1, respectively; see Table 1) and training experience.
Table 1.
Initial aerobic performance results of the heat acclimation and control groups
| Heat Acclimation Group (n = 12) | Control Group (n = 8) | |
|---|---|---|
| V̇o2max, l/min | 4.47 ± 0.21 | 4.70 ± 0.14 |
| (3.00–5.51) | (4.25–5.51) | |
| V̇o2max, ml·kg−1·min−1 | 66.9 ± 2.1 | 66.8 ± 1.7 |
| (57.0–76.1) | (59.1–76.6) | |
| Maximal power output, W | 369 ± 15 | 381 ± 11 |
| (260–430) | (340–420) | |
| Maximal power output, W/kg | 5.5 ± 0.2 | 5.4 ± 0.2 |
| (4.7–6.0) | (5.0–5.9) |
Values are shown as means ± SE for 12 subects in the heat acclimation group and 8 subects in the control group. Range values are shown in parentheses. Reported values of maximal oxygen uptake (V̇o2max) and maximal power output were from V̇o2max test done in cool (13°C) conditions.
Study design.
Participants completed a battery of physiological and performance tests under two environmental conditions, then completed either an exercise-heat acclimation program or a control exercise program (identical exercise intensity but in a cool environment), and then the physiological and performance tests were repeated. The performance tests battery included a lactate threshold test followed by a V̇o2max test, and a time-trial performance test (separate day). The maximal aerobic power and time-trial tests were both included to provide two separate measures of aerobic performance, while the lactate threshold test provided insight into a physiological mechanism. No attempt was made to control for training during the lead-in phase of the study, although subjects were recruited from the same club team and thus had the same competition schedule and essentially identical training routines.
On days the tests were performed under heat stress, the climatic chamber was set to 38°C and 30% relative humidity [wet bulb globe temperature (WBGT) = 33°C]. On days when the studies were performed in cool conditions, the climatic chamber was set to 13°C and 30% relative humidity (WBGT = 12°C). The 13°C environment was selected because it approximates the thermal conditions believed to be optimal for aerobic performance (9). The order between hot and cool trials was randomized. The heat acclimation protocol consisted of 10 exposures of cycle ergometer exercise at a temperature of 40°C and 30% relative humidity (WBGT = 35°C). Subjects performed two bouts of 45 min at 50% of their V̇o2max with 10 min of rest in between. A matched control group exercised at the same intensity but with the chamber set at 13°C and 30% relative humidity (WBGT = 12°C). The 50% of V̇o2max exercise intensity was selected as it would represent compensable heat stress sufficient to induce heat acclimation but not be sufficient to induce training adaptations for our highly trained athletes. Subjects were instructed to maintain their normal training routines during the 10-day intervention period to maintain their fitness level. Postacclimation studies were completed within 1 wk of the conclusion of the heat acclimation period.
On each study visit, subjects reported to the laboratory after a 2-h fast, and well hydrated. Subjects were instructed to avoid consumption of alcohol or caffeine for at least 8–12 h before the study. In addition, they were not allowed to exercise on the same day prior to the study and were told to avoid ingestion of nonprescription drugs for the entire duration of the multiple study visits.
Measurements.
Exercise was preformed while seated on an electronically braked cycle ergometer (Lode Excalibur Sport, Groningen, The Netherlands). Heart rate (HR) was monitored continuously throughout each protocol via telemetry (model RS400, Polar Electro, Lake Success, NY). Core temperature was measured using continuous recordings of rectal temperature by a thermistor (YSI 400 Series, Mallinckrodt Medical, St. Louis, MO) inserted 10 cm beyond the anal sphincter. Dry, nude body weight was taken at the beginning of each study by a precision weighing balance to the nearest 5 g (Sartorius EB6CE-I, Precision Weighing Balances, Bradford, MA). The initial body weight was used to ensure body fluid balance remained constant during the study visits.
Cardiac output was measured by the open-circuit acetylene washin method originally developed in 1975 (39), modified in 1993 (10), and validated in humans during exercise against the direct Fick approach (17). Breath-by-breath measurements of oxygen consumption (V̇o2), carbon dioxide production (V̇co2), and expired minute ventilation (V̇e) were made by custom software (KCBeck Physiological Consulting, St Paul, MN) modified to interface to a respiratory mass spectrometer (Marquette MGA 1100, MA Tech Services). Expired air was also collected into Douglas bags and subsequently analyzed for oxygen and carbon dioxide concentrations (mass spectrometer) and volumes (Tissot gasometer). This permitted the comparison of breath-by-breath (15-s averages) and the Douglas bags determination of V̇o2 and V̇e.
Skin temperature was measured using thermocouples made of copper and constantan at selected body areas on the skin. An estimate of mean skin temperature was calculated using seven body sites (forehead, chest, abdomen, upper arm, forearm, upper thigh, and calf) (33). Mean body temperature was calculated using weighed coefficients for rectal temperature (Tre) and mean skin temperature (Tsk) [body temperature = 0.8(Tre) + 0.2(Tsk)]. Skin blood flow requirements (SKBF) were estimated based on core temperature (Tc), Tsk, specific heat of the blood (SH, ∼1 kcal/°C), and heat production (Hp in kcal/min) using the following formula: SKBF = (1/SH × Hp)/(Tc − Tsk) (28, 35). These estimates assume that blood entering and leaving the cutaneous circulation is equal to core and skin temperatures, respectively. Initial resting plasma volume (pretreatment, or day 1) was calculated from body mass by the equation of Sawka et al. (37) and posttreatment (day 10) plasma volume was calculated by correcting that initial value for the percent change in plasma volume (6).
Before initiating the lactate threshold and V̇o2max test (but not the time trial), subjects immersed in a water bath (∼41°C) for ∼30 min to increase their rectal temperature by 0.8–1.0°C. On the protocols done under cool environmental conditions (13°C), subjects also immersed in a water bath with thermoneutral water (∼34°C) for 30 min to maintain normothermia. The water immersion allowed us to manipulate the subjects' rectal and skin temperatures without employing exercise before the tests, which could potentially act as a confounding variable. Therefore, we could examine the impact of heat acclimation state on the different exercise tests at standardized heat stress condition.
Lactate threshold.
Approximately 30 min after water immersion, subjects performed cycle ergometer exercise continuously with 3-min stages. The initial power output was selected based on the subjects' height, weight, and their reported usual training workloads. Power output increments were selected so the test concluded after four to seven stages. Gas exchange was continuously measured by open-circuit spirometry. During the last 30 s of each stage a capillary blood sample was taken from a fingertip and analyzed for lactate concentration (Lactate Pro, Arkray, Kyoto, Japan). Cardiac output measurements were taken during the last 30 s of each stage by open-circuit acetylene washin method (17). Lactate threshold was determined using the point at which blood lactate increased 1 mM above resting value (5).
Maximal oxygen uptake.
Approximately 45 min after completing the lactate threshold test, subjects performed a V̇o2max test. This recovery time has been shown to be adequate to prevent any bias in subsequent aerobic performance tests (19). To elicit V̇o2max, subjects exercised to exhaustion on a cycle ergometer, with the power output increasing 20 W every minute. The initial power output was chosen based on the subjects' lactate threshold test results to elicit exhaustion within 8–15 min. Cardiac output measurements were taken every 3 min at the early stages of the test and then every minute until fatigue to ensure that a maximal cardiac output was determined. Gas exchange was continuously measured by open-circuit spirometry.
Time-trial performance.
After a brief warm-up (5 min at 40% of maximal power on cycle ergometer) subjects provided their maximal effort for 60 min. Total work completed after 1 h (in kJ) was the performance measured. During the test, the cycle ergometer was set to the hyperbolic mode (pedaling rate independent) and subjects did not receive any feedback (i.e., HR, power output, core temperature, etc.) except for total time elapsed. Subjects were allowed to modify power output as often as needed, but without knowing the power output. Every 5 min measurements of power output, cadence, work performed, heart rate, rate of perceived exertion (RPE), skin temperature, and rectal temperature were obtained. A capillary blood sample was taken from a fingertip and analyzed for lactate concentration (Lactate Pro, Arkray) at 10, 25, 40, and 55 min. Oxygen uptake and cardiac output data were measured at 20, 40, and 60 min. At the end of the time trial, subjects were toweled off, and nude body weight was recorded.
Statistical analyses.
We employed a repeated-measures design (before and after exercise control or heat acclimation) with non-repeated between groups. Data from each treatment (i.e., pre- vs. post-heat acclimation) were compared by using a one-way, repeated-measures ANOVA with Holm-Sidak analysis for post hoc comparisons. Significance was set at P < 0.05, and values are presented as means ± SE, unless otherwise indicated. An analysis selecting conventional α (0.05) and β (0.20) parameters showed that eight subjects would provide sufficient power to detect a 5% difference in time-trial performance between pre- and post-heat acclimation trials. This estimate was made using the mean total work (900 kJ) and the coefficient of variation (5.3%) calculated from prior studies. The postexercise control data from the four subjects who participated in both the control and heat acclimation protocols were also used as the pre-heat acclimation data as there were no differences between the preexercise control and the postexercise control tests. Statistics consulting was provided by Abacus Research (Eugene, OR).
RESULTS
Table 1 shows the initial aerobic performance results of the heat acclimation and control groups. Note that the heat acclimation and control groups have essentially identical maximal aerobic power (66.9 vs. 66.8 ml·kg−1·min−1, respectively) and maximal power output (5.5 vs. 5.4 W/kg, respectively). All subjects completed the 10-day heat acclimation and control group exercise program. To ensure the subjects were properly hydrated, nude body weight and plasma osmolality were measured. Euhydration was demonstrated by their nude body mass being within 1% of their 5-day average and plasma osmolality < 290 mosmol/kgH2O (30).
Table 2 provides plasma volume (rest), and heart rate and core temperature responses at the end of the second exercise bout on day 1 and day 10 of the heat acclimation program or control group exercise program. Heat acclimation group demonstrated a reduction (P < 0.001) in heart rate (15 beats/min) and a reduction (P < 0.002) in core temperature (0.5°C), while no differences were observed in the control group. Heat acclimation group demonstrated an increase (6.5%, P < 0.05) while the control group a reduction (4.6%, P > 0.05) in plasma volume (rest). Body weight did not change in either group between the pre- and posttreatment protocols.
Table 2.
Mean differences between day 1 and day 10 of the heat acclimation or exercise control period
| Heat Acclimation Group |
Control Group |
|||
|---|---|---|---|---|
| Day 1 | Day 10 | Day 1 | Day 10 | |
| Final heart rate, beats/min | 165 ± 2 | 150 ± 3* | 130 ± 3 | 127 ± 5 |
| Final Tc, °C | 39.3 ± 0.1 | 38.8 ± 0.1* | 38.1 ± 0.1 | 38.1 ± 0.1 |
| Hemoglobin, g/dl | 13.8 ± 0.3 | 13.3 ± 0.3 | 13.7 ± 0.2 | 14.0 ± 0.5 |
| Hematocrit | 0.43 ± 0.01 | 0.42 ± 0.01 | 0.42 ± 0.01 | 0.43 ± 0.01 |
| Plasma volume, liters | 3.0 ± 0.1 | 3.2 ± 0.1* | 3.1 ± 0.1 | 2.9 ± 0.1 |
| Plasma volume change, % | 6.5 ± 1.2† | −4.6 ± 2.7 | ||
Values are shown as means ± SE for 12 subects in the heat acclimation group and 8 subects in the control group. Values shown are resting plasma volume, hematocrit, hemoglobin; and final heart rate and core temperature (Tc) at end of the second exercise bout.
P < 0.05 vs. day 1.
P < 0.05 vs. control group.
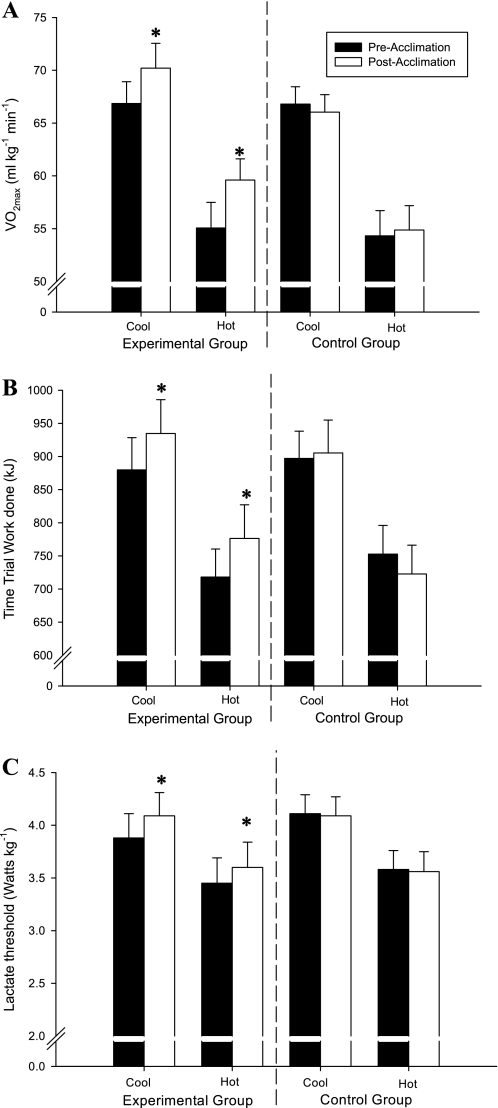
Figure 1 plots individual data against the line of no difference (before and after 10-day treatment) for maximal oxygen uptake (Fig. 1A), time-trial performance (Fig. 1B), and lactate threshold (Fig. 1C) tests in the cool and hot environments for the heat acclimation and control groups. For each of these three independent tests of exercise performance it should be noted the consistency that data points fall above the line of identity for the heat acclimation group and that data points fall on the line of identity for the control group. The heat acclimation group individual data demonstrate a clear and consistent performance improvement in both the cool and hot environments, while the control group shows no tendency toward such trends for all variables.
Fig. 1.
Individual data for relationship between pre- and postacclimation in performance variables of heat acclimation (left) and control (right) groups under hot and cool condition. A: maximal aerobic power (V̇o2max). B: time trial performance. C: lactate threshold. Straight line represents line of equality.
Figure 2 provides the mean responses for each test for both groups for maximal oxygen uptake (Fig. 2A), time-trial performance (Fig. 2B), and lactate threshold (Fig. 2C). Heat acclimation increased (P < 0.05) V̇o2max in cool (66.9 ± 2.1 vs. 70.2 ± 2.4 ml·kg−1·min−1) and hot (55.1 ± 2.4 vs. 59.6 ± 2.0 ml·kg−1·min−1), increased (P < 0.05) time-trial performance in cool (879.8 ± 48.5 vs. 934.7 ± 50.9 kJ) and hot (718.7 ± 42.3 vs. 776.2 ± 50.9 kJ), and increased (P < 0.05) lactate threshold in cool (3.9 ± 0.8 vs. 4.1 ± 0.8 W/kg) and hot (3.5 ± 0.8 vs. 3.6 ± 0.8 W/kg) conditions. For the control group, no changes were found for V̇o2max in cool (66.8 ± 1.7 vs. 66.0 ± 1.6 ml·kg−1·min−1) or hot (54.3 ± 2.4 vs. 54.9 ± 2.3 ml·kg−1·min−1), time-trial performance in cool (897.1 ± 41.0 vs. 905.3 ± 49.5 kJ) or hot (752.8 ± 43.2 vs. 722.7 ± 43.6 kJ), and lactate threshold in cool (4.1 ± 0.5 vs. 4.1 ± 0.5 W/kg) or hot (3.6 ± 0.5 vs. 3.6 ± 0.5 W/kg) conditions. Maximal heart rate did not change in either of the heat acclimation or control groups (data not shown).
Fig. 2.
Effect of heat acclimation on V̇o2max (A), total work done during a 1-h time trial (B), and power output at lactate threshold (C) in a cool (13°C) and hot (38°C) environment. Values are means ± SE for 12 heat acclimation subjects and 8 controls. *P < 0.05 vs. preacclimation within environmental condition.
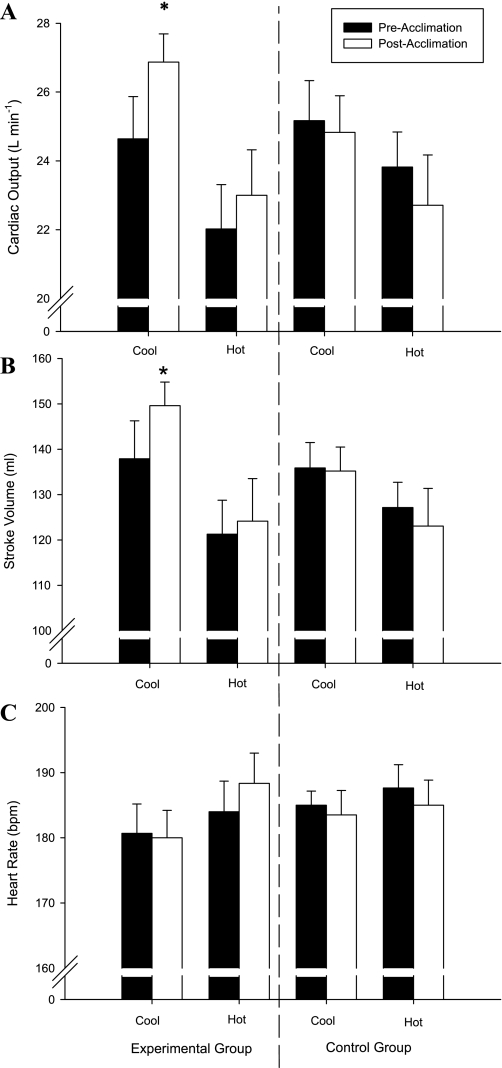
Figure 3 provides the heat acclimation effects on maximal cardiac output (Fig. 3A), and the corresponding stroke volume (Fig. 3B), and heart rate (Fig. 3C) during the V̇o2max test. Heat acclimation increased maximal cardiac output in the cool (24.7 ± 1.2 vs. 26.9 ± 0.82 l/min), but not in the hot (22.0 ± 1.3 vs. 23.0 ± 1.3 l/min) environment. Similarly, stroke volume during maximal cardiac output was increased after heat acclimation in the cool (138 ± 8 vs. 150 ± 5 ml), but not in the hot (121 ± 8 vs. 124 ± 9 ml) environment. Heat acclimation did not alter maximal heart rate achieved in the cool (181 ± 5 vs. 180 ± 4 beats/min) or hot (184 ± 5 vs. 188 ± 5 beats/min) condition. For the control group, no differences were observed in maximal cardiac output, stroke volume, or heart rate in the cool (25.2 ± 1.2 vs. 24.8 ± 1.1 l/min; 136 ± 6 vs. 135 ± 5 ml; 185 ± 2 vs. 184 ± 4 beats/min) or hot (23.8 ± 1.0 vs. 22.7 ± 1.5 l/min; 127 ± 6 vs. 123 ± 8 ml; 188 ± 4 vs. 185 ± 4 beats/min) environment.
Fig. 3.
Heat acclimation effects on maximal cardiac output (A), and their corresponding stroke volume (B), and heart rate (C) during V̇o2max test in a cool (13°C) and hot (38°C) environment. Values are means ± SE for 12 heat acclimation subjects and 8 controls. bpm, beats/min. *P < 0.05 vs. preacclimation within environmental condition.
Table 3 provides the physiological responses during the time-trial performance tests in the heat acclimation group and control group before and after treatment (heat acclimation or exercise control period). All results are shown as means and SE. The heat acclimation group had lower (P = 0.02) skin temperature, greater (P = 0.01) core-skin gradient, and greater (P = 0.04) cardiac output at the end of time-trial test after acclimation in cool conditions. The heat acclimation group had lower (P = 0.01) skin temperatures, and greater (P = 0.01) core-skin gradient at the end of the time-trial test after acclimation in hot conditions. The control group demonstrated lower (P = 0.03) core temperature in the hot condition at the end of the time trial. We also observed higher (P = 0.02) skin temperature, lower (P = 0.03) core-skin gradient, and higher (P = 0.02) skin blood flow at the end of the time-trial test after control exercise treatment in the cool condition.
Table 3.
Mean responses during the 1-h time trial pre- and postacclimation in the experimental and control groups
| Hot Condition (38°C) |
Cool Condition (13°C) |
|||
|---|---|---|---|---|
| Before | After | Before | After | |
| Ending rectal temperature, °C | ||||
| HA | 39.5 ± 0.1 | 39.4 ± 0.2 | 38.8 ± 0.2 | 38.8 ± 0.1 |
| Control | 39.3 ± 0.2 | 38.9 ± 0.1* | 38.9 ± 0.2 | 38.7 ± 0.2 |
| Ending mean skin temperature, °C | ||||
| HA | 34.8 ± 0.3 | 33.9 ± 0.2* | 24.1 ± 0.5 | 23.0 ± 0.3* |
| Control | 34.7 ± 0.4 | 34.6 ± 0.2 | 23.7 ± 0.5 | 25.1 ± 0.7* |
| Core-to-skin gradient, °C | ||||
| HA | 4.7 ± 0.4 | 5.5 ± 0.3* | 14.7 ± 0.5 | 15.8 ± 0.3* |
| Control | 4.6 ± 0.3 | 4.4 ± 0.2 | 15.0 ± 0.4 | 13.3 ± 0.6* |
| Estimated skin blood flow, l/min | ||||
| HA | 2.3 ± 0.2 | 2.3 ± 0.2 | 1.0 ± 0.1 | 1.0 ± 0.1 |
| Control | 3.0 ± 0.3 | 2.8 ± 0.2 | 1.1 ± 0.1 | 1.3 ± 0.1* |
| Ending mean body temperature, °C | ||||
| HA | 38.7 ± 0.1 | 38.3 ± 0.2 | 35.9 ± 0.1 | 35.7 ± 0.1 |
| Control | 38.5 ± 0.1 | 38.1 ± 0.1 | 35.9 ± 0.1 | 36.0 ± 0.1 |
| Total body water loss, liters | ||||
| HA | 1.8 ± 0.2 | 2.2 ± 0.2* | 1.1 ± 0.1 | 1.3 ± 0.1* |
| Control | 1.9 ± 0.2 | 2.0 ± 0.2 | 1.1 ± 0.1 | 1.1 ± 0.1 |
| Mean power output, W | ||||
| HA | 201 ± 12 | 216 ± 14* | 246 ± 13 | 259 ± 14* |
| Control | 208 ± 12 | 201 ± 12 | 249 ± 12 | 254 ± 14 |
| Mean blood lactate, mmol/l | ||||
| HA | 3.0 ± 0.3 | 3.2 ± 0.2 | 4.2 ± 0.4 | 4.7 ± 0.5 |
| Control | 3.3 ± 0.4 | 2.3 ± 0.4 | 3.9 ± 0.3 | 3.6 ± 0.5 |
| Mean cardiac output, l/min | ||||
| HA | 20.1 ± 1.6 | 20.5 ± 1.4 | 22.3 ± 1.4 | 24.3 ± 1.5* |
| Control | 22.6 ± 1.6 | 22.9 ± 1.8 | 25.0 ± 1.6 | 25.4 ± 1.9 |
| Mean V̇o2, l/min | ||||
| HA | 2.79 ± 0.22 | 2.90 ± 0.23* | 3.50 ± 0.20 | 3.78 ± 0.21* |
| Control | 3.11 ± 0.16 | 2.97 ± 0.15 | 3.81 ± 0.19 | 3.73 ± 0.20 |
| Mean RPE | ||||
| HA | 16 ± 1 | 16 ± 1 | 16 ± 1 | 16 ± 1 |
| Control | 16 ± 1 | 16 ± 1 | 15 ± 1 | 16 ± 1 |
Values are means ± SE for 12 subects in the experimental group and 8 subects in the control group. HA, heat acclimation. RPE, rating of received exertion.
P < 0.05 vs. preacclimation trial.
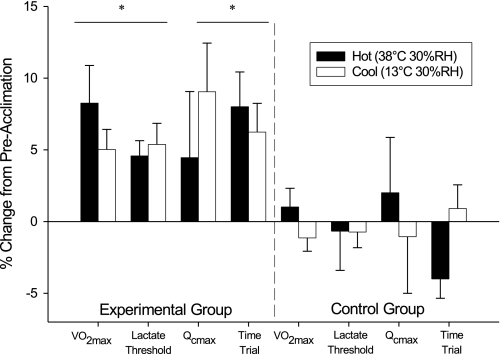
Figure 4 summarizes the cardiorespiratory and performance changes induced by heat acclimation or exercise control programs in both hot and cool environments. The heat acclimation group showed significant improvements in every variable (except for the maximal cardiac output in the hot condition). On the other hand, there was no significant difference in the control group in any of the variables.
Fig. 4.
Cardiorespiratory and performance changes as a percent change from the preacclimation trials in both environmental conditions. *P < 0.05 vs. preacclimation within environmental condition. There was no difference in the variables displayed for the control group. Values are means ± SE for 12 heat acclimation subjects and 8 controls. Qcmax, maximal cardiac output.
DISCUSSION
This study is the first to examine the impact of heat acclimation on aerobic performance in cool (13°C) conditions. We employed three separate tests: maximal aerobic power, time-trial performance, and lactate threshold. We studied competitive cyclists because they would provide more consistent maximal efforts, were highly trained, and provided a target group to demonstrate the potential ergogenic effects of heat acclimation for competitive athletes. Our data clearly demonstrate that 10 days of heat acclimation provide considerable ergogenic benefits in cool conditions. In addition, heat acclimation provided the expected performance benefits in hot conditions.
Heat acclimation is documented to induce numerous physiological adaptations that theoretically could improve aerobic exercise performance in cool-temperate conditions. These physiological adaptations from heat acclimation include reduced oxygen uptake at a given power output (32, 42), muscle glycogen sparing (7, 42), reduced blood lactate at a given power output (42), plasma volume expansion (2, 38), improved myocardial efficiency (14), and increased ventricular compliance (16), and enhanced force generation in the soleus muscle (21). Our observed increase in maximal oxygen uptake could be mediated by plasma volume expansion (31), improved myocardial efficiency, and increased ventricular compliance (14, 16), which would allow larger end-diastolic volume. Although we observed a small plasma expansion, neither myocardial efficiency nor ventricular compliance was measured. While there was a slight hemodilution post-heat acclimation induced by the plasma expansion (138.4 vs. 133.3 g Hb/l, pre- and post-heat acclimation, respectively), we observed a substantial increased maximal cardiac output of 2.2 l/min. This increase in maximal cardiac output can account for the 5% increase in V̇o2max in the cool environment [assuming constant whole body arteriovenous oxygen content difference (a-vO2) of 85% and 1.34 ml O2/g Hb]. However, these estimations should be taken with caution since there is some degree of imprecision when taking measurements, and multiple measurements to estimate certain parameters could increase the degree of inaccuracy.
Heat acclimation increased resting plasma volume by about 6.5% (200 ml), and this is in agreement with others (1, 25, 26, 38). Controversy exists as to whether hypervolemia (i.e., plasma volume expansion) has the potential to increase maximal cardiac output, and how this potential change affects V̇o2max. Kanstrup and Ekblom reported that plasma volume expansion (i.e., 570 ml) increased maximal cardiac output 8% and decreased hemoglobin concentration by 8%; thus maximal oxygen uptake remained unchanged (18). Hopper et al. (13) observed in untrained men that plasma volume expansion (i.e., 400 ml) increased stroke volume by 11% during submaximal exercise. However, a larger plasma volume expansion (i.e., 630 ml) did not elicit further increases in stroke volume (13). There has also been evidence that plasma volume expansion may be responsible for slight but significant increases in V̇o2max (4, 24, 36). Coyle et al. (4) showed that plasma volume expansion by 200–300 ml of 6% dextran significantly increased V̇o2max in untrained subjects, with an increased cardiac output after plasma volume expansion at submaximal exercise intensities (4). More importantly, Coyle et al. (4) stated that the potential for plasma volume expansion to increase V̇o2max depends on the balance between the increased maximal cardiac output compared with the reduced hemoglobin concentration, and thus arterial oxygen content. The present study observed a moderate plasma volume expansion (6.5%) with a small hemodilution (3.3%) and increased maximal cardiac output (9%) and thus increased V̇o2max by 5%.
An improved cardiac performance (maximal cardiac output and maximal stroke volume) following a period of chronic heat stress is also supported by several animal studies, which reported several mechanical and metabolic adaptations in the rat heart (14–16, 23). For instance, heat acclimation increases left ventricular compliance and pressure generation and decreases myocardial oxygen consumption (14, 16). The improved myocardial oxygen consumption results from a transition from fast myosin (V1) to slow myosin isoforms (V3) (15). Finally, combined heat acclimation and exercise training have been shown to have additive effects on the mechanical and metabolic properties of rat hearts compared with the effects of exercise training or heat acclimation alone (23). In addition, these authors (23) reported that augmented force generation (i.e., contractility) post-heat acclimation was associated with elevation of cytosolic calcium concentration on contraction. Together, these studies provide mechanisms that support our observations that heat acclimation increased maximal cardiac output.
Our study was the first to examine the effects of heat acclimation on time-trial performance in either a hot or cool environment. This investigation employed a time-trial approach to explore and quantify the changes in performance of highly trained cyclists, which is a measure more specific to the demands of athletic competitions. Our findings that total work in kilojoules was improved after a period of heat acclimation agrees with our hypothesis. The increased time-trial performance is likely in part due to the increased V̇o2max reducing the relative exercise intensity (%V̇o2max). A reduced relative exercise intensity is associated with improved exercise endurance (11). Heat acclimation has been reported to reduce submaximal oxygen uptake requirements in a temperate and hot environment (32) and this also would act to reduce relative exercise intensity. Unfortunately, we did not measure oxygen uptake at any given submaximal power output before and after acclimation so are unsure whether this adaptation contributed here. Another possible mechanism was that heat acclimation increased the core-to-skin temperature gradient (by lowering skin temperature, perhaps by earlier onset of sweating). The widened gradient would reduce skin blood flow requirement at a given workload and potentially allow a greater percentage of any given cardiac output to be directed to active skeletal muscle. Some studies have reported that heat acclimation induces metabolic adaptations during exercise by reducing the aerobic metabolic rate (32, 42), or decreasing the rate of glycogenolysis (7, 8, 20). Thus, at a given absolute workload, there is a decrease in oxygen consumption post-heat acclimation. Consequently, these adaptations would allow subjects to maintain higher power outputs, reduce relative intensity, and improve the time-trial performance.
A novel finding from this study is that heat acclimation increased lactate threshold in a cool environment. To our knowledge, there have been no studies that have explored this relationship. The lower lactate levels during exercise observed after heat acclimation is in agreement with previous research. At a given exercise intensity, heat acclimation has been shown to reduce the blood lactate concentration (7, 42). In addition to the lower blood lactate levels measured after heat acclimation in both environments, we are the first to report that the threshold at which blood lactate levels begin to rise also is delayed by heat acclimation. As previously described, some studies suggested that heat acclimation induces metabolic adaptations during exercise by reducing the aerobic metabolic rate (1, 32, 42), or decreasing the rate of glycogenolysis (7, 8, 20). Alternatively, the increased plasma volume (and thus, total blood volume) (3, 12, 38, 41) could have an effect in blood lactate concentration by increasing blood flow through the splanchnic circulation, enhancing lactate removal (29), and thus delaying blood lactate accumulation. The previously discussed increase in cardiac output to active muscles, together with the decrease aerobic metabolic rate (1, 32, 42), may account for the delay in blood lactate accumulation. In addition, the possibility of an increased lactate removal by increased splanchnic blood flow (29) cannot be discarded.
There is the possibility that the multiple exercise sessions induced a training or learning effect that might have contributed to improve performance regardless of the heat acclimation status. We believe this is not the case in our study for several reasons. First, the combination of low exercise intensity during heat acclimation (50% of their V̇o2max), plus the subjects' high fitness level (mean V̇o2max of 66 ml·kg−1·min−1) make a training effect unlikely (27). Second, a “learning effect” would be unlikely because all the subjects were well trained and had previous experiences performing similar time-trial competitions. Third, the control group did not show any trends for improvement. Although no attempt was made to control for training during the lead-in phase of the study, all of the subjects who participated in this study were recruited from the same club team and thus had the same competition schedule and essentially identical training routines. In addition, we do not believe that the differences observed post-heat acclimation were related with the subjects' training background, and they were encouraged to keep to their training schedule during participation in the study. There were no differences in the effect of the intervention between the subjects who completed the study in the early winter months (and thus were probably doing mostly longer rides) from those who did the study during the spring/summer (and presumably were doing more high-intensity workouts). Therefore, this heat acclimation protocol may be used to supplement a wide range of training routines.
We are the first to conclusively demonstrate that heat acclimation can improve aerobic exercise performance in cool-temperate conditions. These heat acclimation benefits may be retained for 1 or 2 wk, and the rate of decay for heat acclimation will depend on many factors like fitness level of the subjects, environmental conditions where the subjects live, and intensity and duration of their training post-heat acclimation (40). Our findings are analogous to “live high and train low” concepts developed by Levine and Stray-Gundersen (22) but might require less time and logistical support. Our research and that by Levine and Stray-Gundersen (22) demonstrate that robust adaptations to environmental exposure can be leveraged to augment aerobic performance in highly trained athletes.
GRANTS
Funding of this research project was provided by the Clarissa and Evonuk Memorial Fellowship and National Institutes of Health Grant HL-081671 (Minson).
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author(s).
ACKNOWLEDGMENTS
We greatly appreciate the considerable time and effort of the helpers and subjects who participated in this project.
The views, opinions, and findings in this report are those of the authors and should not be construed as an official US Department of the Army position or decision unless so designated by other official documentation. This has been approved for public release; distribution is unlimited.
REFERENCES
- 1. Aoyagi Y, McLellan TM, Shephard RJ. Effects of training and acclimation on heat tolerance in exercising men wearing protective clothing. Eur J Appl Physiol Occup Physiol 68: 234–245, 1994 [DOI] [PubMed] [Google Scholar]
- 2. Bass DE, Buskirk ER, Iampietro PF, Mager M. Comparison of blood volume during physical conditioning, heat acclimatization and sedentary living. J Appl Physiol 12: 186–188, 1958 [DOI] [PubMed] [Google Scholar]
- 3. Bass DE, Kleeman CR, Quinn M, Henschel A, Hegnauer AH. Mechanisms of acclimatization to heat in man. Medicine 34: 323–380, 1955 [DOI] [PubMed] [Google Scholar]
- 4. Coyle EF, Hopper MK, Coggan AR. Maximal oxygen uptake relative to plasma volume expansion. Int J Sports Med 11: 116–119, 1990 [DOI] [PubMed] [Google Scholar]
- 5. Coyle EF, Martin WH, Ehsani AA, Hagberg JM, Bloomfield SA, Sinacore DR, Holloszy JO. Blood lactate threshold in some well-trained ischemic heart disease patients. J Appl Physiol 54: 18–23, 1983 [DOI] [PubMed] [Google Scholar]
- 6. Dill DB, Costill DL. Calculation of percentage changes in volumes of blood, plasma, and red cells in dehydration. J Appl Physiol 37: 247–248, 1974 [DOI] [PubMed] [Google Scholar]
- 7. Febbraio MA, Snow RJ, Hargreaves M, Stathis CG, Martin IK, Carey MF. Muscle metabolism during exercise and heat stress in trained men: effect of acclimation. J Appl Physiol 76: 589–597, 1994 [DOI] [PubMed] [Google Scholar]
- 8. Febbraio MA, Snow RJ, Stathis CG, Hargreaves M, Carey MF. Blunting the rise in body temperature reduces muscle glycogenolysis during exercise in humans. Exp Physiol 81: 685–693, 1996 [DOI] [PubMed] [Google Scholar]
- 9. Galloway SD, Maughan RJ. Effects of ambient temperature on the capacity to perform prolonged cycle exercise in man. Med Sci Sports Exerc 29: 1240–1249, 1997 [DOI] [PubMed] [Google Scholar]
- 10. Gan K, Nishi I, Chin I, Slutsky AS. On-line determination of pulmonary blood flow using respiratory inert gas analysis. IEEE Trans Biomed Eng 40: 1250–1259, 1993 [DOI] [PubMed] [Google Scholar]
- 11. Gleser MA, Vogel JA. Effects of acute alterations of V̇o2max on endurance capacity of men. J Appl Physiol 34: 443–447, 1973 [DOI] [PubMed] [Google Scholar]
- 12. Harrison MH, Edwards RJ, Graveney MJ, Cochrane LA, Davies JA. Blood volume and plasma protein responses to heat acclimatization in humans. J Appl Physiol 50: 597–604, 1981 [DOI] [PubMed] [Google Scholar]
- 13. Hopper MK, Coggan AR, Coyle EF. Exercise stroke volume relative to plasma-volume expansion. J Appl Physiol 64: 404–408, 1988 [DOI] [PubMed] [Google Scholar]
- 14. Horowitz M, Parnes S, Hasin Y. Mechanical and metabolic performance of the rat heart: effects of combined stress of heat acclimation and swimming training. J Basic Clin Physiol Pharmacol 4: 139–156, 1993 [DOI] [PubMed] [Google Scholar]
- 15. Horowitz M, Peyser YM, Muhlrad A. Alterations in cardiac myosin isoenzymes distribution as an adaptation to chronic environmental heat stress in the rat. J Mol Cell Cardiol 18: 511–515, 1986 [DOI] [PubMed] [Google Scholar]
- 16. Horowitz M, Shimoni Y, Parnes S, Gotsman MS, Hasin Y. Heat acclimation: cardiac performance of isolated rat heart. J Appl Physiol 60: 9–13, 1986 [DOI] [PubMed] [Google Scholar]
- 17. Johnson BD, Beck KC, Proctor DN, Miller J, Dietz NM, Joyner MJ. Cardiac output during exercise by the open circuit acetylene washin method: comparison with direct Fick. J Appl Physiol 88: 1650–1658, 2000 [DOI] [PubMed] [Google Scholar]
- 18. Kanstrup IL, Ekblom B. Blood volume and hemoglobin concentration as determinants of maximal aerobic power. Med Sci Sports Exerc 16: 256–262, 1984 [PubMed] [Google Scholar]
- 19. Kenefick RW, Ely BR, Cheuvront SN, Palombo LJ, Goodman DA, Sawka MN. Prior heat stress: effect on subsequent 15-min time trial performance in the heat. Med Sci Sports Exerc 41: 1311–1316, 2009 [DOI] [PubMed] [Google Scholar]
- 20. Kirwan JP, Costill DL, Kuipers H, Burrell MJ, Fink WJ, Kovaleski JE, Fielding RA. Substrate utilization in leg muscle of men after heat acclimation. J Appl Physiol 63: 31–35, 1987 [DOI] [PubMed] [Google Scholar]
- 21. Kodesh E, Horowitz M. Soleus adaptation to combined exercise and heat acclimation: physiogenomic aspects. Med Sci Sports Exerc 42: 943–952, 2010 [DOI] [PubMed] [Google Scholar]
- 22. Levine BD, Stray-Gundersen J. “Living high–training low”: effect of moderate-altitude acclimatization with low-altitude training on performance. J Appl Physiol 83: 102–112, 1997 [DOI] [PubMed] [Google Scholar]
- 23. Levy E, Hasin Y, Navon G, Horowitz M. Chronic heat improves mechanical and metabolic response of trained rat heart on ischemia and reperfusion. Am J Physiol Heart Circ Physiol 272: H2085–H2094, 1997 [DOI] [PubMed] [Google Scholar]
- 24. Nadel ER, Pandolf KB, Roberts MF, Stolwijk JA. Mechanisms of thermal acclimation to exercise and heat. J Appl Physiol 37: 515–520, 1974 [DOI] [PubMed] [Google Scholar]
- 25. Nielsen B, Hales JR, Strange S, Christensen NJ, Warberg J, Saltin B. Human circulatory and thermoregulatory adaptations with heat acclimation and exercise in a hot, dry environment. J Physiol 460: 467–485, 1993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Patterson MJ, Stocks JM, Taylor NA. Sustained and generalized extracellular fluid expansion following heat acclimation. J Physiol 559: 327–334, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pollock ML. The quantification of endurance training programs. Exerc Sport Sci Rev 1: 155–188, 1973 [PubMed] [Google Scholar]
- 28. Rowell LB. Human Circulation: Regulation During Physical Stress. New York: Oxford Univ. Press, 1986 [Google Scholar]
- 29. Rowell LB, Brengelmann GL, Blackmon JR, Twiss RD, Kusumi F. Splanchnic blood flow and metabolism in heat-stressed man. J Appl Physiol 24: 475–484, 1968 [DOI] [PubMed] [Google Scholar]
- 30. Sawka MN, Burke LM, Eichner ER, Maughan RJ, Montain SJ, Stachenfeld NS. American College of Sports Medicine position stand. Exercise and fluid replacement. Med Sci Sports Exerc 39: 377–390, 2007 [DOI] [PubMed] [Google Scholar]
- 31. Sawka MN, Coyle EF. Influence of body water and blood volume on thermoregulation and exercise performance in the heat. Exerc Sport Sci Rev 27: 167–218, 1999 [PubMed] [Google Scholar]
- 32. Sawka MN, Pandolf KB, Avellini BA, Shapiro Y. Does heat acclimation lower the rate of metabolism elicited by muscular exercise? Aviat Space Environ Med 54: 27–31, 1983 [PubMed] [Google Scholar]
- 33. Sawka MN, Wenger CB. Physiological responses to acute exercise-heat stress. In: Human Performance, Physiology, and Environmental Medicine at Terrestrial Extremes, edited by Pandolf KB, Sawka MN, Gonzalez RR. Traverse City, MI: Cooper Publishing, 1988, p. 97–151 [Google Scholar]
- 34. Sawka MN, Wenger CB, Pandolf KB. Thermoregulatory responses to acute exercise—heat stress and heat acclimation. In: Handbook of Physiology. Environmental Physiology. Bethesda, MD: Am. Physiol. Soc., 1996, sect. 4, vol. I, chapt. 9, p. 157–186 [Google Scholar]
- 35. Sawka MN, Young AJ. Physiological systems and their responses to conditions of heat and cold. In: ACSM's Advance Exercise Physiology, edited by Sawka MN, Tipton CM. Hagerstown MD: Lippincott Williams and Wilkins, 2006, p. 536–563 [Google Scholar]
- 36. Sawka MN, Young AJ, Cadarette BS, Levine L, Pandolf KB. Influence of heat stress and acclimation on maximal aerobic power. Eur J Appl Physiol Occup Physiol 53: 294–298, 1985 [DOI] [PubMed] [Google Scholar]
- 37. Sawka MN, Young AJ, Pandolf KB, Dennis RC, Valeri CR. Erythrocyte, plasma, and blood volume of healthy young men. Med Sci Sports Exerc 24: 447–453, 1992 [PubMed] [Google Scholar]
- 38. Senay LC, Mitchell D, Wyndham CH. Acclimatization in a hot, humid environment: body fluid adjustments. J Appl Physiol 40: 786–796, 1976 [DOI] [PubMed] [Google Scholar]
- 39. Stout RL, Wessel HU, Paul MH. Pulmonary blood flow determined by continuous analysis of pulmonary N2O exchange. J Appl Physiol 38: 913–918, 1975 [DOI] [PubMed] [Google Scholar]
- 40. Williams CG, Wyndham CH, Morrison JF. Rate of loss of acclimatization in summer and winter. J Appl Physiol 22: 21–26, 1967 [DOI] [PubMed] [Google Scholar]
- 41. Wyndham CH, Benade AJ, Williams CG, Strydom NB, Goldin A, Heyns AJ. Changes in central circulation and body fluid spaces during acclimatization to heat. J Appl Physiol 25: 586–593, 1968 [DOI] [PubMed] [Google Scholar]
- 42. Young AJ, Sawka MN, Levine L, Cadarette BS, Pandolf KB. Skeletal muscle metabolism during exercise is influenced by heat acclimation. J Appl Physiol 59: 1929–1935, 1985 [DOI] [PubMed] [Google Scholar]