Abstract
Objective: This article reviews the epidemiology, etiology, assessment, and management of bipolar disorder. Special attention is paid to factors that complicate treatment, including nonadherence, comorbid disorders, mixed mania, and depression. Methods: A Medline search was conducted from January of 1990 through December of 2005 using key terms of bipolar disorder, diagnosis, and treatment. Papers selected for further review included those published in English in peer-reviewed journals, with preference for articles based on randomized, controlled trials and consensus guidelines. Citations de-emphasized original mania trials as these are generally well known. Results: Bipolar disorder is a major public health problem, with diagnosis often occurring years after onset of the disorder. comorbid conditions are common and difficult to treat. Management includes a lifetime course of medication, usually more than one, and attention to psychosocial issues for patients and their families. Management of mania is well-established. Research is increasing regarding management of depressive, mixed and cycling episodes, as well as combination therapy. Conclusions: Bipolar disorder is a complex psychiatric disorder to manage, even for psychiatrists, because of its many episodes and comorbid disorders and nonadherence to treatment.
Keywords: bipolar, diagnosis, review, treatment, depression
Introduction
Bipolar spectrum disorders are a major public health problem, with estimates of lifetime prevalence in the general population of the United States at 3.9 percent,1 with a range from 1.5 to 6.0 percent.2 Bipolar disorder is also associated with significant mortality risk, with approximately 25 percent of patients attempting suicide and 11 percent of patients completing.3 Furthermore, inadequate treatment and service structure causes high rates of jailing for bipolar patients.4 Bipolar depression is still undertreated, too, with patients suffering such symptoms 31.9 percent of the time over nearly 13 years.5
Review articles for adults6,7 and pediatric patients8 imply progress, but we have not fully researched depressive episodes, combination treatment, health services interventions, and special populations. Practice guidelines,9 decision trees,10 and elaborate algorithms11,12 are well written, but are not user friendly.
More pharmacologic options are now available, and psychoeducation, self-help, and psychotherapy (individual, couple, and family) interventions are frequently utilized.9 The Depression and Bipolar Support Alliance has taken a leading role in educating patients, their families, medical professionals, mental health professionals, and the public at large about manic-depressive illness. The National Alliance of the Mentally Ill (NAMI) has also sought information by surveying family members about utilization and value of mental health services.13
Epidemiology
Bipolar I disorder starts on average at 18 years and bipolar II disorder at 22 years.9,14 A community study using the Mood Disorder Questionnaire (MDQ) revealed a prevalence of 3.7 percent.15 The National Comorbidity Study showed onset typically between 18 and 44, with higher rates between 18 and 34 than 35 and 54.1 In a survey of members of the DBSA, more than half of the patients did not seek care for five years and the correct diagnosis was not made until an average of eight years after they first sought treatment.16,17
Bipolar disorder has not consistently been associated with sociodemographic factors. Males and females are equally affected by bipolar I, whereas bipolar II is more common in women. No clear association between race/ethnicity, socioeconomic status, and locale of home (e.g., rural vs. urban). There is a higher rate of bipolar disorder in unmarried people.1,14
Economic analyses usually include direct treatment costs, indirect costs arising from mortality, and indirect costs related to morbidity and lost productivity. This is the model for bipolar disorder and others that are long-term or lifetime disorders. Misdiagnosis leads to exorbitant costs and mistreatment.8 Late presentation, inadequate diagnosis, and undertreatment contribute heavily to costs.
Etiology and Pathophysiology
There is not a single hypothesis that unifies genetic, biochemical, pharmacological, anatomical, and sleep data on bipolar disorder.20 Biochemical investigations are underway for transmitters (catecholamines, serotonin, gamma aminobutyric acid (GABA), glutamate and others), hormones (brain-derived neurotrophic factor, thyroid and others), and steroids—alone and in collaboration. Imaging studies, emerging throughout medicine, may shed light.
Epidemiological evidence, particularly studies of concordance in identical and fraternal twins, implies that affective disorders are heritable. For family members of bipolar probands, the morbid risk is between 2.9 and 14.5 percent for bipolar disorder and 4.2 and 24.3 percent for unipolar disorder, depending on the diagnostic criteria used and the heterogeneity of the probands.19 The degree to which bipolar I, bipolar II, hypomania, cyclothymia, and unipolar depression are genetically related or distinct entities is unknown.20 It remains unclear if mood disturbance (phenotype) is the best indicator of a genetic etiology. Concerns of patients and their relatives can be dealt with through counseling.
Biochemical and pharmacologic studies led to catecholamine hypothesis to explain bipolar disorder, particularly mania, presuming that mania is due to an excess and depression is due to a depletion of catecholamines. Norepinephrine has been implicated mainly because of abnormalities linked with depression including its modulation by tricyclic antidepressants (TCAs). Dopamine has been implicated because the dopamine precursor L-dopa, amphetamines, and TCAs often produce hypomania in bipolar patients. Antipsychotic medications that selectively block dopamine receptors (e.g., pimozide) are effective against severe mania.
A number of serotonin hypotheses have been proposed, in isolation, or in relationship to other systems. The “permissive hypothesis” of serotonin function states that low serotonergic function accounts for both manic and depressive states through defective dampening of other neurotransmitters (mainly norepinephrine and dopamine).6 Some use this as an explanation as to why some bipolar patients do better on such antidepressants, including rare cases of mania that dissipate.
A wide range of neuroanatomical and neuroimaging studies are being conducted to learn more about bipolar disorder.19 Lesions in the frontal and temporal lobes are most frequently associated with bipolar disorder. Left-sided lesions tend to be associated with depression and right-sided lesions with mania, though differences may be reversed in the posterior regions of the brain (e.g., the association of depression with right parietooccipital lesions). No abnormalities have been found consistently via computed tomography (CT) studies, though ventricular enlargement has been suspected. Magnetic resonance imaging (MRI) studies reveal an increase in white matter intensities associated with bipolar disorder and correlated with age,21 though the clinical significance is unknown. Overall, most functional imaging studies (single-photon emission computer tomography [SPECT] and positron emission tomography [PET]) have noted prefrontal and anterior paralimbic hypoactivity in bipolar depression, while preliminary studies of manic patients have yielded inconsistent findings.
There are two other important biochemical models for bipolar disorder. Post and collaborators have proposed a model that electrophysiological kindling and behavioral sensitization underlie bipolar disorder, particularly the increasing frequency of episodes over time.22 Parallels between this model and bipolar disorder include the following: Predisposing effects of both genetic factors and early environmental stress; threshold effects (mild alterations eventually producing full-blown episodes); early episodes requiring precipitants while later ones do not; and repeated episodes of one phase leading to emergence of the other.19
Circadian rhythm desynchronization has also been implicated in bipolar disorder. Animal data indicate that periodic physiological disturbances can occur if two rhythms become desychronized (i.e., if one becomes free-running in and out of phase with the other).19 It is unclear if and how genetics contribute to the course (e.g., rapid cycling), circadian and seasonal rhythms, and the capacity for kindling and sensitization.
Cognitive processing is often impaired in bipolar patients, even in euthymic patients.23,24 Executive function, visulospatial, memory, verbal fluency, and attentional deficits have been noted. This may be a primary feature of bipolar disorder, secondary to other dysregulation (e.g., insomnia) or secondary to comorbid conditions (e.g., substance use). Cognitive assessment is underutilized in assessing medication side effects, the return to the outpatient sector from inpatient, and employing vocational rehabilitation in preparation for work.25
Diagnosis
The fourth edition of the Diagnostic and Statistical Manual of Mental Disorders Text Revision (DSM-IV-TR) includes bipolar I disorder, bipolar II disorder, cyclothymic disorder, and bipolar disorder not otherwise specified.26 The episodes are characterized by mania, hypomania, depressive, and mixed episodes. By definition, patients with bipolar I disorder have had at least one episode of mania. Those with bipolar II have had depressive and hypomanic episodes. Rapid cycling is technically four or more episodes per year, though many clinicians use the term to describe mood oscillations day to day. Mania occurring in the context of medication, substances, or medical illness is known as secondary mania and classified separately.
The reason for the sharp increase in epidemiological studies on “bipolar spectrum” is more systematic sampling and more sophisticated detection of patients with 1 to 2 symptoms (only) or those with 4 to 5 symptoms, which last 2 to 3 days—often placed in the bipolar not otherwise specified. This is an important determination, since many already responded adversely to standard antidepressants prescribed because the patients were previously diagnosed with depression.
The differential diagnosis of bipolar disorder is quite extensive and complex. First, the presentation of patients can be similar to other mood and psychotic disorders, including major depression, schizoaffective disorder, and schizophrenia. A positive family history of mood disorder is suggestive of a mood disorder, even when patients present with prominent psychotic symptoms. Second, bipolar disorder symptoms of recklessness, impulsivity, truancy, and other antisocial behavior are not unique versus substance, personality (borderline, antisocial, and others), and attention deficit hyperactivity disorders. Third, the relationship between affective illness and personality must be considered in making the diagnosis of bipolar disorder.
Bipolar disorder should always be considered in the differential diagnosis of patients with depression, as 3.9 perecent of patients converted to bipolar I disorder and 8.6 percent converted to bipolar II disorder upon follow-up over 2 to 11 years.27 Prospective predictors of bipolar I disorder were acute onset of depression, severity of the depressive episode, and psychosis, while predictors of bipolar II disorder included mood lability, higher rates of substance abuse, disruption of psychosocial functioning, and racing thoughts.19
Assessment
The evaluation of a bipolar patient involves a number of important clinical and psychosocial issues. The primary tool is the neuropsychiatric assessment with the history and physical examination. Brief histories (less than 30 minutes) may be a liability, due to the complexity of the mood course in patients not already diagnosed. Collateral information is required in most cases from family, friends, or prior places of treatment. A delineation of episodic versus chronic symptoms is helpful, except with patients with cycling of mood day-to-day, in a mixed episode, or otherwise very unstable course. Screening instruments can be used for manic episodes (e.g. Mood Disorder Questionnaire [MDQ]), though they may have more utility in primary care settings. The MDQ has 13 yes/no items, and seven positive answers call for a full clinical evaluation.15
The clinician must also assess for the presence of psychotic features, cognitive impairment, risk of suicide, risk of violence to persons or property, risk-taking behavior, sexually inappropriate behavior, and substance abuse. In addition, it is important to assess for the patient's ability to care for himself or herself, childbearing status or plans, housing, financial resources, and psychosocial supports. Again, accurate assessment depends on information from several sources since self-report of symptoms may conflict with observation by others.
Laboratory tests are used on a case-by-case basis and include level of thyroid stimulating hormone (TSH), urine or blood toxicology, a complete blood count (CBC), serum chemistries, electroencephalograms (EEGs), imaging studies, and erythrocyte sedimentation rate (ESR). Generally, head imaging is done early in the course to ensure a central cause is not missed, though rates of positive studies are low in community samples.
It is particularly important to detect episodes of secondary mania, previously recognized as a subtype of mania,19,28 but now as a substance-induced mania or mania due to a general medical condition. Correction of the underlying organic factor (infectious, toxic, and metabolic) may effectively reverse the manic presentation, but some factors are not reversible (e.g., stroke, steroids needed in ongoing way for COPD). Patients with mania originating in late life are more likely to have the following: a negative family history of affective disorder; irritability; treatment resistance; and a higher rate of mortality.19,28 Frequent etiologies of secondary mania are listed in Table 1.
Table 1.
Medical, surgical, and medication differential diagnosis for mania and depression
| Mania | Depression |
|---|---|
|
|
Management
Treatment guidelines. The American Psychiatric Association (APA) developed the Practice Guideline for the Treatment of Patients with Bipolar Disorder.9 The principles of psychiatric management are outlined in Table 2. A therapeutic alliance is crucial for understanding and managing the patient, detecting recurrence of illness, enhancing adherence, and addressing psychosocial stressors. Patients require ongoing education regarding the illness, treatment options, and the impact of the illness on social and family relationships, vocation, and financial issues. Graphic representation of the illness is a method to consolidate information (episode sequence, polarity, severity, frequency, and relationship to stressors and treatment), educate the patient, and may help to develop an alliance.29 For patients who are considering children or are pregnant, decision-making is best done in the therapeutic relationship.30
Table 2.
Principles of psychiatric management
| Principle | Comments |
|---|---|
|
|
The Expert Consensus Guideline Series is another well-known guideline.31 Medications may be functionally classified as those who target mania, depression, mixed/cycling, sleep, and other symptoms. Levels of evidence vary for all medications.32 The 2005 CANMAT guidelines33 (Canadian Network for Mood and Anxiety Treatments) are most comparable to the Expert Consensus Guideline, and it advocates a chronic disease model integrating patient, provider, and health delivery systems. Treatment selections are more based on efficacy data than tolerability. The section for older adults is substantially more detailed compared with other guidelines.
A summary of guidelines for episodes is in Table 3.
Table 3.
Summary of treatment guidelines for mood episodes in bipolar disorder
| EPISODE | APA | CONSENSUS GUIDELINE | CANMAT | OTHER EVIDENCE |
|---|---|---|---|---|
| Mania—euphoric | Lithium | Traditional (non-AAP) MS: lithium or valproate | N/A | Lithium |
| Mania—mild or moderate | Lithium or valproate | Traditional (non-AAP) MS: lithium or valproate | N/A | Valproate and/or AAP(1) |
| Mania—severe | Valproate or lithium with AAP | Valproate and AAP | N/A | Valproate and/or AAP(1) |
| Mania—mixed | Valproate | Traditional and AAP | N/A | Valproate or AAP |
| Rapid cycling—depression | MS(1) and MS(2) | Lamotrigine or lamotrigine/ lithium | Lithium Lamotrigine Valproate | Lamotrigine |
| Rapid cycling—mania | MS(1) and MS(2) | Valproate or valproate/AAP | Lithium Lamotrigine Valproate | Valproate |
| Depression—mild or moderate(2) | Optimize MS | N/A | N/A | N/A |
| Depression—severe | MS(1) and SSRI, MS(2), or ECT | N/A | N/A | N/A |
Key:
- APA—
American Psychiatric Association. In: Hirschfeld RMA, Bowden CL, Gitlin MJ, et al. Practice guideline for the treatment of patients with bipolar disorder (revision). Am J Psychiatry 2002;159(Suppl):1–35.
- Consensus Guideline—
Keck P, Perlis R, Otto M, et al. The Expert Consensus Guideline Series: Medication treatment of bipolar disorder 2004. Postgrad Med 2004;1–120.
- CANMAT—
Canadian Network for Mood and Anxiety Treatments
- AAP—
atypical antipsychotic
- MS—
mood stabilizer
- ECT—
electroconvulsive therapy
- 1—
Particularly if insomnia significant
- 2—
If no mood stabilizer, initiate one
- N/A—
Not addressed
Psychosocial treatments for bipolar disorder. Psychotherapeutic treatments, provided individually or through groups and families, are beneficial to nearly all patients with bipolar disorder and provide the context in which psychiatric management and pharmacotherapy work best.9 Most patients struggle with psychosocial issues (Table 2). Bipolar inpatients were surveyed about their informational needs in one study, and they requested information about bipolar disorder, how to obtain support, how to manage symptoms (e.g., suicidal ideation, anger), and how to improve interpersonal skills.34 Economic, interpersonal, and vocational problems may occur for years, even when patients do not suffer recurrence of illness leading to hospitalization.35
A summary of psychotherapeutic treatments reveals better outcomes and improved adherence to treatment.36 Cognitive-behavioral, family-focused psychoeducation (also known as behavioral family management), inpatient family, and group psychotherapy have been studied. Easy access to a primary nurse provider increases outpatient utilization without increasing costs.37 These interventions bridge the gap between ideal controlled trials and everyday practice, in which patients and families benefit from the increased structure of the interventions.
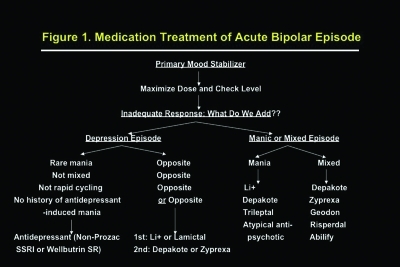
Medication selection. The choice of a mood stabilizer for the treatment of mania can be guided by predictors of response, which are usually determined by the patient's history and the type of episode (Figure 1).38 Several factors influence the selection of medication, including target symptoms, side effects, personal or family history of response, ease of adherence (QD, QHS, or BID preferable), the teratogenic profile for pregnant patients, and access to medications (e.g., cost formulary restrictions) (Table 4).
Figure 1.
Medication treatment of acute bipolar episode
Table 4.
Guidelines on how to select a mood-stabilizing medication for bipolar disorder
| Indication | Lithium | Carbamazepine oxcarbazepine | Valproate | Lamotrigine | Risperidone | Olanzapine | Quetiapine | Ziprasidone | Aripiprazole |
|---|---|---|---|---|---|---|---|---|---|
Mania
|
|
|
|
|
|
|
|
|
|
| Rapid cycling | ± | +? | + | + | ? | + | ? | ? | ? |
| Use in hepatic disease | + | ± | ? | + | + | +(1) | + | + | + |
| Use in renal disease | - | + | + | + | - | + | + | + | + |
| Use in rash patients | + | ± | + | ? | + | + | + | + | + |
| Medical-induced mania | - | + | + | ? | +? | + | ? | + | + |
| Violence/rapid stabilization | ?+ | ?+ | + | - | +? | + | ? | + | ? |
| Substance comorbidity | - | + | + | ? | ? | + | ? | ? | ? |
| Long-term depression | + | ? | ? | + | ? | +(2) | ? | ? | ? |
| FDA Class | D | D/C | D | C | C | C | C | C | C |
| Breastfeeding | - | + | + | - | - | - | - | - | - |
| Hormone effects | - | Ind. OC(3) | ? | - | Prolactin | - | - | - | - |
| Short-term side effects | Cognition Polydip. Tremor | Sedation Anemia LFT elev. | Sedation Weight gain LFT elev. | Rash Headache | Wt. gain EPS(4) Gluc. elev.(5) | Weight gain Sedation Gluc. elev | Gluc. elev | Agitation Sedation | Agitation |
| Long-term side effects | Thyroid Renal | Anemia | Pan's? PCO | - | T.D.? Chol. elev. | T.D.? Chol. elev. | T.D.? Chol. elev. | T.D.? | T.D.? |
| Dosing | 600-2400 (0.6–1.2) QD or BID | 400–1200/ 600–1800 BID | 750–2500(6) (50–125) BID | 100mg BID | 2–6mg BID | 5–20mg HS | 300–600mg BID | 40–80mg BID | 10–30mg AM |
Notes: Evidence base—haloperidol and thioridizine also FDA-approved for mania, but not commonly used.
- (1)
Olanzapine—Rare reports of LFT elevation
- (2)
Option to use combined form (olanzapine/fluoxetine = Symbyax).
- (3)
Induction of oral contraceptives—carbamazepine oxcarbazepine and topiramate.
- (4)
Risperdone—EPS = extrapyramidal side effects and TD = tardive dyskinesia.
- (5)
Glucose and cholesterol elevation—may be more for olanzapine, risperidone, and quetiapine than for ziprasidone and aripiprazole.
- (6)
Valproate ER dosed 500–3000mg HS.
Proportion of depression to mania: A high ratio implies eventual need for lithium, lamotrigine, or quetiapine, though others are effective for depression.
Cycling or mixed episodes: Mood stabilizer combination is likely, with an atypical for sleep and the other, probably an anticonvulsant, good for depression.
Medical illness/fluid shifts: Avoid lithium with old, renally impaired, or dehydrated patients.
Potential for overdose: Lithium with outpatient treatment reduces suicide risk clinically, but a one-month supply can be taken as a lethal dose. Other medications are generally safe.
Insomnia: Risperidone, olanzapine, quetiapine, and perhaps ziprasidone will help.
Low energy/drive: If an antidepressant is needed, bupropion provides energy and has a low rate of inducing mania.
Weight issues: Many patients are overweight or obese before treatment, and medications may add weight (lithium, valproate, risperidone, olanzapine, and quetiapine). Strategies for prevention of weight gain include diet, exercise, support groups, weight neutral medications, management of medical causes of weight gain (e.g. hypothyroidism), and other psychosocial approaches. Gradual weight loss with topiramate at doses of 200 to 400mg has been reported in uncontrolled trials.
Drug interactions: Avoid carbamazepine.
Black boxes: Nearly all medications have one (e.g., valproate—hepatotoxicity, lamotrigine—Steven's Johnson Syndrome).
Metabolic changes: See below.
Mood stabilizers for mania. Mood stabilizers are the mainstay of treatment for bipolar disorder, regardless of whether the patient's presentation is manic or depressed. These medications generally require 1 to 4 weeks at therapeutic doses before their full effects are seen. Approximately 50 to 60 percent of patients will respond sufficiently to a single mood stabilizer,39 while others may require combined pharmacotherapy.40 They are commonly used in conjunction with benzodiazepines (anxiety, agitation) and other medications.9
Extended-release forms are becoming increasingly meaningful to patients. Forms include Eskalith CR (lithium) and Depakote ER (valproate). Generally, they have fewer side effects than their counterpart immediate release (IR) forms, though some side effects persist since they are dose dependent. Cost may be an issue for some patients and organizations.
Lithium is effective for the treatment of acute mania, depressive episodes, and for the prevention of recurrent manic and depressive episodes. A review of 40 years of lithium treatment revealed that the dosage is generally between 600 and 2400mg/day with a therapeutic serum level between 0.8 and 1.2µg/mL.41 Common side effects of lithium include polydipsia, polyuria, weight gain, cognitive problems, tremor, gastrointestinal upset, acne, and hypothyroidism. Rare but potentially serious side effects include arrhythmias and toxicity (upon overdose). Laboratory monitoring includes serum levels to ensure adherence and adequate dosing, as well as annual electrolytes, TSH, and calcium. An EKG is recommended annually for those over 45 or with heart disease.
Valproate is approved for mania and it may offer broader coverage for irritable, mixed mania, and rapid cycling episodes.42 The dosage range of valproate IR (Depakene, Depakote) is 500 to 3500mg/day divided in two doses, and for extended release (ER), approximately the same given in only one dose per day, with a target plasma level between 75 and 125µg/mL. A loading dose strategy of 20–30mg/kg/day) more quickly reaches target levels and reduces symptoms.43 Common side effects of valproate include sedation, tremor, diarrhea, weight gain, alopecia, and benign elevation of liver transaminases. Rare but potentially serious side effects include leukopenia, thrombocytopenia, pancreatitis, and hepatotoxicity. Risk factors for hepatotoxicity may include an age of less than two years old, anticonvulsant polytherapy, developmental disability, and metabolic disorders.44 Data are conflicting regarding its relationship, if any, to polycystic ovarian disease.45 Laboratory monitoring includes levels as indicated to ensure adherence and adequate dosing, as well as baseline, three-month, six-month, and then annual liver function tests (LFTs) and complete blood count (CBC). If there is new-onset cognitive disturbance, an ammonia level may be helpful. Depakote is teratogenic if the fetus is exposed during pregnancy.
Carbamazepine has been approved by the Food and Drug Administration (FDA) for the treatment of bipolar mania in an extended release form (Equetro). The dosage range is generally between 400 and 1200mg/day. Levels are not correlated with response, though levels used in epilepsy (6–12µg/mL) are commonly attained. Carbamazepine initially has a long half-life, but it shortens to 12 to 16 hours after the first month, generally, and induces its metabolism and that of many other drugs by the liver. Common side effects include diplopia, blurred vision, fatigue, nausea, and ataxia. Rare but potentially serious side effects include skin rashes, leukopenia, hyponatremia, aplastic anemia, hepatic failure, exfoliative dermatitis (e.g., Stevens-Johnson Syndrome), pancreatitis, and neurotoxicity (upon overdose). Carbamazepine induces metabolism of many other medications (lowers their serum levels) and certain other drugs increase its level, resulting in toxicity.
Lamotrigine (Lamictal) is approved for maintenance treatment and is not effective alone for acute mania; it may assist other mood stabilizers, but that has not been proven. It must be slowly titrated up to 200mg (taken every morning) over six weeks to reduce the risk of Stevens-Johnson Syndrome (1/1000 in adults). Other side effects include dizziness, headache, double vision, somnolence, and rash. It may also help for bipolar depression and rapid cycling.46 No laboratory dosing is helpful or required.
Atypical antipsychotics are approved for mania. These help with psychosis and insomnia—better than antidepressants due to the latter's potential for inducing cycling. Sedation is sometimes a problem with olanzapine (Zyprexa) and quetiapine (Seroquel); the latter is approved at twice daily dosing, but some have attempted to use it only at bedtime. Nearly all but quetiapine may cause akithisia. There is a small chance of tardive dyskinesia (any), extrapyramidal side effects with risperidone (Risperdal) and ziprasidone (Geodon), and hyperprolactinemia with risperidone. An alternative mood stabilizer with strong efficacy is clozapine, but it is belabored by agranulocytosis, olanzapine's metabolic profile, seizures, hypersalivation, and tachycardia.
Abnormalities in glucose regulation have been reported in mental disorders (e.g., schizophrenia) for some time. A Consensus Development Conference concluded that obesity, diabetes, and dyslipidemia may be linked with an increase in body weight often seen in patients taking an atypical antipsychotic. Risk for weight gain, diabetes, and dyslipidemia is highest with clozapine and olanzapine, then risperidone and quetiapine, then aripiprazole and ziprasidone—though time will tell on these newer medications. The metabolic syndrome (MS) involves coronary artery disease, hypertension, dyslipidemia, glucose dysregulation, and obesity as core components.47 The Clinical Antipsychotic Trials of Intervention Effectiveness Schizophrenia Trial found 40.9 percent prevalence of MS in patients with schizophrenia.48 Metabolic effects of drugs can be monitored by assessing weight, body mass index (BMI), glucose, cholesterol, and high-density lipoprotein screening.49
A review of head-to-head trials before 2004 shows few differences for acute mania,38 though a few studies of valproate and olanzapine (including maintenance follow-up) revealed slight advantages to olanzapine in response and remission, at a cost of increased sedation and weight gain.50
Adjuvant medication, combination strategies, and other options for mania. Adjuvant medication to the primary mood stabilizer includes other mood stabilizers (mood), the benzodiazepines (agitation, insomnia) and antipsychotics (insomnia, agitation, psychosis). A review of polypharmacy discusses open trials of mood stabilizer combinations.51 Patients whose insomnia is treated with sedating antidepressants compared to benzodiazepines have shorter asymptomatic periods between mood episodes.52
Electroconvulsive therapy (ECT) is available for patients who are pregnant, unresponsive to more standard treatments, or unable tolerate first-line treatments. ECT may work rapidly,53 succeed in medication-resistant patients,54 and work in a maintenance fashion.55 For patients who are manic or depressed during the first trimester of pregnancy, ECT is usually the safest and most effective treatment.9
Other treatments are available for patients who are unresponsive to or unable to tolerate more standard treatments or unable tolerate first-line treatments and include clozapine, calcium channel antagonists, and thyroid supplementation rarely used for cycling patients.
Types of mania and response to medication. Euphoric. Patients with euphoric or pure mania respond to lithium between 59 and 91 percent of the time, and at slightly lower rates to valproate treatment.38
Dysphoric or mixed. This is severe, difficult to treat, and common.19 A review of studies revealed associations with suicidality, an earlier age of onset, longer episode duration, higher rates of personal and family depression, higher concomitant alcohol or sedative-hypnotic abuse, more neuropsychiatric abnormalities, and a poorer outcome.56 Patients in acute episodes of mixed mania respond better to valproate than lithium.38 Most atypical antipsychotics have an indication, too, for mixed mania, though combinations are often needed.
Rapid cycling. Cycling ranges from four or more per year (rapid cycling: 15–20%) to those occurring from weeks to several days (ultra-rapid cycling) to distinct, abrupt shifts of less than 24 hours (ultradian cyclers).57 Cyclers are more likely to be female, have associated hypothyroidism,58 and lower likelihood of recovery in the second year of follow-up, but not permanently.57 It may be a parameter of treatment resistance, in general, with many patients not responding even to combinations of mood stabilizers.59 Conceptually, treatment parallels mixed episodes. In acute episodes, patients with a rapid cycling pattern appear to respond better to quetiapine,60 lamotrigine,46 or valproate.58,61 Other treatment options include adding thyroid hormone to a mood stabilizer (at a dose to achieve 150% of normal function58) using a combination of standard mood stabilizers, clozapine as a monotherapy, and clozapine in combination with lithium or valproate.
Populations. All studies have been completed in adults. More data are needed on child, adolescent, and geriatric patients. In elderly patients and those with secondary mania, adverse events often limit the usefulness of lithium and carbamazepine28 in favor of valproate (or by clinical experience, atypical antipspychotics).
Bipolar depression. Treatment of bipolar depression may involve a mood stabilizer, psychotherapy, antidepressant, and/or ECT.9 One challenging aspect is defining populations: bipolar I, bipolar II, mixed, cycling or sub-mixed (i.e., acute mania accompanied by some depressive symptoms). For patients who are not taking a mood stabilizer when they become depressed (or not taking an adequate dosage), a mood-stabilizing medication should be used at adequate blood levels, preferably with psychotherapy for support. Most stabilizers have some antidepressant activity, but if the depression is severe, an antidepressant may be started simultaneously. Quetiapine monotherapy and olanzapine in combination with fluoxetine are effective in controlled trials. A full response may require 4 to 6 weeks.9 For patients already taking an adequate dose of a mood stabilizer when they become depressed, the augmentation with psychotherapy, an antidepressant, or an additional mood stabilizer (for cycling or mixed episodes) may be carried out. ECT is efficacious, works rapidly, and is usually the safest treatment in the first trimester of pregnancy.9 Antidepressants have not been shown to increase the rate of new-onset suicidal ideation.62
Lithium, lamotrigine, olanzapine combined with fluoxetine, and quetiapine are the mood stabilizers of choice for bipolar depression,60,63–65 though several types of depression respond well to valproate.66 There are few trials, though, that meet the highest standard of rigor.39 Effect sizes for quetiapine montherapy and olanzapine combined with fluoxetine were significantly more than for olanzapine monotherapy. ECT remains the most effective treatment for bipolar depression.54
The addition of an antidepressant to the medication regimen for patients with bipolar depression raises special concerns, since antidepressants can provoke manic, mixed, cycling, or hypomanic symptoms. This is particularly true in substance users.67 Whenever possible, psychiatric management and psychotherapy should be maximized before the addition of an antidepressant. The patient (and his or her family) must be educated about the risk of a switch to mania, its warning signs, and a plan for immediate intervention. Antidepressant-induced mania accounts for one-third of episodes in treatment-refractive bipolar patients,68 and higher with venlafaxine XR.69 It is unclear if this data applies to experimental treatments with dopamine (D) or noradrenergic (NA) action: pramipexole (D2/D3), duloxetine (NA) and modafonil (NA/D).
An estimated 30 to 50 percent of patients do not respond to a first-line treatment and require a longer trial (6–12 weeks), an alternate antidepressant, or augmentation of the antidepressant with lithium, psychotherapy, or thyroid hormone.63 Lamotrigine,70 pramipexole,71 and ECT may work for treatment-resistant forms. Once the patient is in remission, the duration of the antidepressant trial depends on the patient's history, ranging from a few months to long-term.63
Comorbidity in Bipolar Disorder
Comorbid psychiatric disorders in individuals with bipolar disorder are associated with poorer outcome and poorer treatment response,72 increased service utilization, and increased cost. Substance use, attention deficit hyperactivity, anxiety, and impulse control disorders are the most common.
Substance disorders. The National Comorbidity Study showed that bipolar disorder was associated with the highest risk for coexistence with a drug or alcohol use disorder (over 60% for bipolar I and 48% for bipolar II) and a lifetime prevalence of over 90 percent.1 Alcohol and marijuana are most frequently used, with alcohol higher in women. Generally, there are higher rates of mixed episodes, cycling, impulsivity, and aggression. These patients are high utilizers of healthcare services, including emergency rooms and hospitals.
There is a great deal of inherent difficulty in diagnosing bipolar disorder when the patient also has a substance use disorder because drugs of abuse, particularly with chronic use, can mimic both mania and depression. It seems most reasonable to ask very specifically about affective symptoms predating the onset of substance use and during abstinent periods and to diagnose an affective disorder only if symptoms clearly predated the substance use or persist during periods of abstinence.
Several studies indicate these patients have a more difficult course of illness and are more treatment-resistant.73 Anticonvulsants may offer neuroprotection and reduce impulsivity. Carbamazepine, valproate, and other anticonvulsants may serve as alternatives to benzodiazepines for alcohol withdraw.74 Valproate also has been shown to reduce alcohol use in a maintenance fashion,75 and it and others are now being studied for cocaine and opiate disorders for patients with and without bipolar disorder. Involvement of the patient in psychosocial rehabilitation, cognitive-behavioral therapy, and group therapy (e.g., family, 12-step) is essential. Residential or intensive outpatient programs may also be useful.
Attention deficit hyperactivity disorder (ADHD). ADHD commonly occurs with bipolar disorder, particularly in comparison to unipolar.76,77 Symptoms of ADHD include poor concentration, distractibility, impulsivity, restlessness, and agitation that are also features of a manic or hypomanic episode. It is important to inquire about the episodic or chronic nature of the symptoms and to inquire about symptoms, which are more specific to mania, such as elated mood, grandiosity, hypersexuality, and decreased need for sleep. When in doubt, treatment with a mood stabilizer first is low risk, followed by an assessment of ADHD symptoms. Finally, if a decision is made to treat ADHD in an individual with bipolar disorder, it is important to avoid agents that might precipitate mania and/or worsen the course of bipolar disorder (e.g., stimulants). Clonidine may be a reasonable alternative to antidepressant or stimulant treatment.78
Anxiety disorders. Several investigators have reported higher rates of one (55.8%) or more (31.8%) anxiety disorders,15,79 with panic (20.8%), generalized anxiety (30.0%), social anxiety (7.8–47.2%), obsessive compulsive (3.2–35.0%), and posttraumatic stress (38.1%) disorders. These anxiety disorders worsen the course and prognosis of bipolar disorder.80
As with the treatment of ADHD, many of the first-line pharmacologic treatments for anxiety disorders (antidepressants) can precipitate mania and must be used with caution. No randomized controlled trials have been conducted with these comorbidities, but some data exist: Valproate for panic disorder; lamotrigine, risperidone, and olanzapine for posttraumatic stress disorder; and risperidone, olanzapine, and quetiapine as adjunctive treatment to SSRI-refractory obsessive-compulsive disorder.81 Gabapentin and pregabalin may not help with mood, but have helped in social and generalized types of anxiety, respectively.81
Personality disorders. The relationship between bipolar disorder and personality is a complex one, both from a theoretical and diagnostic perspective. A number of possible relationships between bipolar disorder and personality have been considered.82,83 Studies of specific personality disorders in bipolar patients have found high rates of cluster B diagnoses and particularly high rates of borderline personality disorder. Some of the criteria for borderline personality disorder and hypomania overlap, but borderline personality is known for the idealization/devaluation, abandonment, lack of identity, and other features (e.g., a more chronic course).
Natural History and Course
The natural course of bipolar disorder is characterized by high rates of relapse and recurrence,19 at rates of 80 to 90 percent,84 at an average of 0.6 episodes per year over a five-year period.85 In prospective outcome studies extending up to four years, less than half of patients followed after an initial manic episode had sustained a good response to treatment.84 Full functional recovery between affective episodes often lags behind symptomatic recovery.35,86 First-episode mania was associated with a significantly shorter hospitalization.85 Data have largely been derived from naturalistic studies and controlled trials, whose treatments may be biased by increased adherence.
Many questions remain regarding predictors of recurrence. The cumulative probability of recurrence during the first year of follow-up was more than 50 percent, by the end of the four years was about 70 percent, and by five years was nearly 90 percent.84,87 Patients with residual symptoms after the acute episode88 or six months after their first episode84 have greater chance of mania or major depression recurrence. There is conflicting data as to whether age of onset, sex, premorbid psychosocial function, number of years ill, and the number of prior episodes predict recurrence.89
Maintenance Treatment
Acute treatment usually occurs between 0 and 8 weeks, with continuation up to six months and then maintenance thereafter. It is usually defined as “following a period of sustained remission.” The goal is to prevent further episodes. Medication selection during the acute episode can be based partly on maintenance factors, with attention to side effects and the patient's natural history. Many patients need more than one medication, and as such, rational combinations are critical to prevent relapse and avoid exacerbations (e.g., induction of depression). Symptom, functional, and vocational stability is desired.
Maintenance treatment with mood stabilizers is better studied over the past decade, but further studies are needed. Only 33 percent of patients on lithium remained symptom free at five years, and combining lithium with other mood stabilizers, benzodiazepines, or antipsychotics provided greater prophylaxis.90 Although overall lithium had a slight advantage over carbamazepine in a 2.5-year maintenance study, this appeared to be confined to patients with classical presentations.91 A comparison of lithium and lamotrigine over 18 months revealed the former more prophylactic against mania and the latter more prophylactic against depression.92 Olanzapine was superior to placebo and comparable to lithium,93 and versus valproate it had shorter time to symptomatic mania remission.94 Aripiprazole is superior to placebo in studies,95 and valproate over one year increased time to depression relapse compared to lithium.9
Combination therapy may have advantages, in general, compared to monotherapy long-term and is significantly increasing.96 Lithium,38,92 olanzapine,97 and valproate39 have been studied with others, revealing enhanced remission and time to intervention.
Conclusions
Bipolar disorder is a major public health problem associated with significant morbidity and a high mortality risk. Several factors make treatment complex, including the fluctuation of mood episodes and the effects of these episodes on patient well-being, treatment nonadherence, and comorbid psychiatric disorders. Guidelines are available for mania, depression, and other episodes. A number of pharmacologic and psychosocial treatments are under study in randomized trials.
Contributor Information
Donald M. Hilty, Dr. Hilty is Associate Professor of Clinical Psychiatry and Behavioral Sciences at University of Califorinia, Davis.
Martin H. Leamon, Dr. Leamon is Associate Professor of Clinical Psychiatry and Behavioral Sciences at University of Califorinia, Davis.
Russell F. Lim, Dr. Lim is Associate Clinical Professor of Psychiatry at University of Califorinia, Davis.
Rosemary H. Kelly, Dr. Kelly is Intructor, Department of Psychiatry, and Faculty, Certificate Program in Infant Mental Health, University of Washington.
Robert E. Hales, Dr. Hales is Joe Tupin Professor and Chair of Psychiatry and Behavioral Sciences, University of California, Davis..
References
- 1.Kessler RC, Bergland P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 2.Ghaemi SN. Bipolar disorder and antidepressants: an ongoing controversy. Primary Psychiatry. 2001;8(2):28–34. [Google Scholar]
- 3.Prien RF, Potter WZ. NIMH workshop report on treatment of bipolar disorder. Psychopharmacol Bull. 1990;26:409–27. [PubMed] [Google Scholar]
- 4.Quanbeck CD, Stone DC, Scott CL, et al. Clinical and legal correlates of inmates with bipolar disorder at time of criminal arrest. J Clin Psychiatry. 2004;65:198–203. doi: 10.4088/jcp.v65n0209. [DOI] [PubMed] [Google Scholar]
- 5.Judd LL, Akiskal HS, Schettler PJ, et al. The long-term natural history of the weekly symptomatic status of bipolar disorder. Arch Gen Psychiatry. 2002;59:530–7. doi: 10.1001/archpsyc.59.6.530. [DOI] [PubMed] [Google Scholar]
- 6.Hilty DM, Brady KT, Hales RE. Bipolar disorder in adults: A review of recent literature. Psychiatric Services. 1999;50:201–13. doi: 10.1176/ps.50.2.201. [DOI] [PubMed] [Google Scholar]
- 7.Belmaker RH. Bipolar disorder. N Eng J Med. 2004;351:476–86. doi: 10.1056/NEJMra035354. [DOI] [PubMed] [Google Scholar]
- 8.Chang KD, Ketter TA. Special issues in the treatment of paediatric bipolar disorder. Exp Opin Pharmacother. 2001;2(4):613–22. doi: 10.1517/14656566.2.4.613. [DOI] [PubMed] [Google Scholar]
- 9.Hirschfeld RMA, Bowden CL, Gitlin MJ, et al. Practice guideline for the treatment of patients with bipolar disorder (revision) [April 14, 2006];Am J Psychiatry. 2002 159(Suppl):1–35. Available at: www.psych.org/psych_pract/treatg/pg/prac_guide.cfm. [PubMed] [Google Scholar]
- 10.Sachs GS. Decision tree for the treatment of bipolar disorder. J Clin Psychiatry. 2003;64(Suppl 5):35–40. [PubMed] [Google Scholar]
- 11.Glick ID, Suppes T, DeBattista C, et al. Pharmacologic treatment strategies for depression, bipolar disorder, and schizophrenia. Ann Int Med. 2001;134:47–60. doi: 10.7326/0003-4819-134-1-200101020-00013. [DOI] [PubMed] [Google Scholar]
- 12.Suppes T, Dennehy EB, Hirschfeld RMA, et al. Texas implementation of medication algorithms: Update to the algorithms for treatment of bipolar I disorder. J Clin Psychiatry. 2005;66:870–86. doi: 10.4088/jcp.v66n0710. [DOI] [PubMed] [Google Scholar]
- 13.Hatfield AB, Gearon JS, Coursey RD. Family members' ratings of the use and value of mental health services: Results of a national NAMI survey. Psychiatric Services. 1996;47:825–31. doi: 10.1176/ps.47.8.825. [DOI] [PubMed] [Google Scholar]
- 14.Weissman MM, Leaf PJ, Tischer GL, et al. Affective disorders in five United States communities. Psychol Med. 1988;18:141–53. doi: 10.1017/s0033291700001975. [DOI] [PubMed] [Google Scholar]
- 15.Hirschfeld RMA, Holzer C, Calabrese JR, et al. Validity of the mood disorder questionnaire: A general population study. Am J Psychiatry. 2003;160:178–80. doi: 10.1176/appi.ajp.160.1.178. [DOI] [PubMed] [Google Scholar]
- 16.Hirschfeld RM. Bipolar spectrum disorder: improving its recognition and diagnosis. J Clin Psychiatry. 2001;62(Suppl 14):5–9. [PubMed] [Google Scholar]
- 17.Lish JD, Dime-Meenan S, Whybrow PC, et al. The National Depressive and Manic-Depressive Association (DMDA) survey of bipolar members. J Affect Disord. 1994;31:281–94. doi: 10.1016/0165-0327(94)90104-x. [DOI] [PubMed] [Google Scholar]
- 18.Matza LS, Rajagopalan KS, Thompson CL, de Lissovoy G. Misdiagnosed patients with bipolar disorder: Comorbidities, treatment patterns, and direct treatment costs. J Clin Psychiatry. 2005;66(11):1432–40. doi: 10.4088/jcp.v66n1114. [DOI] [PubMed] [Google Scholar]
- 19.Goodwin FK, Jamison KR. Manic-Depressive Illness. New York, NY: Oxford University Press; 1990. [Google Scholar]
- 20.Reus VI, Freimer NB. Understanding the genetic basis of mood disorders: Where do we stand? Am J Human Gen. 1997;60:1283–8. doi: 10.1086/515482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Altshuler LL, Curran JG, Hauser P, Mintz J. T2 hyperintensities in bipolar disorder: Magnetic resonance imaging comparison and literature meta-analysis. Am J Psychiatry. 1995;152:1139–44. doi: 10.1176/ajp.152.8.1139. [DOI] [PubMed] [Google Scholar]
- 22.Post RM, Rubinow DR, Ballenger JC. Conditioning, sensitization, and kindling: Implications for the course of affective illness. In: Post RM, Ballenger JC, editors. The Neurobiology of Mood Disorders. Baltimore, MD: Williams &Wilkins; 1984. [Google Scholar]
- 23.Nordenson B, Gruber SA, Yurgelun-Todd DA. Neurocognition in bipolar disorder: A review of the current research. Curr Psychosis Ther Rep. 2004;2:147–52. [Google Scholar]
- 24.Martinez-Aran A, Vieta E, Reinares M, et al. Cognitive function across manic or hypomanic, depressed, and euthymic states in bipolar disorder. Am J Psychiatry. 2004;161:262–70. doi: 10.1176/appi.ajp.161.2.262. [DOI] [PubMed] [Google Scholar]
- 25.Dickerson FB, Boronow JJ, Stallings CR, et al. Association between cognitive functioning and employment status of persons with bipolar disorder. Psychiatr Serv. 2004;55:54–8. doi: 10.1176/appi.ps.55.1.54. [DOI] [PubMed] [Google Scholar]
- 26.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, DC: American Psychiatric Press, Inc.; 2000. [Google Scholar]
- 27.Akiskal HS, Maser JD, Zeller PJ, et al. Switching from “unipolar” to bipolar II. Arch Gen Psychiatry. 1995;52:114–23. doi: 10.1001/archpsyc.1995.03950140032004. [DOI] [PubMed] [Google Scholar]
- 28.Evans DL, Byerly MJ, Greer RA. Secondary mania: Diagnosis and treatment. J Clin Psychiatry. 1995;56(Suppl 3):31–7. [PubMed] [Google Scholar]
- 29.Post RM, Roy-Byrne PP, Uhde TW. Graphic representation of the life course of illness in patients with affective disorder. Am J Psychiatry. 1998;45:844–8. doi: 10.1176/ajp.145.7.844. [DOI] [PubMed] [Google Scholar]
- 30.Hilty DM, Kelly RH, Hales RE. Diagnosis and treatment of bipolar disorder in pregnant women. Primary Care Update OB/GYN. 2000;7:105–12. doi: 10.1016/s1068-607x(00)00030-5. [DOI] [PubMed] [Google Scholar]
- 31.Keck PE, Perlis R, Otto M, et al. The expert consensus guideline series: Medication treatment of bipolar disorder 2004. Postgrad Med. 2004:1–120. [PubMed] [Google Scholar]
- 32.Ketter TA, editor. Advances in the Treatment of Bipolar Disorders. Washington, DC: American Psychiatric Press, Inc.; 2005. pp. 36–47. [Google Scholar]
- 33.Yatham LN, Kennedy SH, O'Donovan C, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) guidelines for the management of patients with bipolar disorder: Consensus and controversies. Bipolar Disord. 2005;7(Suppl 3):5–69. doi: 10.1111/j.1399-5618.2005.00219.x. [DOI] [PubMed] [Google Scholar]
- 34.Pollack LE. Informational needs of patients hospitalized for bipolar disorder. Psychiatr Serv. 1995;46:1191–4. doi: 10.1176/ps.46.11.1191. [DOI] [PubMed] [Google Scholar]
- 35.Coryell W, Scheftner W, Keller M, et al. The enduring psychosocial consequences of mania and depression. Am J Psychiatry. 1993;50:720–7. doi: 10.1176/ajp.150.5.720. [DOI] [PubMed] [Google Scholar]
- 36.Sajatovic M, Davies M, Hrouda DR. Enhancement of treatment adherence among patients with bipolar disorder. Psychiatr Serv. 2004;55:264–9. doi: 10.1176/appi.ps.55.3.264. [DOI] [PubMed] [Google Scholar]
- 37.Bauer MS, McBride L, Shea N, et al. Impact of an easy-access VA clinic-based program for patients with bipolar disorder. Psychiatr Serv. 1997;48:491–6. doi: 10.1176/ps.48.4.491. [DOI] [PubMed] [Google Scholar]
- 38.Bowden CL. Predictors of response to divalproex and lithium. J Clin Psychiatry. 1995;56(Suppl 3):25–30. [PubMed] [Google Scholar]
- 39.Bauer MS, Mitchner L. What is a “mood stabilizer”? An evidence-based response. Am J Psychiatry. 2004;161:3–18. doi: 10.1176/appi.ajp.161.1.3. [DOI] [PubMed] [Google Scholar]
- 40.Mondimore FM, Fuller GA, DePaulo JR., Jr Drug combinations for mania. J Clin Psychiatry. 2003;64(Suppl 5):25–31. [PubMed] [Google Scholar]
- 41.Schou M. Forty years of lithium treatment. Arch Gen Psychiatry. 1997;54:9–13. doi: 10.1001/archpsyc.1997.01830130013002. [DOI] [PubMed] [Google Scholar]
- 42.Keck PE, McElroy SL. Divalproex in the treatment of bipolar disorder. Pharm Bull. 2003;37(Suppl 2):67–73. [PubMed] [Google Scholar]
- 43.Hirschfeld RMA, Baker JD, Wozniak P, Tracy K. The safety and early efficacy of oral-loaded divalproex verses standard-titration Divalproex, lithium, olanzapine, and placebo in the treatment of acute mania associated with bipolar disorder. J Clin Psychiatry. 2003;64(7):841–6. doi: 10.4088/jcp.v64n0717. [DOI] [PubMed] [Google Scholar]
- 44.Bryant AE, Dreifuss FE. Valproic acid hepatic fatalities, III. U.S. experience since 1986. Neurology. 1996;46:465–9. doi: 10.1212/wnl.46.2.465. [DOI] [PubMed] [Google Scholar]
- 45.Ferin M, Morrell M, Xiao E, et al. Endocrine and metabolic responses to long-term monotherapy with antiepileptic drug valproate in the normally cycling rhesus monkey. J Clin Endocrinol Metab. 2003;88:2908–15. doi: 10.1210/jc.2002-021614. [DOI] [PubMed] [Google Scholar]
- 46.Calabrese JR, Suppes T, Bowden CT, Sachs G. A double-blind, placebo-controlled, prophylaxis study of lamotrigine in rapid-cycling bipolar disorder. J Clin Psychiatry. 2000;61:841–50. doi: 10.4088/jcp.v61n1106. [DOI] [PubMed] [Google Scholar]
- 47.Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 48.McEvoy JP, Meyer JM, Goff DC, et al. Prevalence of the metabolic syndrome in patients with schizophrenia: Baseline results from the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) schizophrenia trial and comparison with national estimates from NHANES III. Schiz Res. 2005;80:19–32. doi: 10.1016/j.schres.2005.07.014. [DOI] [PubMed] [Google Scholar]
- 49.Keck PE, McElroy SL. Bipolar disorder, obesity, and pharmacotherapy-associated weight gain. J Clin Psychiatry. 2003;64(12):1426–35. doi: 10.4088/jcp.v64n1205. [DOI] [PubMed] [Google Scholar]
- 50.Tohen M, Ketter TA, Zarate CA, Suppes T. Olanzapine versus divalproex sodium for the treatment of acute mania and maintenance of remission: a 47-week study. Am J Psychiatry. 2003;160:1263–71. doi: 10.1176/appi.ajp.160.7.1263. [DOI] [PubMed] [Google Scholar]
- 51.Solomon DA, Keitner GI, Ryan CE, et al. Polypharmacy in bipolar I disorder. Psychopharmacol Bull. 1996;32:579–87. [PubMed] [Google Scholar]
- 52.Saiz-Ruiz J, Cebollada A, Ibanez A. Sleep disorders in bipolar depression: hypnotics versus sedative antidepressants. J Psychosom Res. 1994;38(Suppl):55–60. doi: 10.1016/0022-3999(94)90136-8. [DOI] [PubMed] [Google Scholar]
- 53.Mukherjee S, Sackeim HA, Schnurr DB. Electroconvulsive therapy of acute manic episodes: A review. Am J Psychiatry. 1994;151:169–76. doi: 10.1176/ajp.151.2.169. [DOI] [PubMed] [Google Scholar]
- 54.Mukherjee S, Sackeim HA, Lee C. Unilateral ECT in the treatment of manic episodes. Convulsive Ther. 1988;4:74–80. [PubMed] [Google Scholar]
- 55.Vanelle JM, Loo H, Galinowski A, et al. Maintenance ECT in intractable manic-depressive disorders. Convulsive Ther. 1994;10:195–205. [PubMed] [Google Scholar]
- 56.McElroy SL, Keck PE, Jr, Pope HG, et al. Clinical and research implications of the diagnosis of dysphoric or mixed mania or hypomania. Am J Psychiatry. 1992;149:1633–44. doi: 10.1176/ajp.149.12.1633. [DOI] [PubMed] [Google Scholar]
- 57.Coryell W, Endicott J, Keller M. Rapidly cycling affective disorder. Arch Gen Psychiatry. 1992;49:126–31. doi: 10.1001/archpsyc.1992.01820020046006. [DOI] [PubMed] [Google Scholar]
- 58.Bauer MS, Whybrow PC. Rapid cycling bipolar affective disorder. Arch Gen Psychiatry. 1990;47:435–40. doi: 10.1001/archpsyc.1990.01810170035006. [DOI] [PubMed] [Google Scholar]
- 59.Calabrese JR, Keck PE, MacFadden W, et al. A randomized, double-blind, placebo-controlled trial of quetiapine in the treatment of bipolar I or II depression. Am J Psychiatry. 2005;162:1351–60. doi: 10.1176/appi.ajp.162.7.1351. [DOI] [PubMed] [Google Scholar]
- 60.Calabrese JR, Shelton MD, Rapport DJ, et al. A 20-month, double-blind, maintenance trial of lithium versus Divalproex in rapid-cycling bipolar disorder. Am J Psychiatry. 2005;162:2152–61. doi: 10.1176/appi.ajp.162.11.2152. [DOI] [PubMed] [Google Scholar]
- 61.Calabrese JR, Markovitz PJ, Kimmel SE, et al. Spectrum of efficacy of valproate in 78 rapid-cycling bipolar patients. J Clin Psychopharmacol. 1992;12(Suppl):53–6. doi: 10.1097/00004714-199202001-00008. [DOI] [PubMed] [Google Scholar]
- 62.Bauer MS, Wisniewski SR, Marangell LB, et al. Are antidepressants associated with new-onset suicidality in bipolar disorder? A prospective study of participants in the Systematic Treatment Enhancement Program for Bipolar (STEP-BD) J Clin Psychiatry. 2006;67:48–55. doi: 10.4088/jcp.v67n0108. [DOI] [PubMed] [Google Scholar]
- 63.Frances A, Docherty JP, Kahn DA. Treatment of bipolar disorder. J Clin Psychiatry. 1996;57(Suppl 12A):1–88. [PubMed] [Google Scholar]
- 64.Zornberg GL, Pope HG. Treatment of depression in bipolar disorder: New directions for research. J Clin Psychopharmacol. 1993;13:397–408. [PubMed] [Google Scholar]
- 65.Gao K, Gajwani P, Elhaj O, Calabrese JR. Typical and atypical antipsychotics in bipolar depression. J Clin Psychiatry. 2005;66:1376–85. doi: 10.4088/jcp.v66n1106. [DOI] [PubMed] [Google Scholar]
- 66.Davis LL, Bartolucci A, Petty F. Divalproex in the treatment of bipolar depression: A placebo-controlled study. J Aff Disorders. 2005;85:259–66. doi: 10.1016/j.jad.2004.09.009. [DOI] [PubMed] [Google Scholar]
- 67.Goldberg JF, Whiteside JE. The association between substance abuse and antidepressant-induced mania in bipolar disorder: a preliminary study. J Clin Psychiatry. 2002;63(9):791. doi: 10.4088/jcp.v63n0907. [DOI] [PubMed] [Google Scholar]
- 68.Altshuler LL, Post RM, Leverich GS, et al. Antidepressant-induced mania and cycle acceleration: a controversy revisited. Am J Psychiatry. 1995;152:1130–8. doi: 10.1176/ajp.152.8.1130. [DOI] [PubMed] [Google Scholar]
- 69.Leverich GS, Altshuler LL, Frye MA, et al. Risk of switch in mood polarity to hypomania or mania in patients with bipolar depression during acute and continuation trials of venlafaxine, sertraline and bupropion as adjuncts to mood stabilizers. J Clin Psychiatry. 2006;163:232–39. doi: 10.1176/appi.ajp.163.2.232. [DOI] [PubMed] [Google Scholar]
- 70.Nierenberg AA, Ostacher MJ, Calabrese JR, et al. Treatment-resistant bipolar depression: A STEP-BD equipoise randomized effectiveness trial of antidepressant augmentation with lamotrigine, inositol or risperidone. Am J Psychiatry. 2006;163:210–6. doi: 10.1176/appi.ajp.163.2.210. [DOI] [PubMed] [Google Scholar]
- 71.Goldberg JF, Burdick KE, Endick CJ. Preliminary randomized, double-blind, placebo-controlled trial of pramipexole added to mood stabilizers for treatment resistance bipolar depression. Am J Psychiatry. 2004;161(3):564–6. doi: 10.1176/appi.ajp.161.3.564. [DOI] [PubMed] [Google Scholar]
- 72.Keitner GI, Ryan CE, Miller IW, et al. Twelve-month outcome of patients with major depression and comorbid psychiatric or medical illness (compound depression) Am J Psychiatry. 1991;148:345–50. doi: 10.1176/ajp.148.3.345. [DOI] [PubMed] [Google Scholar]
- 73.Strakowski SM, Tohen M, Stoll AL, et al. Comorbidity in mania at first hospitalization. Am J Psychiatry. 1992;49:554–6. doi: 10.1176/ajp.149.4.554. [DOI] [PubMed] [Google Scholar]
- 74.Brady KT, Sonne SC, Anton R, et al. Valproate in the treatment of acute bipolar affective episodes complicated by substance abuse: a pilot study. J Clin Psychiatry. 1995;56:118–21. [PubMed] [Google Scholar]
- 75.Brady KT, Myrick H, Henderson S, Coffey SF. The use of divalproex in alcohol relapse prevention: a pilot study. Drug Alcoh Depend. 2002;67(3):323–30. doi: 10.1016/s0376-8716(02)00105-9. [DOI] [PubMed] [Google Scholar]
- 76.Winokur G, Coryell W, Endicott J. Further distinctions between manic-depressive illness (bipolar disorder) and primary depressive disorder (unipolar depression) Am J Psychiatry. 1993;50:1176–81. doi: 10.1176/ajp.150.8.1176. [DOI] [PubMed] [Google Scholar]
- 77.Strober M, Morrell W, Burroughs J, et al. A family study of bipolar I disorder in adolescence. Early onset of symptoms linked to increased familial loading and lithium resistance. J Affective Dis. 1988;15:255–68. doi: 10.1016/0165-0327(88)90023-7. [DOI] [PubMed] [Google Scholar]
- 78.Spencer T, Biederman J, Wilens T, et al. Pharmacotherapy of attention-deficit hyperactivity disorder across the life cycle. J Am Acad Child Adol Psychiatry. 1996;35:409–32. doi: 10.1097/00004583-199604000-00008. [DOI] [PubMed] [Google Scholar]
- 79.Boylan KR, Bielling PJ, Marriott M, Begin LT, et al. Impact of comorbid anxiety disorders on outcome in a cohort of patients with bipolar disorder. J Clin Psychiatry. 2004;65:1106–13. doi: 10.4088/jcp.v65n0813. [DOI] [PubMed] [Google Scholar]
- 80.Keller MB. Prevalence and impact of comorbid anxiety and bipolar disorder. J Clin Psychiatry. 2006;67(Suppl 1):5–7. [PubMed] [Google Scholar]
- 81.Keck PE, Strawn JR, McElroy SL. Pharmacologic treatment considerations in co-occurring bipolar and anxiety disorders. J Clin Psychiatry. 2006;67(Suppl 1):8–15. [PubMed] [Google Scholar]
- 82.Kopacz DR, Janicak PG. The relationship between bipolar disorder and personality. Psychiatr Ann. 1996;26:644–50. [Google Scholar]
- 83.Akiskal HS. Subaffective disorders: Dysthymic, cyclothymic and bipolar II disorders in the “borderline” realm. Psychiatric Clin N Am. 1981;4:25–46. [PubMed] [Google Scholar]
- 84.Tohen M, Waternaux CS, Tsuang MT. Outcome in mania: A 4-year prospective follow-up of 75 patients utilizing survival analysis. Arch Gen Psychiatry. 1990;47:1106–11. doi: 10.1001/archpsyc.1990.01810240026005. [DOI] [PubMed] [Google Scholar]
- 85.Keck PE, Jr, McElroy SL, Strakowski SM, et al. Outcome and comorbidity in first- compared with multiple-episode mania. J Nerv Mental Dis. 1995;183:320–4. doi: 10.1097/00005053-199505000-00008. [DOI] [PubMed] [Google Scholar]
- 86.Dion GL, Tohen M, Anthony WA, et al. Symptoms and functioning of patients with bipolar disorder six months after hospitalization. Hosp Comm Psychiatry. 1998;39:652–7. doi: 10.1176/ps.39.6.652. [DOI] [PubMed] [Google Scholar]
- 87.Keller MB, Waternaux CM, Tsuang MT. Bipolar I: A five-year prospective follow-up. J Nerv Mental Dis. 1993;81:238–45. doi: 10.1097/00005053-199304000-00005. [DOI] [PubMed] [Google Scholar]
- 88.Perlis RH, Ostacher MJ, Patel JK, et al. Predictors of recurrence in bipolar disorder: Outcomes from the Systematic Treatment Enhancement Program for Bipolar Disorder. Am J Psychiatry. 2006;163:217–24. doi: 10.1176/appi.ajp.163.2.217. [DOI] [PubMed] [Google Scholar]
- 89.Solomon DA, Keitner GI, Miller IW, et al. Course of illness and maintenance treatment for patients with bipolar disorder. J Clin Psychiatry. 1995;56:5–13. [PubMed] [Google Scholar]
- 90.Keck PE, Jr, McElroy SL. Outcome in the pharmacologic treatment of bipolar disorder. J Clin Psychopharmacol. 1996;16(Suppl 1):15–23. doi: 10.1097/00004714-199604001-00003. [DOI] [PubMed] [Google Scholar]
- 91.Griel W, Ludwig-Mayerhofer W, Erazo N, et al. Lithium versus carbamazepine in the maintenance treatment of bipolar disorders-a randomised study. J Affect Dis. 1997;43:151–61. doi: 10.1016/s0165-0327(96)01427-9. [DOI] [PubMed] [Google Scholar]
- 92.Bowden CL, Calabrese JR, Sachs G, et al. A placebo-controlled 18-month trial of lamotrigine and lithium maintenance treatment in recently manic or hypomanic patients with bipolar I disorder. Arch Gen Psychiatry. 2003;60(4):392–400. doi: 10.1001/archpsyc.60.4.392. [DOI] [PubMed] [Google Scholar]
- 93.Tohen M, Calabrese JR, Sachs GS, et al. Randomized, placebo-controlled trial of olanzapine as maintenance therapy in patients with bipolar I disorder responding to acute treatment with olanzapine. Am J Psychiatry. 2006;163(2):247–56. doi: 10.1176/appi.ajp.163.2.247. [DOI] [PubMed] [Google Scholar]
- 94.Tohen M, Ketter TA, Zarate CA, et al. Olanzapine versus divalproex sodium for the treatment of acute mania and maintenance of remission: A 47-week study. Am J Psychiatry. 2003;160:1263–71. doi: 10.1176/appi.ajp.160.7.1263. [DOI] [PubMed] [Google Scholar]
- 95.Keck PE, Sanchez R, Marcus RN. Aripiprazole for relapse prevention in bipolar disorder in a 26-week trial. Poster, 157th Annual Meeting of the American Psychiatric Association, 2004.
- 96.Frye MA, Ketter TA, Leverich GS, et al. The increasing use of polypharmacotherapy for refractory mood disorders: 22 years of study. J Clin Psychiatry. 2000;61:9–15. doi: 10.4088/jcp.v61n0104. [DOI] [PubMed] [Google Scholar]
- 97.Tohen M, Chengappa KNR, Suppes T, et al. Relapse prevention in bipolar I disorder: 18-month comparison of olanzapine plus mood stabilizer vs. mood stabilizer alone. Brit J Psychiatry. 2004;184:337–45. doi: 10.1192/bjp.184.4.337. [DOI] [PubMed] [Google Scholar]