Abstract
OBJECTIVE
Increases in blood pressure and visit-to-visit variability have both been found to independently increase the likelihood of cardiovascular events in nondiabetic individuals. This study has investigated whether each may also influence the development of microvascular complications in type 1 diabetes by examining data from the Diabetes Control and Complications Trial (DCCT).
RESEARCH DESIGN AND METHODS
Using binary longitudinal multiple logistic regression, mean systolic (SBP) and diastolic (DBP) blood pressure as well as annual visit-to-visit variability (SD.SBP and SD.DBP, respectively) was related to the risk of the development/progression of nephropathy and retinopathy in initially normotensive subjects who did not become pregnant during the DCCT.
RESULTS
Mean SBP and SD.SBP were independently predictive of albuminuria (odds ratio 1.005 [95% CI 1.002–1.008], P < 0.001 and 1.093 [1.069–1.117], P < 0.001, respectively, for 1 mmHg change), although SBP variability did not add to mean SBP in predicting retinopathy (0.999 [0.985–1.013], P = 0.93). DBP variability was also independently predictive of nephropathy (1.102 [1.068–1.137], P < 0.001) and not of retinopathy (0.991 [0.971–1.010], P = 0.37). Mean SBP was poorly related to SD.SBP (r2 < 0.01) as was mean DBP with SD. DBP (r2 < 0.01).
CONCLUSIONS
Visit-to-visit variability in blood pressure consistently independently added to mean blood pressure in predicting the risk of nephropathy, but not retinopathy, in the DCCT. This observation could have implications for the management and treatment of blood pressure in patients with type 1 diabetes.
Hyperglycemia, and the duration of exposure to hyperglycemia, explains only ∼11% of the risk of developing microvascular complications in type 1 diabetes (1). The remaining 89% of risk must be explained by other factors, one of which is the presence of hypertension, which is known to be especially related to development and progression of nephropathy (2–5). Blood pressure lowering using antihypertensive agents has been shown to be successful in slowing the deterioration in renal function of type 1 diabetic patients with established renal impairment or proteinuria (6) but to only have an influence on retinopathy, not nephropathy, at much earlier stages in normotensive patients with normoalbuminuria (7).
The role of hypertension in the development of small-vessel disease therefore remains unclear. Certainly, hypertension is related to the presence of microalbuminuria in type 1 diabetes, but it is not known whether it is the hypertension that gives rise to nephropathy or vice versa (8). Hypertension also predicts retinopathy and this frequently coexists with nephropathy, but again it is uncertain whether high blood pressure gives rise to eye disease directly or is more a marker that renal disease is also present.
Recently, in two large study meta-analyses (9,10), visit-to-visit variability in systolic blood pressure (SBP) has been found to be a strong predictor of subsequent stroke independent of the mean SBP. We speculated that blood pressure variability may also have an influence on the development of microvascular complications in diabetes. To this end, we have reranalyzed data from the Diabetes Control and Complications Trial (DCCT) to see if blood pressure and its variability influenced the development of nephropathy and retinopathy in its large group of type 1 diabetic patients.
RESEARCH DESIGN AND METHODS
The datasets
We used the publicly accessible datasets collected by the DCCT. The DCCT was a 9-year follow-up study of 1,441 participants with type 1 diabetes comparing the effect of intensive versus conventional blood glucose management on the development of the microvascular complications of diabetes. At randomization, patients were stratified into one of two cohorts. The primary prevention cohort (n = 726) had no evidence of retinopathy by fundus photography and a urinary albumin excretion rate (AER) <40 mg/24 h (28 μg/min). The secondary prevention cohort (n = 715) had only minimal retinopathy and an AER <200 mg/24 h (140 μg/min). The study participants were randomized into intensive (n = 711) and conventional (n = 730) treatment groups. Individuals were excluded from the DCCT study if their SBP was >140 mmHg and/or their diastolic blood pressure (DBP) was >90 mmHg or they were treated with antihypertensive medication (11). The following DCCT SAS files were used in our analyses (retinopathy: ms2exprt.sas7bdat; nephropathy: ms3exprt.sas7bdat).
Blood pressure and definition of events
The effect of SBP and DBP on microvascular complications was assessed by examining annual measurements during the DCCT in all subjects who were not pregnant at any stage during the study (n = 1,261: 761 male and 500 female, median age 28 years [interquartile range {IQR} 22–33]). Blood pressure was measured with a random-zero sphygmomanometer twice in a sitting position. Variability of SBP/DBP (mmHg) was calculated as the SD of the between-visit measurements. Because the SD is influenced by the number of observations, the generalized estimating equation regression models were weighted by the number of SBP/DBP measurements. This ranged from 1 to 10 (median 6), being the same for SBP and DBP. The blood pressure value recorded was used irrespective of whether the patient was started on antihypertensive treatment during the course of the DCCT.
Severity of retinopathy was determined by the 25-point Early Diabetic Retinopathy Treatment Study (EDRTS) interim score (12). The development and progression of sustained retinopathy was defined as a change from baseline of three or more units on the EDRTS score on any two successive evaluations as predefined by the DCCT investigators. During the 9 years of follow-up, 334 people developed sustained retinopathy, 114 of whom were in the intensive treatment group. Nephropathy was defined as the development of an AER ≥40 mg/24 h (28 μg/min) on any annual evaluation, providing that the baseline AER was <40 mg/24 h (28 μg/min). The mean age was 27 years (range 13–39). Just over half (n = 761, 52.8%) were men. Seventy-three secondary-prevention patients had an AER ≥40 mg/24 h at baseline but <200 mg/24 h, so a separate analysis was performed excluding these individuals. Primary- or secondary-intervention grouping was based solely on retinopathy, which did not allow a similar analysis based on nephropathy development.
Average BMI was 23.4 kg/m2; <2% had a BMI >30 kg/m2. Nearly all participants were Caucasian. The median disease duration was 4 years. Approximately one-fifth declared themselves as current smokers.
Statistical methods
We used the generalized estimating equation (GEE) with a logit link to assess the effect of covariates on the odds of the development and progression of both retinopathy and nephropathy over repeated time points (13,14). The GEE logistic regression method, which is implemented in the Stata statistical computer package (15), allows for the correlation between successive repeated measurements on the same subject. Covariates to blood pressure indexes in the models included age (years) at entry into the DCCT, duration of diabetes (months) prior to DCCT, sex, randomization treatment (intensive versus conventional), A1C (%) at baseline, and A1C (averaged across the study). The size, direction, and statistical significance of relationships were estimated by the odds ratio (OR) with 95% CIs. The OR is an approximation to the relative risk (16). The 95% CIs were estimated from Wald robust SEs (i.e., using the empirical [information sandwich] variance estimates). An arbitrary level of 5% statistical significance (two tailed) was assumed. Unweighted linear regression was used to relate blood pressure variability (SD) to mean blood pressure averaged over all study visits. The Stata statistical computer package was used to analyze the data (StataCorp), and the Analyze-It add-in for Microsoft Excel was used for linear correlation.
RESULTS
The average of each patients' mean SBP during the DCCT was (means ± SD) 114.8 ± 8.5 mmHg and DBP was 73.7 ± 5.8 mmHg. Intraindividual variability (SD) of SBP (SD.SBP) and DBP ranged from 0 to 24 mmHg (median 8.0 mmHg) and 1 to 14 mmHg (median 6.5 mmHg), respectively, being similar for both randomization treatments.
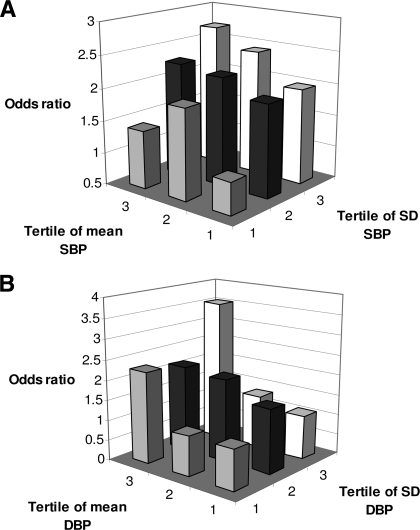
Table 1 shows the relationship between both mean SBP and SBP variability and the development or progression in retinopathy and nephropathy. Table 2 gives the equivalent data for DBP. While a relationship between retinopathy and mean SBP approached statistical significance, there was none with SD.SBP, either overall or by randomization treatment (Table 1). In contrast, there was a significant independent relationship between both mean SBP and SD.SBP and nephropathy in each randomization group and when the groups were combined (Table 1). Table 2 shows an association between mean DBP and retinopathy risk, with DBP variability contributing no further, whereas, overall, the opposite was true for nephropathy with DBP variability. Figure 1A shows the risk of nephropathy according to tertiles of both mean SBP and SD.SBP relative to subjects in the lowest tertile for each, with Fig. 1B showing the same data for DBP. Restricting analysis to only those individuals with a baseline AER <40 mg/24 h made no difference to the findings.
Table 1.
SBP longitudinal multiple logistic regression models for nephropathy and retinopathy excluding pregnant patients
| Nephropathy |
Retinopathy |
|||
|---|---|---|---|---|
| Odds ratio (95% CI) | P value | Odds ratio (95% CI) | P value | |
| All Patients | ||||
| Model 1 | ||||
| SBP (mmHg) | 1.006 (1.003–1.010) | <0.001 | 1.002 (1.000–1.005) | 0.014 |
| Model 2 | ||||
| SBP (mmHg) | 1.005 (1.002–1.008) | <0.001 | 1.002 (1.000–1.005) | 0.014 |
| SD.SBP (mmHg) | 1.093 (1.069–1.117) | <0.001 | 0.999 (0.985–1.013) | 0.93 |
| Intensive | ||||
| Model 1 | ||||
| SBP (mmHg) | 1.007 (1.001–1.014) | 0.015 | 1.008 (1.004)–1.012) | <0.001 |
| Model 2 | ||||
| SBP (mmHg) | 1.006 (1.000–1.012) | 0.023 | 1.008 (1.004–1.012) | <0.001 |
| SD.SBP (mmHg) | 1.065 (1.022–1.109) | 0.002 | 1.015 (0.989–1.042) | 0.24 |
| Conventional | ||||
| Model 1 | ||||
| SBP (mmHg) | 1.004 (1.000–1.008) | 0.018 | 0.999 (0.996–1.002) | 0.70 |
| Model 2 | ||||
| SBP (mmHg) | 1.003 (0.999–1.007) | 0.056 | 0.999 (0.996–1.002) | 0.76 |
| SD.SBP (mmHg) | 1.111 (1.083–1.139) | <0.001 | 0.99 (0.974–1.006) | 0.23 |
Model 1 relates to mean SBP alone, model 2 incorporates visit-to-visit SD.SBP. Models were adjusted for age, sex, disease duration, A1C (baseline), and A1C (mean). Model for all patients further adjusted for randomization treatment. Models weighted for number of SBP measurements. Odds ratio for SBP per 1-mmHg increase.
Table 2.
DBP longitudinal multiple logistic regression models for nephropathy and retinopathy excluding pregnant patients
| Nephropathy |
Retinopathy |
|||
|---|---|---|---|---|
| Odds ratio (95% CI) | P value | Odds ratio (95% CI) | P value | |
| All patients | ||||
| Model 1 | ||||
| DBP (mmHg) | 0.998 (0.995–1.004) | 0.95 | 1.009 (1.006–1.013) | <0.001 |
| Model 2 | ||||
| DBP (mmHg) | 1.000 (0.995–1.004) | 0.89 | 1.009 (1.006–1.013) | <0.001 |
| SD.DBP (mmHg) | 1.102 (1.068–1.137) | <0.001 | 0.991 (0.971–1.010) | 0.37 |
| Intensive | ||||
| Model 1 | ||||
| DBP (mmHg) | 1.015 (1.007–1.023) | <0.001 | 1.006 (1.001–1.012) | 0.01 |
| Model 2 | ||||
| DBP (mmHg) | 1.016 (1.007–1.024) | <0.001 | 1.006 (1.001–1.012) | 0.01 |
| SD.DBP (mmHg) | 0.954 (0.901–1.009) | 0.1 | 0.994 (0.962–1.028) | 0.76 |
| Conventional | ||||
| Model 1 | ||||
| DBP (mmHg) | 0.991 (0.986–0.997) | 0.005 | 1.011 (1.007–1.015) | <0.001 |
| Model 2 | ||||
| DBP (mmHg) | 0.993 (0.987–0.998) | 0.01 | 1.011 (1.007–1.015) | <0.001 |
| SD.DBP (mmHg) | 1.16 (1.118–1.204) | <0.001 | 0.986 (0.962–1.011) | 0.29 |
Model 1 relates to mean DBP alone. Model 2 incorporates visit-to-visit SD.DBP. Models adjusted for as for SBP.
Figure 1.
Risk of nephropathy according to rising tertiles of mean SBP and visit-to-visit SBP variability (SD.SBP) (A) and mean DBP and DBP variability (SD.DBP) (B). The lowest tertile for mean blood pressure and SD blood pressure is the reference. Data adjusted as in Table 1.
Looking at primary- and secondary-intervention groups separately, the only signal for blood pressure variability (SBP or DBP) influencing retinopathy among the eight groups examined (primary/secondary, intensive/conventional, SD.SBP/SD.DBP) was in the SD.SBP of the intensively treated primary prevention patients (hazard ratio 1.144[95% CI 1.089–1.203]), P < 0.001), although this, understandably, was in the group with the least number of subjects showing a consistent three-step change (n = 23).
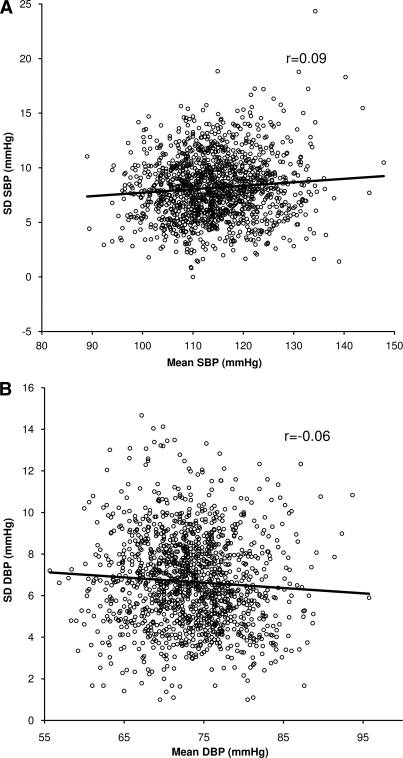
The linear relationship between mean SBP and SBP variability was poor, although statistically significant, due to the large number of subjects involved (r = 0.09, P = 0.0013) (Fig. 2A), with SD.SBP rising by 0.3 mmHg for every 10-mmHg rise in mean SBP. Likewise, changes in mean DBP explained little of any change in DBP variability (r = 0.06, P = 0.026) (Fig. 2B), with SD.DBP falling by 0.2 mmHg for every 10-mmHg rise in mean DBP. There was more of an association between variability in SBP and variability in DBP (r = 0.29, P < 0.0001).
Figure 2.
Relationship between SBP variability (SD.SBP) and mean SBP (A) and between DBP variability (SD.DBP) and mean DBP (B).
CONCLUSIONS
This study has shown that annual visit-to-visit variability in both SBP and DBP are associated with the development of nephropathy in type 1 diabetes, independently of their mean values. While mean DBP was related to the appearance of retinopathy, blood pressure variability was less of a feature of this microvascular complication.
Looked at from the basis of patients participating in the DCCT, the magnitude of the contribution of SBP variability to nephropathy is at least as much as that which can be attributed to changes in mean SBP (Fig. 1). Indeed, using the models in Table 1, it means that a DCCT patient on the 97.5th centile of SBP variability (SD 13.3 mmHg) has 2.34 times the nephropathy risk of a patient on the 2.5th centile (SD 3.7 mmHg) for a given mean SBP. By comparison, a patient on the 97.5th centile of mean SBP (129 mmHg) has 1.15 times the nephropathy risk of a patient on the 2.5th centile (101.1 mmHg) for a given SBP variability.
These findings are in keeping with recent studies that have shown that in various population studies not particularly targeting patients with diabetes that visit-to-visit variability in SBP is a powerful predictor of stroke and coronary events, independent of mean SBP (9,10). As type 1 diabetic patients with diabetic nephropathy are at an especial risk of these macrovascular complications (17), it may point to SBP variability being a common risk factor for both.
It is perhaps surprising that visit-to-visit blood pressure variability itself (both SBP and DBP) was not more closely related to the respective mean blood pressure values. Mean SBP and mean DBP explained <1% of the variance (r2) in SD.SBP and SD.DBP. Indeed, linear regression suggested that the magnitude of any change in variability associated with changes in mean BP and variability was modest and for DBP even suggested a fall in variability as mean DBP rose. This lack of concordance makes the association between blood pressure variability and nephropathy all the more likely to be due to an independent effect, as it has been found without attempting to statistically tease out the relative contribution of two closely related blood pressure factors.
Mention must be made of the fact that SBP variability did have a statistically significant effect on retinopathy development in the intensively treated primary-prevention cohort. However, this was the sole retinopathy signal in all the analyses performed and was found in the group with the fewest of patients having events. By comparison, there was over six times the number of patients experiencing retinopathy worsening in the conventionally treated secondary-prevention group. Therefore, although this is perhaps one of the clinically most important groups, the possibility of this finding being a type 1 error cannot be excluded.
The more consistent influence of blood pressure and its variability predicting nephropathy rather than retinopathy is in contrast to that of glycemia. In another analysis of DCCT data, both mean A1C and A1C variability have been found to be considerably more predictive of retinopathy changes than in nephropathy (18).
There remains the question of whether blood pressure is having an influence on albuminuria or nephropathy is having an influence on blood pressure. A previous examination of DCCT data were unable to provide a definitive answer, since although 90% of subjects who developed nephropathy did so before the diagnosis of hypertension, a rise in DBP preceded the rise in albuminuria among intensively treated patients (19). If nephropathy does lead to hypertension, then this current analysis of the same dataset suggests that nephropathy would need influence both mean blood pressure and its visit-to-visit variability. Since average blood pressure and blood pressure variability are not closely related, it means nephropathy would probably need to affect both by two different mechanisms. Rather, it seems more plausible that there be an independent effect of raised blood pressure and of episodic hypertension on the development of albuminuria.
Should increasing blood pressure variability prove to have an influence on the development of diabetic nephropathy, then the effect of different antihypertensive drug classes on this instability may be of relevance. For some time, ACE inhibitors and angiotensin 2 receptor antagonists (A2As) have been the first-line antihypertensive drug of choice due to their beneficial effect on blood pressure and an especial effect on albuminuria. However, ACE inhibitors and A2As lead to relatively increased SBP variability compared with other drug classes, such as calcium channel blockers and nonloop diuretics, and only calcium channel blockers reduce visit-to-visit SBP variability compared with placebo (20). Therefore, although drugs affecting the renin-angoiotensin system have theoretical advantages over other antihypertensive classes in preventing nephropathy, their effect on blood pressure variability may not be one of them.
This observation on the effect of antihypertensive classes on blood pressure variability, together with our current findings, may help explain the results from the recent Renin-Angiotensin System Study (RASS), which investigated the effect of enalapril and losartan compared with placebo on the progression of renal disease in a group of 285 normotensive normoalbuminuric type 1 diabetic patients (7). Despite a significant reduction in SBP and DBP with the two antihypertensive drugs, there were no beneficial renal histological changes compared with placebo, nor were there any reductions the development of microalbuminuria (actually being higher among patients taking the A2A) or in the decline in glomerular filtration rate. As most patients in the DCCT were at a similar primary-prevention stage in their type 1 diabetes to those in the RASS trial and were also initially normotensive, it is possible that any benefits related to reduction in mean blood pressure by the ACE inhibitor and A2A were being mitigated by a lack of effect on blood pressure variability. This is in marked contrast to eye disease in the RASS, where both enalapril and losartan led to marked reduction in the development of retinopathy, a complication that was found to be less related to blood pressure variability in this current study.
Finally, the data presented here also have implications for the interpretation of blood pressure measurements in patients with type 1 diabetes. Received wisdom is that antihypertensive treatment should only be instituted if hypertension can be confirmed on the basis of several raised blood pressure measurements on separate days (21). As for both coronary heart disease and stroke risk (22), the assumption that blood pressure need not require treatment when it is not consistently raised may now need to be reconsidered for preventing the development of diabetic nephropathy.
In conclusion, in contrast to retinopathy, visit-to-visit variability in blood pressure consistently added to mean blood pressure in predicting the risk of developing albuminuria among the patients participating in the DCCT. This observation could have implications for the management and treatment of blood pressure in patients with type 1 diabetes.
Acknowledgments
The Diabetes Control and Complications Trial (DCCT) and its follow-up the Epidemiology of Diabetes Interventions and Complications (EDIC) Study were conducted by the DCCT/EDIC Research Group and supported by National Institutes of Health (NIH) Grants and contracts and by the General Clinical Research Center Program, National Center for Research Resources.
No potential conflicts of interest relevant to this article were reported.
E.S.K. conceived the idea for the analysis and wrote the manuscript. A.S.R. performed the statistical analysis and helped write the manuscript. S.L.A. developed the idea and helped write the manuscript.
We thank the DCCT/EDIC investigators for making their trial dataset public and therefore allowing independent investigators to analyze their work for the benefit of patients with type 1 diabetes.
Footnotes
This article was not prepared under the auspices of the DCCT/EDIC Study and does not represent analyses nor conclusions of the DCCT/EDIC Study Group nor the NIH.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1. Lachin JM, Genuth S, Nathan DM, Zinman B, Rutledge BN. The effect of glycemic exposure on the risk of microvascular complications in the diabetes control and complications trial: revisited. Diabetes 2008;57:995–1001 [DOI] [PubMed] [Google Scholar]
- 2. Adler AI, Stratton IM, Neil HAW, Yudkin JS, Matthews DR, Cull CA, Wright AD, Turner RC, Holman RR. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study BMJ 2000;321:412–419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mortensen HB, Marinelli K, Nørgaard K, Main K, Kastrup KW, Ibsen KK, Villumsen J, Parving H-H. A nation-wide cross-sectional study of urinary albumin excretion rate, arterial blood pressure and blood glucose control in Danish children with type 1 diabetes mellitus. Diabet Med 1990;7:887–897 [DOI] [PubMed] [Google Scholar]
- 4. Lurbe E, Redon J, Kesani A, Pascual JM, Tacons J, Alvarez V, Batlle D. Increase in nocturnal blood pressure and progression to microalbuminuria in type 1 diabetes. N Engl J Med 2002;347:797–805 [DOI] [PubMed] [Google Scholar]
- 5. Raile K, Galler A, Hofer S, Herbst A, Dunstheimer D, Busch P, Holl RW. Diabetic nephropathy in 27,805 children, adolescents, and adults with type 1 diabetes. Diabetes Care 2007;30:2523–2528 [DOI] [PubMed] [Google Scholar]
- 6. Lewis EJ, Hunsicker LG, Bain RP, Rohde RD. The Collaborative Study Group: The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. N Engl J Med 1993;329:1456–1462 [DOI] [PubMed] [Google Scholar]
- 7. Mauer M, Zinman B, Gardiner R, Suissa S, Sinaiko A, Strand T, Drummond K, Donnelly S, Goodyer P, Gubler MC, Klein R. Renal and retinal effects of enalapril and losartan in type 1 diabetes. N Engl J Med 2009;361:40–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gallego PH, Craig ME, Hing S, Donaghue KC. Role of blood pressure in development of early retinopathy in adolescents with type 1 diabetes: prospective cohort study. 2008;BMJ 337:a918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rothwell P, Howard S, Dolan E, O'Brien E, Dobson J, Dahlöf B, Sever P, Poulter N. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet 2010;375:895–905 [DOI] [PubMed] [Google Scholar]
- 10. Rothwell P, Howard S, Dolan E, O'Brien E, Dobson J, Dahlöf B, Poulter N, Sever P. Effects of [beta] blockers and calcium-channel blockers on within-individual variability in blood pressure and risk of stroke. Lancet Neurol 2010;9:469–80 [DOI] [PubMed] [Google Scholar]
- 11. de Boer I, Kestenbaum B, Rue T, Steffes M, Cleary P, Molitch M, Lachin J, Weiss N, Brunzell J. Insulin therapy, hyperglycemia, and hypertension in type 1 diabetes mellitus. Arch Intern Med 2008;168:1867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329:977–986 [DOI] [PubMed] [Google Scholar]
- 13. Liang K, Zeger S. Longitudinal data analysis using generalized linear models. Biometrika 1986;73:13–22 [Google Scholar]
- 14. Diggle PH, Liang PJ, Zeger K-Y, SL. Analysis of Longitudinal Data, Oxford University Press, 2002, Oxford, U.K. [Google Scholar]
- 15. Horton N, Lipsitz S. Review of software to fit generalized estimating equation regression models. Am Stat 1999;53:160–169 [Google Scholar]
- 16. Rigby A. Statistical methods in epidemiology: III. the odds ratio as an approximation to the relative risk. Disabil Rehabil 1999;21:145–151 [DOI] [PubMed] [Google Scholar]
- 17. Tuomilehto J, Borch-Johnsen K, Molarius A, Forsén T, Rastenyte D, Sarti C, Reunanen A. Incidence of cardiovascular disease in type 1 (insulin-dependent) diabetic subjects with and without diabetic nephropathy in Finland. Diabetologia 1998;41:784–790 [DOI] [PubMed] [Google Scholar]
- 18. Kilpatrick ES, Rigby AS, Atkin SL. A1C variability and the risk of microvascular complications in type 1 diabetes. Diabetes Care 2008;31:2198–2202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Thomas W, Shen Y, Molitch ME, Steffes MW. Rise in albuminuria and blood pressure in patients who progressed to diabetic nephropathy in the Diabetes Control and Complications Trial. J Am Soc Nephrol 2001;12:333–340 [DOI] [PubMed] [Google Scholar]
- 20. Webb A, Fischer U, Mehta Z, Rothwell P. Effects of antihypertensive-drug class on interindividual variation in blood pressure and risk of stroke: a systematic review and meta-analysis. Lancet 2010;375:906–915 [DOI] [PubMed] [Google Scholar]
- 21. American Diabetes Association: Standards of medical care in diabetes, 2010. Diabetes Care 2010;33(Suppl. 1):S11–S61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rothwell P. Limitations of the usual blood-pressure hypothesis and importance of variability, instability, and episodic hypertension. Lancet 2010;375:938–948 [DOI] [PubMed] [Google Scholar]