Abstract
OBJECTIVE
To investigate the association between neck circumference and central obesity, overweight, and metabolic syndrome in Chinese individuals with type 2 diabetes.
RESEARCH DESIGN AND METHODS
A total of 3,182 diabetic subjects (aged 20–80 years) were recruited from 15 community health centers in Beijing using a multistage random sampling approach.
RESULTS
Receiver operating characteristic analysis showed that the area under the curve for neck circumference and central obesity was 0.77 for men and 0.75 for women (P < 0.001). Furthermore, a neck circumference of ≥38 cm for men and ≥35 cm for women was the best cutoff point for determining overweight subjects. A neck circumference of ≥39 cm for men and ≥35 cm for women was the best cutoff point to determine subjects with metabolic syndrome.
CONCLUSIONS
In the present study, neck circumference is positively related with BMI, waist circumference, and metabolic syndrome in Chinese individuals with type 2 diabetes.
Neck circumference (NC) as an index for upper-body subcutaneous adipose tissue distribution has been evaluated in relation to cardiovascular risk factors, insulin resistance, and biochemical components of metabolic syndrome (MS) (1–4). However, epidemiological population-based studies on the clinical significance of NC in connection with overweight and MS in diabetic people are lacking. The aim of this study was to determine whether NC alone can predict overweight and central obesity and to evaluate the association between NC and MS.
RESEARCH DESIGN AND METHODS
In Beijing, 15 community health centers were selected by multistage random sampling approach. People with type 2 diabetes (aged 20–80 years) who had lived in the community over 5 years were recruited between August 2008 and July 2009. A total of 3,182 diabetic subjects with measurement of NC were available for analysis. People with severe disabilities, hepatic failure, renal failure, schizophrene, or goiter were excluded. Written informed consent was obtained from all participants.
Past medical history was determined with a standardized questionnaire. Blood pressure was measured twice after each subject had been seated for 10 min. The average was used for analysis. Waist circumference (WC) was measured at the level midway between the lower rib margin and the iliac crest. NC was measured with head erect and eyes facing forward, horizontally at the upper margin of the laryngeal prominence (Adam's apple). Fasting glucose and lipid profiles were determined using an autoanalyzer.
Overweight was defined as BMI ≥24 kg/m2, central obesity was defined as WC ≥85 cm for men and ≥80 cm for women (5–6). MS was defined according to the Chinese Diabetes Society definition (7).
Receiver operating characteristic (ROC) curve analyses were performed using SPSS 11.5 software. The Youden index, defined as “sensitivity + specificity − 1,” was used to determine the optimal NC cutoff points.
RESULTS
The study sample consisted of 1,294 men and 1,888 women with a mean age of 64.0 ± 10.1 years. Men, with a mean of 38.4 ± 3.6 cm, had an NC 3 cm wider than women, with a mean of 35.4 ± 3.3 cm (P < 0.001). NC correlated positively with BMI (men r = 0.41; women r = 0.84; each, P < 0.0001). NC also correlated positively with WC (men r = 0.47; women r = 0.47; each, P < 0.0001).
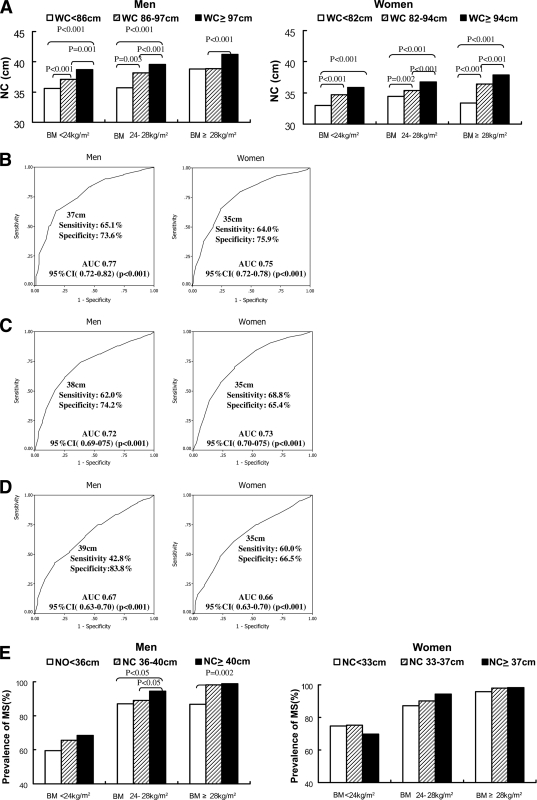
All subjects were divided into subgroups based on their BMI. The BMI limits were set at <24, 24–28, and >28 kg/m2. NC was positively correlated with WC in the three BMI subgroups in men (r = 0.352, 0.261, 0.340; all P < 0.001). Similar results were found for the subgroups in women (r = 0.318, 0.277, 0.356; all P < 0.001). Each BMI subgroup was further divided into three subgroups based on percentile 25, 25–75, 75 of WC. In both men and women, NC increased from the lower WC subgroups to the higher WC subgroups within each BMI subgroup. (Fig. 1A).
Figure 1.
A: NC in the BMI and WC subgroups. ROC curves related to NC and central obesity (B), overweight (C) and MS (D) in men and women. E: The prevalence of MS in the BMI and NC subgroups.
The prevalence of central obesity was 87.2%. ROC analysis showed that the area under the curve (AUC) for NC and central obesity was 0.77 for men and 0.75 for women. An NC of ≥37 cm for men and ≥35 cm for women was the best cutoff point for determining subjects with central obesity (Fig. 1B).
The prevalence of overweight was 65.0%. NC in the overweight group was 36.2 ± 3.1 cm, higher than in the BMI <24 kg/m2 group (33.8 ± 3.0 cm) (P < 0.001). An NC of ≥38 cm for men and ≥35 cm for women was the best cutoff point for determining subjects with overweight. The AUC was 0.72 for men and 0.73 for women (Fig. 1C).
Two thousand seven hundred and nine subjects with MS had 1.5 cm wider NC than the subjects without MS (36.8 ± 3.7 vs. 35.3 ± 3.4 cm; P < 0.001). An NC of ≥39 cm for men and ≥35 cm for women was the best cutoff point for determining subjects with MS (Fig. 1D). Each BMI subgroup was further divided into three subgroups based on percentile 25, 25–75, 75 of NC. In men and women, the prevalence of MS had a tendency to increase from the lower BMI and NC subgroups to the higher subgroups (Fig. 1E). A logistic regression analysis, using MS as the dependent variable, showed that the relationship between NC and MS after adjusting for sex and age was statistically significant (odds ratio 1.20 [95% CI 1.16–1.24]; P < 0.001).
CONCLUSIONS
The present study showed that an NC of ≥37 cm for men and ≥35 cm for women was the best cutoff point to determine subjects with central obesity. An NC of ≥38 cm for men and ≥35 cm for women was the best cutoff point to determine subjects with overweight.
The NC cutoff points for evaluating overweight or obesity have been differently defined in different studies (4,8). The discrepancy with the results of this study may be due to different diagnostic standards or study populations. Prevalence of overweight and obesity in diabetic people is higher than in the general population, which might be one cause for the discrepancy.
In this cross-sectional analysis of diabetic population–based data, we found NC to be independently related to MS indicating that NC may be used as a simple test for identifying MS. This is in accordance with previous studies (2,4).The optimal NC cutoff points for evaluating MS and obesity were found to be different. MS is a constellation of a variety of metabolic risk factors, one of which is obesity. Thus, the correlation between NC and MS is less pronounced compared with the NC and central obesity correlation. Furthermore, the prevalence of MS in this study was higher than the prevalence in the general population. These may be possible explanations for the different NC cutoff points for MS and central obesity.
This study of a diabetic population has certain limitations. Further studies are needed to identify the relationship of NC with central obesity and MS in general population. Additionally, the reproducibility of the NC cutoff point results should be further studied.
In summary, in this community diabetic population–based study, NC is related with BMI, WC, and MS in Chinese subjects with type 2 diabetes. NC seems thus suitable to be used in a clinical setting as a strong indicator for central obesity and metabolic abnormalities in type 2 diabetic subjects.
Acknowledgments
This work was supported by the Capital Medical Development Foundation of China (2007-1035). Tilman Altmeppen of Novo Nordisk assisted in editing the article.
No other potential conflicts of interest relevant to this article were reported.
G.Y. researched data, contributed to the discussion, and wrote the manuscript. S.Y. contributed to the discussion, wrote the manuscript, and reviewed the manuscript. H.F. researched data, contributed to the discussion, and reviewed manuscript. G.W. researched data. L.Z. researched data and reviewed the manuscript. X.B. researched data. J.Z., X.D., Y.L., Y.J., X.G., and Y.L. researched data.
APPENDIX
Additional participating investigators for the Beijing Community Diabetes Study Group: Su-fang Pan, the Department of Endocrinology, Beijing Tongren Hospital, Capital Medical University, Beijing; Xue-li Cui, Sanlitun Community Health Service Center, Beijing; Wei Bai, Dongfeng Community Health Service Center, Beijing; Yu-jie Chen, Sijiqing Community Health Service Center, Beijing; Zi-ming Wang, Jiangtai Community Health Service Center, Beijing; Qing-sheng Zhu, Balizhuang Community Health Service Center, Beijing; Ying Gao, The First People's Hospital of Chongwen District, Beijing; De-yuan Liu, Zuojiangzhuang Community Health Service Center, Beijing; Yun-tao Ji, Majiapu Community Health Service Center, Beijing.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1. Sjöström CD, Håkangård AC, Lissner L, Sjöström L. Body compartment and subcutaneous adipose tissue distributionrisk factor patterns in obese subjects. Obes Res 1995;3:9–22 [DOI] [PubMed] [Google Scholar]
- 2. Onat A, Hergenç G, Yüksel H, Can G, Ayhan E, Kaya Z, Dursunoğlu D. Neck circumference as a measure of central obesity: associations with metabolic syndrome and obstructive sleep apnea syndrome beyond waist circumference. Clin Nutr 2009;28:46–51 [DOI] [PubMed] [Google Scholar]
- 3. Laakso M, Matilainen V, Keinänen-Kiukaanniemi S. Association of neck circumference with insulin resistance-related factors. Int J Obes Relat Metab Disord 2002;26:873–875 [DOI] [PubMed] [Google Scholar]
- 4. Ben-Noun LL, Laor A. Relationship between changes in neck circumference and cardiovascular risk factors. Exp Clin Cardiol 2006;11:14–20 [PMC free article] [PubMed] [Google Scholar]
- 5. Chinese diabetes society. China guideline for type 2 diabetes (2007 edition). Natl Med J China 2008;88:1227–1245 [Google Scholar]
- 6. Cooperative Meta-Analysis Group of China Obesity Task Force. Predictive values of body mass index and waist circumference to risk factors of related diseases in Chinese adult population. Chin J Epidemiol 2002;23:5–10 [PubMed] [Google Scholar]
- 7. Expert Panel on Metabolic Syndrome of Chinese Diabetes Society. Recommendations on metabolic syndrome of Chinese diabetes society. Chin J Diab 2004;12:156–161 [Google Scholar]
- 8. Ben-Noun L, Sohar E, Laor A. Neck circumference as a simple screening measure for identifying overweight and obese patients. Obes Res 2001;9:470–477 [DOI] [PubMed] [Google Scholar]