Abstract
Objectives:
To determine the prevalence, age of onset, severity, associated disability, and treatment of major depression among United States ethnic groups, national survey data were analyzed.
Methods:
National probability samples of US household residents ages 18-years and older (N=14,710) participated. The main outcomes were past-year and lifetime major depression (World Mental Health Composite International Diagnostic Interview). Major depression prevalence estimates, age of onset, severity, associated disability, and disaggregated treatment use (pharmacotherapy and psychotherapy) and treatment guideline concordant use were examined by ethnicity.
Results:
The prevalence of major depression was higher among US-born ethnic groups compared to foreign-born groups, but not among older adults. African Americans and Mexicans had significantly higher depression chronicity and significantly lower depression care use and guideline concordant use than Whites.
Discussion:
We provide concise and detailed guidance for better understanding the distribution of major depression and related mental healthcare inequalities and related morbidity. Inequalities in depression care primarily affecting Mexican Americans and African Americans may relate to excesses in major depression disease burden.
Keywords: Major depression, depression, epidemiology, ethnicity, race
INTRODUCTION
In the coming decades, unipolar depression is projected to be the second leading cause of disability worldwide and the leading cause of disability in high-income nations, including the United States.1 Within the US, depression is a leading cause of disability among major ethnic and racial groups and a common problem in medical comorbidity.2 Several technical problems have impeded the ability to identify disparities in depression prevalence and treatment access and quality. The aggregation of ethnic subgroups (i.e., all Latinos or Asians as opposed to specific ethnic subgroups) in national studies creates uncertainty. As a result this practice is discouraged by the Surgeon General and the National Institutes of Health because important differences in major depression are overlooked by “masking” intra-ethnic differences.3-5 Furthermore, discrete determinants of seeking and obtaining treatment for depression and related disability and treatment use, such as variable access to insurance, and are similarly masked when ethnic groups are lumped together. 6
Several recent studies have reported that differences in depression exist within ethnic groups; however, those studies did not present comprehensive comparisons across groups (e.g., Whites and Filipinos).7-10 Our current understanding of the epidemiology of major depression is further complicated because in the United States, mood disorders are combined (e.g., major depression and dysthymia) which makes it difficult if not impossible to specify the prevalence of this leading cause of disability. 4, 7, 11, 12 Extant prevalence estimates are often presented in broad demographic and sociodemographic categories and some are outdated, particularly for older adults. Prevalence estimates for major depression among older adults rely on data from the Epidemiologic Catchment Area (ECA), which are over 30-years old and preceded major changes in current diagnostic criteria and demographic composition, especially shifts in the age structure and ethnic composition of the U.S. population in the new millennium.13, 14 Later work with original ECA data have yielded interesting ethnic/racial comparisons of depressive symptoms and patterns of psychopathology among older adults; however, these aggregated data do not permit within ethnic/racial groups (e.g., African Americans and Caribbean Blacks) comparisons.15-17 One purpose of this study was to provide a concise and precise report on the epidemiology of major depression among major ethnic and nativity groups across adulthood in the United States. Secondly, we compared the epidemiology of major depression within major ethnic subgroups. To achieve these objectives, nationally representative data was disaggregated by ethnic and nativity groups to provide prevalence estimates of US adults who met criteria for 12-month and lifetime major depression.
METHOD
Data Collection
The National Institute of Mental Health's Collaborative Psychiatric Epidemiology Surveys (CPES) data were used in this study. The CPES combines three nationally representative studies: the National Survey of American Life (NSAL), the National Comorbidity Survey-Replication (NCS-R) and the National Latino and Asian American Study (NLAAS). Data for the CPES were collected between February 2001 and November 2003. Specially trained non-clinician interviewers administered face-to-face computer-assisted interview technology to collect data. The overall CPES response rate was 72.3%.
Complex multi-stage area probability sampling methods were used for data collection and sampling weights accounting for unequal probability of selection into the CPES samples and non-response rates were created by CPES staff to enable nationally representative analyses using the integrated data set. These weights were incorporated in all analyses presented in this study, allowing for the generation of population estimates by analyzing data specific to populations of interest.18
Analysis of Subpopulations
Ethnic and racial categorization in the CPES was based on respondent self-identification. Since we were unable to adequately specify the Race or Ethnicity of respondents classified as “other” ethnic groups, we restricted our study subpopulation to nine groups including: Chinese (n=600); Filipinos (n=508); Vietnamese (n=520); Cubans (n=577); Mexican Americans (n=1422); Puerto Ricans (n=495); Caribbean Blacks (n=1476); African Americans (n=4249); and Whites who are not Latinos (n=5,071). The overall sample size for the study was n=14,710. Appropriate methods for subpopulation analyses of complex sample survey data were used for all analyses in this study.
Our primary interest was in the subpopulation meeting World Mental Health Composite International Diagnostic Interview (WMH-CIDI) criteria for Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria 12-month and lifetime major depression.19, 20
Measures
The WMH-CIDI was administered by well-trained, non-clinical interviewers. Five sets of major depression epidemiological outcomes were examined: prevalence, age of onset, severity, associated disability, and treatment use.
Prevalence and age of onset
Prevalence estimates were based on the sample proportion that met WMH-CIDI criteria for 12-month and lifetime major depression, and the first episode age was used for calculating the mean age of onset.
Severity
The Quick Inventory of Depressive Symptomatology Self-Report (QIDS-SR) was used to measure symptom severity during the worst two-week period of the past-year.21 The QIDS-SR is a brief and reliable test that has been validated using other established measures of depression severity (e.g., 24-item Hamilton Depression Rating Scale). Following depression care guidelines and to facilitate the interpretability of our results, severity was dichotomized with individuals scoring 10 or less being classified as “Mild” and those scoring more than 10 grouped in a second category containing “Moderate, Severe, and Very Severe” cases.
Impairment
The World Health Organization Disability Assessment Scale (WHODAS-II) was used to measure depression-related impairment (i.e., past-30 days out of role) in five domains from the International Classification of Function, Disease and Health: 1) overall role impairment; 2) cognition; 3) mobility; 4) self-care; and 5) social impairment.22, 23 The WHO-DAS II has been used in previous psychiatric epidemiologic studies.7, 12 Individuals reporting no such problems in a specific domain the past 30-days were assigned a zero-value for that domain. All other respondents were assigned values based on their self-reported number of out-of-role days in specific domains.
Treatment
For past-year treatment, two depression care modalities were examined: pharmacotherapy and psychotherapy. Pharmacotherapy was determined by self-report and pill bottle inventories. Generic and trade names were reviewed by two board certified psychiatrists and a psychiatric nurse specialist to verify that the drugs were antidepressants prior to drug coding for the analyses. For psychotherapy, treatment codes were based on self-reports of visits to mental health professionals, including psychologists, counselors, social workers and other health professionals (lay counselors were excluded), and the mean time (minutes) spent during those visits. Three past-year depression care use outcomes were computed for analyses: 1) any pharmacotherapy; 2) any psychotherapy; and 3) either therapy. To determine the depression care adequacy, we applied the American Psychiatric Association, Practice Guidelines for the Treatment of Patients with Major Depressive Disorder.24 We considered Guideline concordant pharmacotherapy as the use of antidepressant agents for at least 60-days with supervision by a psychiatrist, or other prescribing clinician, for at least four visits in the past year. For psychotherapy, Guideline concordance was operationalized as having at least four visits to a mental health professional in the past-year lasting on average for at least 30 minutes each.
Analytic Approach
Procedures designed for the analysis of complex sample survey data in the Stata (10.1) software package were used for analyses on all subpopulations.25 All statistical estimates were weighted, utilizing the CPES sampling weights to account for individual-level unequal probabilities of selection into the samples, individual non-response, and additional post-stratification to ensure US population representation.26 Design-based analyses, specifically a Taylor Series Linearization approach to variance estimation, were used to account for the complex multistage clustered design of the CPES samples when computing estimated standard errors.27
First, sample estimates describing demographic characteristics including age, sex, education, income and nativity were calculated. Second, prevalence estimates of 1) lifetime and 2) 12-month depression for the nine ethnic groups were estimated. These prevalence estimates were further disaggregated over seven age categories (18-24; 25-34; 35-44; 45-54; 55-64; 65-74; and 75 and over) in years and respondents' nativity (US-born; foreign-born). Third, group and nativity specific means estimates for average age of depression onset for respondents meeting criteria for WMH-CIDI lifetime and 12-month major depression were calculated. The following analyses were exclusively focused on the subpopulation of respondents who met WMH-CIDI 12-month major depression criteria. Fourth, five ordinary least squares regression models were used to estimate ethnic group level number of days of impairment over the past 30-days relative to the White reference category controlling for age and sex. Fifth, prevalence estimates for depression severity status using a dichotomized indicator of the QIDS-SR are provided. Subsequently, a logistic regression model is fit to test the odds of placement in the moderate/severe category for our racial and ethnic groups relative to their Whites and controlling for age and sex. Sixth, prevalence estimates for treatments and Guideline concordant treatments for pharmacotherapy, psychotherapy, and any of these two treatments are calculated. Finally, two age and sex adjusted logistic regression models were conducted to test the odds of any Guideline concordant treatment for our ethnic/racial groups relative to Whites and the attenuating effect of depression severity on these odds.
Results
Prevalence
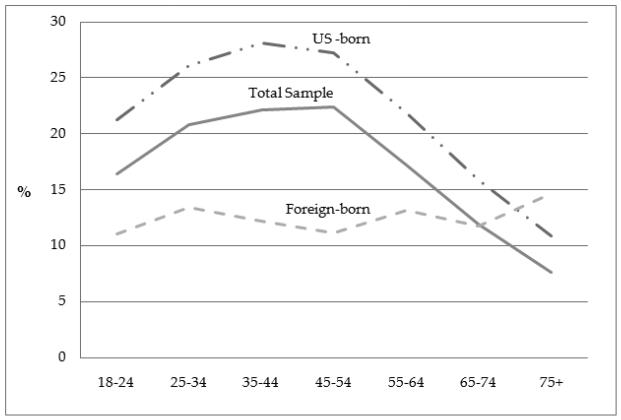
The CPES sample is described in Table 1. Educationally, Vietnamese, Latinos and African Americans were the least likely to complete high-school, and the most likely to fall into the lowest annual household income brackets. Both past year (χ2=33.7; P<0.001) and lifetime (χ2=4.6; P<0.001) major depression varied by ethnic groups with the highest prevalence among Puerto Ricans and the lowest among all three Asian groups (Table 2). Overall, the prevalence of past year major depression was significantly higher for US-born respondents compared to the foreign-born sample (χ2 =28.2; P<0.001). Cuban and Puerto Rican nativity groups were the exception to this pattern. Similar prevalence estimate patterns emerged for lifetime major depression (χ2 =87.3; P<0.001). For nativity, the prevalence of lifetime major depression of US-born respondents was twice that of foreign-born respondents, with the exception of the Vietnamese, Cubans, and Puerto Ricans. The prevalence of major depression, however, was significantly higher for foreign-born respondents over age 65-years compared to US-born respondents (OR=0.46;95%CI=0.28-0.77). The relationship between nativity and the prevalence of major depression across the life-course are shown in Figure 1.
Table 1.
Demographic Characteristics of the Collaborative Psychiatric Epidemiology Study Respondents.
| Chinese | Filipinos | Vietnamese | Cubans | Mexican Americans |
Puerto Ricans |
Black Caribbeans |
African Americans |
Whites | Total | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n=600 | n=508 | n=520 | n=577 | n=1442 | n=495 | n=1,492 | n=4,746 | n=7,587 | n=17,967 | |||||||||||
| % | SE | % | SE | % | SE | % | SE | % | SE | % | SE | % | SE | % | SE | % | SE | % | SE | |
| Age (Years) | ||||||||||||||||||||
| 18-24 | 11.3 | 1.6 | 16.7 | 2.5 | 11.4 | 1.8 | 9.2 | 1.5 | 24.6 | 1.3 | 17.7 | 2.2 | 18.7 | 2.0 | 16.8 | 0.9 | 13.8 | 1.3 | 15.0 | 1.0 |
| 25-34 | 20.6 | 2.9 | 19.2 | 2.3 | 18.6 | 2.4 | 16.1 | 1.6 | 27.2 | 1.3 | 21.1 | 2.7 | 22.6 | 1.8 | 19.2 | 0.7 | 14.4 | 0.5 | 16.2 | 0.4 |
| 35-44 | 25.3 | 2.9 | 21.5 | 2.2 | 24.4 | 2.0 | 19.4 | 2.1 | 21.6 | 0.9 | 24.2 | 2.6 | 23.2 | 1.1 | 23.7 | 0.6 | 20.9 | 0.8 | 21.4 | 0.6 |
| 45-54 | 23.4 | 2.1 | 17.1 | 2.0 | 23.0 | 2.8 | 14.6 | 1.5 | 14.6 | 1.3 | 16.5 | 1.5 | 15.6 | 1.9 | 18.5 | 0.6 | 20.2 | 0.6 | 19.5 | 0.5 |
| 55-64 | 8.8 | 1.2 | 12.7 | 1.8 | 10.4 | 2.0 | 17.8 | 1.6 | 5.5 | 0.6 | 10.9 | 1.4 | 9.8 | 1.4 | 10.1 | 0.6 | 13.0 | 0.5 | 12.0 | 0.4 |
| 65-74 | 6.8 | 1.9 | 7.5 | 2.0 | 9.3 | 2.3 | 15.0 | 1.8 | 4.6 | 0.8 | 5.6 | 2.1 | 7.2 | 1.5 | 7.8 | 0.5 | 10.1 | 0.4 | 9.3 | 0.3 |
| 75 or more | 3.8 | 1.3 | 5.3 | 1.1 | 2.9 | 0.9 | 8.0 | 1.9 | 1.9 | 0.4 | 4.0 | 1.6 | 2.9 | 1.0 | 3.9 | 0.4 | 7.7 | 0.4 | 6.6 | 0.3 |
| Sex | ||||||||||||||||||||
| Female | 53.7 | 2.0 | 55.4 | 2.2 | 54.6 | 1.9 | 47.5 | 1.5 | 47.7 | 1.8 | 51.0 | 2.1 | 50.9 | 2.8 | 55.7 | 0.7 | 51.7 | 0.7 | 51.9 | 0.5 |
| Male | 46.3 | 2.0 | 44.6 | 2.2 | 45.4 | 1.9 | 52.5 | 1.5 | 52.3 | 1.8 | 49.0 | 2.1 | 49.1 | 2.8 | 44.3 | 0.7 | 48.3 | 0.7 | 48.1 | 0.5 |
| Education (Years) | ||||||||||||||||||||
| Less than high school | 18.8 | 2.9 | 11.7 | 2.2 | 34.2 | 2.9 | 30.6 | 2.4 | 45.1 | 1.8 | 34.6 | 2.8 | 19.6 | 1.7 | 24.0 | 1.0 | 13.2 | 0.8 | 17.5 | 0.7 |
| High school | 16.8 | 2.0 | 19.9 | 2.3 | 21.3 | 2.0 | 24.3 | 1.6 | 31.7 | 1.8 | 28.3 | 2.2 | 31.5 | 1.8 | 37.0 | 0.9 | 31.2 | 1.4 | 31.5 | 1.1 |
| Some college | 20.5 | 2.6 | 33.0 | 2.1 | 22.2 | 1.9 | 20.9 | 2.2 | 16.2 | 1.4 | 25.7 | 2.0 | 27.1 | 3.2 | 25.0 | 0.8 | 28.3 | 0.9 | 26.8 | 0.7 |
| College or more | 44.0 | 3.7 | 35.4 | 3.7 | 22.4 | 3.6 | 24.1 | 2.8 | 7.0 | 0.8 | 11.5 | 1.6 | 21.8 | 1.2 | 14.0 | 0.9 | 27.3 | 1.4 | 24.3 | 1.1 |
| Annual Household Income ($) | ||||||||||||||||||||
| $0 - $17,999 | 24.5 | 2.6 | 14.8 | 1.7 | 31.7 | 2.0 | 33.0 | 3.6 | 28.7 | 3.0 | 31.0 | 2.1 | 18.9 | 1.7 | 28.0 | 1.2 | 10.6 | 0.6 | 14.7 | 0.6 |
| $18,000 - $31,999 | 7.9 | 1.3 | 8.1 | 1.6 | 14.3 | 2.6 | 13.9 | 1.5 | 16.5 | 1.4 | 14.3 | 2.2 | 25.9 | 2.0 | 21.6 | 0.8 | 9.4 | 0.5 | 11.5 | 0.4 |
| $32,000 - $54,999 | 17.9 | 2.5 | 14.9 | 2.6 | 18.3 | 2.2 | 20.3 | 1.3 | 18.7 | 1.5 | 19.0 | 2.4 | 22.8 | 1.7 | 21.1 | 0.8 | 15.2 | 0.5 | 16.3 | 0.4 |
| $55,000 or more | 49.7 | 3.8 | 62.2 | 4.0 | 35.7 | 2.7 | 32.9 | 4.5 | 36.1 | 2.3 | 35.7 | 2.8 | 32.4 | 2.3 | 29.2 | 1.3 | 64.8 | 1.2 | 57.4 | 0.9 |
| Nativity | ||||||||||||||||||||
| Foreign-born | 81.9 | 3.3 | 69.9 | 4.4 | 97.0 | 0.5 | 86.3 | 1.6 | 44.1 | 3.1 | 45.2 | 3.1 | 66.6 | 2.8 | 2.3 | 0.3 | 2.9 | 0.4 | 10.8 | 0.8 |
| US-born | 18.1 | 3.3 | 30.1 | 4.4 | 3.0 | 0.5 | 13.8 | 1.6 | 55.9 | 3.1 | 54.8 | 3.1 | 33.4 | 2.8 | 97.7 | 0.3 | 97.1 | 0.4 | 89.2 | 0.8 |
Table 2.
Prevalence of 12-Month and Lifetime Major Depressiona in the United States. Results are from the Collaborative Psychiatric Epidemiology Surveys.
| 12-month Major Depression |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total Sample | 18-24 | 25-34 | 35-44 | 45-54 | 55-64 | 65-74 | 75+ | Foreign-born | US-born | ||
| Chinese | % | 4.6 | 9.8 | 8.3 | 2.7 | 1.9 | 1.0 | 7.8 | 1.8 | 3.7 | 8.8 |
| SE | 1.2 | 4.1 | 2.5 | 1.0 | 1.0 | 1.0 | 7.6 | 1.8 | 1.3 | 2.1 | |
| Filipinos | % | 4.2 | 5.6 | 9.6 | 3.5 | 2.0 | 0.0 | 0.0 | 5.6 | 2.8 | 7.5 |
| SE | 1.1 | 2.5 | 2.9 | 2.0 | 1.5 | 0.0 | 0.0 | 5.6 | 1.1 | 2.0 | |
| Vietnamese | % | 4.2 | 2.4 | 8.0 | 3.6 | 5.5 | 0.0 | 1.3 | 4.8 | 4.1 | 7.0 |
| SE | 1.1 | 2.0 | 3.9 | 2.1 | 1.7 | 0.0 | 1.3 | 4.9 | 1.1 | 6.6 | |
| Cubans | % | 8.0 | 10.1 | 5.1 | 10.0 | 8.1 | 10.3 | 6.5 | 3.7 | 8.4 | 5.4 |
| SE | 0.8 | 3.6 | 2.4 | 2.9 | 2.6 | 2.5 | 2.4 | 2.6 | 0.7 | 2.8 | |
| Mexican Americans | % | 8.0 | 9.3 | 8.9 | 6.6 | 8.5 | 6.2 | 3.9 | 6.2 | 6.8 | 10.4 |
| SE | 0.6 | 1.7 | 1.4 | 1.2 | 1.7 | 3.4 | 3.0 | 4.0 | 0.6 | 1.2 | |
| Puerto Ricans | % | 11.9 | 16.1 | 10.0 | 12.0 | 10.2 | 12.0 | 5.0 | 17.7 | 13.2 | 10.7 |
| SE | 1.5 | 5.0 | 2.5 | 3.0 | 3.0 | 3.9 | 6.3 | 5.9 | 2.1 | 1.9 | |
| Black Caribbeans | % | 7.8 | 13.4 | 9.0 | 4.5 | 1.3 | 15.7 | 4.7 | 4.4 | 4.8 | 13.4 |
| SE | 1.7 | 7.8 | 3.6 | 1.5 | 0.5 | 8.6 | 3.7 | 3.2 | 1.1 | 3.7 | |
| African Americans | % | 6.8 | 9.4 | 7.6 | 6.5 | 7.6 | 5.4 | 2.3 | 0.8 | 8.0 | 7.2 |
| SE | 0.4 | 1.4 | 1.1 | 0.8 | 0.9 | 1.0 | 0.9 | 0.6 | 2.9 | 0.4 | |
| Whites | % | 8.3 | 8.8 | 12.3 | 11.0 | 8.6 | 6.3 | 3.6 | 1.7 | 6.8 | 10.7 |
| SE | 0.3 | 0.9 | 1.0 | 0.7 | 0.7 | 0.8 | 0.6 | 0.8 | 1.9 | 0.4 | |
| Total | % | 8.1 | 9.0 | 11.0 | 9.8 | 8.3 | 6.2 | 3.6 | 1.9 | 6.3 | 10.2 |
| SE | 0.3 | 0.7 | 0.7 | 0.5 | 0.6 | 0.7 | 0.6 | 0.7 | 0.5 | 0.4 | |
| Foreign-born | % | 6.3 | 7.7 | 7.5 | 6.5 | 4.5 | 5.5 | 5.1 | 3.7 | -- | -- |
| SE | 0.5 | 1.7 | 1.1 | 1.0 | 0.9 | 1.7 | 2.1 | 1.1 | -- | -- | |
| US-born | % | 10.2 | 11.5 | 13.9 | 12.4 | 10.1 | 7.8 | 4.3 | 2.8 | -- | -- |
| SE | 0.4 | 0.9 | 1.0 | 0.7 | 0.7 | 0.9 | 0.7 | 1.1 | -- | -- | |
|
Lifetime Major Depression
|
|||||||||||
| Total Sample | 18-24 | 25-34 | 35-44 | 45-54 | 55-64 | 65-74 | 75+ | Foreign-born | US-born | ||
|
|
|||||||||||
| Chinese | % | 10.1 | 15.7 | 14.5 | 4.8 | 5.5 | 13.7 | 14.1 | 18.9 | 7.7 | 21.5 |
| SE | 1.6 | 5.7 | 3.0 | 1.5 | 2.0 | 5.1 | 9.6 | 11.8 | 1.5 | 3.5 | |
| Filipinos | % | 7.2 | 8.7 | 13.2 | 6.5 | 7.4 | 2.2 | 0.0 | 5.6 | 5.2 | 12.0 |
| SE | 1.4 | 2.8 | 3.1 | 2.5 | 3.6 | 1.6 | 0.0 | 5.6 | 1.4 | 3.0 | |
| Vietnamese | % | 8.4 | 2.4 | 12.0 | 6.0 | 13.0 | 5.1 | 8.7 | 4.8 | 8.5 | 7.0 |
| SE | 1.8 | 2.0 | 4.3 | 2.3 | 4.2 | 3.0 | 5.3 | 4.9 | 1.9 | 6.6 | |
| Cubans | % | 17.4 | 23.1 | 15.5 | 15.9 | 19.3 | 19.4 | 14.7 | 15.0 | 17.8 | 14.9 |
| SE | 0.8 | 4.9 | 3.6 | 3.7 | 4.8 | 4.4 | 3.7 | 6.6 | 1.0 | 3.9 | |
| Mexican Americans | % | 14.5 | 13.1 | 16.9 | 13.3 | 16.5 | 14.9 | 10.1 | 6.2 | 11.7 | 19.2 |
| SE | 0.7 | 2.3 | 1.6 | 1.7 | 1.8 | 4.4 | 3.5 | 4.0 | 1.1 | 1.4 | |
| Puerto Ricans | % | 22.2 | 22.2 | 22.0 | 21.2 | 19.5 | 32.4 | 14.0 | 25.2 | 23.5 | 21.2 |
| SE | 1.8 | 6.0 | 4.4 | 3.3 | 4.2 | 7.6 | 9.4 | 6.4 | 2.8 | 2.6 | |
| Black Caribbeans | % | 14.3 | 23.3 | 17.8 | 8.1 | 11.1 | 16.3 | 5.3 | 7.1 | 9.1 | 24.1 |
| SE | 2.3 | 7.6 | 3.1 | 1.9 | 2.9 | 8.6 | 3.8 | 3.8 | 2.1 | 5.1 | |
| African Americans | % | 12.3 | 13.0 | 13.7 | 12.8 | 15.2 | 10.2 | 5.6 | 2.1 | 13.4 | 13.1 |
| SE | 0.5 | 1.5 | 1.3 | 1.3 | 1.4 | 1.4 | 1.3 | 0.8 | 3.4 | 0.6 | |
| Whites | % | 20.4 | 17.6 | 23.4 | 25.6 | 24.5 | 18.3 | 12.8 | 7.8 | 17.2 | 26.1 |
| SE | 0.5 | 1.3 | 1.4 | 1.3 | 1.1 | 1.4 | 1.3 | 1.4 | 2.8 | 0.6 | |
| Total | % | 18.6 | 16.4 | 20.8 | 22.2 | 22.4 | 17.3 | 11.9 | 7.7 | 12.4 | 23.8 |
| SE | 0.4 | 1.0 | 1.0 | 1.0 | 0.9 | 1.2 | 1.1 | 1.2 | 0.8 | 0.6 | |
| Foreign-born | % | 12.4 | 11.1 | 13.4 | 12.2 | 11.2 | 13.2 | 11.7 | 14.6 | -- | -- |
| SE | 0.8 | 2.1 | 1.6 | 1.5 | 1.7 | 2.4 | 3.2 | 3.8 | -- | -- | |
| US-born | % | 23.8 | 21.3 | 26.1 | 28.1 | 27.3 | 21.9 | 15.9 | 10.8 | -- | -- |
| SE | 0.6 | 1.3 | 1.3 | 1.4 | 1.1 | 1.7 | 1.7 | 2.1 | -- | -- | |
Based on World Mental Health Composite International Diagnostic Interview
Figure 1.
Nativity and the Prevalence of Lifetime Major Depression across the life-course. Results are from the Collaborative Psychiatric Epidemiology Surveys.
Age of Onset
The mean age of major depression onset was older for foreign-born respondents (cf. US-born) across nearly all ethnic groups, except for African Americans. However, only the US-born Cuban and Puerto Ricans groups had significantly earlier ages of 12-month and lifetime major depression onset compared to foreign-born Cuban and foreign-born groups (Table 3). In addition, difference tests for mean age of onset for the 8 considered ethnic/racial groups relative to Whites indicated that Cubans (M=29.2; P<0.05) meeting criteria for 12-month major depression were significantly older than Whites (M=24.6). Next, ethnic/racial comparisons, regardless of nativity were conducted. Among respondents meeting 12-moht major depression criteria, the mean age of onset for Cubans (M=29.2; P<0.05) was significantly later than Whites (M=24.6). For lifetime depression, the mean age of onset for Cubans (M=30.2; P<0.01) was significantly later than Whites.
Table 3.
Average age of onset of Major Depressiona among respondents meeting criteria for 12-Month and Lifetime Depression by ethnicity/race. Results are from the Collaborative Psychiatric Epidemiology Surveys.
| Respondents with 12-Month Depression | Respondents with Lifetime Depression | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall Sample | Foreign-born | US-born | Overall Sample | Foreign-born | US-born | |||||||
| Mean | SE | Mean | SE | Mean | SE | Mean | SE | Mean | SE | Mean | SE | |
| Chinese | 25.2 | 3.5 | 28.4 | 4.3 | 19.2 | 1.9 | 28.6 | 2.6 | 28.9 | 3.6 | 28.1 | 3.1 |
| Filipino | 25.9 | 4.2 | 29.0 | 8.5 | 23.2 | 2.2 | 27.6 | 2.6 | 27.7 | 4.3 | 27.5 | 2.4 |
| Vitenamese | 30.0 | 3.0 | 31.3 | 2.8 | n/ab | -- | 28.4 | 2.1 | 29.0 | 2.1 | n/ab | n/a |
| Cubans | 29.2 | 2.2 | 30.6 | 2.3 | 15.8 | 2.7 | 30.2 | 1.3 | 31.9 | 1.4 | 17.9 | 2.1 |
| Puerto Rican | 24.8 | 2.3 | 31.0 | 4.3 | 18.6 | 1.6 | 26.0 | 1.4 | 30.5 | 2.2 | 21.9 | 1.6 |
| Mexican Americans | 23.0 | 1.6 | 23.1 | 2.7 | 22.9 | 1.3 | 23.8 | 1.2 | 23.7 | 2.4 | 24.0 | 1.1 |
| Caribbean Blacks | 23.3 | 1.9 | 26.3 | 3.0 | 20.8 | 2.6 | 23.3 | 0.8 | 25.8 | 2.2 | 21.2 | 0.9 |
| African Americans | 25.9 | 0.9 | 18.9 | 2.9 | 26.1 | 1.0 | 26.7 | 0.5 | 21.6 | 2.2 | 26.8 | 0.5 |
| Whites | 24.6 | 0.6 | 29.6 | 3.3 | 24.5 | 0.6 | 26.2 | 0.5 | 29.2 | 1.9 | 26.2 | 0.5 |
| Total | 24.6 | 0.5 | 26.7 | 1.4 | 24.5 | 0.5 | 26.1 | 0.39 | 27.3 | 1.3 | 26.0 | 0.4 |
Based on World Mental Health Composite International Diagnostic Interview.
Total number of US-born Vietnamese Americans is too small to estimate the mean age of depression onset.
Impairment
African Americans reported higher general functioning role impairment (β=1.95; P<0.01) relative to Whites. Cubans (β=3.03; P<0.10), also, reported higher role impairment relative to Whites; however, the diferences were only marginally statistically significant. Asian subgroups (β=−1.31; P<0.01, β=−1.58; P<0.01, and β=−1.81; P<0.05 for Chinese, Filipinos and Vietnamese respectively) meeting 12-month major depression criteria reported lower general functioning role impairment relative to Whites (Table 4). Ethnic/racial estimates of impairment in the other considered domains did not present consistent statistical differences when compared to Whites. However, among the Asian groups, Filipinos (β=−3.23; P<0.01) and Vietnamese (β2=−3.30; P<0.01) respondents were less likely to report cognitive problems, Chinese respondents (β=−2.81; P<0.05) less likely to report mobility problems, and Chinese (β=−1.81; P<0.05) and Vietnamese (β=−2.56; P<0.05) respondents less likely to report social interaction problems relative to Whites.
Table 4.
World Health Organization Disiablity Assessment Scales-II Fast 30-Day Impairment Ratings among respondents meeting criteria for 12-Month Depressiona. Results are from the Collaborative Psychiatric Epidemiology Surveys.
| Out of Role | Cognition | Mobility | Self-Care | Social Interaction |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| β b | SE | β b | SE | β b | SE | β b | SE | β b | SE | |
| Ethnicity/Racec | ||||||||||
| Chinese | −1.31† | 0.50 | −1.64 | 1.59 | −2.81‡ | 1.38 | −0.36 | 0.61 | −1.8‡ | 0.76 |
| Filipinos | −1.58† | 0.36 | −3.23† | 0.71 | 0.08 | 1.82 | −0.38 | 0.57 | −0.86 | 1.37 |
| Vietnamese | −1.81‡ | 0.76 | −3.30† | 1.26 | −2.02 | 2.52 | −0.29 | 1.14 | −2.56‡ | 1.14 |
| Cubans | 3.03§ | 1.67 | 4.01 | 2.58 | 1.85 | 1.60 | 1.63 | 1.20 | 2.34 | 1.59 |
| Mexican Americans | 0.13 | 0.62 | −1.16 | 0.92 | −0.55 | 0.88 | 0.17 | 0.65 | −0.58 | 0.99 |
| Puerto Ricans | −0.32 | 0.75 | −0.95 | 1.24 | 0.84 | 1.75 | 2.86§ | 1.46 | −0.40 | 1.22 |
| Black Caribbeans | 5.41 | 3.43 | 6.53 | 4.80 | 3.08 | 2.53 | 2.40 | 1.69 | 1.18 | 1.12 |
| African Americans | 1.95† | 0.58 | 0.24 | 0.71 | 0.11 | 0.70 | 0.46 | 0.36 | 0.42 | 0.49 |
Based on World Mental Health Composite International Diagnostic Interview.
Unstandardized regression coefficients. Estimates are age and sex adjusted.
Whites are the reference category
P < 0.01
P < 0.05
P < 0.10
Chronicity and severity
Mexicans (OR=1.54; P<0.01), Puerto Ricans (OR=1.57; P<0.05) and African Americans (OR=1.55; P<0.01) had significantly higher odds of recurrent major depressive episodes compared to Whites after accounting for age and sex (Table 5). Our groups did not differ significantly in their mean QIDS-SR severity score relative to Whites. When the QIDS score was dichotomized, only Puerto Rican respondents (OR=0.45; P<0.05) were less likely than Whites to fall into the more severe category.
Table 5.
Ethnic correlates of recurrent Major Depressiona. Results are from the Collaborative Psychiatric Epidemiology Surveys.
| ORb | 95% CI | |
|---|---|---|
| Race/Ethnicityc | ||
| Whites | 1.00 | -- |
| Chinese | 1.14 | 0.63-2.06 |
| Filipino | 1.69 | 0.89-3.23 |
| Vietnamese | 1.46 | 0.69-3.10 |
| Cubans | 1.30 | 0.85-1.98 |
| Mexican Americans | 1.54† | 1.12-2.12 |
| Puerto Ricans | 1.57‡ | 1.05-2.34 |
| Black Caribbeans | 1.49 | 0.92-2.41 |
| African Americans | 1.66† | 1.33-2.07 |
Based on World Mental Health Composite International Diagnostic Interview.
Estimates are age and sex adjusted
Whites are the reference category
P < 0.01
P < 0.05
Treatment
Overall, about half (50.6%) of respondents meeting 12-months major depression criteria used either pharmacotherapy or psychotherapy in the past-year, but fewer (21.2%) used either depression Guideline concordant therapy (Table 6). Psychotherapy (44.3%) was much more commonly used than pharmacotherapy (33.6%) among all ethnic/racial groups examined. Guideline concordant psychotherapy was also higher than pharmacotherapy for each group, especially among Mexicans and the two Black groups. Multivariate ethnic/racial comparisons of past-year depression care use (i.e., age and sex adjusted) showed that Mexicans (OR=0.48; P<0.05) and African Americans (OR=0.54; P<0.01) meeting 12-month major depression criteria had significantly lower odds of any Guideline concordant depression therapy relative to non-Latino Whites (Table 7). After accounting for depression severity, African Americans (OR-0.55; P<0.01) continued to present significantly lower odds of Guideline concordant therapy, and the lower odds for Mexican Americans were statistically attenuated (OR=0.47; P<0.10).
Table 6.
Prevalence of 12-Month Major Depression Care Use and American Psychiatric Association Guideline Concordant Use among respondents meeting criteria for 12-Month Major depressiona in the United States. Results are from the Collaborative Psychiatric Epidemiology Surveys.
| Use |
||||||
|---|---|---|---|---|---|---|
| Pharmacotherapy | Psychotherapy | Any Therapy | ||||
| % | SE | % | SE | % | SE | |
| Chinese | 17.0 | 7.9 | 33.0 | 10.1 | 33.0 | 10.1 |
| Filipino | 12.5 | 7.9 | 36.6 | 10.9 | 41.9 | 11.3 |
| Vietnamese | 8.7 | 5.3 | 44.5 | 12.0 | 44.5 | 12.0 |
| Cubans | 35.1 | 5.8 | 45.2 | 6.2 | 51.6 | 6.8 |
| Mexican Americans | 19.3 | 4.3 | 29.5 | 4.9 | 33.6 | 4.9 |
| Puerto Ricans | 31.6 | 7.8 | 42.9 | 8.1 | 49.2 | 7.2 |
| Black Caribbeans | 18.4 | 11.4 | 24.0 | 10.8 | 29.2 | 12.0 |
| African Americans | 18.3 | 3.0 | 34.4 | 2.9 | 39.7 | 3.1 |
| Whites | 37.3 | 2.1 | 47.3 | 2.9 | 54.0 | 3.2 |
| Total | 33.6 | 1.8 | 44.3 | 2.5 | 50.6 | 2.7 |
|
Guideline Concordant Use
|
||||||
| Pharmacotherapy | Psychotherapy | Any Therapy | ||||
|
|
||||||
| % | SE | % | SE | % | SE | |
|
|
||||||
| Chinese | 12.1 | 6.2 | 9.7 | 5.8 | 15.1 | 6.9 |
| Filipino | 0.0 | 0.0 | 20.8 | 8.6 | 20.8 | 8.6 |
| Vietnamese | 0.0 | 0.0 | 6.3 | 4.5 | 6.3 | 4.5 |
| Cubans | 14.0 | 3.9 | 23.8 | 5.1 | 25.1 | 5.1 |
| Mexican Americans | 5.6 | 2.7 | 11.2 | 3.8 | 12.1 | 3.8 |
| Puerto Ricans | 12.4 | 6.3 | 18.8 | 5.8 | 24.4 | 8.0 |
| Black Caribbeans | 0.5 | 0.4 | 13.3 | 10.9 | 13.5 | 10.9 |
| African Americans | 4.9 | 1.1 | 13.6 | 2.1 | 14.0 | 2.1 |
| Whites | 12.3 | 1.5 | 20.6 | 1.8 | 23.1 | 1.9 |
| Total | 10.9 | 1.2 | 19.1 | 1.5 | 21.2 | 1.6 |
Based on World Mental Health Composite International Diagnostic Interview.
Table 7.
Ethnic/racial comparisons of Past-year American Psychiatric Association Depression Care Guideline Concordant Therapy in the United States among respondents meeting criteria for 12-Month Major Depressiona. Results are from the Collaborative Psychiatric Epidemiology Surveys.
| Model 1b | Model 2c | |||
|---|---|---|---|---|
| ORd | 95 % CI | ORd | 95 % CI | |
| Race/Ethnicitye | ||||
| Whites | 1.00 | -- | 1.00 | -- |
| Chinese | 0.64 | 0.22-1.86 | 0.37 | 0.05-3.05 |
| Filipino | 0.95 | 0.34-2.67 | 0.43 | 0.07-2.61 |
| Vietnamese | 0.24§ | 0.05-1.14 | 0.37 | 0.07-2.05 |
| Cubans | 1.12 | 0.64-1.99 | 1.29 | 0.63-2.62 |
| Mexican Americans | 0.48‡ | 0.23-0.99 | 0.47§ | 0.19-1.13 |
| Puerto Ricans | 1.11 | 0.47-2.64 | 1.11 | 0.44-2.78 |
| Black Caribbeans | 0.57 | 0.09-3.61 | 0.77 | 0.12-4.89 |
| African Americans | 0.54† | 0.37-0.79 | 0.55† | 0.35-0.85 |
| Severity | ||||
| Mild | -- | -- | 1.00 | -- |
| Moderate/Severe/Very severe | -- | -- | 2.22‡ | 1.00-4.93 |
Based on World Mental Health Composite International Diagnostic Interview.
Model 1 presents the estimated ORs for the study's ethnic and racial groups relative to White respondents.
Model 2 presents the estimated ORs for the study's ethnic and racial groups relative to White respondents controlling for depression severity.
Estimates are age and sex adjusted
Whites are the reference category
P < 0.01
P < 0.05
P < 0.10
DISCUSSION
The epidemiology of major depression in the United States between ethnic and nativity groups varies in prevalence rates, age of onset, severity, disability, and treatment use. This is the first US national study to provide a comprehensive and detailed view of major depression among important US ethnic groups throughout adulthood, and decomposed into ethnic subgroups. Additionally, this is the first study to provide ethnic comparisons of the epidemiology of major depression, chronicity, severity, associated disability, and treatment use. While we observed many differences between ethnic groups, two major findings emerge from this study. First, major depression chronicity was higher among Mexican Americans, Puerto Ricans and African Americans compared to Whites. Secondly, among those meeting 12-month major depression criteria, Vietnamese, Mexican and African Americans were the least likely to receive APA Guideline concordant depression therapy.24 Together, these findings suggest that the excess chronicity and disease burden of major depression we found in the two largest Black and Latino groups in the United States (i.e., Mexican Americans and African Americans) might relate to their lack of consistent access to depression care.
Major depression is a leading cause of disability worldwide, particularly in high-income nations and regions, such as the US and Western Europe.28, 29 Our findings suggest that extant global disease burden projections may underestimate the depression related disability if lack of available mental healthcare and major depression recurrence among ethnic minorities is not well-considered. Compounding extant disease burden underestimates are previously untold inequalities in healthcare and depression morbidity befalling large and increasingly important ethnic minority populations. Reconciling the precision of disease burden estimates with the untoward costs of healthcare inequalities should garner appropriate attention and resources needed to improve public health.
We provided major depression epidemiological evidence that updates ECA work from 30-years ago. The pioneering studies from the ECA have reshaped psychiatric epidemiology to consider age and ethnicity/race as fundamental factors associated with the distribution of psychopathology worldwide.16, 17, 30 Demographically, much has changed over the past decades in the public health of the United States and internationally.31 Compared to when the ECA studies were conducted, middle-aged “baby boomers” are now entering retirement age and Latinos, largely ignored in previous national health surveys until relatively recently, are now the largest ethnic minority in the country.32 Furthermore, in contrast to the ECA, we were able to provide ethnic/racial differences that are often overlooked in previous studies.5 Our major depression estimates for older adults are more detailed by age and ethnicity than previously reported for the US. Nevertheless, additional work is needed to understand major depression among older adults.
Despite growing recognition that the practice of aggregating or lumping ethnic groups in reporting epidemiologic findings ignores important cultural, historical, economic and heath needs of groups, it continues. 4 Our findings indicate that those significant differences among older Latinos were largely driven by the markedly higher rates of major depression among Cubans and Puerto Ricans. Furthermore, our disaggregated findings showed that the prevalence of major depression among the largest Latino ethnicity, Mexican Americans, were nearly identical to those of Whites. In summary, using the same national datasets does not ensure similar findings and promotes misinterpretation. We believe our presentation of disaggregated ethnic/racial data provides the detail necessary to better inform public mental health policy. Finally, our findings indicate that lumping large and heterogeneous ethnic groups is potentially misleading and reduces the value of epidemiologic data.
The prevalence of major depression among foreign-born respondents was roughly half that of the US-born sample. This finding is consistent with the “healthy immigrant hypothesis,” which is born-out of epidemiologic observations that immigrants often have health advantages over US-born co-ethnic groups. 8, 33-35 Our findings suggest that healthy immigrant effects do not hold in older age. In this study, we observed a transition or crossover in prevalence rates of major depression among foreign-born ethnic groups that exceeds their US-born co-ethnic groups in later decades of life. This observation is consistent with the non-linear acculturation-health hypothesis stating that immigrant health advantages yield to the overwhelming effects of socioeconomic disadvantages in later years when health needs and costs rise sharply. 36, 37 While it may be that immigrants are a physically and psychologically advantaged earlier in life, those advantages may succumb to homeland estrangement, social isolation and low income and cumulative adversity as an ethnic minority in the United States. 36, 37 Additional research is needed to replicate our findings and identify risks. Secondly, if modifiable risks for major depression among older immigrants are found, they may prove useful in circumventing the crossover in mental health we observed among immigrants in later years.
Several caveats should be considered when interpreting our findings. First, while this is the largest multiethnic psychiatric epidemiologic study to-date, several ethnic age groups meeting criteria for major depression had few observations, which introduces uncertainty for those estimates. This was particularly true among Asians in older age groups. Our prevalence estimates for immigrants are also more difficult to interpret because they rely on cross-sectional data and thus we cannot separate age from cohort effects. Longitudinal data are needed to better examine the life-course acculturation-health relationship observed in this research report.. Secondly, extensive work was undertaken to ensure survey consistency across ethnic/racial groups;38 however, unrecognized sources of bias may have been introduced to the survey inadvertently. Thirdly, the sampling frame did not include homeless and institutionalized persons, which could yield underestimates, particularly among ethnic/racial minorities who are incarcerated at a higher rate than non-Latino whites nationally.39 Fourthly, the WMH-CIDI has a modest sensitivity and high specificity for detecting “true” psychiatric disorders (e.g., major depression) among CPES respondents. Therefore, it is possible that “true” cases of major depression may have been missed, which could have biased our estimates. Finally, although we restricted our examination of psychotherapy use to mental health professionals, we were unable to determine if the treatments provided were truly “evidence based” as specified in American Psychiatric Association guidelines. 24
CONCLUSION
Major depression is a leading cause of disability worldwide and in the United States.28, 29 We found both excess recurrence and greater severity of major depression among the largest and most socioeconomically disadvantaged US ethnic minorities, namely Mexican and African Americans, concurrent with inequalities in mental healthcare. Secondly, our findings provide support for presenting disaggregated ethnic/racial groups and that ignoring these important differences may yield erroneous and misleading findings. Thirdly, we found that healthy immigrants advantages for young adults did not endure into later decades of life may crossover with the US-born in later life.37 Our findings suggest that extant global burden of disease estimates and projections may undervalue the burden of major depression without duly considering inequalities in healthcare befalling ethnic minorities.
Acknowledgments
Funding sources: Drs. González, Tarraf and Whitfield are supported by the National Institute of Mental Health (R01 MH 84994; González PI). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH and NIMH.
References
- 1.Mathers C, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006 Nov;3(11):e442. doi: 10.1371/journal.pmed.0030442. 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McKenna MT, Michaud CM, Murray CJ, Marks JS. Assessing the burden of disease in the United States using disability-adjusted life years. Am J Prev Med. 2005 Jun;28(5):415–423. doi: 10.1016/j.amepre.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 3.IOM . Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare. The National Academies Press; Washington, DC: 2003. [PubMed] [Google Scholar]
- 4.Jimenez DE, Alegría A, Chih-nan C, Chan D, Laderman M. Prevalence of Psychiatric Illnesses in Older Ethnic Minority Adults. Journal of the American Geriatrics Society. 2010;58(2):256–264. doi: 10.1111/j.1532-5415.2009.02685.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alegría M, Chatterji P, Wells KB, et al. Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatric Services. 2008;59(11):1264–1272. doi: 10.1176/appi.ps.59.11.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.González HM, Vega WA, Williams DR, Tarraf W, West BT, Neighbors HW. Depression Care in the United States: Too Little for Too Few. Arch Gen Psychiatry. 2010;67(1):37–46. doi: 10.1001/archgenpsychiatry.2009.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Williams DR, González HM, Neighbors H, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: results from the National Survey of American Life. Arch Gen Psychiatry. 2007 Mar;64(3):305–315. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- 8.Alegria M, Mulvaney-Day N, Torres M, Polo A, Cao Z, Canino G. Prevalence of psychiatric disorders across Latino subgroups in the United States. Am J Public Health. 2007 Jan;97(1):68–75. doi: 10.2105/AJPH.2006.087205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alegria M, Shrout PE, Woo M, et al. Understanding differences in past year psychiatric disorders for Latinos living in the US. Soc Sci Med. 2007 Jul;65(2):214–230. doi: 10.1016/j.socscimed.2007.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alegria M, Canino G, Shrout PE, et al. Prevalence of mental illness in immigrant and non-immigrant U.S. Latino groups. Am J Psychiatry. 2008 Mar;165(3):359–369. doi: 10.1176/appi.ajp.2007.07040704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alegria M, Chatterji P, Wells K, et al. Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatr Serv. 2008 Nov;59(11):1264–1272. doi: 10.1176/appi.ps.59.11.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003 Jun 18;289(23):3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 13.Weissman MM, Leaf PJ, Tischler GL. Affective disorders in five United States communities. Psychological Medicine. 1988;18:141–153. doi: 10.1017/s0033291700001975. [DOI] [PubMed] [Google Scholar]
- 14.Blazer D, Bachar JR, Hughes DC. Major depression with melancholia: a comparison of middle-aged and elderly adults. J Am Geriatr Soc. 1987 Oct;35(10):927–932. doi: 10.1111/j.1532-5415.1987.tb02294.x. [DOI] [PubMed] [Google Scholar]
- 15.Rabins PV, Black B, German P, et al. The prevalence of psychiatric disorders in elderly residents of public housing. Journals of Gerontology, Series A: Biological Sciences and Medical Sciences. 1996;51A(6):M319–M324. doi: 10.1093/gerona/51a.6.m319. [DOI] [PubMed] [Google Scholar]
- 16.Gallo JJ, Anthony JC, Muthen BO. Age differences in the symptoms of depression: a latent trait analysis. Journal of Gerontology. 1994 Nov;49(6):P251–264. doi: 10.1093/geronj/49.6.p251. [DOI] [PubMed] [Google Scholar]
- 17.Gallo JJ, Cooper-Patrick L, Lasikar S. Depressive symptoms of whites and African Americans aged 60 years and older. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 1998;53B(5):P277–P286. doi: 10.1093/geronb/53b.5.p277. [DOI] [PubMed] [Google Scholar]
- 18.Pennell BE, Bowers A, Carr D, et al. The development and implementation of the National Comorbidity Survey Replication, the National Survey of American Life, and the National Latino and Asian American Survey. Int J Methods Psychiatr Res. 2004;13(4):241–269. doi: 10.1002/mpr.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Haro JM, Arbabzadeh-Bouchez S, Brugha TS, et al. Concordance of the Composite International Diagnostic Interview Version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health surveys. Int J Methods Psychiatr Res. 2006 Dec;15(4):167–180. doi: 10.1002/mpr.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.APA . Diagnostic and statistical manual of mental disorders : DSM-IV. 4th ed. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- 21.Rush AJ, Trivedi MH, Ibrahim HM, et al. The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatry. 2003 Sep 1;54(5):573–583. doi: 10.1016/s0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- 22.WHO . World Health Organization Disability Assessment Schedule II (WHODAS II) World Health Organization; Geneva: 2001. [Google Scholar]
- 23.WHO . International classification of functioning, disability and health: ICF. World Health Organization; Geneva: 2001. [Google Scholar]
- 24.APA . Practice Guideline for the Treatment of Patients With Major Depressive Disorder. American Psychiatric Association; Washington, DC: 2000. [PubMed] [Google Scholar]
- 25.Stata Statistical Software (Release 10.1) College Station, TX: 2008. [computer program] [Google Scholar]
- 26.Heeringa SG, Wagner J, Torres M, Duan N, Adams T, Berglund P. Sample designs and sampling methods for the Collaborative Psychiatric Epidemiology Studies (CPES) Int J Methods Psychiatr Res. 2004;13(4):221–240. doi: 10.1002/mpr.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rust K. Variance Estimation for Complex Estimators in Sample Surveys. Journal of Official Statistics. 1985;1(4):381–397. [Google Scholar]
- 28.Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet. 1997;349(9063):1436–1442. doi: 10.1016/S0140-6736(96)07495-8. [DOI] [PubMed] [Google Scholar]
- 29.McKenna MT, Michaud CM, Murray CJ, Marks JS. Assessing the burden of disease in the United States using disability-adjusted life years. American Journal of Preventive Medicine. 2005 Jun;28(5):415–423. doi: 10.1016/j.amepre.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 30.Weissman MM, Bland RC, Canino GJ, et al. Cross-national epidemiology of major depression and bipolar disorder. Journal of the American Medical Association. 1996 Jul 24-31;276(4):293–299. [PubMed] [Google Scholar]
- 31.Wang Y, Beydoun MA, Liang L, Caballero B, Kumanyika SK. Will all Americans become overweight or obese? estimating the progression and cost of the US obesity epidemic. Obesity (Silver Spring) 2008 Oct;16(10):2323–2330. doi: 10.1038/oby.2008.351. [DOI] [PubMed] [Google Scholar]
- 32.Census . We Are the Americans… Hispanics. U.S. Dept. of the Commerce Economics and Statistics Administration Bureau of the Census; Washington, DC: 2004. [Google Scholar]
- 33.Alderete E, Vega WA, Kolody B, Aguilar-Gaxiola S. Effects of time in the United States and Indian ethnicity on DSM-III-R psychiatric disorders among Mexican Americans in California. Journal of Nervous and Mental Disease. 2000;188(2):90–100. doi: 10.1097/00005053-200002000-00005. [DOI] [PubMed] [Google Scholar]
- 34.Alderete E, Vega WA, Kolody B, Aguilar-Gaxiola S. Lifetime prevalence of and risk factors for psychiatric disorders among Mexican migrant farmworkers in California. American Journal of Public Health. 2000 Apr;90(4):608–614. doi: 10.2105/ajph.90.4.608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alegría M, Canino G, Shrout PE, et al. Prevalence of Mental Illness in Immigrant and Non-Immigrant U.S. Latino Groups. Am J Psychiatry. 2008;165(3):359–369. doi: 10.1176/appi.ajp.2007.07040704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rogler LH, Cortes DE, Malgady RG. Acculturation and mental health status among Hispanics: Convergence and new directions for research. Am Psychol. 1991;46(6):585–597. doi: 10.1037//0003-066x.46.6.585. [DOI] [PubMed] [Google Scholar]
- 37.González HM, Ceballos M, Tarraf W, West BT, Bowen ME, Vega WA. The Health of Older Mexican Americans in the Long Run. American Journal of Public Health. 2009;10(99):1879–1885. doi: 10.2105/AJPH.2008.133744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Alegria M, Vila D, Woo M, et al. Cultural relevance and equivalence in the NLAAS instrument: integrating etic and emic in the development of cross-cultural measures for a psychiatric epidemiology and services study of Latinos. Int J Methods Psychiatr Res. 2004;13(4):270–288. doi: 10.1002/mpr.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sabol WJ, Couture H. Prison Inmates at Midyear 2007. Bureau of Justice Statistics. 2008 http://bjs.ojp.usdoj.gov/index.cfm?ty=pbdetail&iid=1005.