Abstract
Purpose
The objectives of this study were to evaluate whether morphologic differences correlated with urodynamic and clinical characteristics in patients with benign prostatic hyperplasia (BPH) with intravesical prostatic protrusion (IPP) of trilobar or bilobar adenoma.
Materials and Methods
Between January 2008 and June 2009, 72 male patients who had undergone transurethral resection (TUR) owing to BPH with IPP were included in this study. They underwent preoperative urodynamic studies, the International Prostate Symptom Score (IPSS)/quality of life (QoL), maximal flow rate (Qmax), post-voiding residual urine volume (PVR), transrectal ultrasonography (TRUS), and serum prostate-specific antigen (PSA) measurement. The patients were classified into 2 groups (the trilobar and bilobar adenoma groups) on the basis of video findings during the TUR operation.
Results
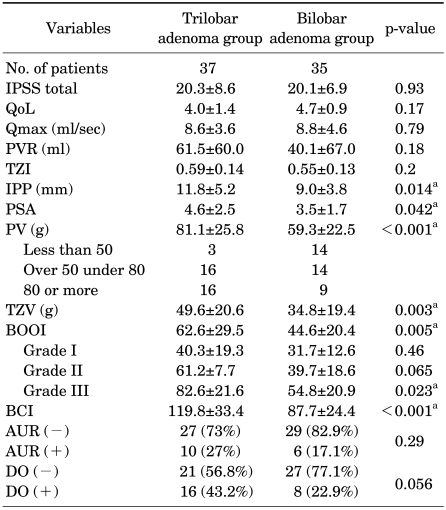
The trilobar and bilobar adenoma groups consisted of 37 patients and 35 patients, respectively. The Mean±SD IPP, prostate volume (PV), and transition zone volume of the trilobar and bilobar adenoma groups were 11.8±5.2 mm and 9.0±3.8 mm (p=0.014), 81.1±25.8 g and 59.3±22.5 g (p<0.001), and 49.6±20.6 g and 34.8±19.4 g (p=0.003), respectively. The Mean±SD PSA, bladder contractility index (BCI), and bladder outlet obstruction index (BOOI) were 4.6±2.5 ng/ml and 3.5±1.7 ng/ml (p=0.042), 119.8±33.4 and 87.7±24.4 (p<0.001), and 62.6±29.5 and 44.6±20.4 (p=0.005), respectively. There were no significant differences in IPSS/QoL, Qmax, PVR, acute urinary retention, or detrusor overactivity in the 2 groups.
Conclusions
IPP has two morphologic types of trilobar or bilobar enlargement. The PV, BOOI, and BCI were significantly smaller in the bilobar adenoma group than in the trilobar adenoma group.
Keywords: Prostatic hyperplasia, Ultrasonography, Urodynamics
INTRODUCTION
Benign prostatic enlargement is known to be the most common cause of bladder outlet obstruction (BOO) in male adults in their 50s or older [1,2]. The proper selection of patients is essential for adequate treatment in a clinical setting. Many tests have been proposed as the criteria for evaluation and selection of patients with prostatic enlargement, among which urodynamic tests are known to be the most helpful in the diagnosis of such patents [3,4]. However, these tests have some limitations in clinical application owing to their invasiveness and complications. Thus, a method for evaluating the degree of BOO by ultrasonography has been introduced. Since intravesical prostatic protrusion (IPP) assessed by ultrasonography has a significant correlation with the BOO index (BOOI), it is used as a potent predictor of BOO [5]. Although IPP has been widely used as a predictor of BOO, morphological patterns of IPP have not yet been determined. Doo and Uh reported that there are significant differences in clinical parameters according to the structure of the prostate [6].
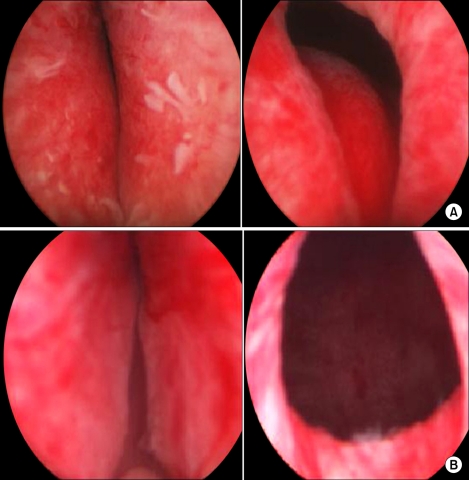
IPP usually presents with 2 patterns at surgery: (1) the transition zone is enlarged and protrudes into the bladder, which is called bilobar adenoma, and (2) both the central and transition zones protrude into the bladder, which is called trilobar adenoma [6].
Although IPP is usually found in a trilobar adenoma, where the median lobe of the prostate protrudes into the bladder, IPP with enlargement of the lateral lobe and no prominent median lobe is sometimes observed during transurethral resection of the prostate (TURP). Therefore, this study was conducted to determine the prevalence of trilobar and bilobar adenomas and to evaluate the relationship between morphological patterns and clinical and urodynamic parameters.
MATERIALS AND METHODS
1. Study subjects
In this study, we retrospectively analyzed 72 patients with IPP confirmed by transrectal ultrasonography (TRUS) among 121 patients who underwent TURP between January 2008 and June 2009. The following patients were excluded from the study: (1) those with bladder cancers, (2) those with bladder stones, (3) those with neurogenic bladders, and (4) those on medication with anticholinergics.
2. Methods
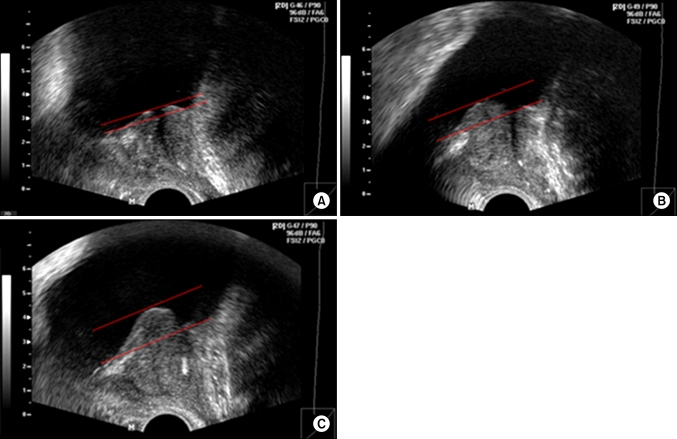
We investigated the correlations between morphological patterns of IPP and preoperative urodynamic test results, TRUS findings, International Prostate Symptom Score (IPSS), quality of life (QoL), and uroflowmetric results. We also investigated the correlations between morphological patterns of IPP and IPSS, QoL, and uroflowmetric results obtained 3 months after TURP. TRUS was performed with a 5 MHz transverse transducer and a 7.5 MHz longitudinal transducer by a urologist. The maximum transverse and longitudinal diameters of the prostate were measured, and prostate volume (PV) was calculated by the following formula: PV = width x height x length x (π/6). The degree of IPP was defined as the shortest diameter between the bladder neck and the tip of the IPP on a sagittal image as described by Mariappan et al [7]. It was divided into 3 grades: grade I, an IPP of <5 mm; grade II, an IPP of 5 to 10 mm; and grade III, an IPP of >10 mm (Fig. 1).
FIG. 1.
The grading system for IPP. (A) Grade I (<5 mm), (B) Grade II (5-10 mm), and (C) Grade III (>10 mm) IPP. IPP: intravesical prostatic protrusion.
The protrusion of the median and lateral lobes was evaluated through operative videotapes. By operative endoscopy, bilobar adenoma was defined as a prominent lateral lobe with a kissing appearance without a prominent median lobe (the bilobar adenoma group), and trilobar adenoma was defined as a prominent median lobe that covered more than half of the bladder neck (the trilobar adenoma group) (Fig. 2). Adenomas with protrusion of a unilateral lobe or a median lobe only were excluded.
FIG. 2.
Anatomical differences in IPP configuration between trilobar (A) and bilobar (B) adenomas. IPP: intravesical prostatic protrusion.
3. Statistical analysis
Statistical comparisons of preoperative IPSS, QoL, uroflowmetric results, serum prostate-specific antigen (PSA), PV, transition zone volume (TZV), transition zone index (TZI), BOOI, and bladder contractility index (BCI) between the 2 groups were made with the independent t-test. Comparisons of preoperative acute urinary retention (AUR) and detrusor overactivity (DO) between the 2 groups were made with the chi-square test. The association between IPP and the aforementioned parameters was tested with the Pearson's correlation coefficient and chi-square. All statistical analyses were performed by using the SPSS program version 12.0. A p-value of <0.05 was considered statistically significant.
RESULTS
The mean age of the patients was 68.4±6.2 years. Mean serum PSA was 4.1±2.2 ng/ml. Mean PV was 70.5±26.4 g, and mean TZV was 42.4±21.2 g. Mean TZI was 0.58±0.14 g. The mean weight of the prostate adenoma resected by TURP was 34.6±17.2 g. The mean length of IPP was 10.4±4.8 mm; grade I was observed in 9 patients (12.5%), grade II in 30 patients (41.7%), and grade III in 33 patients (45.8%).
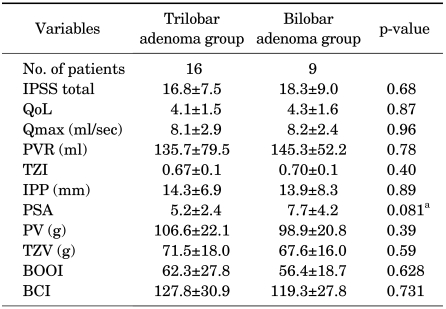
The trilobar group included 37 patients (51.4%), and the bilobar group included 35 patients (48.6%). There were no significant differences in preoperative IPSS, QoL, urine volume, maximal flow rate (Qmax), residual urine, TZI, or weight of the resected prostate adenoma between the 2 groups. However, there were significant differences in IPP (11.8±5.2 mm vs. 9.0±3.8 mm, p=0.014), PV (81.1±25.8 g vs. 59.3±22.5 g, p< 0.001), TZV (49.6±20.6 g vs. 34.8±19.4 g, p=0.003), BOOI (62.6±29.5 vs. 44.6±20.4, p=0.005), and BCI (119.8±33.4 vs. 87.1±24.4, p<0.001) between the 2 groups (Table 1). There were no significant differences in IPSS, QoL, urine volume, Qmax, or residual urine at the 3-month follow-up between the 2 groups.
TABLE 1.
Comparisons of the trilobar and bilobar adenoma groups
IPSS: International Prostate Symptom Score, QoL: quality of life, Qmax: maximal flow rate, PVR: postvoid residual urine, TZI: transition zone index, IPP: intravesical prostatic protrusion, PSA: prostate-specific antigen, PV: prostate volume, TZV: transition zone volume, BOOI: bladder outlet obstruction index, BCI: bladder contractility index, AUR: acute urinary retention, DO: detrusor overactivity, a: p<0.05
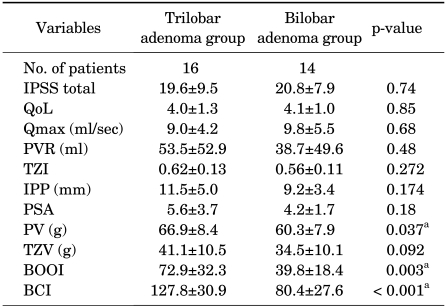
In the groups with grades I and II IPP, there were no significant differences in the BOOI between the 2 groups. In the grade III group, however, the BOOI was significantly higher in the trilobar adenoma group than in the bilobar adenoma group (Table 1). In cases with a PV over 50 and under 80, PV and the BOOI were significantly higher in the trilobar adenoma group than in the bilobar adenoma group (Table 2, 3).
TABLE 2.
Comparisons of the trilobar and bilobar adenoma groups (prostate volume over 50 and under 80)
IPSS: International Prostate Symptom Score, QoL: quality of life, Qmax: maximal flow rate, PVR: postvoid residual urine, TZI: transition zone index, IPP: intravesical prostatic protrusion, PSA: prostate-specific antigen, PV: prostate volume, TZV: transition zone volume, BOOI: bladder outlet obstruction index, BCI: bladder contractility index, a: p<0.05
TABLE 3.
Comparisons of the trilobar and bilobar adenoma groups (prostate volume 80 or more)
IPSS: International Prostate Symptom Score, QoL: quality of life, Qmax: maximal flow rate, PVR: postvoid residual urine, TZI: transition zone index, IPP: intravesical prostatic protrusion, PSA: prostate-specific antigen, PV: prostate volume, TZV: transition zone volume, BOOI: bladder outlet obstruction index, BCI: bladder contractility index, a: p<0.05
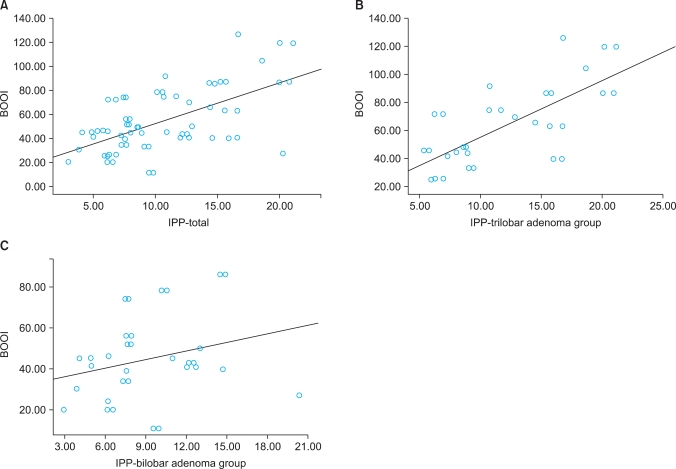
AUR and DO were higher in the trilobar adenoma group than in the bilobar adenoma group, but the difference was not statistically significant (Table 1). In the trilobar adenoma group, IPP had a significant correlation with the BOOI (r=0.718, p<0.001), whereas in the bilobar adenoma group, it had no significant correlation with the BOOI (r=0.265, p=0.136) (Fig. 3).
FIG. 3.
Scatter plot of the relationship between BOOI and IPP. (A) Scatter plot of the relationship between BOOI and IPP in the total patients (r=0.608, p<0.001). (B) Scatter plot of the relationship between BOOI and IPP in the trilobar adenoma group (r=0.718, p<0.001). (C) Scatter plot of the relationship between BOOI and IPP in the bilobar adenoma group (r=0.265, p=0.136). BOOI: bladder outlet obstruction index, IPP: intravesical prostatic protrusion.
During hospitalization, blood transfusion was performed on 3 patients (8.1%) and 2 patients (5.7%) in the trilobar and bilobar adenoma groups, respectively. AUR due to blood clotting was observed in 7 patients (18.9%) and 4 patients (11.4%) in the trilobar and bilobar adenoma groups, respectively, whereas infection signs such as fever due to urinary tract infections were noted in 2 patients (5.4%) and 2 patients (5.7%), respectively. These differences were not statistically significant.
DISCUSSION
Numerous studies have pointed out that BOO cannot be accurately diagnosed on the basis of a single factor such as urinary symptoms, residual urine, or Qmax [8,9]. Ultrasonography has been widely used to examine the prostate owing to its safety and noninvasiveness. Chia et al reported that IPP assessed by ultrasonography is an excellent criterion for predicting BOO [5]. Nose et al documented that the IPP grading system and Doppler urodynamic study have high sensitivities and specificities in the prediction of BOO [10]. Mariappan et al reported that when trial without catheter was performed on AUR patients 2 weeks after administration of α-blockers, the degree of IPP was more potent for the prediction of successful urination than was PV [7]. Although IPP has been widely applied because of its clinical usefulness, there have been few studies on the morphological patterns and clinical implications of IPP.
IPP is a morphological change by which the prostate protrudes into the bladder during the process of prostatic enlargement. It is induced by the enlargement of the lateral and median lobes, which leads to the ball-valve type of BOO and abnormal movement of the bladder due to the inhibition of the funnel effect of the bladder neck at urination [11,12]. Chia et al have described that because strong bladder contraction opens the channel between the lateral lobes but accelerates the ball-valve effect by IPP, IPP induces more BOO than does the enlargement of the lateral lobe alone or prostatic enlargement without protrusion [5]. Early treatment including surgery is recommended for patients with IPP because IPP differs from dynamic obstruction by an increase in prostatic smooth muscle tone [13]. In this study, urodynamic tests showed that BOO was less severe in the bilobar adenoma group than in the trilobar adenoma group. In addition, PV was smaller in the bilobar adenoma group than in the trilobar adenoma group (81.1±25.8 g vs. 59.4±22.5 g, p<0.001), but the mean BOOI was >40. These results imply that the ball-valve effect may exist in the bilobar adenoma group. It is conceivable that unilateral or bilateral lateral lobes that protruded to and floated in the bladder may have exerted the ball effect, unlike in the trilobar adenoma group where the median lobe exerted the ball effect. It is also conceivable that in the bilobar adenoma group, grade III IPP showed a greater BOOI than did grade I (54.8±20.9 vs. 31.7±12.6, p<0.05).
Because morphological patterns of IPP were difficult to discriminate between trilobar and bilobar adenomas, the AUC values of IPP, PV, and TZV were measured by ROC curve analysis. Among these 3 parameters, PV showed the highest AUC value (AUC, 0.737); PV showed the highest sensitivity and specificity when it was 64.5 g (sensitivity, 80.6%; specificity, 60.0%). A number of patients with both grade III by TRUS and a PV of >60 g have the possibility of trilobar adenomas with apparently protruding median lobes, subsequently leading to severe BOO.
The BCI was significantly lower in the bilobar adenoma group than in the trilobar adenoma group. BCI was measured by using the formula introduced by Abrams [3]:
BCI=PdetQmax+5Qmax
Because at urination, BOO was more severe in the trilobar adenoma group than in the bilobar adenoma group, bladder contractility was more elevated in order to overcome the resistance, which subsequently led to an increase in PdetQmax. In contrast, it is thought that because the resistance was smaller in the bilobar adenoma group, Pdet-Qmax was decreased and BCI was lower. In this study, because patients with neurogenic bladders and those on medication with anticholinergics were excluded from the randomly selected study samples, considerable selection bias may have been avoided.
Transabdominal ultrasonography has been used since the introduction of the concept of IPP. Mariappan et al used TRUS to measure the size of IPP and the prostate and confirmed that there was a significant correlation between IPP and BOO [7]. TRUS has some advantages over transabdominal ultrasonography: (1) transabdominal ultrasonography requires the bladder to be filled with 150 to 200 ml of normal saline, which may cause patient discomfort; (2) clinicians are more familiar with TRUS because TRUS is more frequently performed in a clinical setting than transabdominal ultrasonography; and (3) IPP assessed by TRUS is able to excellently predict BOO in clinical practice. It has been reported that clinical parameters such as IPSS and QoL do not correlate with BOO [14], which is similar to our result.
We acknowledge, however, the potential limitations of this study: (1) it is a retrospective study and (2) because there are no definite criteria for discrimination between trilobar and bilobar adenomas, there may have been bias in our results. However, despite the bias, this study provides the basis for understanding morphological patterns of IPP and urodynamic differences according to morphological changes in the prostate.
CONCLUSIONS
All IPPs assessed by TRUS did not represent trilobar adenomas with apparent enlargement of the median lobe of the prostate. The results of this study confirm that the degree of IPP, PV, BOOI, and BCI were significantly smaller in the bilobar adenoma group than in the trilobar adenoma group. More research with a prospective study design and a larger sample size is needed to establish definite criteria for determination of morphological patterns of IPP.
Footnotes
The authors have nothing to disclose.
References
- 1.Lim KB, Ho H, Foo KT, Wong MY, Fook-Chong S. Comparison of intravesical prostatic protrusion, prostate volume and serum prostatic-specific antigen in the evaluation of bladder outlet obstruction. Int J Urol. 2006;13:1509–1513. doi: 10.1111/j.1442-2042.2006.01611.x. [DOI] [PubMed] [Google Scholar]
- 2.Chung HY, Han DS, Jang YS, Song KH. The influences of bladder outlet obstruction on improvement of storage symptoms in patients who underwent transurethral resection of prostate. Korean J Urol. 2008;49:912–916. [Google Scholar]
- 3.Abrams P. Bladder outlet obstruction index, bladder contractility index and bladder voiding efficiency: three simple indices to define bladder voiding function. BJU Int. 1999;84:14–15. doi: 10.1046/j.1464-410x.1999.00121.x. [DOI] [PubMed] [Google Scholar]
- 4.Jung YS, Hwang TK, Kim JC. The outcome and satisfaction of patients with lower urinary tract symptoms/benign prostatic hyperplasia following transurethral resection of the prostate according to urodynamic obstruction and the bladder function. Korean J Urol. 2007;48:965–970. [Google Scholar]
- 5.Chia SJ, Heng CT, Chan SP, Foo KT. Correlation of intravesical prostatic protrusion with bladder outlet obstruction. BJU Int. 2003;91:371–374. doi: 10.1046/j.1464-410x.2003.04088.x. [DOI] [PubMed] [Google Scholar]
- 6.Doo CK, Uh HS. Anatomic configuration of prostate obtained by noninvasive ultrasonography can predict clinical voiding parameters for determining BOO in men with LUTS. Urology. 2009;73:232–236. doi: 10.1016/j.urology.2008.09.055. [DOI] [PubMed] [Google Scholar]
- 7.Mariappan P, Brown DJ, McNeill AS. Intravesical prostatic protrusion is better than prostate volume in predicting the outcome of trial without catheter in white men presenting with acute urinary retention: a prospective clinical study. J Urol. 2007;178:573–577. doi: 10.1016/j.juro.2007.03.116. [DOI] [PubMed] [Google Scholar]
- 8.Rosier PF, de Wildt MJ, Wijkstra H, Debruyne FF, de la Rosette JJ. Clinical diagnosis of bladder outlet obstruction in patients with benign prostatic enlargement and lower urinary tract symptoms: development and urodynamic validation of a clinical prostate score for the objective diagnosis of bladder outlet obstruction. J Urol. 1996;155:1649–1654. [PubMed] [Google Scholar]
- 9.el Din KE, Kiemeney LA, de Wildt MJ, Rosier PF, Debruyne FM, de la Rosette JJ. The correlation between bladder outlet obstruction and lower urinary tract symptoms as measured by the international prostate symptom score. J Urol. 1996;156:1020–1025. doi: 10.1097/00005392-199609000-00050. [DOI] [PubMed] [Google Scholar]
- 10.Nose H, Foo KT, Lim KB, Yokoyama T, Ozawa H, Kumon H. Accuracy of two noninvasive methods of diagnosing bladder outlet obstruction using ultrasonography: intravesical prostatic protrusion and velocity-flow video urodynamics. Urology. 2005;65:493–497. doi: 10.1016/j.urology.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 11.Kuo HC. Clinical prostate score for diagnosis of bladder outlet obstruction by prostate measurements and uroflowmetry. Urology. 1999;54:90–96. doi: 10.1016/s0090-4295(99)00092-8. [DOI] [PubMed] [Google Scholar]
- 12.Keqin Z, Zhishun X, Jing Z, Haixin W, Dongqing Z, Benkang S. Clinical significance of intravesical prostatic protrusion in patients with benign prostatic enlargement. Urology. 2007;70:1096–1099. doi: 10.1016/j.urology.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 13.Tan YH, Foo KT. Intravesical prostatic protrusion predicts the outcome of a trial without catheter following acute urine retention. J Urol. 2003;170:2339–2341. doi: 10.1097/01.ju.0000095474.86981.00. [DOI] [PubMed] [Google Scholar]
- 14.Chancellor MB, Rivas DA, Keeley FX, Lotfi MA, Gomella LG. Similarity of the American Urological Association Symptom Index among men with benign prostate hyperplasia (BPH), urethral obstruction not due to BPH and detrusor hyperreflexia without outlet obstruction. Br J Urol. 1994;74:200–203. doi: 10.1111/j.1464-410x.1994.tb16586.x. [DOI] [PubMed] [Google Scholar]