Abstract
In December 2004, Togo was the first country to conduct a nationwide free insecticide-treated net (ITN) distribution as part of its National Integrated Child Health Campaign. Community-based cross-sectional surveys were conducted one and nine months post-campaign as part of a multidisciplinary evaluation of the nationwide distribution of ITNs to children 9–59 months of age to evaluate ITN ownership, equity, and use. Our results demonstrated that at one month post-campaign, 93.1% of all eligible children received an ITN. Household ITN ownership and equity increased significantly post-campaign. Nine months post-campaign, 78.6% of households with a child eligible to participate in the campaign retained at least one campaign net. Use by eligible children was 43.5% at one month post-campaign (during the dry season) and 52.9% at nine months post-campaign (during the rainy season). Household ownership of at least one ITN increased from 8.0% pre-campaign to 62.5% one month post-campaign. Together, these findings demonstrate that in this setting, increased household ITN ownership, equity, and retention can be achieved on a national scale through free ITN distribution during an integrated campaign.
Introduction
In 2000, the Roll Back Malaria (RBM) Partnership committed to increase insecticide-treated net (ITN) coverage among high risk groups, namely young children (children less than five years of age) and pregnant women, to more than 60%.1 This goal has since been increased to universal coverage of all people in malaria-risk areas by appropriate prevention interventions including ITNs.2 High coverage with ITNs has been shown to be effective in averting approximately one in five infant deaths in areas of intense transmission.3 However, the challenge remains in establishing delivery methods that provide high and equitable coverage among high risk groups regardless of socioeconomic status. Free mass distribution of ITNs through immunization or antenatal clinics or by vaccination or deworming campaigns have been found to achieve high coverage among the poorest children.4
In Togo, a country with 5.8 million persons, 17.2% of the population is less than five years of age.5,6 In 2003, malaria was estimated to have accounted for approximately one-fourth to one-third of all deaths in children in Togo less than five years of age (Ministry of Health, 2005, unpublished data). In December 2004, the Togo National Integrated Child Health campaign provided a free ITN for each child between the ages of nine months and five years along with measles and polio vaccinations and presumptive treatment of helminthic infection. This campaign was the first national distribution of ITNs coupled with a vaccination campaign. Previous sub-national campaigns in one district in Ghana and five districts in Zambia7,8 showed rapid increase in ITN ownership and use when free distribution was paired with a vaccination campaign. Although bed net ownership and use in Togo were low before the integrated campaign, immunization coverage in Expanded Program on Immunization campaigns was more than 90%.
The primary objective of the integrated campaign was to reduce morbidity and mortality of young children in Togo by high population coverage with measles vaccination and ITNs. To evaluate this campaign, cross-sectional coverage surveys were conducted to evaluate delivery of services (January 2005) and ITN ownership and use (January and September 2005) post-campaign. We present results of these surveys. Methods of the integrated campaign and preliminary results from the first survey have been reported.9 Therefore, we focus primarily on results from the second survey.
Methods
Campaign and evaluation timeline.
The distribution campaign was conducted during December 13–19, 2004. In addition to the distribution of long-lasting insecticide-treated mosquito nets (LLINs), the campaign provided measles vaccination, polio vaccination, and mebendazole for deworming. At the time of distribution, families were provided information on use and care of LLINs and encouraged to use their nets nightly.
The multidisciplinary evaluation of the campaign had the following components: morbidity/anemia surveys conducted in September 2004 (baseline) and September 2005; a coverage survey measuring campaign efficiency (the proportion of the specific population receiving one or more of the campaign interventions) and ITN ownership and use in January 2005; a coverage survey measuring ITN ownership and use in September 2005; and a mortality survey conducted during December 2007–March 2008. After the distribution campaign and before the January 2005 survey, more than 15,000 community-based volunteers were reported to have visited 762,937 households and encouraged those with nets, especially pregnant women and children less than five years of age, to hang and use them.
Study site.
Both coverage surveys were conducted in urban and rural communities from all six regions in Togo (Lomé, Maritime, Plateaux, Centrale, Kara, Savanes). The classification as urban or rural was provided by the Togo Department of Statistics on the basis of the 2000 census.
Because of the necessity of integrating the two coverage surveys with other components of the multidisciplinary evaluation, sampling methods differed somewhat between the first and second surveys. For the January 2005 survey, two districts were selected from each of the six regions by probability proportional to size sampling for 12 of 21 districts nationwide. Within all selected districts, probability proportional to size was used to select 12 enumeration areas (EAs), which are non-politically recognized census blocks; this selection provided 72 of 4,842 EAs nationwide. Within each EA, a simple random sample of 16 households was selected regardless of the presence of children less than five years of age, with five alternates in case no one was available at a selected household.10 For operational and financial reasons, the September coverage survey took place in combination with the follow-up morbidity/anemia survey. The previous morbidity/anemia survey had been carried out in Yoto District in Maritime Region, Ogou District in Plateaux Region, and in Tone District in Savanes Region to represent malaria transmission patterns in the southern, central, and northern areas of the country, respectively. For these three regions, the same three districts were included in the September coverage survey in place of the two districts selected in the January survey. For these districts, within each EA, a random sample of 27 households with six alternates was selected. Because weights were computed separately for each survey, national estimates between the two surveys were comparable. These weights, which were used in all estimates and confidence interval computations, accounted for the different urban/rural sampling fractions. Where possible, one selected district from each region had an active Red Cross promotion to hang up nets before the evaluation. All selected households were invited to participate in the September 2005 coverage survey.
Survey design.
The distribution campaign was conducted during December 13–19, 2004. The first coverage survey took place (January 24–February 4, 2005), one month post-campaign, during the dry season. We conducted the second coverage survey (September 12–October 8, 2005), nine months post-campaign, during rainy season, presumably when malaria transmission was at its annual peak (Figure 1). Both surveys used a community-based cross-sectional survey design with a stratified three-stage cluster sampling strategy. District level sample sizes were based on an assumed household ITN coverage of 65%. The study was designed to estimate the proportion of households who received an ITN during the campaign within a range of 4% with 95% confidence, assuming a non-response rate of 10% and a design effect of 1.2. The Togo Department of Statistics provided the sampling frame with defined enumeration areas with populations between 452 and 1,440 persons. Sample sizes were calculated by using the StatCalc module (EpiInfo 2000, Centers for Disease Control and Prevention, Atlanta, GA).
Figure 1.
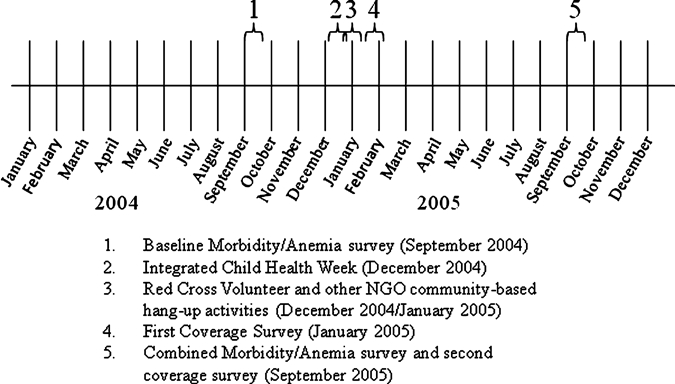
Timeline of intervention and surveys, Togo, 2004.
The January 2005 survey measured campaign coverage, efficiency of the campaign in reaching the target population, equity, and net use during the dry season. The September 2005 survey primarily measured ITN retention and use during the high malaria transmission season. Both surveys contained several components, including questions about ITN ownership, use, care, and retention including net use among pregnant women and children less than five years of age. Information was also elicited to assess impact of post-campaign social mobilization activities to encourage ITN use. Additionally, household characteristics and economic status were included. Questionnaires were administered by trained enumerators to primary childcare providers in selected households. All answers were entered directly into a database on handheld computers in the field (Visual CE version 9.0; Syware Inc., Cambridge, MA). The data were downloaded at the end of the survey into a Microsoft (Redmond, WA) Access database.
Definitions.
Households were defined as consisting of the head of household and all his spouses and children living in the same compound or if a female headed household, the head and all of her dependents. Coverage was defined as the proportion of the target population that received a particular intervention during the integrated campaign. Equitable coverage was defined as equal access to the interventions between households determined to be in the highest and lowest wealth quintiles. Eligible children were defined as children 9–59 months of age at the time of the campaign. The ITNs were defined as either long-lasting insecticidal nets (LLIN, including the brands PermaNet®, Olyset® Net, or Serena Net) or conventional nets that had been treated with insecticide within the previous 12 months. Serena Net, which is marketed by Population Services International (Washington, DC), is also a PermaNet,® However, it is branded and distributed differently. Surveyors were trained to physically examine nets to distinguish among net brands. If a net was long lasting, re-treatment history was not taken. Ownership was defined categorically: possession of any bed net, possession of an ITN, or possession of a campaign net. Households were classified into wealth quintiles on the basis of an asset score calculated by using World Bank criteria.11 Because of tied values in the socioeconomic status index, there were unequal numbers of households in each of the quintiles.
Statistical analyses.
Analyses were performed by using SAS version 9.1 (SAS Institute, Cary, NC). Household, child, and bed net/ITN analyses were weighted for the sampling design on the basis of the probability of being selected. The SAS survey procedures (Proc SurveyFreq, Proc SurveyLogistic) were used to produce valid estimates and standard errors accounted for the stratified and clustered sampling design. Rao-Scott chi-square statistics were used for tests of association. The data were clustered by household for child indicators, by enumeration area for household level indicators, and the prefecture was used to define the strata in the sample. Tests of trend were performed by using general estimating equations with an exchangeable correlation structure. Economic equity ratio was calculated as the ratio of proportions in the poorest quintile to the wealthiest quintile.
Results
Household characteristics.
During the first survey, 2,254 households were interviewed, of which 63.8% were rural and 36.2% were urban. During the second survey, 3,523 households were surveyed, of which 86% were rural and 14% were urban. The difference in urban/rural distribution was caused by the inclusion of different districts in the second coverage survey to accommodate the study design for the morbidity/anemia survey. The selected enumeration areas for the morbidity/anemia survey were more urban, as defined Department of Statistics of Togo. Overall, 77.2% of households in the first survey and 72.8% of households in the second survey had at least one child less than five years of age.
Campaign attendance and ITN distribution.
The first survey showed that 96.2% of all eligible children (nine months to five years of age at the time of the campaign) attended the campaign. Persons reported hearing about the campaign through community mobilizers (46.8%), radio (36.4%), and community leaders (28.8%). The most common reasons caretakers reported for taking the child to the campaign were to receive an ITN (58.9%), to receive a polio vaccination (57.4%), and to receive a measles vaccination (52.7%). The reason provided was generally one of the three main interventions. Of persons who did not attend the campaign, the most common reason was families being away from home during that time (38.1%).
As previously reported,9 among all children nine months to five years of age, coverage for eligible children was 93.1% (95% confidence interval [CI] = 90.9–96.4%) for measles vaccine, 93.7% (95% CI = 91.7–99.1%) for polio vaccine, 92.7% (95% CI = 90.6–95.5%) for mebendazole, and 90.8% (95% CI = 84.4–98.0%) for an ITN. Of the 7.1% of eligible children who did not attend the campaign, the most common reasons for not receiving an ITN from the campaign were an absence of workers at the ITN station at the time they went (49.0%) or vaccination posts were out of nets (34.0%).
ITN ownership and equity.
Household ownership of ITNs increased from 8.0% (95% CI = 5.7–10.2%) of all households (including households that were not eligible to participate in the campaign) before the December campaign to 62.5% (95% CI = 58.3–66.6%) in January. At nine months post-campaign, 63.8% (95% CI = 61.3–66.3%) of households owned at least one net of any kind, and ITN ownership in all households was similar at 59.7% (95% CI = 57.2–62.2%) (Table 1). Among households with at least one child less than five years of age, 73.4% (95% CI = 70.4–76.5%) of households had at least one ITN. It should be noted that at the time of the second survey only children 18–69 months of age would have been eligible to have received an ITN at the time of the campaign because of the age change of the original cohort.
Table 1.
Percentage of households owning nets before, one month, and nine months post-campaign, Togo, 2004*
| Characteristic | Pre-campaign (n = 2,254) | 1 month post-campaign (n = 2,254) | 9 months post-campaign (n = 3,523) |
|---|---|---|---|
| Household ownership of any net | 18.9% (15.3–22.6%) | 65.6% (61.1–70.2%) | 63.8% (61.3–66.3%) |
| Household ownership of an ITN | 8.0% (5.7–10.2%) | 62.5% (58.3–66.6%) | 59.7% (57.2–62.2%) |
ITN = insecticide-treated net. Values in parentheses are 95% confidence intervals. Data reflect ownership from the first coverage survey (reported pre-campaign and 1 month post-campaign) and the second coverage survey (9 month post-campaign).
Before the December campaign, coverage was substantially lower in the poorest quintiles compared with the wealthiest (equity ratio = 0.25, 95% CI = 0.05–0.46), and there was a strong statistical association between greater wealth and higher coverage (P < 0.001). Nine months post-campaign, household ownership was similar across all economic quintiles with an equity ratio among ITN owners of 1.0 (95% CI = 0.87–1.14) (Figure 2).
Figure 2.
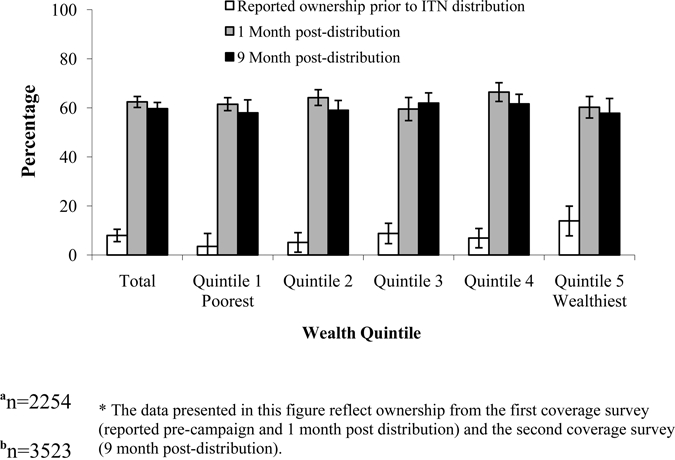
Percent of households owning an insectide-treated net by economic quintile beforea, one montha, and nine 9 months post-campaignb, Togo, 2005. Error bars represent 95% confidence intervals.
Bed net characteristics.
During the surveys, information was collected on 3500 nets in 2174 households. Of the 3500 nets, 3146 were ITNs. The majority of nets found (2917) were ITNs distributed during the December 2004 campaign. Nets reported as either “other” or unknown types were considered to be conventional nets. Of these nets, 36.3% had been treated or re-treated within the previous 12 months. Despite the free re-treatment campaign sponsored by the MOH in 2004 four months pre-survey, there was a difference in re-treatment rates by wealth quintile, with wealthier households more likely to have re-treated their conventional nets (P < 0.001). If a net was long-lasting, re-treatment history was not taken.
ITN use.
In the first survey, during the dry season, 36.2% of all households had an ITN hanging at the time of the survey (regional range = 27.8–72.7%). The proportion of persons hanging at least one ITN given they own at least one ITN, or hanging rate, was 57.9% (95% CI = 51.1–64.7%). Overall 43.5% of children les than five years of age were reported to have slept under an ITN the previous night. The percent of children who slept under an ITN the previous night was lower in the southern two regions (Lomé = 35.8% and Maritime = 30.9%) than the other four regions (Plateaux = 56.7%, Centrale = 72.9%, Kara = 49.7%, and Savanes = 70.9%).
At the time of the second coverage survey during the rainy season, 45.7% (95% CI = 42.9–48.5%) of all households had an ITN hanging (regional range = 26.0% for Lomé to 67.2% for Savanes) and a hanging rate of 76.6% (95% CI = 73.5–79.6%). However, only 52.9% (95% CI = 50.6–55.1%) of children less than five years of age were reported to have slept under an ITN the previous night. Of children less than five years of age residing in households that owned at least one ITN, 69.5% (95% CI = 67.2–71.8%) were reported to have slept under an ITN the previous night.
Use of ITNs varied by age with the youngest group.
Children less than 12 months of age (none of whom were individually eligible to receive an ITN from the campaign) had the lowest use at (49.3%) and children 24–35 months of age had the highest use (57.9%). Similar to the first dry season survey, the number of children who slept under an ITN the previous night was lower in the southern two regions (Lomé and Maritime) than the other four regions (Plateaux, Centrale, Kara, and Savanes). In addition, fewer children slept under an ITN the previous night in urban areas (36.3%; 95% CI = 29.7–42.9%) than in rural areas (55.7%; 95% CI = 53.5–58.0%) (Table 2).
Table 2.
Percentage of 3,523 children less than five years of age who slept under an ITN the previous night during the rainy season, Togo, 2004*
| Characteristic | Category | 9 Months post-campaign |
|---|---|---|
| Total | 52.9% (50.6–55.1%) | |
| Region | Lomé | 37.9% (30.5–45.3%) |
| Maritime | 35.9% (51.6–40.3%) | |
| Plateaux | 49.4% (45.1–53.8%) | |
| Centrale | 63.6% (55.6–71.7%) | |
| Kara | 66.7% (60.1–73.2%) | |
| Savanes | 80.9% (78.1–83.9%) | |
| Type | Urban | 36.3% (29.7–42.9%) |
| Rural | 55.7% (53.5–58.0%) |
ITN = insecticide-treated net. Values in parentheses are 95% confidence intervals.
Overall, of children eligible to have received an ITN at the time of the campaign (excluding children less than 18 months of age at the time of the rainy season survey because they were not directly targeted to receive an ITN from the campaign), 55.6% were reported to have slept under an ITN the previous night. This value includes children of campaign-eligible households that did not receive a net during the campaign.
Effect of household follow-up visits.
A total of 55.1% of households owning an ITN were visited at least once by a Red Cross Volunteer, a health worker, or a representative from an non-government organization after the campaign to discuss the use of bed nets and other health-related matters. Follow-up visits increased the likelihood of hanging nets in homes that owned them (80.4% versus 72.3%; P < 0.001), but no effect on whether children less than five years of age slept under an ITN the previous night (89.0% versus. 86.2%; P = 0.1265).
Discussion
The results of the surveys conducted one month and nine months, respectively, after the Togo National Integrated Child Health Campaign demonstrated that integrating ITN delivery into the vaccination campaign throughout the six regions of Togo rapidly achieved high levels of ITN ownership and equity, and that this was maintained nine months post-campaign.
The September 2004 pre-campaign survey established that in rural districts, net ownership was positively associated with higher wealth quintile, suggesting possible competition for limited funds to supply other basic needs.6 The Togo National Integrated Health Campaign appears to have been an effective strategy to achieve high, equitable ITN coverage reaching > 90% coverage for all eligible children. In a study by Noor and others, free mass distribution campaigns were found to achieve the highest coverage among the poorest children compared with heavily subsidized and commercially available nets.4 Moreover, a similar free distribution integrated campaign carried out in Niger, which used a voucher system, achieved 73.4% coverage compared with 90.8% coverage in Togo among children less than five years of age, suggesting that apart from the cost of nets, eliminating additional layers of complexity during distribution campaigns may contribute to greater success.12
The rate of use was significantly lower than the rate of possession, and use by children less than five years of age did not meet the 2000 RBM target set at 60%.1 Nevertheless, use by all households, including households that did not have an eligible child during the campaign and therefore did not receive a net at that time, increased from 43.5% (January) to 52.9% (September). Similarly, in all households, the proportion that hung an ITN the night before increased in the September survey compared with the January survey. During that same period, there was no significant change in the level of household ownership between the January and September surveys. Korenromp and others demonstrated that net use is markedly higher in the rainy season than in the dry season in surveys that reported on seasonal use patterns; the higher usage and hanging of ITNs in the September survey coincided with the high-transmission season towards the end of the rainy season.13 Furthermore, there was an increase in net use in children less than five years of age observed across all regions and wealth quintiles. This increase included children born after the campaign and those who were too young to receive a net during the campaign. Both children less than 18 months of age (at the time of the peak malaria season and second coverage survey) and pregnant women, despite not being targeted by the campaign, saw increases in ITN use. It is possible that these households had an eligible child at the time of the campaign that was more than five years of age by the time the September survey was conducted. In that case, it may appear that a household without a campaign eligible child received an ITN from the campaign. It should be noted that we did not directly measure this in these surveys.
High coverage with ITNs has been shown to reduce malaria morbidity and all-cause mortality in malaria-endemic areas.14,15 Togo Ministry of Health data, the September 2004 anemia survey, and the January 2005 coverage survey indicate that ITN coverage in Togo was low before the integrated campaign.6,16 Although we have shown that coverage was high after the campaign, use still failed to reach contemporary RBM goals, indicating than additional strategies are needed to achieve these use goals. Assuming that all areas received the same mass media messages before and after the campaign (although reach/access may vary), it should be noted that use differed somewhat on the basis of visits to households by community-based volunteers. A significant difference between ITN use rates between houses that received follow-up visits after the campaign and those that did not suggests that this may be a useful strategy to increase overall ITN use after a mass distribution campaign in some settings. Despite a number of free re-impregnation stations in the community to re-treat existing nets (set up by the Togo Ministry of Health with support from the World Health Organization), in September 2004, less than 10% of the nets had been treated with insecticide in the previous six months.6 This low rate of re-treatment highlights the need for long-lasting ITNs as a feasible, long-term malaria control tool.
Expanded Program on Immunization campaigns typically reach more than 90% of targeted children, and this is the first time that ITN distribution has been integrated with a vaccination campaign on a national scale. A cost-effectiveness study conducted by the London School of Hygiene and Tropical Medicine on the Togo National Integrated Health Campaign found that integrating ITN delivery into health campaigns is as cost-effective as other malaria intervention strategies when averted treatment costs are taken into consideration.17 Moreover, the study found that many costs were shared by the ITN and vaccination components of the campaign underlining the economic gains of merging health campaigns. Conversely, there are potential limitations of this type of campaign.
Vaccination campaigns can be disruptive to the routine delivery of health care services because of increased demand on health care workers to plan, organize, mobilize, and conduct the campaign, and impose an additional burden on limited logistic capabilities. Although it seems unlikely that the addition of ITNs to vaccination campaigns would cause significantly greater disruption than a vaccination campaign, further investigation of these potentially deleterious outcomes may be warranted. In addition, the target groups for vaccination campaigns may differ from those targeted for ITNs. In this survey the vaccination target group was children 9–59 months of age, whereas the ideal ITN target for a child-oriented distribution would have been all children less than five years of age. This finding may require additional planning and logistics to ensure the desired target groups are appropriately covered for ITN and vaccination delivery.
In conclusion, there have been considerable efforts using various methods to increase ITN ownership and use across Africa.17 The results of these surveys reinforce previous findings that integrating ITN distribution with measles campaigns is an effective way to rapidly increase ITN ownership and use, and represents an important route towards attaining the Abuja and RBM targets for ITN use in children.7,8 In addition, these findings demonstrated the potential capability of this strategy when scaled up to a national level and was the pioneering effort upon which several other countries (Niger, Mozambique, Kenya, Sierra Leone, Madagascar) built their campaigns. Integrated campaigns continue to present an important opportunity for reaching malaria control goals and merit continued large-scale implementation. Future campaigns should include efforts to maintain coverage for children less than nine months of age born since the campaign because these children are among the most vulnerable. Increasing household ownership of ITNs and efforts to promote increased use rates among vulnerable populations will provide Togo with an effective tool in their efforts to control malaria.
Acknowledgments
We thank the families for participating in this survey, the data collectors for working diligently in challenging conditions, the Canadian Red Cross for logistic support, and the Togolese Red Cross and the Togolese Bureau of Statistics for assistance.
Footnotes
Financial support: This work was supported by the Canadian International Development Agency, through the Canadian Red Cross.
Authors' addresses: Adam Wolkon, Jodi L. Vanden Eng, M. James Eliades, Julie Thwing, Allen W. Hightower, Laurence Slutsker, and William A. Hawley, Division of Parasitic Diseases, National Centre for Infectious Diseases, Centers for Disease Control and Prevention, Atlanta, GA. Dianne J. Terlouw, Child and Reproductive Health Group, Liverpool School of Tropical Medicine, Pembroke Place, Liverpool, United Kingdom. Kodjo Morgah, Vincent Takpa, Aboudou Dare, Yao K. Sodahlon, and Yao Doumanou, Togolese Ministry of Health, Lomé, Togo. Marcel Lama, World Health Organization, Africa Regional Office, Harare, Zimbabwe. Neeta Thawani, Canadian Red Cross, Ottawa, ON, Canada.
References
- 1.Roll Back Malaria Partnership The African Summit on Roll Back Malaria, Abuja, 25 April 2000. 2000. http://www.rbm.who.int/docs/abuja_declaration.pdf Available at. Accessed August 3, 2008.
- 2.Roll Back Malaria Partnership The Global Malaria Action Plan. 2008. http://www.rbm.who.int/gmap/gmap.pdf Available at. Accessed March 12, 2009.
- 3.Lengeler C. Insecticide-treated bednets and curtains for preventing malaria. Cochrane Database Syst Rev. 2000:CD000363. doi: 10.1002/14651858.CD000363. [DOI] [PubMed] [Google Scholar]
- 4.Noor AM, Amin AA, Akhwale WS, Snow RW. Increasing coverage and decreasing inequity in insecticide-treated bed net use among rural Kenyan children. PLoS Med. 2007;4:e255. doi: 10.1371/journal.pmed.0040255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization The World Health Report, Statistical Annex. 2004. http://www.who.int/whr/2004/annex/en/index.html Available at. Accessed August 3, 2008.
- 6.Eliades MJ, Wolkon A, Morgah K, Crawford SB, Dorkenoo A, Sodahlon Y, Hawley WA, Hightower AW, Kuile FO, Terlouw DJ. Burden of malaria at community level in children less than 5 years of age in Togo. Am J Trop Med Hyg. 2006;75:622–629. [PubMed] [Google Scholar]
- 7.Grabowsky M, Nobiya T, Ahun M, Donna R, Lengor M, Zimmerman D, Ladd H, Hoekstra E, Bello A, Baffoe-Wilmot A, Amofah G. Distributing insecticide-treated bednets during measles vaccination: a low-cost means of achieving high and equitable coverage. Bull World Health Organ. 2005;83:195–201. [PMC free article] [PubMed] [Google Scholar]
- 8.Grabowsky M, Farrell N, Hawley W, Chimumbwa J, Hoyer S, Wolkon A, Selanikio J. Integrating insecticide-treated bednets into a measles vaccination campaign achieves high, rapid and equitable coverage with direct and voucher-based methods. Trop Med Int Health. 2005;10:1151–1160. doi: 10.1111/j.1365-3156.2005.01502.x. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention Distribution of insecticide-treated bednets during an integrated nationwide immunization campaign–Togo, West Africa, December 2004. MMWR Morb Mortal Wkly Rep. 2005;54:994–996. [PubMed] [Google Scholar]
- 10.Vanden Eng JL, Wolkon A, Frolov AS, Terlouw DJ, Eliades MJ, Morgah K, Takpa V, Dare A, Sodahlon YK, Doumanou Y, Hawley WA, Hightower AW. Use of handheld computers with global positioning systems for probability sampling and data entry in household surveys. Am J Trop Med Hyg. 2007;77:393–399. [PubMed] [Google Scholar]
- 11.World Bank African Development Indicators 2000. 2000. http://go.worldbank.org/QKQMQQBO70 Available at. Accessed August 3, 2008.
- 12.Thwing J, Hochberg N, Vanden Eng J, Issifi S, Eliades MJ, Minkoulou E, Wolkon A, Gado H, Ibrahim O, Newman RD, Lama M. Insecticide-treated net ownership and usage in Niger after a nationwide integrated campaign. Trop Med Int Health. 2008;13:827–834. doi: 10.1111/j.1365-3156.2008.02070.x. [DOI] [PubMed] [Google Scholar]
- 13.Korenromp EL, Miller J, Cibulskis RE, Kabir Cham M, Alnwick D, Dye C. Monitoring mosquito net coverage for malaria control in Africa: possession vs. use by children under 5 years. Trop Med Int Health. 2003;8:693–703. doi: 10.1046/j.1365-3156.2003.01084.x. [DOI] [PubMed] [Google Scholar]
- 14.Phillips-Howard PA, Nahlen BL, Kolczak MS, Hightower AW, ter Kuile FO, Alaii JA, Gimnig JE, Arudo J, Vulule JM, Odhacha A, Kachur SP, Schoute E, Rosen DH, Sexton JD, Oloo AJ, Hawley WA. Efficacy of permethrin-treated bed nets in the prevention of mortality in young children in an area of high perennial malaria transmission in western Kenya. Am J Trop Med Hyg. 2003;68:23–29. [PubMed] [Google Scholar]
- 15.Phillips-Howard PA, ter Kuile FO, Nahlen BL, Alaii JA, Gimnig JE, Kolczak MS, Terlouw DJ, Kariuki SK, Shi YP, Kachur SP, Hightower AW, Vulule JM, Hawley WA. The efficacy of permethrin-treated bed nets on child mortality and morbidity in western Kenya II. Study design and methods. Am J Trop Med Hyg. 2003;68:10–15. [PubMed] [Google Scholar]
- 16.Programme National de Lutte contre le Paludisme (PNLP), Togolese Ministry of Health . Rapport: Collecte Dynamique des Donnees de Moridite et de Mortalite sure le Paludisme pour le Suivi et l'Evaluation de RRP au Togo. 2003. [Google Scholar]
- 17.Mueller DH, Wiseman V, Bakusa D, Morgah K, Dare A, Tchamdja P. Cost-effectiveness analysis of insecticide-treated net distribution as part of the Togo Integrated Child Health Campaign. Malar J. 2008;7:73. doi: 10.1186/1475-2875-7-73. [DOI] [PMC free article] [PubMed] [Google Scholar]


