Abstract
Edema, parasthesias, and paresis affected 10 residents of an Indian community in Roraima state; three died. Mining with mercury occurs locally; caxirí, a traditional alcoholic drink, is consumed daily. We conducted a 1:2 unmatched case-control study; a case was an Indian from Uiramutã county (population of 9,127) who presented ≥ 1 of lower extremity edema, paresthesias, paresis, or weakness. Controls were asymptomatic Indians randomly selected from the population. We identified 90 cases (prevalence of 1%) and 180 controls; all were enrolled. Among cases, 79% were male, and the median age was 31 years. Ethnicity was Macuxí, and 49% had income. Cases had lower extremity edema (85%), upper extremity paresthesias (84%), and lower extremity weakness and pain (78%). Risk factors were male sex (odds ratio [OR] = 6.8; P < 0.001), age 31–40 years (OR = 5.63; P < 0.001), and consumption of caxirí (OR = 2.7; P < 0.003). Mercury exposure was not a risk. Thiamine therapy produced complete rapid clinical recovery in all cases, confirming the diagnosis of beriberi. We recommend surveillance, thiamine supplementation, and nutritional intervention.
Introduction
Beriberi is a clinical syndrome caused by vitamin B1 (thiamine) deficiency that entails cardiovascular and neurological manifestations. Its presence has been reported for centuries in southeast Asia, Africa, and Latin America; in Brazil, it has been recognized since the mid-19th century.1 Outbreaks have been reported in recent years.2 Thiamine acts as a coenzyme in the metabolism of carbohydrates, proteins, and fats. Beriberi is associated with a thiamine-deficient diet, classically in populations dependent on polished rice.3 Thiamine is water-soluble, and natural reserves last up to 3 months. The recommended daily dose of thiamine is 0.2 mg/day for children < 6 months of age and 1.2 g/day for adults, the latter being obtainable from 100 g wheat or oat germ, 50 g of whole rice, 600 g of bovine liver, or 1,200 g of white rice.4 In thiamine-deficient persons, the risk of beriberi is augmented by intense physical effort, fever, infection, and alcohol consumption.5–7
The principal manifestations are cardiovascular and neurological. Cardiovascular manifestations include peripheral edema, increased heart rate, and increased cardiac output (wet beriberi); these can manifest in fulminant cardiac failure, lactic acidosis, and death from cardiac and vasodilatory shock. Neurological manifestations include peripheral neuropathy and parasthesias, weakness, loss of muscular strength, and decreased distal tendon reflexes (dry beriberi); these symptoms may be indistinguishable form mercury intoxication. Central nervous system involvement produces the Wernicke–Korsakoff Syndrome, which is characterized by disorientation, confusion, diplopia, ophthalmoplegia, and inability to form short-term memories.8 These syndromes can coexist in the same patient.
The Região das Serras (Mountain Region) of Roraima state in northern Brazil is a remote area of the Amazon Basin populated by Amerindian tribes and straddling the frontier with Guyana and Venezuela. The inhabitants are generally rural and poor, and they subsist on communal farming and livestock and fishing. Small-scale mining entailing the use of mercury has been practiced for decades. The local indigenous diet includes various alcohol-containing fermentation products of manioc and potatoes. In Brazil, medical care is provided to Amerindian peoples under a special system. Community healthcare workers provide immediate assistance; dedicated clinics may be present in regional townships. More complicated cases are transported to the Indian Referral Hospital (Casa de Saúde do Índio [CASAI]) at the state capital. CASAI exclusively treats members of Amerindian tribes residing in the state.
During a vaccination campaign in Amerindian communities of Roraima in 2008, seven patients with lower extremity edema and paralysis, abdominal pain, weakness, dyspnea, chest pain, difficulty walking, and tachycardia were identified in the township of Uiramutã (Figure 1); three deaths preceded by similar presentation were also noted. Uiramutã has an area of 8,066 km2 (two times the size of Rhode Island) and 9,127 inhabitants living in 92 indigenous communities. Local health authorities conducted a retrospective review of CASAI (the Indian Hospital at Boa Vista, the state capital of Roraima) medical records and patient referral logs for the period of January 2007 to July 2008 to identify additional patients with these findings. We conducted an investigation between June 9 and July 14, 2008, to establish the diagnosis, define the prevalence of disease in the indigenous population, and identify risk factors and measures of control and prevention.
Figure 1.
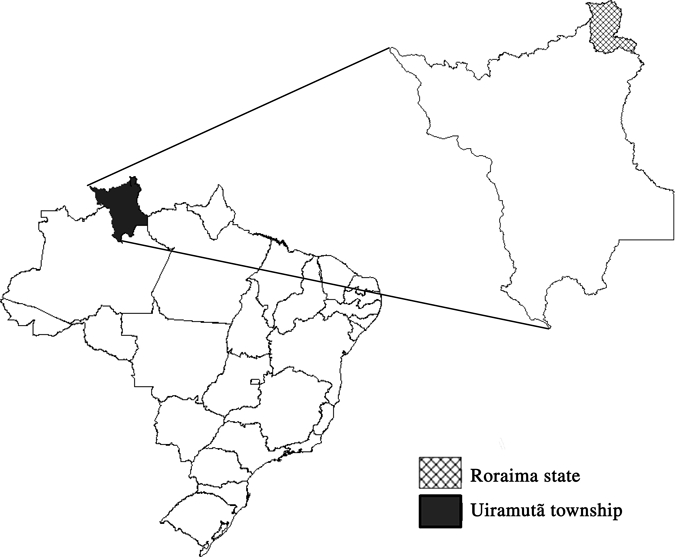
Map of Brazil highlighting the state of Roraima and within it, the municipality of Uiramutã.
Materials and Methods
Retrospective finding of patients of interest.
We conducted retrospective case finding among hospital records and referral logs for CASAI, the Indian Referral Hospital in Boa Vista, the capital of Roraima State, for the period 2007–2008. This is the only hospital to which patients from Uiramutã are referred. We defined a patient of interest as any person hospitalized with the following symptoms: edema and paralysis of the lower extremities or abdominal pain, weakness, dyspnea, thoracic pain, difficulty walking, or tachycardia. The findings of these patients of interest were used subsequently to develop a differential diagnosis and case definitions for the epidemiologic study.
Observation of treated patients.
Observation was documented by clinical staff treating the patients at the local hospital of Uiramutã in medical charts. The study team abstracted data from charts and interviewed the patients and treating physicians.
Case-control study.
We conducted a 1:1 non-matched case-control study in the township of Uiramutã. We defined a case as an Amerindian aged 16–70 years who was a resident of a community in Uiramutã and between January and June 2008, presented at least one of the symptoms (lower extremity edema, parasthesias, paresis, or weakness); persons with diabetes, hypertension, cardiomyopathy, neuropathy, and peripheral vascular disease were excluded. Cases were identified in Amerindian communities by the resident community Indian Community Health Agent. We defined a control as an Amerindian aged 16–70 years who was a resident of a community in Uiramutã and between January and June 2008, did not present any symptoms (lower extremity edema, parasthesias, paresis, or weakness) and did not have diabetes, hypertension, cardiomyopathy, neuropathy, or peripheral vascular disease. Controls were selected from a list of names of all persons residing in the Amerindian communities of Uiramutã in which cases were identified. Three hundred controls were randomly selected without replacement from the list. When a control could not be located, a repeat random selection was conducted from the list.
Ill persons were evaluated using a standard protocol. Persons meeting the case definition were treated with injectable or oral thiamine based on the evaluating clinician's judgment. Cases and controls responded to a standard questionnaire containing questions about demographics, food intake, and environmental exposures. The questionnaire named 46 foods and the frequency of their consumption. Blood samples were collected from all case patients and the first 50 controls enrolled.
Laboratory testing.
Whole blood and serum were collected from each tested subject for thiamine level (physiologically active direct thiamine diphosphate) determination by high performance liquid chromatograpghy (HPLC; H. Pardini Laboratory, Belo Horizonte, Minas Gerais, Brazil) and biochemical profile, liver transaminases, blood urea nitrogen (BUN), creatinine, and total proteins (Public Health Laboratory, Roraima, Brazil). Blood was collected for mercury level determination as well.
Environmental investigation.
The leader (Tuchauá) of each community visited was interviewed about the dietary habits and the environment of the community using a standardized questionnaire.
Data analysis.
Data were analyzed in EPI-INFO 2000 (CDC, Atlanta, GA USA). We calculated odds ratios (OR) and used the χ2 and Fisher's exact tests for categorical variables, and the Student t test and Kruskal–Wallis tests for continuous variables; α was 5%, and we calculated 95% confidence intervals (CI). Study power was 75% for OR = 2.
Results
Retrospective finding of patients of interest.
In the CASAI (Indian Referral Hospital) of Boa Vista, we reviewed 3,947 charts from 2007 and 2008, among which we identified 103 patients of interest. All were from 2008. Of these, 66 (64%) were male, median age was 41 years (range = 1–85 years), and patients were residents of 14 of 20 Amerindian communities in Uiramutã Municipality. The most frequent combinations of signs and symptoms were edema and myalgia in 25 (28%) patients, paresthesia and paresis in 20 (22%) patients, edema and paresthesia in 11 (12%) patients, edema and paresis 10 (11%) patients, and edema, fever, myalgia, and paresthesia in 9 (10%) patients. We developed case and control definitions for the epidemiology study using these findings.
Case-control study.
We identified 90 persons meeting the case definition residing in 20 communities in Uiramutã. Of these, 72 (79%) were males, the median age was 35 years, and 65 (71%) had 8 or fewer years of schooling. All case patients were of the Macuxi Amerindian ethnicity, and 45 (49%) reported having a family income. Their most common signs and symptoms were the following: lower extremity edema, parestheisa of upper extremities, weakness and pains in lower extremities, difficulty walking, and fatigue (Table 1). Fifty-five (62%) case patients reported walking long distances carrying burdens with a median weight of 30 kg (range = 10–70 kg). The median daily walk reported by 80 (89%) case patients was 2 hours (range = 0.5–17 hours), and the median number of hours spent in field work reported by 76 (84%) cases was 6 hours (range = 2–12 hours) per day.
Table 1.
Principal signs and symptoms of case patients in Amerindian communities of Uiramutã, state of Roraima, Brazil, June 2008
| Signs and symptoms | N | Percent |
|---|---|---|
| Lower extremity edema | 77 | 85 |
| Lower extremity parasthesias | 76 | 83 |
| Leg pain | 71 | 78 |
| Weakness | 71 | 78 |
| Difficulty walking | 69 | 76 |
| Fatigue | 67 | 74 |
| Difficulty running | 60 | 66 |
| Arthralgia | 49 | 54 |
| Upper extremity parasthesias | 42 | 46 |
Male sex was a risk factor for illness (OR = 6.8, 95% CI = 3.5–13.4, P ≤ 0,001) as was belonging to any age group above age 20 (Table 2). Of the 46 food exposures explored on the questionnaire, the most commonly consumed were damorida, a soup of pepper, beef, manioc leaves, and potato as well as manioc flour, beans, rice, and caxiri, a fermented manioc beverage (Table 3). The only foods associated significantly with illness were those prepared by fermentation of carbohydrate-rich tubers and containing alcohol. Weak caxiri, said by interviewees to have a lesser alcohol content, was consumed daily by all cases and controls. We used consumption of this alcoholic beverage as the reference value for calculating the association of other alcohol-containing fermented carbohydrate beverages with illness. These include weak pajuaru, strong pajuaru, a mixture of weak caxiri with weak pajuaru, and strong caxiri. Only consumption of strong caxiri was significantly associated with illness (OR = 2.7, P < 0.003) (Table 4).
Table 2.
Illness by age range in case patients and controls of Amerindian communities in Uiramutã, state of Roraima, Brazil, 2008
| Age range (years) | Cases n (%) | Controls n (%) | OR | 95% CI | P value |
|---|---|---|---|---|---|
| < 20 | 8 (9) | 56 (31) | Reference | – | – |
| 20–30 | 24 (28) | 41 (23) | 4.1 | 1.7–10.0 | 0.001 |
| 31–40 | 29 (33) | 36 (20) | 5.6 | 2.3–13.7 | < 0.001 |
| 41–50 | 14 (16) | 30 (17) | 3.3 | 1.2–8.7 | 0.014 |
| 51–60 | 9 (10) | 11 (6) | 5.7 | 1.8–18.1 | 0.001 |
| > 60 | 3 (3) | 6 (3) | 3.5 | 0.7–16.8 | 0.101 |
OR = odds ratio; CI = confidence interval.
Table 3.
Reported frequency of habitual consumption of specific foods, by meal time, among cases in Amerindian communities, Uiramutã, state of Roraima, Brazil, 2008
| Meal | Food | Persons consuming (n) | Percent |
|---|---|---|---|
| Breakfast | Damorida* | 77 | 89 |
| Manioc flour | 57 | 66 | |
| Caxiri† | 46 | 53 | |
| Lunch | Manioc flour | 66 | 77 |
| Beans | 63 | 73 | |
| Rice | 60 | 70 | |
| Damorida* | 57 | 66 | |
| Caxiri† | 52 | 60 | |
| Supper | Damorida* | 59 | 69 |
| Manioc flour | 57 | 67 | |
| Caxiri† | 49 | 58 |
Damorida is a soup containing pepper, beef, cassava plant leaves, and potato.
Caxiri is an alcohol-containing product of fermented cassava.
Table 4.
Univariate analysis of reported consumption of alcohol-containing fermented beverages among case patients and controls in Amerindian communities, Uiramutã, state of Roraima, Brazil, 2008
| Beverage | Cases n (%) | Controls n (%) | OR | 95% CI | P value |
|---|---|---|---|---|---|
| Weak caxiri* | |||||
| Yes | 76 (100) | 160 (100) | Reference | – | – |
| No | 0 | 0 | |||
| Pajuaru† | |||||
| Yes | 52 (75) | 108 (69) | 1.4 | 0.7–2.6 | 0.31 |
| No | 17 (25) | 49 (31) | |||
| Strong pajuaru‡ | |||||
| Yes | 42 (48) | 79 (43) | 1.2 | 0.7–2.1 | 0.43 |
| No | 45 (52) | 104 (57) | |||
| Caxiri and pajuaru | |||||
| Yes | 78 (90) | 162 (89) | 1.1 | 0.5–2.6 | 0.92 |
| No | 42 (48) | 71 (40) | |||
| Strong caxiri§ | |||||
| Yes | 62 (82) | 100 (63) | 2.7 | 1.4–5.2 | 0.003 |
| No | 14 (14) | 60 (37) | |||
OR = odds ratio; CI = confidence interval.
Weak caxiri is a beverage of manioc root fermented ≤ 2 days.
Pajuaru is a high-alcohol beverage of manioc root and other root vegetables fermented 2–7 days.
Strong pajuaru is a high-alcohol beverage of manioc root and other vegetables fermented ≥ 7 days.
Strong caxiri is a beverage of manioc root fermented > 2 days.
Of all occupational exposures analyzed, only working as an Indian Health Agent was significantly associated with illness (OR = 3.3, P < 0.006). Various exposures related to mining and mercury exposure were examined, and none were associated with illness (Table 5).
Table 5.
Univariate analysis of types of employment and occupational exposures among case patients and controls in Amerindian communities of Uiramutã, state of Roraima, Brazil, 2008
| Exposure | Cases n (%) | Controls n (%) | OR | 95% CI | P value |
|---|---|---|---|---|---|
| Type of occupation | |||||
| Community health agent | 13 (18) | 10 (7) | 3.3 | 1.3–7.8 | 0.006 |
| Field work | 76 (87) | 164 (90) | 0.8 | 0.4–1.8 | 0.58 |
| Cowboy | 5 (7) | 4 (3) | 3.0 | 0.8–11.4 | 0.09 |
| Public servant | 4 (6) | 9 (6) | 1.0 | 0.3–3.4 | 0.97 |
| Occupational exposures | |||||
| Carries heavy loads | 56 (70) | 114 (70) | 1.0 | 0.6–1.8 | 1.0 |
| Does field work and carries heavy loads | 48 (55) | 110 (60) | 0.8 | 0.5–1.4 | 0.4 |
| Does mining work currently | 10 (12) | 20 (11) | 1.0 | 0.5–2.5 | 0.8 |
| Uses mercury in mining currently | 3 (33) | 7 (32) | 1.1 | 0.2–5.6 | 0.9 |
| Did mining work in the past | 36 (49) | 68 (41) | 1.3 | 0.8–2.3 | 0.3 |
| Used mercury in mining work in the past | 14 (39) | 25 (35) | 1.2 | 0.5–2.7 | 0.7 |
Laboratory testing.
Blood and serum samples were obtained from 90 cases and 46 controls; thiamine level was determined in 53 case patients and 35 controls, after which funding for laboratory tests was exhausted. Among case patients and controls, 90% had thiamine levels within the normal range (28.0–85.0 mcg/L); the median thiamine level among case patients was 31 mcg/L (range = 10–77 mcg/L), and among controls, it was 34 mcg/L (range = 15–67 mcg/L; P > 0.05). Blood chemistries from case patients and controls did not differ markedly (Table 6). Regretfully, all specimens collected for mercury testing were lost during shipment to the out-of-state reference laboratory.
Table 6.
Biochemical test results in serum of case patients and controls in Amerindian communities of Uiramutã, state of Roraima, Brazil, 2008
| Test | Reference range | Result outside normal range | Result within normal range | ||
|---|---|---|---|---|---|
| Cases n (%) | Controls n (%) | Cases n (%) | Controls n (%) | ||
| Albumin | 3.5–5.5 mg | 19 (24) | 24 (46) | 60 (76) | 28 (54) |
| Urea | 20–40 mg | 42 (53) | 25 (48) | 37 (47) | 27 (52) |
| Creatinine | 0.4–1.4 mg | 9 (11) | 3 (6) | 73 (89) | 48 (94) |
| Total proteins | 6.5–8.3 mg | 37 (53) | 18 (44) | 33 (47) | 23 (56) |
| ALT | 2–17 IU | 38 (49) | 26 (51) | 39 (51) | 25 (49) |
| AST | 2–15 IU | 45 (58) | 34 (67) | 32 (42) | 17 (33) |
ALT = alanine aminotransferase; AST = aspartate aminotransferase; IU = international units.
Environmental investigation.
The 20 Tuchauás (community leaders) provided the following information about their communities. Eighteen (90%) communities had rivers as the principle source of drinking water; of these, 16 (80%) treated their water, and 14 (68%) of those used chlorination to do so. In all 20 communities, farming was collective, and all communities planted manioc, corn, and potatoes. Sugar cane was planted in 18 (92%) communities, and beans were planted in 3 (14%) communities. Livestock was collectively owned in all communities. All communities had cattle, poultry, and swine, and 19 (95%) communities had goats. Seventeen (84%) communities were located < 200 m from a mining site, and of these, 13 (67%) were located upriver from the mining operation.
Clinical description.
The following two cases are illustrative of the clinical presentation and therapeutic response of the patients evaluated and treated during this investigation.
Patient 1.
The 51-year-old male weighed 80.2 kg on the day of admission. Symptoms included weakness, lethargy, light-headedness, diminished vision, paresthesias, loss of appetite for the preceding 13 days, and band-like pain below the costal margins. On examination, the patient was noted to have jugular venous distention while upright, anasarca, tender hepatomegaly, loud heart sounds, S3 gallop, nystagmus, paresis of upper and lower extremities, gait disturbance, and difficulty maintaining erect posture. On the day of presentation, daily administration of thiazide 25 mg orally was begun, and a single dose of intravenous B1 complex was administered, which was followed immediately by a visible reduction in edema. At 24 hours after presentation, intramuscular administration of thiamine 100 mg every 24 hours was begun. Within minutes of the first intravenous thiamine dose, the patient reported substantial reduction of paresthesias, and paresis decreased resolved partially. On day 2 after initiation of treatment, edema was notably decreased, and cardiac rate and rhythm were normal. On day 3, moderate hypertension was noted, and antihypertensive therapy was initiated. On day 5, jugular venous distension resolved; thiamine supplementation was changed to 300 mg orally per day. On day 10, the patient's weight was 74.0 kg, and he manifested residual lower extremity edema and paresis. He was discharged on day 15 on oral thiamine, and he weighed 71 kg.
Patient 2.
The 37-year-old male weighed 80.2 kg on the day of admission. He complained of weakness, lethargy, light-headedness, diminished vision, loss of appetite for 9 days before presentation, and band-like pain in the subcostal region for 1 day. On examination, the patient had paresthesias and paresis of the upper and lower extremities, difficulty ambulating and maintaining upright posture, and diminished motor ability in the lower extremities. He had slight jugular venous distention, edema of the face and upper and lower extremities, ascites, and loud heart sounds with an S3 gallop. Treatment with thiazide, 25 mg orally daily, was begun, and the patient received a single dose of intravenous vitamin B complex, which was followed by reduction of edema. Twenty-four hours after admission, 100-mg thiamine intramuscular injections every 24 hours were initiated. Within hours of the first intramuscular thiamine dose, the patient reported improvement of prasthesia and paresis; 48 hours later, edema was markedly reduced, and cardiac findings were resolved. At 72 hours, the patient had mild persistent lower extremity paresis only. Hypertension was noted on day 5 of admission, and anti-hypertensive treatment was begun. On the same day, thiamine supplementation was switched to 300 mg thiamine orally daily. At 30 days, the patient was ambulating normally, with trace lower extremity edema and residual distal lower extremity paresis.
Discussion
An outbreak of beriberi occurred in men aged 20–60 years residing in 20 Amerindian communities in the municipality of Uiramutã in the state of Roraima beginning in January 2008. The diagnosis was based on clinical presentation and the dramatic therapeutic response to thiamine supplementation in all cases.3,6–8 Mercury exposure during mining activities was reported in the affected communities; although we were not able to test patient specimens for mercury, we discarded this diagnosis after observing the rapid resolution of clinical symptoms with thiamine supplementation. We also note that the epidemiologic study showed no association between illness and mining in general and mercury exposure specifically.
Thiamine levels in blood samples from cases and controls were within normal limits, and levels did not differ significantly between the groups. These findings are not necessarily incompatible with beriberi for several reasons. First, the laboratory's normal reference range was validated in urban Brazilian populations that are quite different from the rural Amerindian population in which the disease occurred. Second, the test in question, separation by HPLC from direct whole blood, reflects present thiamine levels only and can be affected by dietary intake within hours of sample collection; a normal result does not exclude chronic deficiency in the preceding weeks or months. Third, the thiamine levels in case patients and controls were both at the lowest end of the normal range, indicating that the population as a whole is at risk for beriberi because of dietary deficiencies and added thiamine requirements known to be caused by physical effort, high carbohydrate consumption, and alcohol consumption; these factors have been repeatedly associated with beriberi.9–11 Not surprisingly, the epidemiologic study showed an association between illness and consumption of strong caxiri, one of several home-fermented, alcohol-containing beverages frequently consumed by this population. The only other risk factor significantly associated with illness was being an Indian Health Agent, which we interpret as a marker for protracted physical exertion, because these health agents typically walk many hours daily over difficult terrain while making their rounds visiting households in different communities. The findings, in toto, suggest that this rural, agricultural Amerindian population experiences beriberi because of chronic low dietary thiamine intake that is exacerbated by known causes of increased thiamine requirements, including alcohol consumption, high carbohydrate intake, and physical effort. We do not know why cases were first noted in 2008. This may reflect some change in the population's thiamine intake or other risk factors or simply, improved detection.
Limitations of our study include possible recall bias in response to questionnaires and information bias in data provided by relatives of case patients. Laboratory tests were validated in non-Amerindian populations, and the accuracy of their range of normalcy in the Amerindian population that we studied is unknown. We were unable to test all available samples because of cost constraints, and we did not test for mercury intoxication.
In the short term, intensive surveillance of the affected population for beriberi with prompt reporting, medical evaluation, and treatment of cases is needed, along with thiamine supplementation of the population. Thiamine supplementation is safe, cheap, and readily available in Brazil, and it can be distributed to the population through the existing infrastructure of community health agents and clinics.12 Effective education of the population is necessary for these interventions to be successful. Standardized clinical evaluation, treatment, and follow-up protocols are needed to optimize care for patients in this remote region. Improved shipment protocols are needed so that specimens, collected with considerable effort in remote locations, arrive promptly and safely at the designated laboratories. In the longer term, a thorough nutritional assessment of this remote Amerindian population's diet is required, and interventions will need to be devised that will allow all individuals to consume an adequate, nutritious diet that is sustainable and compatible with local traditions and preferences.
Acknowledgments
Acknowledgments: Support for this manuscript was provided by the Centers for Disease Control and Prevention, Center for Global Health, through TEPHINET, a program of the Task Force for Global Health, Inc.
Footnotes
Authors' addresses: Matheus P. Cerroni, Jean C. S. Barrado, and Aglaer A. Nobrega, Field Epidemiology Training Program, Secretariat of Health Surveillance, Ministry of Health, Brasilia, Distrito Federal, Brazil, E-mails: mtcerroni@gmail.com, jean.barrado@gmail.com, and aglaer.nobrega@saude.gov.br. Alysson B. M. Lins, Secretaria Estadual de Saúde de Roraima, Boa Vista, RR, Brazil, E-mail: alyssonlins@hotmail.com. Iolanda P. da Silva, Conselho Indígena do Estado de Roraima, Boa Vista, Roraima, Brasil, E-mail: mtcerroni@gmail.com. Robson R. Mangueira, Fundação Nacional de Saúde do Estado de Roraima, Ministério da Saúde, Boa Vista, Roraima, Brasil, E-mail: robmd34@hotmail.com. Rômulo H. da Cruz, Fundação Nacional de Saúde do Brasil, Ministério da Saúde, Brasília, Distrito Federal, Brasil, E-mail: Romulo.rhc@gmail.com. Sandra M. F. Mendes, Unidade Regional de Saúde de Imperatriz, Maranhão, Brasil, E-mail: mendesmesquita@gmail.com. Jeremy Sobel, Center for Global Health, Centers for Disease Control and Prevention, Atlanta, GA, E-mail: jsobel@cdc.gov.
References
- 1.da Silva Lima JF. Contribuições para a história de uma molestia que reina atualmente na Bahia, sob a forma epidêmica e caracterizada por paralisia, edema e fraqueza geral. Gazeta Medica da Bahia. 1866;1:110–113. [Google Scholar]
- 2.Lima HC, Porto EA, Marins JR, Alves RM, Machado RR, Braga KN, de Paiva FB, Carmo GM, Silva e Santelli AC, Sobel J. Outbreak of beriberi in the state of Maranhão, Brazil: revisiting the mycotoxin aetiologic hypothesis. Trop Doct. 2010;40:95–97. doi: 10.1258/td.2009.090439. [DOI] [PubMed] [Google Scholar]
- 3.Tanphaichitr V. In: Modern Nutrition in Health and Disease. 9th ed. Shils M, Shike M, Olso J, Ross AC, editors. Baltimore, MD: Williams & Wilkins; 1998. pp. 381–389. (Thiamin). [Google Scholar]
- 4.World Health Organization . Handbook on Human Nutritional Requirements. WHO Monograph Series No. 61. Geneva, Switzerland: World Health Organization; 1974. [PubMed] [Google Scholar]
- 5.World Health Organization . Nutrition in Preventive Medicine. The Major Deficiency Syndromes, Epidemiology and Approaches to Control. WHO Monograph Series No. 62. Geneva, Switzerland: World Health Organization; 1976. pp. 136–145. (Beriberi). [Google Scholar]
- 6.Takahashi K. Thiamine deficiency neuropathy. Int J Neurol. 1981;15:245–253. [PubMed] [Google Scholar]
- 7.Davis RE, Icke GC. Clinical chemistry of thiamin. Adv Clin Chem. 1983;23:93–140. doi: 10.1016/s0065-2423(08)60399-6. [DOI] [PubMed] [Google Scholar]
- 8.Kril JJ. Nerupathology of thiamine deficiency disorders. Metab Brain Dis. 1996;11:9–17. doi: 10.1007/BF02080928. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization . Energy and Protein Requirements: Report of a Joint FAO/WHO/UNU Expert Consultation. WHO Technical Report Series No. 724. Geneva, Switzerland: World Health Organization; 1985. [PubMed] [Google Scholar]
- 10.Mcardle WD, Katch FI, Katch VL. Fisiologia do Exercício, Energia e Desempenho Humano. 5th ed. Rio de Janeiro, Brazil; Guanabara Koogan: 2003. [Google Scholar]
- 11.Macias-Matos C, Rodriguez-Ojea A, Chi N, Jimenez S, Zulueta D, Bates CJ. Biochemical evidence of thiamine depletion during the Cuban neuropathy epidemic, 1992–1993. Am J Clin Nutr. 1996;64:347–353. doi: 10.1093/ajcn/64.3.347. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization . Thiamine Deficiency and Its Prevention and Control in Major Emergences. Geneva, Switzerland: World Health Organization; 1999. [Google Scholar]


