Abstract
Since February 2002, the Drug Resources Enhancement against AIDS and Malnutrition Program has provided highly active antiretroviral therapy (HAART) and immunologic and virologic monitoring free of charge. We conducted a cohort study of persons infected with human immunodeficiency virus in Mozambique. Only persons treated with HAART with available CD4 cell counts at baseline and ≥ 1 CD4 cell count after HAART were included. Survival analysis was applied to evaluate the prognostic value of CD4 cell counts measured at three months. Possible confounders were considered. A total of 753 persons who started HAART included; 59% were females. Median age was 34 years (range = 16–67 years), and the median CD4 cell count at baseline was 172 cells/mm3 (interquartile range = 87–261 cells/mm3, range = 0–1,322 cells/mm3). Overall, 105 persons (14%) died. Of these persons 54 (51%) developed AIDS before they died; 25 (3%) died during the first three months. After three months of therapy, the individual median CD4 cell count change from the baseline value was +101 cells/mm3 (interquartile range = +27 to +187 cells/mm3, range = –723 to +310 cells/mm3). A median CD4 increment of 100 cells/mm3 in three months was associated with a mortality reduction of 50% compared with an increase of < 50 cells (relative hazard of death adjusted for baseline CD4 cell count = 0.54, 95% confidence interval = 0.30–0.95). A good initial response to HAART was associated with a significant reduction of mortality. This finding supports the effectiveness of HAART in resource-poor settings.
Introduction
Sub-Saharan Africa is region most affected by morbidity and mortality from infection with human immunodeficiency virus (HIV) and has approximately two-thirds of the world's HIV-infected persons.1 Although the need is great, access to antiretroviral highly active antiretroviral therapy (HAART) treatment in most countries in this region and in other poor-resource regions remains limited. However, great progress has been made in recent years. Up to now, almost 30% of persons estimated to be in need of treatment have been provided antiretroviral drugs.2 Expanded access to antiretroviral drugs in this setting needs appropriate evaluation of the effectiveness of treatment programs.
As previously reported, early pessimism concerning effective delivery of HAART on a large scale has largely proven unfounded,3 and high levels of treatment compliance and virologic suppression have been achieved in hospital-based and community-based programs.4–6 Moreover, meta-analyses of treatment cohorts have shown similar results for viral load suppression and CD4 cell count recovery among patients treated in high-income and resource-poor settings.7,8 However, early mortality after initiation of HAART was several-fold higher in resource-poor settings than in high-income settings.7
Low baseline CD4 cell count, symptomatic disease (World Health Organization Stages 3 and 4), and low body mass index (BMI) have been reported to be independent risk factors of early mortality.3 However, although early mortality (as measured four months after treatment initiation) was associated with patient characteristics at baseline, later mortality was only associated with the updated absolute CD4 cell counts at four months and with failure of viral load suppression,9 which suggested that the response to HAART is the key long-term determinant of mortality among HIV-infected patients in Africa.10
In this study, we analyzed the CD4 cell count decreases over time after initiation of treatment among HIV-infected persons in Mozambique and explored the role of early response to treatment (i.e., CD4 cell count decrease and viral load suppression) on longer-term mortality, taking into account possible confounders.
Methods
Selection of participants.
This study involved HIV-1-positive persons recruited during February 2002–February 2003 as part of a large prospective cohort in The Drug Resource Enhancement against AIDS and Malnutrition (DREAM) program. A description of the DREAM program structure and laboratory diagnostic methods has been reported.11,12 Briefly, DREAM is a multiregional health program that provides a free package of care, consisting of education and social support, and voluntary counseling and HIV testing Participants were from either urban (i.e., Maputo and Beira) or rural-urban areas (Machava) of Mozambique. HAART and laboratory diagnostics, including viral load and CD4 cell counts, have been provided since February 2002. In Mozambique, DREAM monitors and provides assistance and care to more than 43,000 HIV-infected persons, of whom 24,000 received or are receiving HAART.
HIV-positive persons who attended one of the clinical centers of the DREAM project and never received antiretroviral therapy were included in the study. Since the time of study initiation (i.e., HAART administration in February 2002), 1,968 persons were enrolled. Most of them (1,344, 68%) had begun receiving HAART, and the remaining 624 (32%) did not start HAART because they did not fulfill the criteria of the guidelines for initiation of treatment11 (i.e., CD4 cell count < 200 cells/mm3 and/or clinical stage 3–4, or a CD4 cell count < 350 cells/mm3 and a viral load > 55,000 copies/mL). Furthermore, only persons with CD4 cell counts for the six months before the date of HAART initiation (i.e., baseline CD4 cell count) and with ≥ 1 CD4 cell count in the first three months after HAART inception were included in this study. Most persons who did not start HAART were females (64% versus 36% males) and maintained relatively high CD4 cell counts without starting antiretroviral therapy. Overall, they showed a median CD4 cell counts of 600 cells/mm3 after three years and 500 cells/mm3 after five years since the date of recruitment.
Treatment and monitoring.
HAART was defined as fixed-combination nevirapine-based regimens (stavudine/azidothymidine, 2′,3′-dideoxy-3′-thiacytidine, nevirapine). Alanine aminotransferase, aspartate aminotransferase, and hemoglobin levels and clinical conditions were monitored weekly during the first month of HAART. CD4 cell counts were measured every three months and the viral load was measured every six months.
Statistical analysis.
Statistical analyses included summaries of baseline characteristics of the study population and CD4+ cell counts (median, interquartile ranges [IQRs], ranges for continuous variables, and percentages for categorical variables). To plot CD4 cell count trends, the locally weighted scatterplot smoothing method was used13 and relative fitted curves were presented.
To estimate immunologic response to HAART, median increments of CD4 cell counts from baseline (δ) were considered. Survival analysis was applied and considered increments of CD4 cell counts from baseline as the main variable of interest. Survival was estimated as time from initiation of HAART to time of death; follow-up was censored at the last visit before December 31, 2007. Analyses were repeated and censored persons who were lost to follow-up at the time when they were last known to be alive (usually the date of leaving the center mainly for dropout or transfer.) Univariable and multiple Cox models were applied to take into account possible confounders: CD4 cell count and HIV-1 load at baseline (within six months before starting HAART), hemoglobin level, BMI, age, and sex.
Results
The study population included 753 HIV-positive persons fulfilling the inclusion criteria (Table 1). Median age at start of HAART of 34 years, and 59% of the participants were female. Median BMI was 20.7, and median hemoglobin level was 10.5 mg/dL. Median CD4+ cell count at baseline was < 200 cells/mm3 (172 cells/mm3), and the median log10 HIV-1 load was 4.8 (i.e., 63,096 copies/mL).
Table 1.
Characteristics of 753 study participants at start of highly active antiretroviral therapy, Mozambique*
| Characteristic | Value |
|---|---|
| Sex, no. (%) | |
| Female | 441 (59) |
| Male | 312 (41) |
| Age, years | |
| Median | 34 |
| IQR, range | 28–41, 16–47 |
| Body mass index | |
| Median | 20.7 |
| IQR, range | 18.6–23.3, 10.2–38.8 |
| Hemoglobin | |
| Median | 10.50 |
| IQR, range | 9.0–11.9, 3.8–13.4 |
| CD4 cell count/mm3 | |
| Median | 172 |
| IQR, range | 87–261, 1–367 |
| HIV-1 viral load, copies/mL | |
| Median | 4.8 |
| IQR, range | 4.2–5.2, 1.1–5.7 |
IQR = interquartile range; HIV-1 = human immunodeficiency virus 1.
Persons were followed-up for a median of 3 years (IQR = 1–4 years, range = 0.1–5 years); 71 (9%) persons moved and 50 (7%) dropped out. Acquired immunodeficiency syndrome developed in 142 (19%) patients; 105 patients (14% of the study population) died. Of these patients, 25 (3% of the population) died during the first 3 months of follow-up, 41 (5%) died between 4 and 12 months of follow-up, and 39 (5%) died after 12 months and up to 5 years after follow-up. Furthermore, 51% of the deaths fulfilled the criteria for diagnosis of acquired immunodeficiency syndrome.
Trends of CD4 cell counts after HAART.
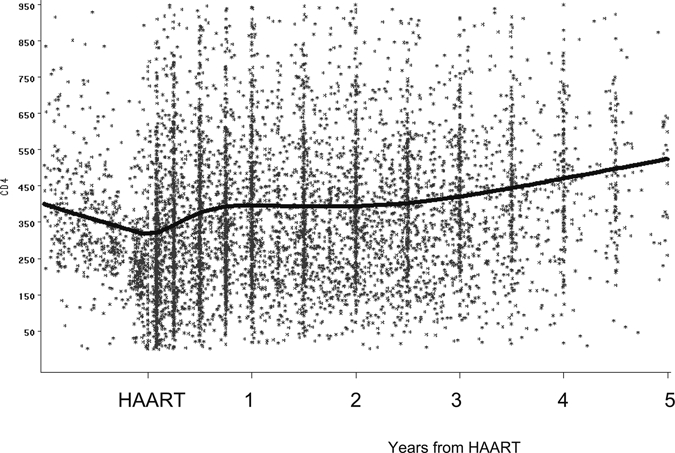
Trends of CD4 cell counts from 1 year before HAART up to 5 years after starting HAART are shown in Figure 1, which highlights a clear increase in CD4+ cell counts over time. Descriptive statistics of increments of CD4 cell counts after three months from baseline are shown in Table 2. A median increase of 101 CD4 cells and a median decrease in log10 viral load of 2.6 was estimated after three months. A total of 85% of those who started HAART reached an undetectable viral load by three months.
Figure 1.
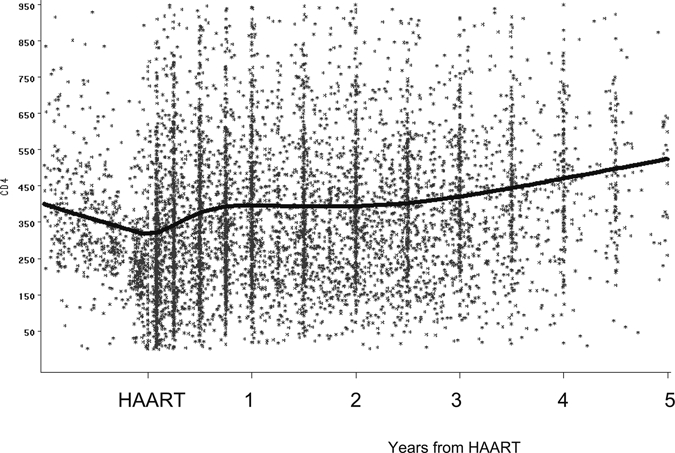
Locally weighted scatterplot smoothing curve describing CD4 cell count trends six months before (CD4 cell count baseline) and after start of highly active antiretroviral therapy for one year, Mozambique.
Table 2.
Immunologic and virologic response and mortality after three months of HAART, Mozambique*
| Characteristic | Median (*) | IQR | Range |
|---|---|---|---|
| Changes of CD4 cell counts/mm3 relative to baseline | +101 | (+27 to 187) | (–723 to +310) |
| Log10 HIV-1 viral load† relative to baseline‡ | −2.6 | (–3.5 to −1.26) | (–5.7 to +3.8) |
| No. (%) patients with HIV-1 viral load < 400 copies/mL for those available | 179 (90) | ||
| No. (% of the study population) of deaths | p months | Death rate × 1,000 p months | |
| Start of HAART through 3 months | 25 (3) | 2,225 | 11.2 |
| 4–12 months | 41 (5) | 6,002 | 6.5 |
| 13–60 months | 39 (5) | 23,095 | 1.7 |
HAART = highly active antiretroviral therapy; HIV-1 = human immunodeficiency virus 1.
For most persons, only 1 value was available after 3 months; the mean or median was considered for those with > 2 values available.
After 3 months data were available for 200 persons.
Effect of response to HAART and survival.
Curves showing progression to death according to the three-month CD4 cell count increments after HAART relative to baseline are shown in Figure 2. Increments of ≥ 101 cells predicted less progression to death compared with increments between 50 and 100 or < 50 (P = 0.071, by log-rank test).
Figure 2.
Survival curves according to CD4 cell count increments from baseline after at least three months of highly active antiretroviral therapy, Mozambique.
Univariable and multiple Cox models are shown in Table 3. A univariable Cox model showed that increments of CD4 cell counts from baseline (δ) after three months of HAART were associated with longer survival in five years of follow-up. Significant improvement in δ was observed when δ was considered as a categorical and continuous variable. When δ was used as a continuous variable, relative hazard [RH] of death × increments of 100 was 0.84 (95% confidence interval [CI] = 0.72–0.99). When δ was used as a categorical variable, significant reduction of mortality (approximately 50%) was observed for increments of at least 100 cells, and no effect on survival was observed for persons with low δ values (50–100 cells) when compared with increments of ≤ 49 cells. Results were confirmed in the multiple Cox model after considering variables significantly associated with survival (CD4 cell count and viral load at baseline, hemoglobin level , BMI, and sex) or censoring survival times of persons when they were last known to be alive (i.e., those lost to follow-up). The magnitude of estimates was confirmed for a subgroup with an HIV load < 400 after three months of HAART and adjusting for baseline HIV load, age, sex, and BMI, even if statistical significance was not obtained.
Table 3.
Crude and adjusted RH after three months of HAART according to immunologic response, Mozambique*
| Characteristic | Crude RH | 95% CI | Adjusted† RH | 95% CI |
|---|---|---|---|---|
| Median changes of CD4 cell count from baseline | ||||
| Reference δ ≤ 50 | 1.00 | – | 1.00 | – |
| 50 < δ ≤ 100 | 0.95 | 0.53–1.72 | 1.15 | 0.61–2.17 |
| δ > 100 | 0.57 | 0.35–0.94 | 0.53 | 0.30–0.96 |
| Median changes of CD4 cell count from baseline (δ continuous) | ||||
| × increments of 100 cells | 0.84 | 0.72–0.99 | – | – |
| CD4 cell count baseline × (–100 cells) | 0.68 | 0.55–0.83 | 0.85 | 0.70–1.00 |
| HIV-1 load at baseline × (1 log10) | 1.29 | 1.00–1.69 | 1.20 | 0.95–1.05 |
| Hemoglobin < 10.5 vs. ≥ 10.5 mg/dL | 3.01 | 1.83–4.97 | 2.34 | 1.31–4.16 |
| Body mass index | ||||
| < 20 vs. ≥ 20 | 1.95 | 1.26–3.02 | 1.61 | 0.96–2.73 |
| Sex | ||||
| Males vs. females | 1.49 | 0.96–2.31 | 1.81 | 1.08–3.02 |
| Age at baseline × 1 year | 0.99 | 0.97–1.02 | – | – |
RH = relative hazard; HAART = highly active antiretroviral therapy; CI = confidence interval; HIV-1 = human immunodeficiency virus 1.
Adjusted for variables with crude RH and P < 0.20 and considering δ as dichotomous.
We performed an additional analysis that considered CD4 cell counts at the start of HAART (baseline CD4 cell count ≥ 200 cells/mm3 versus CD4 cell counts < 200 cells/mm3) as a covariate of interest among persons with an increment of at least 100 cells/mm3 after three months of HAART (366 persons). We observed a mortality reduction of 70% for those who started HAART with CD4 cell counts > 200 cells (RH = 0.32, 95% CI = 0.12–0.83). This result was confirmed by using the CD4 cell count at baseline as a continuous covariate (reduction of mortality of approximately 50% for increments of 100 cells/mm3 at baseline (RH = 0.56, 95% CI = 0.38–0.82) and possible confounders such as age, sex, BMI, and HIV load at baseline.
Discussion
We evaluated the clinical and immunologic response to HAART in a cohort of HIV-infected persons from Mozambique. Mortality rates were relatively high in the first three months of treatment (approximately 3%), with an overall mortality rate of 14% by five years after treatment initiation.
The 12-month survival proportion in 18 studies of HIV-infected patients from Africa ranged from 0.74 to 0.92, with the greatest burden of mortality occurring during the initial months of HAART.14 Mortality rates in the second year of HAART were much lower than those in the first year. This finding is consistent with results of longitudinal studies conducted in South Africa, which showed mortality rates of 19.1 deaths/100 person-years in the first four months, which decreased to 2.9 after 4 months and 1.3 after 1 year.9,10 Another study conducted in Senegal showed a similar trend, but substantial mortality was observed during 12–24 months of follow-up, with mortality rates of 12.5, 6.6, and 4.5 deaths/100 person-years in the first, second, and third year of treatment, respectively.15 Because higher mortality rates are likely to be explained by lower rates of virologic suppression and associated poor immunologic recovery, it is of paramount importance to investigate CD4+ cell count trends and the role of decreases in CD4 cell counts in predicting survival after HAART initiation. This necessity is also a key point in creating mathematical models that predict epidemic patterns.16
Our study also aimed to identify determinants of outcome. Median change in CD4+ cell counts three months after starting HAART was associated with survival. Participants with an increase of > 100 cells were 50% less likely to die than those who had an increase of < 50 cells.
Early immunologic response was observed, with a median increase of approximately 100 CD4+ cells three months after starting HAART. These findings suggest that response to treatment in our cohort was at least as good as that observed in a European study, in which the median increase in CD4+ cell counts from baseline to six months after HAART initiation was 90 cells/mm3.17
Among possible confounders included in the model, CD4 cell count at the start of HAART, hemoglobin level, BMI, and sex were also associated with the outcome. The HIV viral load was marginally associated after adjusting for the other variables and sex. Furthermore, we confirmed in our study cohort the importance of baseline CD4 cell counts as a prognostic marker of survival. We observed that the higher the CD4 cell count at baseline, the higher the reduction in mortality rates, again confirming the results of the European study.17
In conclusion, our findings suggest that survival of HIV-infected persons treated with antiretroviral drugs in our study cohort was similar to that of European persons. Initial CD4 cell count and early response to treatment measured by an increase of CD4 cells in the first three months were predictors of longer survival. These data indicate that appropriate use of HAART in Africa may be as effective as that in industrialized countries and that CD4 cell count is a good indicator of response to treatment in difficult settings.
Footnotes
Authors' addresses: Leonardo Palombi, Paola Scarcella, Sandro Mancinelli, and Ersilia Buonomo, Department of Public Health and Cellular Biology, University Tor Vergata, Rome, Italy. Maria Dorrucci and Giovanni Rezza, Department of Infectious, Parasitic, and Immunomediated Diseases, Istituto Superiore di Sanità, Rome, Italy. Ines Zimba, Drug Resources Enhancement against AIDS and Malnutrition Program Coordination, Maputo, Mozambique. Giovanni Guidotti, Department of Therapeutic Research and Medicines Evaluation, Istituto Superiore di Sanità, Rome, Italy. Maria C. Marazzi, Training Unit, University Libera Università Maria Ss. Assunta, Rome, Italy.
References
- 1.UNAIDS/WHO AIDS Epidemic Update. 2008. http://data.unaids.org/pub/GlobalReport/2008/jc1510_2008_global_report_pp29_62_en.pdf Available at.
- 2.World Health Organization . Towards Universal Access: Scaling Up Priority HIV/AIDS Intervention in the Health Sector: Progress Report. Geneva: World Health Organization; 2007. http://www.who.int/hiv/mediacentre/univeral_access_progress_report_en.pdf April. Available at. [Google Scholar]
- 3.Lawn SD, Harries AD, Anglaret X, Myer L, Wood R. Early mortality among adults accessing antiretroviral treatment programmes in sub-Saharan Africa. AIDS. 2008;22:1897–1908. doi: 10.1097/QAD.0b013e32830007cd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bekker LG, Myer L, Orrel C, Lawn S, Wood R. Rapid scale-up of a community-based HIV treatment service: programme performance over 3 consecutive years in Guguletu, South Africa. S Afr Med J. 2006;96:315–320. [PubMed] [Google Scholar]
- 5.Coetzee D, Hildebrand K, Boulle A, Maartens G, Louis F, Labatala V, Reuter H, Ntwana N, Goemaere E. Outcomes after two years of providing antiretroviral treatment in Khayelitsha, South Africa. AIDS. 2004;18:887–895. doi: 10.1097/00002030-200404090-00006. [DOI] [PubMed] [Google Scholar]
- 6.Wester CW, Kim S, Bussmann H, Avalos A, Ndwapi N, Peter PF, Gaolathe T, Mujugira A, Busang L, Vanderwarker C, Cardiello P, Johnson O, Thior I, Mazonde P, Moffat H, Essex M, Marlink R. Initial response to highly active antiretroviral therapy in HIV-1 C-infected adults in a public sector treatment program in Botswana. J Acquir Immune Defic Syndr. 2005;40:336–342. doi: 10.1097/01.qai.0000159668.80207.5b. [DOI] [PubMed] [Google Scholar]
- 7.Braitstein P, Brinkhof MW, Dabis F, Schechter M, Boulle A, Miotti P, Wood R, Laurent C, Bangsberg DR, Balestre E, Sterne JA, May M, Egger M. Mortality of HIV-1 infected patients in the first year of antiretroviral therapy; comparison between low-income and high-income countries. Lancet. 2006;367:817–824. doi: 10.1016/S0140-6736(06)68337-2. Antiretroviral Therapy in Lower Income Countries (ART-LINC) Collaboration; ART Cohort Collaboration (ART-CC) Groups. [DOI] [PubMed] [Google Scholar]
- 8.Ivers LC, Kendrick D, Doucette K. Efficacy of antiretroviral therapy programs in resource-poor settings: a meta-analysis of the published literature. Clin Infect Dis. 2005;41:217–224. doi: 10.1086/431199. [DOI] [PubMed] [Google Scholar]
- 9.Lawn SD, Myer L, Harling G, Orrel C, Bekker LG, Wood R. Determinants of mortality and nondeath losses from an antiretroviral treatment service in South-Africa: implications for program evaluation. Clin Infect Dis. 2006;43:770–776. doi: 10.1086/507095. [DOI] [PubMed] [Google Scholar]
- 10.Moh R, Danel C, Messou E, Ouassa T, Gabillard D, Anzian A, Abo Y, Salamon R, Bissagnene E, Seyler C, Eholié S, Anglaret X. Incidence and determinants of mortality and morbidity following early antiretroviral therapy initiation in HIV-infected adults in Wet Africa. AIDS. 2007;21:2483–2491. doi: 10.1097/QAD.0b013e3282f09876. [DOI] [PubMed] [Google Scholar]
- 11.Marazzi MC, Guidotti G, Liotta G, Palombi L. Perspectives and Practice in Antiretroviral Ttreatment. Sant' Egido Mozambique and Geneva: World Health Organization; 2005. (DREAM: An Integrated Faith-Based Initiative to treat HIV/AIDS in Mozambique, Case Study). [Google Scholar]
- 12.Marazzi MC, Germano P, Liotta G, Guidotti G, Loureiro S, da Cruz Gomes A, Valls Blazques MC, Narciso P, Perno CF, Mancinelli S, Palombi L. Safety of nevirapine-containing antiretroviral triple therapy regimens to prevent vertical transmission in an African cohort of HIV-1-infected pregnant women. HIV Med. 2006;7:338–344. doi: 10.1111/j.1468-1293.2006.00386.x. [DOI] [PubMed] [Google Scholar]
- 13.Cleveland WS. Robust locally-weighted regression and smoothing scatterplots. JASA. 1979;74:829–836. [Google Scholar]
- 14.Rosen S, Fox MP, Gill CJ. Patient retention in antiretroviral therapy programs in sub-Saharan Africa: a systematic review. PLoS Med. 2007;4:e298. doi: 10.1371/journal.pmed.0040298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Etard JF, Ndiaye I, Thierry-Mieg M, Guèye NF, Guèye PM, Lanièce I, Dieng AB, Diouf A, Laurent C, Mboup S, Sow PS, Delaporte E. Mortality and causes of death in adults receiving highly active antiretroviral therapy in Senegal: a 7-year cohort study. AIDS. 2006;20:1181–1189. doi: 10.1097/01.aids.0000226959.87471.01. [DOI] [PubMed] [Google Scholar]
- 16.De Cock KM, Gilks CF, Lo YR, Guerma T. Can antiretroviral therapy eliminate HIV transmission? Lancet. 2009;373:7–9. doi: 10.1016/S0140-6736(08)61732-8. [DOI] [PubMed] [Google Scholar]
- 17.Chêne G, Sterne JA, May M, Costagliola D, Ledergerber B, Phillips AN, Dabis F, Lundgren J, D'Arminio Monforte A, de Wolf F, Hogg R, Reiss P, Justice A, Leport C, Staszewski S, Gill J, Fatkenheuer G, Egger ME. Prognostic importance of initial response in HIV-1 infected patients starting potent antiretroviral therapy: analysis of prospective studies. Lancet. 2003;362:679–686. doi: 10.1016/s0140-6736(03)14229-8. Antiretroviral Therapy Cohort Collaboration. [DOI] [PubMed] [Google Scholar]


