Abstract
Objective:
To address whether secretion removal techniques increase airway clearance in people with chronic spinal cord injury (SCI).
Data Sources and Study Selection:
MEDLINE/PubMed, CINAHL, EMBASE, and PsycINFO were searched from inception to May 2009 for population keywords (spinal cord injury, paraplegia, tetraplegia, quadriplegia) paired with secretion removal–related interventions and outcomes. Inclusion criteria for articles were a research study, irrespective of design, that examined secretion removal in people with chronic SCI published in English.
Review Methods:
Two reviewers determined whether articles met the inclusion criteria, abstracted information, and performed a quality assessment using PEDro or Downs and Black criteria. Studies were then given a level of evidence based on a modified Sackett scale.
Results:
Of 2,416 abstracts and titles retrieved, 24 met the inclusion criteria. Subjects were young (mean, 31 years) and 84% were male. Most evidence was level 4 or 5 and only 2 studies were randomized controlled trials. Three reports described outcomes for secretion removal techniques in addition to cough, whereas most articles examined the immediate effects of various components of cough. Studies examining insufflation combined with manual assisted cough provided the most consistent, high-level evidence. Compelling recent evidence supports the use of respiratory muscle training or electrical stimulation of the expiratory muscles to facilitate airway clearance in people with SCI.
Conclusion:
Evidence supporting the use of secretion removal techniques in SCI, while positive, is limited and mostly of low level. Treatments that increase respiratory muscle force show promise as effective airway clearance techniques.
Keywords: Spinal cord injuries, Paraplegia, Tetraplegia, Respiratory complications, Ventilation, Physiotherapy, Airway clearance, Assisted breathing devices, Paripep, Flutter, Threshold
INTRODUCTION
Respiratory complications are a leading cause of morbidity and mortality in people with spinal cord injury (SCI) and are more pronounced in individuals with higher level and complete injuries (1–5). A major contributor to respiratory illness in individuals with SCI is secretion retention, particularly among individuals with cervical lesions (1–5). Higher levels of SCI result in greater denervation of the ventilatory muscles thereby decreasing both inspiratory capacity and expiratory muscle force and resulting in an impaired cough (5). Figure 1 shows the innervation of the respiratory muscles (2). Cervical SCI also denervates sympathetic pathways leading to a state of parasympathetic dominance that may increase mucus production (6) and contribute to airway hyperresponsiveness (7). A diminishing cough combined with mucus hypersecretion can overwhelm mucociliary clearance in people with SCI.
Figure 1.
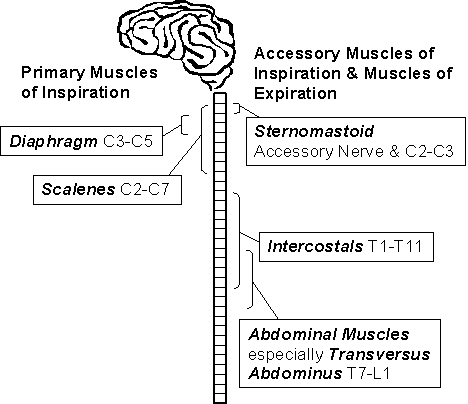
Innervation of respiratory muscles. Reprinted with permission from ICORD Press (2).
The impact of SCI on normal airway clearance can be exemplified by examining the sequence of a cough. After full inspiration to total lung capacity, the glottis is closed followed by an increasing intrathoracic pressure. Opening of the glottis is followed by a forced, high-velocity expiratory flow, which facilitates propagation of sputum towards the upper airway to expectorate or swallow. The ability to inspire to a normal vital capacity (VC) is progressively hindered with higher levels of SCI due to a greater denervation of inspiratory muscles. Inspiring to a lower VC therefore decreases the inward recoil of the chest wall and lungs that contributes to maximal expiratory flow. Forced expiratory flow is further impaired in people with SCI when the injury affects the abdominals (T7-L1) and other expiratory muscles, such as intercostals (thoracic roots), pectoralis (C5-T1), or latissimus dorsi (C6-C8). With high thoracic SCI (T2-T4) the VC might only be 30% to 50% of normal, and the cough might be weak and possibly ineffective (8). Spirometric measures, such as forced vital capacity (FVC), forced expiratory volume in 1 second, and VC, are therefore often valuable predictors of cough strength (9,10).
Non-SCI factors such as smoking, chronic obstructive pulmonary disease, asthma, and aging exacerbate increased mucus secretions resulting from cervical SCI (2,11). Increasing mucus production combined with a diminishing cough and breathing at a lower lung volume, contributes to microatelectasis and potential trapping of retained secretions (12). Ultimately, an ineffective cough, microatelectasis, and retained secretions increase the risk for both pneumonia and mucus plugs, which may lead to potential lung collapse and consolidation (12).
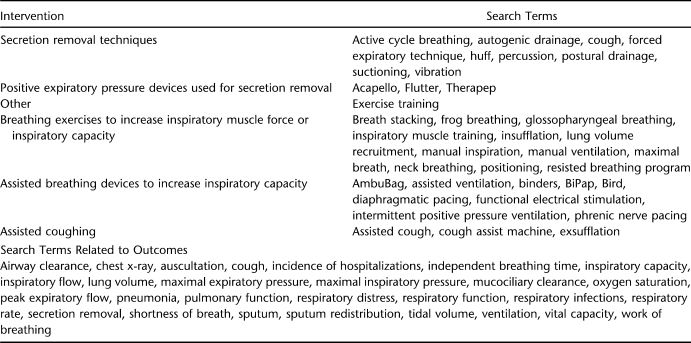
Physiotherapy treatment to facilitate airway clearance (5,13) in people with SCI has included traditional chest physiotherapy techniques of manual percussions and vibrations as well as postural drainage (5). In addition, techniques to enhance forced expiration, including cough, have been used, such as those that improve inspiratory capacity and strength or increase expiratory flow and strength (1,9,12,14–23). Despite these physiotherapy techniques being commonly used there is a scarcity of published evidence to support their effectiveness in SCI. This systematic review was done to answer the question, “Do secretion removal techniques increase airway clearance in people with chronic SCI?” We focused on interventional and survey studies within the scope of physiotherapy practice, therefore excluding pharmaceutical interventions. With the exception of case series or case reports, no studies using a more rigorous design, such as ones that examined percussions, postural drainage, or positive expiratory pressure valves (eg, Flutter) (24), were retrieved from our systematic review. Thus, we extended our search to include studies that examined various outcomes that would contribute to an effective cough as outlined in Table 1. We also limited our systematic review to the chronic phase of SCI among adults with tetraplegia or high paraplegia recognizing that respiratory complications associated with the acute phase of SCI are often managed using more invasive interventions in an acute care hospital setting (25–27). In addition, sequelae associated with this acute phase, such as neurogenic pulmonary edema, unstable fractures, or aspiration pneumonia (25–27), would complicate the interpretation of outcomes as the result of airway clearance interventions such as percussion or assisted cough.
Table 1.
Search Terms Used to Identify Articles About Physiotherapy Interventions and Secretion Removal Outcomes
METHODS
Search Strategy
The databases MEDLINE/PubMed, CINAHL, EMBASE, and PsycINFO were searched for relevant literature from the databases' inceptions through to May 2009. The grey literature was also searched using Google Scholar. Population keywords (spinal cord injury, paraplegia, tetraplegia, quadriplegia) were paired with known terms related to secretion removal interventions and outcomes (see Table 1 for details). References of pertinent articles were also searched and relevant studies were retrieved.
Study Criteria
Studies needed to meet several inclusion criteria, including (a) assessing a physical therapy secretion removal technique as a means of increasing airway clearance; (b) comprising a predominately (≥50%) SCI sample; and (c) examining techniques among individuals with chronic tetraplegia or high paraplegia, which was defined as individuals who were extubated or on chronic modes of mechanical ventilation. Studies not reporting respiratory outcomes related to secretion removal (see Table 1 for search terms related to outcomes) were excluded, as were articles with a sole focus on pharmaceutical interventions. Only studies published in English were reviewed. See Appendix 1 for excluded articles. Titles and abstracts were scanned independently by 2 reviewers (D.R. and J.B.) to identify intervention and survey studies for possible inclusion in the review. Discordant selections were settled by consensus between the 2 reviewers in the presence of a third reviewer (K.K.) who offered an opinion when consensus could not be reached.
Evaluation of Methodologic Quality
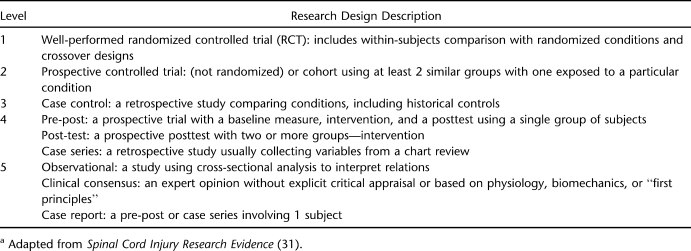
The methodologic quality of articles was assessed using either the PEDro scale (28,29) for randomized controlled trials or the Downs and Black tool for all other study designs (30,31). PEDro scores range from 0 to 10 and Downs and Black scores range from 0 to 27. Higher scores on both scales indicate greater methodologic quality. Scoring was executed by 3 independent reviewers (K.K., J.R., B.S.) and discrepancies were resolved through discussion or a fourth independent reviewer. Studies were also assigned levels of evidence as per a modified Sackett scale (Table 2) (32).
Table 2.
Five Levels of Evidencea
Data Abstraction
Data were abstracted from selected articles by 4 reviewers (J.B., D.R., J.R., and B.S.). Tables were generated from the extracted data and included subject characteristics, nature of the intervention, outcome measures, key results, and respective methodologic scores.
Data Synthesis
Due to the diverse range of interventions captured and the myriad of outcomes with which they were assessed, a quantitative merging of the data was not feasible. Therefore, this review is limited to a systematic assessment of the captured studies' findings.
RESULTS
The search strategy, as outlined in Table 1 and Figure 2, yielded 2,416 articles. After review of titles and abstracts, 133 were of potential interest. After review of the full-length articles, 24 were found to meet the inclusion criteria and 109 articles were excluded because no intervention was examined, the intervention was not focused toward secretion removal, the article was descriptive and did not utilize a clearly described research design, people with SCI were not included, and/or the person with SCI was in the acute rather than the chronic phase (see Appendix 1 for the list of excluded articles). Of the 24 studies, 2 were randomized controlled trials, 3 were prospective controlled design, 9 had pre-post designs, 3 were retrospective case series, and 7 were case reports.
Figure 2.
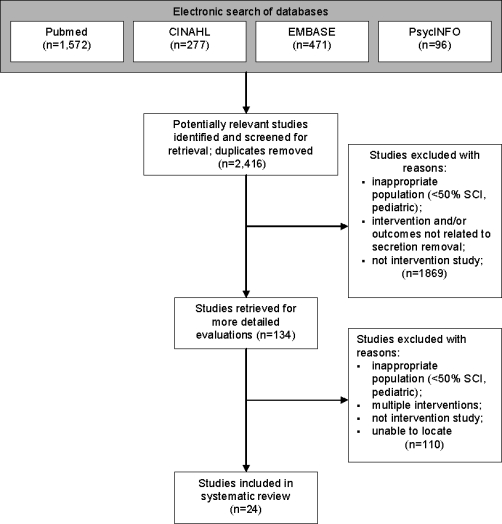
Flowchart illustrating different phases of the search.
The participants in each of the studies ranged in number from 1 to 40 and in age from 15 to 70 years, with a mean age of 30.9 years. Gender, as reported in 22 studies, was shown to be 84% male. Most studies reported on people who had sustained cervical level SCI, only 2 studies (12,23) described individuals with thoracic level SCI, and none included people with paraplegia. Most of the studies examined the immediate effect of the interventions; however, some of the reports described long-term outcomes and benefits.
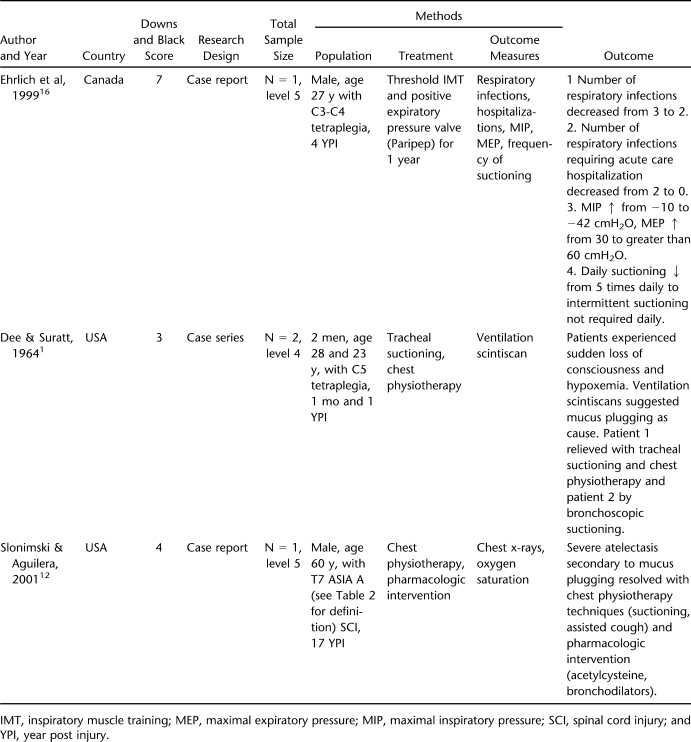
Secretion Removal Techniques
Our systematic search strategy did not reveal any experimental studies in people after SCI that examined facilitation of secretion removal by manual techniques including postural drainage, manual or mechanical vibrations, or any that investigated the use of positive expiratory flow devices that increase airway clearance such as Flutter, Therapep, Acapello, or Paripep. Two case reports and 1 case series, however, described positive outcomes from “chest physiotherapy” (1,12) and an expiratory flow device (16) (Table 3). Two of the studies highlight the significance of how mucus plugging, a life-threatening consequence in people after cervical SCI, can be successfully managed with vigorous chest physiotherapy (1,12). In spite of these 2 reports, evidence of the positive benefit of this intervention is lacking due to (a) the limited number of subjects (only 1 or 2 persons in each report) and (b) a vague description of the chest physiotherapy techniques that were applied to each of these patients. Although 1 report described this type of treatment more fully at the end of the article, this is still insufficient evidence to adequately endorse the techniques.
Table 3.
Secretion Removal Techniques
The article by Ehrlich et al (16) reported that the use of Paripep and inspiratory muscle training for 1 year decreased respiratory infections, decreased hospitalizations due to infection, and decreased suctioning. Although inspiratory muscle force increased 4-fold from 10 to 42 cmH2O, the 2 interventions were used in conjunction with one another for all but 3 weeks of the 1-year intervention; thus, it is difficult to separate any benefit derived from the use of Paripep from that derived from inspiratory muscle training.
In summary, level 4 and 5 evidence, based on 2 case reports (12,16) and 1 case series (1), supports the effectiveness of secretion removal techniques.
Interventions Affecting Cough
The search strategy for our systematic review retrieved several studies that focused on components of cough. These were classified according to the sequential events that contribute to an effective cough including breathing exercises, assistive breathing, and respiratory muscle training (RMT) that improve the VC. The impact of electrical muscle stimulation on inspiratory and expiratory muscle force was examined, as was the effectiveness of assistive devices that facilitate inspiratory capacity, expiratory flow, or cough.
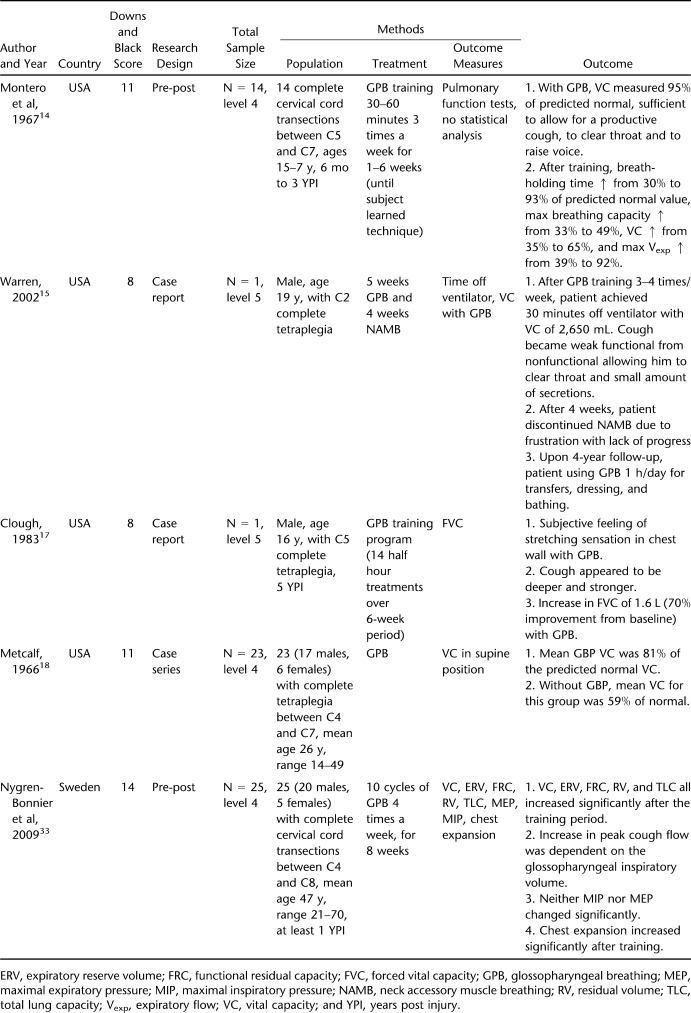
Breathing Exercises
See Table 4. Five articles reported the benefits of different types of breathing exercises such as glossopharyngeal breathing (GPB) or neck accessory muscle breathing in subjects with cervical injuries (level of C2 or higher) (14,15,17,18,33). Length of training ranged from 1 to 8 weeks. The 2 pre-post studies and 2 case reports showed improvements in VC of 7.5% (33), 86% (18), 70% (17), and 35-fold (15). This latter result came from a single case study in which the subject improved from an FVC of 75 to 2,650 mL over the course of 5 weeks of GPB training. Further, 2 of the studies stated that the mean GPB VC was 16% (18) and 28% (33) higher than the VC without GPB. Attributes of cough improved as reflected by an increased strength of cough (17), increased expiratory flow (14,33), and changes from a nonfunctional to a functional cough (15).
Table 4.
Breathing Exercises
Thus, there is level 4 (based on 2 pre-post studies (14,33) and 1 case series (18)) and level 5 evidence (from 2 case reports (15,17)) supporting the effectiveness of GPB to improve cough, a secretion removal technique.
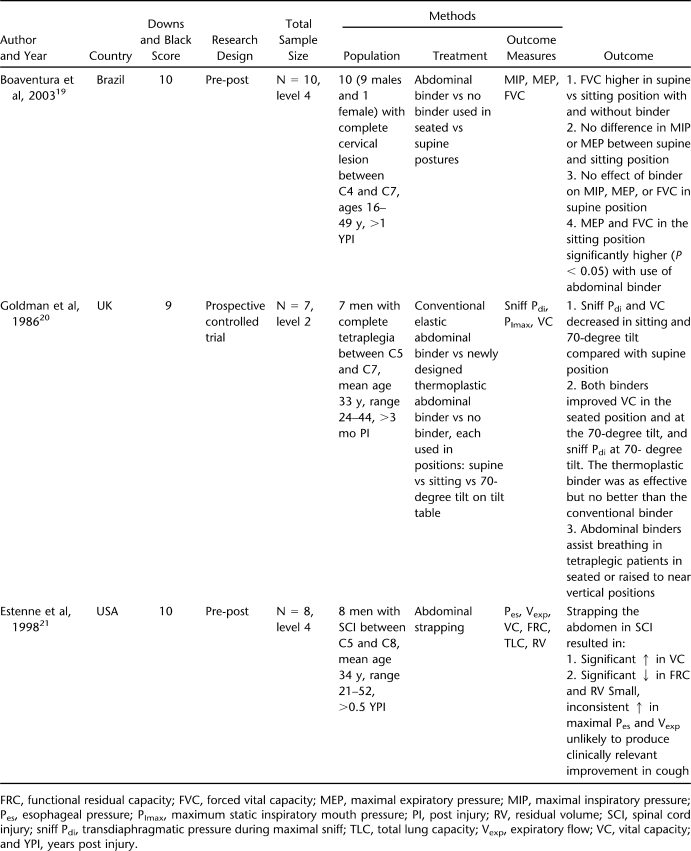
Assisted Breathing by Use of Abdominal Binders or Strapping
See Table 5. Three studies that used either a pre-post or prospective controlled design described the benefits of abdominal binders or strapping on VC or expiratory muscle force in people after cervical SCI (n ranged between 7 and 10) (19–21). In spite of different binder techniques, all studies reported improvements in inspiratory pressures (20,21), VC (20,21), maximal expiratory flow rate (21), or maximal expiratory pressures (19).
Table 5.
Assisted Breathing—Abdominal Binders and Posture
Two studies incorporated postural changes with and without binder use. In both, FVC was greater in the supine position than in sitting (19,20) and FVC (19,20) and maximal expiratory pressure (19) were greater in the seated position when the binder was used. The binders also increased VC and transdiaphragmatic pressure on maximal sniff in the 70-degree tilt position (20). Both studies conclude that binders assist breathing of individuals with tetraplegia when used in upright postures.
In the study by Estenne et al (21), abdominal strapping resulted in a significant increase in VC and decreases in both functional residual capacity and residual volume. Small, inconsistent increases in maximal esophageal pressure and expiratory flow rates were also observed, but the authors question whether these changes would translate to an improved cough.
Thus, there is level 2 evidence (from 1 prospective controlled trial (20)) and level 4 evidence (based on 2 pre-post studies (19,21)) supporting the effectiveness of abdominal binders for assisted breathing.
Respiratory Muscle Training
The benefit of inspiratory muscle training (IMT) in this population has been recently summarized in 4 systematic reviews (2,11,34,35), the most recent one published in September 2008. In brief, because of differing research designs, heterogeneity of subjects, and differences in training protocols, none of the studies performed to date could be combined for a meta-analysis. Further, none of the studies performed thus far appear to apply an effective IMT protocol with the exception of the case study that used a threshold training device (16) and a randomized control trial (RCT) on 14 participants that used normocapnic hyperpnea training (36). Both of these reports provide evidence that respiratory infections occur less frequently and inspiratory muscle strength and endurance improve after IMT (16,36). This recent, high-quality RCT (PEDro = 8) provides level 1 evidence that RMT improves respiratory muscle strength and decreases the number of respiratory infections (36), both of which infer improved airway clearance. Specific measures of airway clearance, however, were not measured.
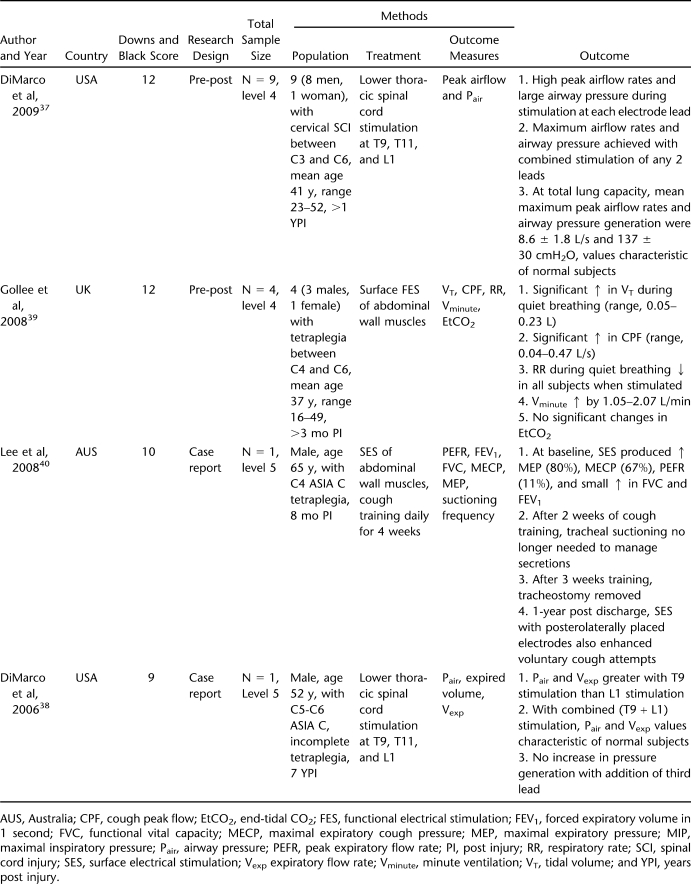
Electrical Stimulation
See Table 6. Two case reports and 2 pre-post test design studies described the effect of electrical stimulation of the lower thoracic-lumbar spinal cord (T9, T11, and L1) (37,38) and the abdominal wall muscles on expiratory pressures and peak expiratory flow rates (39,40). Stimulation of the lower thoracic-lumbar spinal cord was performed up to 60 times daily for 2 to 3 months (37,38), whereas stimulation of the abdominal muscle wall was performed over 3 sessions (39) or daily for 4 weeks (40). The intensity of the stimulation was increased to obtain maximal expiratory flow rates but was constrained to a level that did not induce spasticity or co-contraction of the adjacent musculature. All protocols increased peak flow rates and cough peak flows in all studies (37–40). During combined T9 + L1 stimulation, airway pressures and expiratory flow rates increased to at least 132 cmH2O and 7.4 L/s, respectively (37,38), which are consistent with values from a healthy person. The mean maximal pressure generation was lower (137 cmH2O); however, several subjects achieved values in the normal range (37) (normal maximal expiratory pressure is approximately 200 cmH2O in men and approximately 150 cmH2O in women) (41).
Table 6.
Functional Electrical Stimulation
Thus, there is level 4 evidence based on 2 pre-post trials and level 5 evidence from 2 case reports that supports the use of electrical stimulation of the lower thoracic-lumbar spinal cord (T9, T11, and L1) (37,38) and the abdominal wall muscles (39,40) to improve expiratory flow rates during cough.
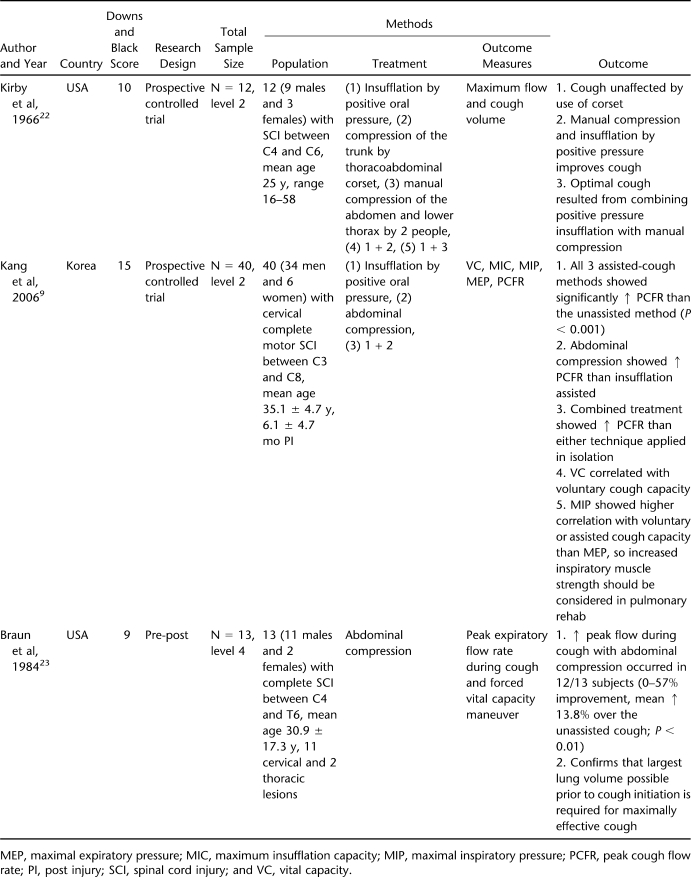
Assisted Coughing
See Table 7. The systematic search retrieved 3 reports that described outcomes related to assisted cough techniques including 2 controlled trials (9,22) and 1 pre-post design (23). Most patients had cervical lesions with the exception of the report by Braun et al (23), which included 2 individuals with thoracic SCI. All 3 reports showed that manual abdominal compression applied by 1 (22) or 2 persons (9,22,23) resulted in improved cough expiratory flows. The 2 articles that examined the combination of 2 or more methods found that positive oral pressure insufflation combined with abdominal compression resulted in the highest cough expiratory flow rates (9,22).
Table 7.
Assisted Coughing—Manual Assistance, Insufflation-Exsufflation
Thus, there is level 2 (based on 2 prospective controlled trials (9,22)) and level 4 (based on 1 pre-post trial (23)) evidence supporting the effectiveness of abdominal assisted coughing.
Intermittent Positive Pressure Breathing
Intermittent positive pressure breathing (IPPB) has been reported to improve cough; however, our search strategy did not reveal any articles that evaluated the impact of this technique on any aspect of secretion removal including VC, expiratory flow rates, or cough. Three studies, however, described the impact of IPPB on lung mechanics and aspects of ventilation (42–44), but no increases in VC were reported that could be attributed solely to the IPPB intervention. Another RCT that examined mechanical insufflation-exsufflation as a clearance technique was excluded because it provided insufficient description of the subjects to determine time from injury (45).
Adverse Effects
The systematic search strategy revealed only a couple of reports that described adverse effects of physical therapy techniques aimed toward secretion removal. Both of these articles described adverse events in response to assisted cough maneuvers. Greenfield filters that are inserted into the inferior vena cava can be displaced distally and be deformed by quad coughs (46). Further, a case report described a perforation of the small bowel after a quad cough maneuver that required surgical repair (47). Although an assisted cough was not definitively determined to be the underlying trauma that caused the bowel perforation, this case report highlights the importance of applying the appropriate force during this maneuver to people after SCI.
DISCUSSION
We found only 3 articles that addressed secretion removal directly (1,12,16). This was surprising given that respiratory complications are the leading cause of morbidity and mortality in people with chronic SCI. Most articles examined related interventions that improve different components of cough, including those that increase VC, maximum respiratory pressures, or flow rates. Dramatic reductions of suctioning frequency (16) and changes in a ventilation scintiscan and chest radiograph (1,12) provide evidence that chest physiotherapy (1,12) or the use of the expiratory flow device Paripep (Table 3) (16), can be effective; however, a major limitation of these studies was that the specific chest physiotherapy techniques (postural drainage, manual or mechanical vibrations, etc) were not described (1,12).
Enhancement of VC, an essential component of an effective cough, is improved by the use of abdominal binders or strapping (19–21), GPB (14,15,17,18,33), and RMT by normocapnic hyperpnea (36). Benefits from each of these strategies may be dependent on a variety of factors. For instance, abdominal binding is a passive approach but requires skill in its application and may be more effective in upright postures. From a clinical perspective, anatomy of the thorax and abdomen, in addition to patient compliance, may determine whether changes are sufficient to improve cough (21). GPB, the most widely studied of the 3 techniques, requires engagement and learning of the person with SCI but has the advantage of being a technique that can be performed independently. RMT likely shows the most untapped potential of the three. Although earlier systematic reviews (2,11,34,35) describe questionable benefit from RMT, a recent RCT provides strong evidence that this therapy enhances lung expansion and flow rates in patients with SCI and reduces respiratory infection frequency (36).
Respiratory muscle training has been used with variable success in other patient groups with neuromuscular conditions such as myasthenia gravis (48) and amyotrophic lateral sclerosis (ALS) (49) and in patients with chronic respiratory disease (50). Major considerations when determining potential benefit include an evaluation of the underlying adaptability of the respiratory muscles in addition to the choice of training technique. A finite potential for respiratory muscle adaptation might explain the equivocal benefit of RMT reported in ALS and Duchenne muscular dystrophy (49,51). This variable should be considered when evaluating RMT for those with high SCI; however, to date, the lack of improvements following RMT in many previous studies on this population have been attributed to ineffective training protocols and not to limited ability of the respiratory muscles to adapt (2,11,34,35). In contrast, the normocapnic hyperpnea training used in a recent RCT (36) consistently provided a training load via high flow ventilation that could be reasonably expected to recruit muscles at a higher velocity of contraction and a greater range of motion during inspiration and expiration. A more practical approach that may prove to be equally effective for people with SCI is the use of a Threshold device (HealthScan Products Inc, Cedar Grove, NJ); however, this method primarily stresses the inspiratory muscles only. Inspiratory muscle training using threshold or targeted techniques have demonstrated widespread benefits in people with chronic obstructive pulmonary disease (50).
Assisted cough techniques that include insufflation and manual compression (9,22,23) or electrical stimulation (37–40) are effective in improving cough and/or peak expiratory flow rates in people with SCI. Normocapnic hyperpnea training may result in comparable gains toward improving cough (36); however, the relative benefits of these approaches have not been compared. Assisted cough techniques require another person with the necessary skill, whereas electrical stimulation and the benefits derived from RMT can be used independently. The most obvious drawback of electrical stimulation is the surgical implantation of the electrodes (37,38) or maintenance of the surface application of electrodes (39,40). Preference for a given technique might not only depend on successful outcomes of airway clearance but also on the potential adverse events, as well as comfort and compliance of the person with SCI.
Worthy of note, none of the reports describing IPPB that met the inclusion criteria of this systematic review showed improvements in VC, flow rates, or cough (42–44). However, considering the potential benefit of IPPB on respiratory compliance and lung volumes, this intervention is worthy of further study. Another study (45) that used an RCT design showed improvements in forced expiratory volume in 1 second, FVC, and peak expiratory flow rate following mechanical insufflation-exsufflation (MIE); however, this study did not include a detailed description of the level of injury or the time since injury to allow for adequate comparison of the 2 groups. Other issues of concern were a lack of description of the random allocation method or subject number and characteristics in the control vs treatment group. Although this RCT implies a strong design, the poor comparability of subject groups and lack of information confound interpretation of the positive outcomes. Several reports describe the use of MIE to successfully facilitate airway clearance in mid and late stages of ALS (52–55); however, in spite of the similarities between late-stage ALS and high-level SCI, published reports on the efficacy of MIE in airway clearance for SCI remain lacking. Indeed, only 2 other reports on the use of MIE in SCI were retrieved from our search. One was a survey study investigating patient and care-provider perceptions of MIE for airway clearance in SCI (56). The other examined the use of MIE in 46 patients with various neuromuscular disorders including 9 with SCI (57). Although neither of these studies met the inclusion criteria of this systematic review, both report positive outcomes and perceptions of MIE use in SCI. In view of the sparse yet positive literature on this subject, further investigation into the use of MIE in SCI is warranted.
A systematic search of adverse effects resulting from secretion removal techniques only revealed 2 reports that described events purportedly due to manual assisted cough. In 9 individuals, Greenfield filters were displaced proximally (46) and in 1 individual, the small bowel was perforated and required surgical repair (47). The small number of reported adverse affects is consistent with the sparse literature investigating secretion removal in people with SCI. In other populations that experience respiratory complications, bronchial clearance by manual percussion and vibration techniques has been associated with such adverse events as oxygen desaturation, bronchospasm, fractured ribs, bruising, and patient intolerance (58). Although people with SCI may be at risk of experiencing similar adverse responses, these data are not available. Of clinical importance, individuals predisposed to such adverse events are more often critically ill patients or those with comorbid issues such as bronchial hyperresponsiveness, bone decalcification, or coagulopathy (58). In any event, the adverse events reported in response to the manual assisted cough technique in people with SCI provide ample indication that therapists should be prudent when applying this technique and should monitor the patient accordingly.
This systematic review is limited by the small number of studies that primarily consisted of weaker designs and small sample sizes. Most of the studies had 14 subjects or less and 50% were a pre-post design or case series, which only provide level 4 evidence. A second major limitation was that the studies asked various questions related to aspects of airway clearance; however, no two RCTs asked a similar question. Of those studies that showed improved pulmonary function related to airway clearance, more clinically relevant outcomes such as hospitalizations, respiratory infections, or impact on health-related quality of life were not often reported. Of course, publication bias of studies primarily reporting positive outcomes need to be considered while reviewing the evidence of this systematic review.
Perhaps the greatest void in the literature was a lack of reference to other secretion removal techniques that have proved to be effective in other patient populations (59–61). Techniques such as huffing, active cycle breathing techniques, autogenic drainage, and the use of positive expiratory pressure devices are well-described airway clearance therapies used in people with respiratory conditions that result in excessive mucus production (24). Only Ehrlich et al (16) described the use of a positive expiratory pressure valve even though similar devices have shown significant benefits in patients with chronic bronchitis (60), cystic fibrosis (61), and bronchiectasis (62). Similar to the technique used by Ehrlich et al (16), use of IMT may be a prerequisite to ensure adequate inspiratory volumes for the effective use of positive expiratory pressure devices. The successful application or limitations of other airway clearance techniques in people with SCI, in addition to those reported in this review, are worthy of exploration.
CONCLUSION
In conclusion, level 4 evidence supports the use of secretion removal techniques in people with SCI and higher levels of evidence (levels 1, 2, and 4) are reflected by investigations that examined the various components of cough. The most promising are treatments that promote respiratory muscle force. A thorough scouring of the literature revealed a paucity of articles that used a large number of participants and only 2 randomized controlled trials were retrieved. The more common study designs of case reports and pre-post tests during the last decade reflects the difficulty of performing large-scale randomized trials in people with SCI and limits clinical recommendations supported by higher levels of evidence. In spite of this low level of evidence, clinical use of secretion removal techniques in individuals with chronic SCI are highly recommended given the high incidence of pulmonary complications. The merits of various airway clearance techniques are described elsewhere for other populations and should be carefully considered when selecting the best approach for those with chronic SCI (58).
This review yielded the following clinical messages:
-
(a)
The evidence supporting use of secretion removal techniques in people with SCI, although positive, is limited and mostly low level.
-
(b)
Insufflation combined with manual assisted cough provides the most consistent evidence.
-
(c)
Treatments that increase respiratory muscle force show promise as effective airway clearance techniques.
Appendix 1 Excluded Articles (n = 109)
- Alshekhlee A, Onders RP, Syed TU, Elmo M, Katirji B. Phrenic nerve conduction studies in spinal cord injury: applications for diaphragmatic pacing. Muscle Nerve. 2008;38((6)):1546–1552. doi: 10.1002/mus.21123. [DOI] [PubMed] [Google Scholar]
- Alvarez SE, Peterson M, Lunsford BR. Respiratory treatment of the adult patient with spinal cord injury. Phys Ther. 1981;61((12)):1737–1745. doi: 10.1093/ptj/61.12.1737. [DOI] [PubMed] [Google Scholar]
- Amodie-Storey C, Nash MS, Roussell PM, Knox AW, Crane LD. Head position and its effect on pulmonary function in tetraplegic patients. Spinal Cord. 1996;34((10)):602–607. doi: 10.1038/sc.1996.107. [DOI] [PubMed] [Google Scholar]
- Andrews BJ, Wheeler GD. Functional and therapeutic benefits of electrical stimulation after spinal injury. Curr Opin Neurol. 1995;8((6)):461–466. doi: 10.1097/00019052-199512000-00012. [DOI] [PubMed] [Google Scholar]
- Bach JR. Alternative methods of ventilatory support for the patient with ventilatory failure due to spinal cord injury. J Am Paraplegia Soc. 1991;14((4)):158–174. doi: 10.1080/01952307.1991.11735849. [DOI] [PubMed] [Google Scholar]
- Bach JR. Cough in SCI patients. Arch Phys Med Rehabil. 1994;75((5)):610. [PubMed] [Google Scholar]
- Bach JR. Inappropriate weaning and late onset ventilatory failure of individuals with traumatic spinal cord injury. Paraplegia. 1993;31((7)):430–438. doi: 10.1038/sc.1993.72. [DOI] [PubMed] [Google Scholar]
- Bach JR. Mechanical insufflation/exsufflation: has it come of age?: a commentary. Eur Respir J. 2003;21((3)):385–386. doi: 10.1183/09031936.03.00098702. [DOI] [PubMed] [Google Scholar]
- Bach JR. Respiratory muscle aids for the prevention of pulmonary morbidity and mortality. Semin Neurol. 1995;15((1)):72–83. doi: 10.1055/s-2008-1041010. [DOI] [PubMed] [Google Scholar]
- Bell S, Shaw-Dunn J, Gollee H, Allan DB, Fraser MH, McLean AN. Improving respiration in patients with tetraplegia by functional electrical stimulation: an anatomical perspective. Clin Anat. 2007;20((6)):689–693. doi: 10.1002/ca.20493. [DOI] [PubMed] [Google Scholar]
- Beraldo PS, Mateus SR, Fernandes MC. Cough in patients with SCI. Phys Ther. 2000;80((4)):416. doi: 10.1093/ptj/80.4.416. [DOI] [PubMed] [Google Scholar]
- Berlowitz DJ, Brown DJ. Sleep disordered breathing. Arch Phys Med Rehabil. 2002;83((9)):1325. [PubMed] [Google Scholar]
- Bianchi C, Grandi M, Felisari G. Efficacy of glossopharyngeal breathing for a ventilator-dependent, high-level tetraplegic patient after cervical cord tumor resection and tracheotomy. Am J Phys Med Rehabil. 2004;83((3)):216–219. doi: 10.1097/01.phm.0000113408.96258.06. [DOI] [PubMed] [Google Scholar]
- Biering-Sorensen F, Lehmann Knudsen J, Schmidt A, Bundgaard A, Christensen I. Effect of respiratory training with a mouth-nose-mask in tetraplegics. Paraplegia. 1991;29((2)):113–119. doi: 10.1038/sc.1991.15. [DOI] [PubMed] [Google Scholar]
- Biering-Sorensen M, Norup PW, Jacobsen E, Biering-Sorensen F. Treatment of sleep apnoea in spinal cord injured patients. Paraplegia. 1995;33((5)):271–273. doi: 10.1038/sc.1995.61. [DOI] [PubMed] [Google Scholar]
- Broggi G, Franzini A, Borroni V. Phrenic nerve pacing in reversible cervical cord lesion: a case report. Acta Neurochir. 1980;51((3–4)):273–278. doi: 10.1007/BF01406754. [DOI] [PubMed] [Google Scholar]
- Brown R, DiMarco AF, Hoit JD, Garshick E. Respiratory dysfunction and management in spinal cord injury. Respir Care. 2006;51((8)):853–870. [PMC free article] [PubMed] [Google Scholar]
- Cahill JL, Okamoto GA, Higgins T, Davis A. Experiences with phrenic nerve pacing in children. J Pediatr Surg. 1983;18((6)):851–854. doi: 10.1016/s0022-3468(83)80035-9. [DOI] [PubMed] [Google Scholar]
- Cameron TS, McKinstry A, Burt SK, et al. Outcomes of patients with spinal cord injury before and after introduction of an interdisciplinary tracheostomy team. Crit Care Resusc. 2009;11((1)):14–19. [PubMed] [Google Scholar]
- Campbell DA, Homan SD, McCulloch GA, Stern LM, Leckie WJ. Phrenic nerve pacing in two young quadriplegic ventilator-dependent patients. Aust N Z J Med. 1992;22((5)):463–468. [PubMed] [Google Scholar]
- Chatwin M, Simonds A. Mechanical technique for assisted cough. Physiotherapy. 2002;88((6)):381–382. [Google Scholar]
- Cheng PT, Chen CL, Wang CM, Chung CY. Effect of neuromuscular electrical stimulation on cough capacity and pulmonary function in patients with acute cervical cord injury. J Rehabil Med. 2006;38((1)):32–36. doi: 10.1080/16501970510043387. [DOI] [PubMed] [Google Scholar]
- Churliaev I, Lukashev KV, Martynenkov VI, Chepizhko SI, Voevodin SV. External respiratory function in patients with spinal cord damage at the cervical and thoracic levels [Russian] Anesteziol Reanimatol. 2008;3:43–45. [PubMed] [Google Scholar]
- Claxton AR, Wong DT, Chung F, Fehlings MG. Predictors of hospital mortality and mechanical ventilation in patients with cervical spinal cord injury. Can J Anaesth. 1998;45((2)):144–149. doi: 10.1007/BF03013253. [DOI] [PubMed] [Google Scholar]
- Crane L, Klerk K, Ruhl A, Warner P, Ruhl C, Roach KE. The effect of exercise training on pulmonary function in persons with quadriplegia. Paraplegia. 1994;32((7)):435–441. doi: 10.1038/sc.1994.70. [DOI] [PubMed] [Google Scholar]
- Cruzado D, Jones MJ, Segebart S, Mcdonagh J. Resistive inspiratory muscle training improves inspiratory muscle strength in subjects with cervical spinal cord injury. Neurol Rep. 2002;26:3–7. [Google Scholar]
- Davis K, Jr, Johannigman JA, Campbell RS, et al. The acute effects of body position strategies and respiratory therapy in paralyzed patients with acute lung injury. Crit Care. 2001;5((2)):81–87. doi: 10.1186/cc991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derrickson J, Ciesla N, Simpson N, Imle PC. A comparison of two breathing exercise programs for patients with quadriplegia. Phys Ther. 1992;72((11)):763–769. doi: 10.1093/ptj/72.11.763. [DOI] [PubMed] [Google Scholar]
- Dicpinigaitis PV, Grimm DR, Lesser M. Cough reflex sensitivity in subjects with cervical spinal cord injury. Am J Respir Crit Care. 1999;159(5p+1):1660–1662. doi: 10.1164/ajrccm.159.5.9810060. [DOI] [PubMed] [Google Scholar]
- DiMarco A, Onders R, Kowalski K, Miller M, Ferek S, Mortimer J. Phrenic nerve pacing in a tetraplegic patient via intramuscular diaphragm electrodes. Am J Respir Crit Care. 2002;66((1604)):1606. doi: 10.1164/rccm.200203-175CR. [DOI] [PubMed] [Google Scholar]
- DiMarco AF, Onders RP, Ignagni A, Kowalski KE. Inspiratory muscle pacing in spinal cord injury: case report and clinical commentary. J Spinal Cord Med. 2006;29((2)):95–108. doi: 10.1080/10790268.2006.11753863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiMarco AF, Romaniuk JR, Kowalski KE, Supinski G. Mechanical contribution of expiratory muscles to pressure generation during spinal cord stimulation. J Appl Physiol. 1999;87((4)):1433–1439. doi: 10.1152/jappl.1999.87.4.1433. [DOI] [PubMed] [Google Scholar]
- DiMarco AF, Romaniuk JR, Kowalski KE, Supinski G. Pattern of expiratory muscle activation during lower thoracic spinal cord stimulation. J Appl Physiol. 1999;86((6)):1881–1889. doi: 10.1152/jappl.1999.86.6.1881. [DOI] [PubMed] [Google Scholar]
- Dimarco AF, Romaniuk JR, Supinski GS. Electrical activation of the expiratory muscles to restore cough. Am J Respir Crit Care. 1995;151((5)):1466–1471. doi: 10.1164/ajrccm.151.5.7735601. [DOI] [PubMed] [Google Scholar]
- Dimarco AF, Supinski G, Petro J, Tahaoka Y. Evaluation of intercostal pacing to provide artificial ventilation in quadriplegics. Am J Respir Crit Care. 1994;150:934–940. doi: 10.1164/ajrccm.150.4.7921466. [DOI] [PubMed] [Google Scholar]
- DiMarco AF, Takaoka Y, Kowalski KE. Combined intercostal and diaphragm pacing to provide artificial ventilation in patients with tetraplegia. Arch Phys Med Rehabil. 2005;86((6)):1200–1207. doi: 10.1016/j.apmr.2004.11.027. [DOI] [PubMed] [Google Scholar]
- DiMarco AF. Restoration of respiratory muscle function following spinal cord injury: review of electrical and magnetic stimulation techniques. Respir Physiol Neurobiol. 2005;147((2–3)):273–287. doi: 10.1016/j.resp.2005.03.007. [DOI] [PubMed] [Google Scholar]
- Elefteriades JA, Quin JA, Hogan JF, et al. Long-term follow-up of pacing of the conditioned diaphragm in quadriplegia. Pacing Clin Electrophysiol. 2002;25((6)):897–906. doi: 10.1046/j.1460-9592.2002.00897.x. [DOI] [PubMed] [Google Scholar]
- Elmo MJ, Onders RP, Ignagni A. Diaphragm pacing in tetraplegics: living better without the ventilator. Sci Nurs. 2008;25((1)):59–60. [Google Scholar]
- Epstein SW, Vanderlinden RG, Hyland RH, Lenkei SCM, Wise DJ, Mendok H. Lung function in diaphragm pacing. Can Med Assoc J. 1979;120:1360–1369. [PMC free article] [PubMed] [Google Scholar]
- Estenne M, De Troyer A. Cough in tetraplegic subjects: an active process. Ann Intern Med. 1990;112((1)):22–28. doi: 10.7326/0003-4819-112-1-22. [DOI] [PubMed] [Google Scholar]
- Estenne M, Knoop C, Vanvaerenbergh J, Heilporn A, De Toyer A. The effect of pectoralis muscle training in tetraplegic subjects. Am Rev Respir Dis. 1989;139((5)):1989. doi: 10.1164/ajrccm/139.5.1218. [DOI] [PubMed] [Google Scholar]
- Estenne M, Pinet C, De Troyer A. Abdominal muscle strength in patients with tetraplegia. Am J Respir Crit Care. 2000;161:707–712. doi: 10.1164/ajrccm.161.3.9906020. [DOI] [PubMed] [Google Scholar]
- Estenne M, Van Muylem A, Gorini M, Kinnear W, Heilporn A, De Troyer A. Evidence of dynamic airway compression during cough in tetraplegic patients. Am J Respir Crit Care. 1994;150((4)):1081–1085. doi: 10.1164/ajrccm.150.4.7921440. [DOI] [PubMed] [Google Scholar]
- Finnerup NB, Johannesen IL, Bach FW, Jensen TS. Sensory function above lesion level in spinal cord injury patients with and without pain. Somatosens Mot Res. 2003;20((1)):71–76. doi: 10.1080/0899022031000083843. [DOI] [PubMed] [Google Scholar]
- Fujiwara T, Hara Y, Chino N. Expiratory function in complete tetraplegics: study of spirometry, maximal expiratory pressure, and muscle activity of pectoralis major and latissimus dorsi muscles. Am J Phys Med Rehabil. 1999;78((5)):464–469. doi: 10.1097/00002060-199909000-00009. [DOI] [PubMed] [Google Scholar]
- Garrido-Garcia H, Martin-Escribano P, Palomera-Frade J, Arroyo O, Alonso-Calderon JL, Mazaira-Alvarez J. Transdiaphragmatic pressure in quadriplegic individuals ventilated by diaphragmatic pacemaker. Thorax. 1996;51((4)):420–423. doi: 10.1136/thx.51.4.420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrido-Garcia H, Mazaira Alvarez J, Martin Escribano P, et al. Treatment of chronic ventilatory failure using a diaphragmatic pacemaker. Spinal Cord. 1998;36((5)):310–314. doi: 10.1038/sj.sc.3100558. [DOI] [PubMed] [Google Scholar]
- Garstang SV, Kirshblum SC, Wood KE. Patient preference for in-exsufflation for secretion management with spinal cord injury. J Spinal Cord Med. 2000;23((2)):80–85. doi: 10.1080/10790268.2000.11753511. [DOI] [PubMed] [Google Scholar]
- Gilgoff IS, Barras DM, Jones MS, Adkins HV. Neck breathing: a form of voluntary respiration for the spine-injured ventilator-dependent quadriplegic child. Pediatrics. 1988;82((5)):741–745. [PubMed] [Google Scholar]
- Girsch W, Koller R, Holle J, et al. Vienna phrenic pacemaker-experience with diaphragm pacing in children. Eur J Pediatr Surg. 1996;6((3)):140–143. doi: 10.1055/s-2008-1066491. [DOI] [PubMed] [Google Scholar]
- Glenn WW, Hogan JF, Loke JS, Ciesielski TE, Phelps ML, Rowedder R. Ventilatory support by pacing of the conditioned diaphragm in quadriplegia. N Engl J Med. 1984;310((18)):1150–1155. doi: 10.1056/NEJM198405033101804. [DOI] [PubMed] [Google Scholar]
- Glenn WW, Holcomb WG, Shaw RK, Hogan JF, Holschuh KR. Long-term ventilatory support by diaphragm pacing in quadriplegia. Ann Surg. 1976;183((5)):566–577. doi: 10.1097/00000658-197605000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldsmith HS, Saunders RL. Low chest compression for removal of pulmonary secretions. Surgery. 1983;94((5)):847–848. [PubMed] [Google Scholar]
- Gollee H, Hunt KJ, Allan DB, Fraser MH, McLean AN. A control system for automatic electrical stimulation of abdominal muscles to assist respiratory function in tetraplegia. Med Eng Phys. 2007;29((7)):799–807. doi: 10.1016/j.medengphy.2006.08.007. [DOI] [PubMed] [Google Scholar]
- Gross D, Ladd HW, Riley EJ, Macklem PT, Grassino A. The effect of training on strength and endurance of the diaphragm in quadriplegia. Am J Med. 1980;68((1)):27–35. doi: 10.1016/0002-9343(80)90157-6. [DOI] [PubMed] [Google Scholar]
- Gutierrez CJ, Harrow J, Haines F. Using an evidence-based protocol to guide rehabilitation and weaning of ventilator-dependent cervical spinal cord injury patients. J Rehabil Res Dev. 2003;40((5 suppl)):99–110. doi: 10.1682/jrrd.2003.10.0099. [DOI] [PubMed] [Google Scholar]
- Hall AM, Watt JW. The use of tracheal stoma stents in high spinal cord injury: a patient-friendly alternative to long-term tracheostomy tubes. Spinal Cord. 2008;46((11)):753–755. doi: 10.1038/sc.2008.18. [DOI] [PubMed] [Google Scholar]
- Hascakova-Bartova R, Dinant JF, Parent A, Ventura M. Neuromuscular electrical stimulation of completely paralyzed abdominal muscles in spinal cord-injured patients: a pilot study. Spinal Cord. 2008;46((6)):445–450. doi: 10.1038/sj.sc.3102166. [DOI] [PubMed] [Google Scholar]
- Hirschfeld S, Exner G, Luukkaala T, Baer GA. Mechanical ventilation or phrenic nerve stimulation for treatment of spinal cord injury-induced respiratory insufficiency. Spinal Cord. 2008;46((11)):738–742. doi: 10.1038/sc.2008.43. [DOI] [PubMed] [Google Scholar]
- Hoit J, Banzett S. Speech breathing in individuals with cervical spinal cord injury. J Speech Hear Res. 1990;33((4)):798–807. doi: 10.1044/jshr.3304.798. [DOI] [PubMed] [Google Scholar]
- Hsiao IN, Lin VW. Improved coil design for functional magnetic stimulation of expiratory muscles. IEEE Trans Biomed Eng. 2001;48((6)):684–694. doi: 10.1109/10.923786. [DOI] [PubMed] [Google Scholar]
- Huang C, Kuhlemeier KV, Ratanaubol U. Cardiopulmonary response in spinal cord injury patients: effect of pneumatic compressive devices. Arch Phys Med Rehabil. 1983;64((3)):101–106. [PubMed] [Google Scholar]
- Huldtgren AC, Fugl-Meyer AR, Jonasson E, Bake B. Ventilatory dysfunction and respiratory rehabilitation in post-traumatic quadriplegia. Eur J Respir Dis. 1980;61((6)):347–356. [PubMed] [Google Scholar]
- Imle PC, Boughton AC. The physical therapist's role in the early management of acute spinal cord injury. Top Acute Care Trauma Rehabil. 1987;1((3)):32–47. [Google Scholar]
- Iriarte J, Narbona J, Garcia del Barrio L, Artieda J. Diaphragmatic flutter after spinal cord trauma in a child. Neurology. 2005;65((11)):1839. doi: 10.1212/01.wnl.0000187081.72301.8b. [DOI] [PubMed] [Google Scholar]
- Jaeger RJ, Turba RM, Yarkony GM, Roth EJ. Cough in spinal cord injured patients: comparison of three methods to produce cough. Arch Phys Med Rehabil. 1993;74((12)):1358–1361. doi: 10.1016/0003-9993(93)90093-p. [DOI] [PubMed] [Google Scholar]
- James WS, III, Minh VD, Minteer MA, Moser KM. Cervical accessory respiratory muscle function in a patient with a high cervical cord lesion. Chest. 1977;71((1)):59–64. doi: 10.1378/chest.71.1.59. [DOI] [PubMed] [Google Scholar]
- Liaw MY, Lin MC, Cheng PT, Wong MK, Tang FT. Resistive inspiratory muscle training: its effectiveness in patients with acute complete cervical cord injury. Arch Phys Med Rehabil. 2000;81((6)):752–756. doi: 10.1016/s0003-9993(00)90106-0. [DOI] [PubMed] [Google Scholar]
- Lin KH, Lai YL, Wu HD, Wang TQ, Wang YH. Effects of an abdominal binder and electrical stimulation on cough in patients with spinal cord injury. J Formos Med Assoc. 1998;97((4)):292–295. [PubMed] [Google Scholar]
- Lin VW, Hsiao IN, Zhu E, Perkash I. Functional magnetic stimulation for conditioning of expiratory muscles in patients with spinal cord injury. Arch Phys Med Rehabil. 2001;82((2)):162–166. doi: 10.1053/apmr.2001.18230. [DOI] [PubMed] [Google Scholar]
- Lin VW, Singh H, Chitkara RK, Perkash I. Functional magnetic stimulation for restoring cough in patients with tetraplegia. Arch Phys Med Rehabil. 1998;79((5)):517–522. doi: 10.1016/s0003-9993(98)90065-x. [DOI] [PubMed] [Google Scholar]
- Linder SH. Functional electrical stimulation to enhance cough in quadriplegia. Chest. 1993;103((1)):166–169. doi: 10.1378/chest.103.1.166. [DOI] [PubMed] [Google Scholar]
- Liszner K, Feinberg M. Cough assist strategy for pulmonary toileting in ventilator-dependent spinal cord injured patients. Rehabil Nurs. 2006;31((5)):218–221. doi: 10.1002/j.2048-7940.2006.tb00138.x. [DOI] [PubMed] [Google Scholar]
- Loveridge B, Badour M, Dubo H. Ventilatory muscle endurance training in quadriplegia: effects on breathing pattern. Paraplegia. 1989;27((5)):329–339. doi: 10.1038/sc.1989.50. [DOI] [PubMed] [Google Scholar]
- Lucke KT. Pulmonary management following acute SCI. J Neurosci Nurs. 1998;30((2)):91–104. doi: 10.1097/01376517-199804000-00003. [DOI] [PubMed] [Google Scholar]
- March A. A review of respiratory management in spinal cord injury. J Orthop Nurs. 2005;9((1)):19–26. [Google Scholar]
- Massery M. Manual breathing and coughing aids. Phys Med Rehabil Clin North Am. 1996;7((2)):407–422. [Google Scholar]
- Milane J, Jonquet O, Bertrand P. Ventilatory assistance by pneumatic belt. Eur Respir Rev. 1993;3((12)):305–307. [Google Scholar]
- Miller HJ, Thomas E, Wilmot CB. Pneumobelt use among high quadriplegic population. Arch Phys Med Rehabil. 1988;69:369–372. [PubMed] [Google Scholar]
- Nelson VS. Noninvasive mechanical ventilation for children and adolescents with spinal cord injuries. Top Spinal Cord Inj Rehabil. 2000;6((suppl 1)):12–15. [Google Scholar]
- Pillastrini P, Bordini S, Bazzocchi G, Belloni G, Menarini M. Study of the effectiveness of bronchial clearance in subjects with upper spinal cord injuries: examination of a rehabilitation program involving mechanical insufflation and exsufflation. Spinal Cord. 2006;44((10)):614–616. doi: 10.1038/sj.sc.3101870. [DOI] [PubMed] [Google Scholar]
- Pryor JA. Physiotherapy for airway clearance in adults. Eur Respir J. 1999;14((6)):1418–1424. doi: 10.1183/09031936.99.14614189. [DOI] [PubMed] [Google Scholar]
- Ribeiro RN, de Menezes A, Goretti LC, Lanschi J. Effects of inspiratory muscle training for quadriplegic patients [Portuguese] Fisother Pesquisa. 2007;14((1)):72–78. [Google Scholar]
- Rutchik A, Weissman AR, Almenoff PL, Spungen AM, Bauman WA, Grimm DR. Resistive inspiratory muscle training in subjects with chronic cervical spinal cord injury. Arch Phys Med Rehabil. 1998;79((3)):293–297. doi: 10.1016/s0003-9993(98)90009-0. [DOI] [PubMed] [Google Scholar]
- Sapienza CM, Wheeler K. Respiratory muscle strength training: functional outcomes versus plasticity. Semin Speech Lang. 2006;27((4)):236–244. doi: 10.1055/s-2006-955114. [DOI] [PubMed] [Google Scholar]
- Schmitt JK, Stiens S, Trincher R, et al. Survey of use of the insufflator-exsufflator in patients with spinal cord injury. J Spinal Cord Med. 2007;30((2)):127–130. doi: 10.1080/10790268.2007.11753923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh H, Magruder M, Bushnik T, Lin VW. Expiratory muscle activation by functional magnetic stimulation of thoracic and lumbar spinal nerves. Crit Care Med. 1999;27((10)):2201–2205. doi: 10.1097/00003246-199910000-00022. [DOI] [PubMed] [Google Scholar]
- Sortor S. Pulmonary concerns in quadriplegia. AARC Times. 1992;16((6)):34–38. [Google Scholar]
- Sortor S. Pulmonary issues in quadriplegia. Eur Respir Rev. 1992;2((10)):330–334. [Google Scholar]
- Spivak E, Keren O, Niv D, et al. Electromyographic signal-activated functional electrical stimulation of abdominal muscles: the effect on pulmonary function in patients with tetraplegia. Spinal Cord. 2007;45((7)):491–495. doi: 10.1038/sj.sc.3102039. [DOI] [PubMed] [Google Scholar]
- Spungen AM, Grimm DR, Lesser M, Bauman WA, Almenoff PL. Self-reported prevalence of pulmonary symptoms in subjects with spinal cord injury. Spinal Cord. 1997;35((10)):652–657. doi: 10.1038/sj.sc.3100489. [DOI] [PubMed] [Google Scholar]
- Spungen AM, Grimm DR, Schilero G, et al. Relationship of respiratory symptoms with smoking status and pulmonary function in chronic spinal cord injury. J Spinal Cord Med. 2002;25((1)):23–27. doi: 10.1080/10790268.2002.11753597. [DOI] [PubMed] [Google Scholar]
- Stanic U, Kandare F, Jaeger R, Sorli J. Functional electrical stimulation of abdominal muscles to augment tidal volume in spinal cord injury. IEEE Trans Rehabil Eng. 2000;8((1)):30–34. doi: 10.1109/86.830946. [DOI] [PubMed] [Google Scholar]
- Sugarman B. Atelectasis in spinal cord injured people after initial medical stabilization. J Am Paraplegia Soc. 1985;8((3)):47–50. [PubMed] [Google Scholar]
- Sutbeyaz ST, Koseoglu BF, Gokkaya NK. The combined effects of controlled breathing techniques and ventilatory and upper extremity muscle exercise on cardiopulmonary responses in patients with spinal cord injury. Int J Rehabil Res. 2005;28((3)):273–276. doi: 10.1097/00004356-200509000-00012. [DOI] [PubMed] [Google Scholar]
- Taylor PN, Tromans AM, Harris KR, Swain ID. Electrical stimulation of abdominal muscles for control of blood pressure and augmentation of cough in a C3/4 level tetraplegic. Spinal Cord. 2002;40((1)):34–36. doi: 10.1038/sj.sc.3101250. [DOI] [PubMed] [Google Scholar]
- Toki A, Tamura R, Sumida M. Long-term ventilation for high-level tetraplegia: a report of 2 cases of noninvasive positive-pressure ventilation. Arch Phys Med Rehabil. 2008;89((4)):779–783. doi: 10.1016/j.apmr.2007.09.043. [DOI] [PubMed] [Google Scholar]
- Tubbs RS, Pearson B, Loukas M, Shokouhi G, Shoja MM, Oakes WJ. Phrenic nerve neurotization utilizing the spinal accessory nerve: technical note with potential application in patients with high cervical quadriplegia. Childs Nerv Syst. 2008;24((11)):1341–1344. doi: 10.1007/s00381-008-0650-4. [DOI] [PubMed] [Google Scholar]
- Uijl SG, Houtman S, Folgering HT, Hopman MT. Training of the respiratory muscles in individuals with tetraplegia. Spinal Cord. 1999;37((8)):575–579. doi: 10.1038/sj.sc.3100887. [DOI] [PubMed] [Google Scholar]
- van Der Schans CP, Piers DA, Mulder GA. Efficacy of coughing in tetraplegic patients. Spine. 2000;25((17)):2200–2203. doi: 10.1097/00007632-200009010-00010. [DOI] [PubMed] [Google Scholar]
- Vereen LE, Payne DK, George RB. Unilateral absence of ventilation and perfusion associated with a bronchial mucous plug. South Med J. 1987;80((3)):391–393. doi: 10.1097/00007611-198703000-00033. [DOI] [PubMed] [Google Scholar]
- Viroslav J, Rosenblatt R, Tomazevic SM. Respiratory management, survival, and quality of life for high-level traumatic tetraplegics. Respir Care Clin North Am. 1996;2((2)):313–322. [PubMed] [Google Scholar]
- Voelker KG, Chetty KG, Mahutte CK. Resolution of recurrent atelectasis in spinal cord injury patients with administration of recombinant human DNase. Intens Care Med. 1996;22((6)):582–584. doi: 10.1007/BF01708100. [DOI] [PubMed] [Google Scholar]
- Walker J, Cooney M, Norton S. Improved pulmonary function in chronic quadriplegics after pulmonary therapy and arm ergometry. Paraplegia. 1989;27((4)):278–283. doi: 10.1038/sc.1989.41. [DOI] [PubMed] [Google Scholar]
- Wang AY, Jaeger RJ, Yarkony GM, Turba RM. Cough in spinal cord injured patients: the relationship between motor level and peak expiratory flow. Spinal Cord. 1997;35((5)):299–302. doi: 10.1038/sj.sc.3100370. [DOI] [PubMed] [Google Scholar]
- Wang TG, Wang YH, Tang FT, Lin KH, Lien IN. Resistive inspiratory muscle training in sleep-disordered breathing of traumatic tetraplegia. Arch Phys Med Rehabil. 2002;83((4)):491–496. doi: 10.1053/apmr.2002.30937. [DOI] [PubMed] [Google Scholar]
- Yarkony GM, Jaeger RJ, Gittler M. Medical grand rounds: cough in tetraplegia. Top Spinal Cord Inj Rehabil. 1997;3((1)):67–70. [Google Scholar]
- Zupan A, Savrin R, Erjavec T, et al. Effects of respiratory muscle training and electrical stimulation of abdominal muscles on respiratory capabilities in tetraplegic patients. Spinal Cord. 1997;35((8)):540–545. doi: 10.1038/sj.sc.3100433. [DOI] [PubMed] [Google Scholar]
References
- Dee PM, Suratt PM. Mucous plugging stimulating pulmonary embolism in patients with quadriplegia. Chest. 1964;85(3):363–366. doi: 10.1378/chest.85.3.363. [DOI] [PubMed] [Google Scholar]
- Sheel AW, Reid WD, Townson AF, Ayas N. Respiratory management following spinal cord injury. In: Eng JJ, Teasell RW, Miller WC, et al., editors. Spinal Cord Injury Rehabilitation Evidence (SCIRE). Vol 2.0. Vancouver, BC: ICORD Press; 2008. pp. 8.1–8.40. [Google Scholar]
- Hoit JD, Banzett RB, Brown R, Loring SH. Speech breathing in individuals with cervical spinal cord injury. J Speech Hear Res. 1990;33(4):798–807. doi: 10.1044/jshr.3304.798. [DOI] [PubMed] [Google Scholar]
- Shavelle RM, DeVivo MJ, Strauss DJ, Paculdo DR, Lammertse DP, Day SM. Long-term survival of persons ventilator dependent after spinal cord injury. J Spinal Cord Med. 2006;29(5):511–519. doi: 10.1080/10790268.2006.11753901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey L. Respiratory management. In: Anonymous, editor. Management of Spinal Cord Injuries: A Guide for Physiotherapists. Vol 1. New York: Elsevier Ltd; 2008. pp. 205–225. [Google Scholar]
- Bhaskar KR, Brown R, O'Sullivan DD, Melia S, Duggan M, Reid L. Bronchial mucus hypersecretion in acute quadriplegia. Am Rev Respir Dis. 1991;143(3):640–648. doi: 10.1164/ajrccm/143.3.640. [DOI] [PubMed] [Google Scholar]
- Dicpinigaitis PV, Spungen AM, Bauman WA, Absgarten A, Almenoff PL. Bronchial hyperresponsiveness after cervical spinal cord injury. Chest. 1994;105(4):1073–1076. doi: 10.1378/chest.105.4.1073. [DOI] [PubMed] [Google Scholar]
- Zejdlik CP. Management of Spinal Cord Injury. 2nd ed. Sudbury, MA: Jones and Bartlett Publishers Inc; 1992. [Google Scholar]
- Kang SW, Shin JC, Park CI, Moon JH, Rha DW, Cho DH. Relationship between inspiratory muscle strength and cough capacity in cervical spinal cord injured patients. Spinal Cord. 2006;44(4):242–248. doi: 10.1038/sj.sc.3101835. [DOI] [PubMed] [Google Scholar]
- Kang SW, Bach JR. Maximum insufflation capacity: the relationships with vital capacity and cough flows for patients with neuromuscular disease. Am J Phys Med Rehabil. 2000;79(3):222–227. doi: 10.1097/00002060-200005000-00002. [DOI] [PubMed] [Google Scholar]
- Sheel AW, Reid WD, Townson AF, Ayas N. Respiratory management following spinal cord injury. In: Eng JJ, Teasell RW, Miller WC, et al., editors. Spinal Cord Injury Rehabilitation Evidence. Vancouver, BC: ICORD Press; 2006. pp. 8.1–8.30. [Google Scholar]
- Slonimski M, Aguilera EJ. Atelectasis and mucus plugging in spinal cord injury: case report and therapeutic approaches. J Spinal Cord Med. 2001;24(4):284–288. doi: 10.1080/10790268.2001.11753586. [DOI] [PubMed] [Google Scholar]
- Pryor JA. Physiotherapy for airway clearance in adults. Eur Respir J. 1999;14(6):1418–1424. doi: 10.1183/09031936.99.14614189. [DOI] [PubMed] [Google Scholar]
- Montero JC, Feldman DJ, Montero D. Effects of glossopharyngeal breathing on respiratory function after cervical cord transection. Arch Phys Med Rehab. 1967;48(12):650–653. [PubMed] [Google Scholar]
- Warren V. Glossopharyngeal and neck accessory muscle breathing in a young adult with C2 complete tetraplegia resulting in ventilator dependency. Phys Ther. 2002;82(6):590–600. [PubMed] [Google Scholar]
- Ehrlich M, Manns PJ, Poulin C. Respiratory training for a person with C3-C4 tetraplegia. Aust J Physiother. 1999;45(4):301–307. doi: 10.1016/s0004-9514(14)60359-7. [DOI] [PubMed] [Google Scholar]
- Clough P. Glossopharyngeal breathing: its application with a traumatic quadriplegic patient. Arch Phys Med Rehabil. 1983;64(8):384–385. [PubMed] [Google Scholar]
- Metcalf VA. Vital capacity and glossopharyngeal breathing in traumatic quadriplegia. Phys Ther. 1966;46(8):835–838. doi: 10.1093/ptj/46.8.835. [DOI] [PubMed] [Google Scholar]
- Boaventura GM, Gastaldi AG, Silveira JM, Santos PR, Guimaraes RG, De Lima LG. Effect of an abdominal binder on the efficacy of respiratory muscles in seated and supine tetraplegic patients. Physiotherapy. 2003;89(5):290–295. [Google Scholar]
- Goldman JM, Rose LS, Williams SJ, Silver JR, Denison DM. Effect of abdominal binders on breathing in tetraplegic patients. Thorax. 1986;41(12):940–945. doi: 10.1136/thx.41.12.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estenne M, Van Muylem A, Gorini M, Kinnear W, Heilporn A, De Troyer A. Effects of abdominal strapping on forced expiration in tetraplegic patients. Am J Resp Crit Care. 1998;157(1):95–98. doi: 10.1164/ajrccm.157.1.9701010. [DOI] [PubMed] [Google Scholar]
- Kirby NA, Barnerias MJ, Siebens AA. An evaluation of assisted cough in quadriparetic patients. Arch Med Phys Rehab. 1966;47(11):705–710. [PubMed] [Google Scholar]
- Braun SR, Giovannoni R, O'Connor M. Improving the cough in patients with spinal cord injury. Am J Phys Med. 1984;63(1):1–10. [PubMed] [Google Scholar]
- Reid WD, Chung F. Clinical Management Notes and Case Histories in Cardiopulmonary Physical Therapy. Thorofare, NJ: Slack Publishers; 2004. Airway clearance techniques; pp. 103–114. [Google Scholar]
- Claxton AR, Wong DT, Chung F, Fehlings MG. Predictors of hospital mortality and mechanical ventilation in patients with cervical spinal cord injury. Can J Anaesth. 1998;45(2):144–149. doi: 10.1007/BF03013253. [DOI] [PubMed] [Google Scholar]
- Lucke KT. Pulmonary management following acute SCI. J Neurosci Nurs. 1998;30:91–104. doi: 10.1097/01376517-199804000-00003. [DOI] [PubMed] [Google Scholar]
- March A. A review of respiratory management in spinal cord injury. J Orthop Nurs. 2005;9(1):19–26. [Google Scholar]
- Maher CG SC, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83(8):713–721. [PubMed] [Google Scholar]
- Physiotherapy Evidence Database PEDro. Available at: www.pedro.org.au. Accessed October 29, 2009.
- Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Commun Health. 1998;52(6):377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eng J, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC. Spinal Cord Injury Research Evidence. Vancouver, BC: ICORD Press; 2006. Methods of the systematic reviews; pp. 2.1–2.11. [Google Scholar]
- Sackett DL, Strauss SE, Richardson WS, Rosenberg W, Haynes RB. Evidence-Based Medicine: How to Practice and Teach EBM. 2nd ed. Toronto, Ontario: Churchill Livingstone; 2000. [Google Scholar]
- Nygren-Bonnier M, Wahman K, Lindhom P, Markstrom A, Westgren N, Klefbeck B. Glossopharyngeal pistoning for lung insufflation in patients with cervical spinal cord injury. Spinal Cord. 2009;47(5):418–422. doi: 10.1038/sc.2008.138. [DOI] [PubMed] [Google Scholar]
- Brooks D, O'Brien K, Geddes EL, Crowe J, Reid WD. Is inspiratory muscle training effective for individuals with cervical spinal cord injury?: a qualitative systematic review. Clin Rehabil. 2005;19(3):237–246. doi: 10.1191/0269215505cr856oa. [DOI] [PubMed] [Google Scholar]
- Van Houtte S, Vanlandewijck Y, Gosselink R. Respiratory muscle training in persons with spinal cord injury: a systematic review. Resp Med. 2006;100(11):1886–1895. doi: 10.1016/j.rmed.2006.02.029. [DOI] [PubMed] [Google Scholar]
- Van Houtte S, Vanlandewijck Y, Kiekens C, Spengler CM, Gosselink R. Patients with acute spinal cord injury benefit from normocapnic hyperpnoea training. J Rehabil Med. 2008;40(2):119–125. doi: 10.2340/16501977-0140. [DOI] [PubMed] [Google Scholar]
- DiMarco AF, Kowalski KE, Geertman RT, Hromyak DR. Lower thoracic spinal cord stimulation to restore cough in patients with spinal cord injury: results of a National Institutes of Health-sponsored clinical trial. Part I: Methodology and effectiveness of expiratory muscle activation. Arch Phys Med Rehabil. 2009;90(5):717–725. doi: 10.1016/j.apmr.2008.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiMarco AF, Kowalski KE, Geertman RT, Hromyak DR. Spinal cord stimulation: a new method to produce an effective cough in patients with spinal cord injury. Am J Resp Crit Care. 2006;173:1386–1389. doi: 10.1164/rccm.200601-097CR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gollee H, Hunt KJ, Allan DB, Fraser MH, McLean AN. Automatic electrical stimulation of abdominal wall muscles increases tidal volume and cough peak flow in tetraplegia. Technol Health Care. 2008;16(4):273–281. [PubMed] [Google Scholar]
- Lee BB, Boswell-Ruys C, Butler JE, Gandevia SC. Surface functional electrical stimulation of the abdominal muscles to enhance cough and assist tracheostomy decannulation after high-level spinal cord injury. J Spinal Cord Med. 2008;31(1):78–82. doi: 10.1080/10790268.2008.11753985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black LF, Hyatt RE. Maximal respiratory pressures: normal values and relationship to age and sex. Am Rev Respir Dis. 1969;99(5):696–702. doi: 10.1164/arrd.1969.99.5.696. [DOI] [PubMed] [Google Scholar]
- McCool FD, Mayewski RF, Shayne DS, Gibson CJ, Griggs RC, Hyde RW. Intermittent positive pressure breathing in patients with respiratory muscle weakness: alterations in total respiratory system compliance. Chest. 1986;90(4):546–552. doi: 10.1378/chest.90.4.546. [DOI] [PubMed] [Google Scholar]
- Bach J. New approaches in the rehabilitation of the traumatic high level quadriplegic. Am J Phys Med Rehab. 1991;70(1):13–19. doi: 10.1097/00002060-199102000-00004. [DOI] [PubMed] [Google Scholar]
- Laffont I, Bensmail D, Lortat-Jacob S, et al. Intermittent positive-pressure breathing effects in patients with high spinal cord injury. Arch Phys Med Rehabil. 2008;89(9):1575–1579. doi: 10.1016/j.apmr.2007.12.037. [DOI] [PubMed] [Google Scholar]
- Pillastrini P, Bordini S, Bazzocchi G, Belloni G, Menarini M. Study of the effectiveness of bronchial clearance in subjects with upper spinal cord injuries: examination of a rehabilitation program involving mechanical insufflation and exsufflation. Spinal Cord. 2006;44(10):614–616. doi: 10.1038/sj.sc.3101870. [DOI] [PubMed] [Google Scholar]
- Balshi J. Complications of caval interruption by Greenfield filter in quadriplegics. J Vasc Surg. 1989;9(4):558–562. doi: 10.1067/mva.1989.vs0090558. [DOI] [PubMed] [Google Scholar]
- Pearl J, Ramirez AR, Petruzziello M, Perdue P. Small bowel perforation after a quad cough maneuver. J Trauma. 2001;51(1):162–163. doi: 10.1097/00005373-200107000-00028. [DOI] [PubMed] [Google Scholar]
- Fregonezi G, Resqueti VR, Güell R, Pradas J, Casan P. Effects of 8-week, interval-based inspiratory muscle training and breathing retraining in patients with generalized myasthenia gravis. Chest. 2005;128(3):1524–1530. doi: 10.1378/chest.128.3.1524. [DOI] [PubMed] [Google Scholar]
- Cheah BC, Boland RA, Brodaty NE, et al. INSPIRATIonAL-INSPIRAtory muscle training in amyotrophic lateral sclerosis. Amyotroph Lateral Scler. 2009;10(5–6):384–392. doi: 10.3109/17482960903082218. [DOI] [PubMed] [Google Scholar]
- Geddes EL, O'Brien K, Reid WD, Brooks D, Crowe J. Inspiratory muscle training in adults with chronic obstructive pulmonary disease: an update of a systematic review. Respir Med. 2008;102(12):1715–1720. doi: 10.1016/j.rmed.2008.07.005. [DOI] [PubMed] [Google Scholar]
- Gozal D. Pulmonary manifestations of neuromuscular disease with special reference to Duchenne muscular dystrophy and spinal muscular atrophy. Pediatr Pulmonol. 2000;29(2):141–150. doi: 10.1002/(sici)1099-0496(200002)29:2<141::aid-ppul9>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- Sancho J, Servera E, Diaz J, Marin J. Efficacy of mechanical insufflation-exsufflation in medially stable patients with amyotrophic lateral sclerosis. Chest. 2004;125(4):1400–1405. doi: 10.1378/chest.125.4.1400. [DOI] [PubMed] [Google Scholar]
- Sancho S, Servera E, Vergara P, Marin J. Mechanical insufflation-exsufflation vs. tracheal suctioning via tracheostomy tubes for patients with amyotrophic lateral sclerosis. Am J Phys Med Rehabil. 2003;82(10):750–753. doi: 10.1097/01.PHM.0000087456.28979.2E. [DOI] [PubMed] [Google Scholar]
- Hanayama K, Ishikawa Y, Bach JR. Amyotrophic lateral sclerosis. Successful treatment of mucous plugging by mechanical insufflation-exsufflation. Am J Phys Med Rehabil. 1997;76(4):338–339. doi: 10.1097/00002060-199707000-00017. [DOI] [PubMed] [Google Scholar]
- Lahrmann H, Wild M, Zdrahal F, Grisold W. Expiratory muscle weakness and assisted cough in ALS. Amyotroph Lateral Scler Other Motor Neuron Disord. 2003;4(1):49–51. doi: 10.1080/14660820310006733. [DOI] [PubMed] [Google Scholar]
- Schmitt JK, Stiens S, Trincher R, et al. Survey of use of the insufflator-exsufflator in patients with spinal cord injury. J Spinal Cord Med. 2007;30(2):127–130. doi: 10.1080/10790268.2007.11753923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bach JR. Mechanical insufflation-exsufflation. Comparison of peak expiratory flows with manually assisted and unassisted coughing techniques. Chest. 1993;104(5):1553–1562. doi: 10.1378/chest.104.5.1553. [DOI] [PubMed] [Google Scholar]
- Reid WD, Chung F. Thorofare, NJ: Slack Publisher; 2004. Clinical management notes and case histories in cardiopulmonary physical therapy. [Google Scholar]
- Volsko TA, DiFiore JM, Chatburn RL. Performance comparison of two oscillating positive expiratory pressure devices: Acapella versus Flutter. Respir Care. 2003;48(2):124–130. [PubMed] [Google Scholar]
- Bellone A, Lascioli R, Raschi S, Guzzi L, Adone R. Chest physical therapy in patients with acute exacerbation of chronic bronchitis: effectiveness of three modes. Arch Phys Med Rehabil. 2000;81(5):558–560. doi: 10.1016/s0003-9993(00)90034-0. [DOI] [PubMed] [Google Scholar]
- Flume PA, Robinson KA, O'Sullivan BP, et al. Clinical practice guidelines for pulmonary therapies committee. Respir Care. 2009;54:522–537. [PubMed] [Google Scholar]
- Murray MP, Pentland JL, Hill AT. A randomised crossover trial of chest physiotherapy in non-cystic fibrosis bronchiectasis. Eur Respir J. 2009;34:1086–1092. doi: 10.1183/09031936.00055509. [DOI] [PubMed] [Google Scholar]