Abstract
Objective
To evaluate the positive predictive value (PPV) of a diagnosis of heart failure (HF) in the Danish National Registry of Patients (NRP) among patients admitted to a University Hospital cardiac care unit, and to evaluate the impact of misdiagnosing HF.
Design
The NRP was used to identify patients with heart failure from July 1, 2005 to June 30, 2007. Heart failure was defined in accordance with European Society of Cardiology (ESC) guidelines. The recorded diagnoses from the NRP were compared with clinical data from the medical records.
Results
We identified 758 patients with a diagnosis of heart failure in the NRP. The PPV of a heart failure discharge diagnosis was 84.0% (95% confidence interval: 81.2–86.6). Patients with a discharge diagnosis of HF in the NRP without fulfilling the ESC criteria for HF had a better survival rate, a lower rate of rehospitalization, none were followed in the outpatient clinic, and they had a lower consumption of anticongestive medicine after discharge.
Conclusion
We found a relatively high PPV of the HF diagnosis in the NRP, and the NRP can therefore be a valuable tool for identification of patients with HF. However, using the NRP alone will not give a true picture of the cost and total burden of the disease.
Keywords: heart failure, diagnosis, positive predictive value, National Registry of Patients
Introduction
Heart failure (HF) is a growing public health problem. The prevalence of HF is 2%–3% in western countries and rises sharply among 70- to 80-year-old people with a prevalence of about 10%–20%.1 HF is the cause of 5% of acute hospital admissions and is present among 10% of patients in hospital beds in the United Kingdom (UK).1 It has been estimated that HF accounts for more than 2% of national expenditure on health in the UK.1
The diagnosis of HF can be difficult to define. It might be easy to diagnose HF in its moderate or severe form where the patient has characteristic symptoms and signs of HF with echocardiographic evidence of structural abnormalities. However, symptoms and signs of early HF can be difficult to interpret among elderly with higher degrees of comorbidities and among obese patients. And the problem of defining heart failure can especially be seen in its milder forms where patients may complain of breathlessness, tiredness, and fatigue but without having echocardiographic evidence of left ventricular systolic dysfunction.2–3 The European Society of Cardiology (ESC) has developed guidelines for the diagnosis, assessment, and treatment of HF which to some extent may have clarified the difficulties in diagnosing HF.1,2 However, there might still be some isolated patients with difficulties in heart failure classification.
Following the considerable health problem of HF there is a need for reliable methods for identification of patients with HF. Data on hospitalization due to HF are registered in hospital discharge registers with specific HF codes. These administrative registers are increasingly used in health research and provide important information on diagnosis-related group (DRG)-values and patient volume. However, due to the difficulties in diagnosing HF the accuracy of coding HF has been questioned.4–9 The aim of this study was therefore to estimate the positive predictive value (PPV) of recorded diagnoses of HF in a University Hospital discharge register against ESC guidelines, and to examine the impact of misdiagnosing HF.
Material and methods
Herlev University Hospital is serving a local population of 200,000. The Danish National Registry of Patients (NRP) identified patients referred to the outpatient clinic (OPC), heart failure clinic (HFC), or those admitted to the cardiology ward in Herlev University Hospital and discharged with a HF diagnosis, during the period July 1, 2005 to June 30, 2007. This register contains 99.4% of all discharge records from Danish hospitals including outpatient visits, and information about the diagnoses has been coded according to the International Classification of Diseases, 10th edition (ICD-10).10 The codes used for identification of heart failure patients were: I11.0 (hypertensive heart disease with heart failure), I13.0 (hypertensive heart and renal disease with heart failure), I13.2 (hypertensive heart and renal disease with both heart failure and renal disease), I42.0 (dilated cardiomyopathy), I42.6–9 (other cardiomyopathies), I50.0–I50.1 and I50.9 (heart failure).
The authors systematically reviewed the records of all patients with a discharge diagnosis of heart failure during the period of October 14, 2009 to March 23, 2010. Author SM, who is following a clinical and research training programme in cardiology, initially reviewed the records. The recorded data were checked and transferred to a database by author FN, who is a specialist in cardiology. If the two authors disagreed about a HF diagnosis, the case was adjudicated by consensus agreement after discussion.
The following information was obtained from the records: age; gender; weight; height; tobacco use and alcohol consumption; results of laboratory tests; the probability of heart failure, and if the registered heart failure diagnosis was a primary or secondary diagnosis, and if heart failure was new, onset or chronic heart failure; New York Heart Association class (NYHA); history of ischemic heart disease (IHD), ie, angina pectoris, previous myocardial infarction, previous performed percutanous coronary intervention (PCI) or coronary artery by-pass grafting (CABG); history of valve disease; other comorbidities, ie, chronic pulmonary disease, hypertension, diabetes mellitus, stroke, atrial fibrillation, thyroid disease; and pacemaker or implantable cardioverter defibrillator unit implant. Diabetes mellitus was considered present if the patients were on antidiabetic therapy with diet or medication. Hypertension, chronic pulmonary lung disease, and thyroid disease were defined as a history of the specific diseases diagnosed by the patient’s doctor. Previous stroke was considered present if the diagnosis was confirmed from the records.
The 12-lead electrocardiogram (ECG) were reviewed and analyzed for rhythm (sinus rhythm, atrial fibrillation, other rhythms), bundle branch block, left ventricular hypertrophy (LVH), and ischemia. LVH was determined as the voltage sum SV1 + RV5 or RV6 ≥ 35 mm using Sokolow–Lyon voltage criteria, and myocardial ischemia was considered present if a ≥1 mm horizontal or downward sloping ST shift in >1 of the 12 electrocardiographic leads was found.
All echocardiographic descriptions were reviewed by the authors and information on dimensions of the left chambers, left ventricular ejection fraction (LVEF), and severity of valve diseases was registered. Information on pulmonary congestion was obtained from the descriptions of the chest X-ray.
Information was obtained from the records regarding medical treatment, referral to the HFC or the OPC after discharge, referrals for invasive examinations (coronary angiography) and invasive treatments (PCI, CABG, valve operation), and readmissions during the first years.
Inadequate information about some of the variables (eg, NYHA classification, chamber dimensions on echocardiograms, laboratory tests) excluded them from further analyses.
Data on survival were obtained from the Danish Civil Registration System. The study was registered and approved by the Danish Data Protection Agency.
Definition of heart failure
ESC guidelines for the diagnosis of heart failure, valid for the period under study, were used as diagnostic criteria.1 In accordance with these criteria the patients should have the following symptoms of heart failure: typically breathlessness or fatigue, either at rest or during exertion, or ankle swelling, and objective evidence of cardiac dysfunction shown by echocardiography.
The records and referral notes from the patient’s general practitioner (GP) were reviewed carefully for description of symptoms and signs of heart failure on admission or at the time for referring from the GP.
The probability of heart failure was graded in definite heart failure (DHF) and no heart failure (NHF). DHF was defined as symptoms and signs of heart failure with at least one objective evidence of a structural or functional abnormality of the heart. Patients with structural abnormalities of the heart on echocardiography but with doubts about symptoms and signs of HF were classified as having DHF.
Statistics
All patients were followed from the date of admission until death or end of follow-up, whichever came first. Continuous data were summarized as median, interquartile range (IQR), and range. Categorical variables were reported as frequencies and percentages. Differences in baseline variables were estimated by use of absolute differences (DIF) with 95% confidence intervals (CI) for categorical variables or Wilcoxon rank-sum test for continuous variables.
Survival was estimated by the Kaplan–Meier method. The non parametric log-rank procedure was used to compare survival times in groups. The proportional-hazards assumption was evaluated graphically, with plots of logarithm of negative logarithm of survival.
The PPV was calculated as the proportion of patients registered with a HF diagnosis in the NRP and who also fulfilled the ESC criteria for HF.
Data were analyzed using Stata 11.0 (StataCorp, College Station, TX).
Results
During the study period, 758 patients were either hospitalized acute (60.0%) or referred to the OPC or HFC, and all had a discharge diagnosis of heart failure. A total of 320 (42.2%) of the patients were women. The median age was 75 years (interquartile range [IQR] 65–82; range 33–99).
Baseline characteristics according to the criteria of HF used are shown in Table 1. A total of 637 patients with a registered HF diagnosis in the NRP fulfilled the criteria of DHF (Table 1). The PPV of a HF discharge diagnosis was estimated to 84.0% (95% CI: 81.2–86.6). Among patients (n = 479) with first time HF the PPV were 77.9% (95% CI: 74.1–81.6).
Table 1.
Characteristics of patients in relation to heart failure classification
| DHF | NHF | |
|---|---|---|
| Registered HF in the NRP (n) | 637 | 121 |
| Age, years | 75.7 | 69.9 |
| Male (%) | 60.4 | 43.8 |
| IHD (%) | 55.9 | 29.8 |
| BMI (kg/m2) | 25.5 | 28.2 |
| Hypertension (%) | 45.5 | 53.7 |
| Diabetes (%) | 18.7 | 16.5 |
| COPD (%) | 15.5 | 9.9 |
| Atrial fibrillation (%) | 47.6 | 19.0 |
| ECG performed (%) | 97.8 | 91.7 |
| Sinus rhythm (%) | 56.0 | 82.0 |
| Atrial fibrillation (%) | 39.2 | 16.2 |
| Hypertrophy (%) | 20.4 | 10.8 |
| Ischemia (%) | 58.4 | 29.7 |
| Echo performed (%) | 95.1 | 77.7 |
| LVEF%; median | 35 | 60 |
| Aortic stenosis | ||
| Mild (%) | 1.0 | 0 |
| Moderate (%) | 1.7 | 0 |
| Severe (%) | 5.3 | 0 |
| Mitral valve regurgitation | ||
| Mild (%) | 36.8 | 15.4 |
| Moderate (%) | 15.2 | 0 |
| Severe (%) | 4.2 | 0 |
| Tricuspid regurgitation (≥40 mmHg) (%) | 20.4 | 0 |
| Chest X-ray performed (%) | 79.7 | 62.8 |
| Pulmonary congestion (%) | 43.7 | 0 |
| Creatinine (umol/L); median | 106 | 106 |
| Follow-up in HFC/OPC (%) | 56.2 | 1.7 |
| Medical treatment | ||
| ACE-inhibitor/AII-antagonist (%) | 78.6 | 33.9 |
| Beta-blocker (%) | 67.5 | 28.9 |
| Spironolactone (%) | 32.7 | 5.8 |
| Readmission (12 months)% | 54.6 | 37.2 |
| H F (%) | 13.8 | 0 |
| AMI (%) | 3.5 | 0 |
| Angina pectoris (%) | 5.0 | 3.3 |
| Stroke (%) | 2.7 | 1.7 |
| Atrial fibrillation (%) | 2.7 | 2.5 |
Abbreviations: ACE, angiotensin-converting enzyme; AMI, acute myocardial infarction; BMI, body mass index; COPD, chronic obstructive pulmonary disease; IHD, ischemic heart disease; HF, heart failure; HFC, heart failure clinic; LVEF, left ventricular ejection fraction; OPC, outpatient clinic.
Patients with DHF were older (P < 0.001) and were more often men (DIF 16.6%; 95% CI: 6.9–26.1); they more often had a history of ischemic heart disease (DIF 26.1%; 95% CI: 16.8–34.8) and atrial fibrillation (DIF 28.6%; 95% CI: 20.1–36.1), and their body mass index (BMI) was lower (P = 0.002). Patients with DHF were more often examined with ECG (DIF 6.1%; 95% CI: 1.4–11.8) and echocardiography (DIF 17.4; 95% CI: 10.2–25.4), and they more often showed signs of hypertrophy (DIF 9.6%; 95% CI: 2.3–15.7) and ischemia (DIF 28.7%; 95% CI: 19.0–37.6) on the ECG, and had a lower LVEF (P < 0.001). A greater proportion of HF patients were followed in the HFC or OPC (DIF 54.5%; 95% CI: 49.0–58.5). A greater proportion of patients with DHF were more often treated with ace-inhibitors and angiotensine II receptor blockers (DIF 44.8%; 95% CI: 35.4–53.4), beta-blockers (DIF 38.6%; 95% CI: 29.4–47.0), and spironolactone (DIF 26.9%; 95% CI: 20.5–31.9). Only a few of the NHF patients were readmitted to hospital during the 12 months period after discharge (Table 1).
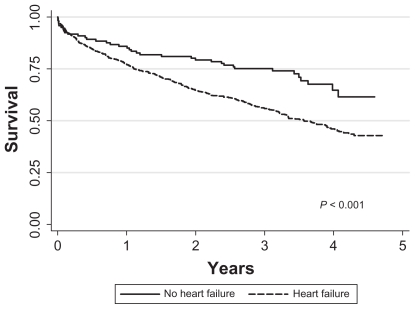
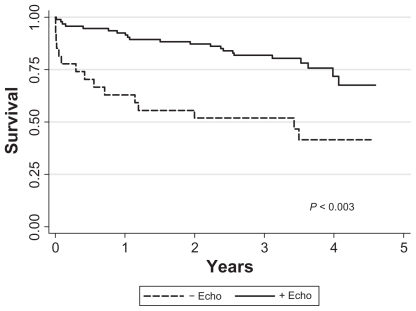
The median follow-up time for survival was 2.9 years. Survival rate among patients with DHF was 0.41 (95% CI: 0.36–0.46) compared to 0.61 (95% CI: 0.46–0.72) among NHF patients (P < 0.001) (Figure 1). Restriction of survival analysis to NHF patients depending on echocardiographic examinations revealed a significant lower survival rate of 0.41 (95% CI: 0.21–0.60) among patients without echocardiography compared to patients with echocardiography who had a survival rate of 0.66 (95% CI: 0.47–0.80) with a dramatic decline in survival during the initial phase of the follow-up period (Figure 2).
Figure 1.
Kaplan–Meier plot of survival in patients with a discharge diagnosis of heart failure (HF) in accordance with criteria from the European Society of Cardiology (ESC) and patients with a discharge diagnosis of heart failure but without fulfilling the ESC criteria for HF.
Figure 2.
Kaplan–Meier survival plot of patients classified as having no heart failure in relation to if echocardiography was performed.
Discussion
We found a PPV of coding for HF among patients admitted to a University Hospital cardiac care unit of 84%. One study found a lower PPV (65.1%).8 However, several other studies found similar or higher PPV compared to our study.4–5,7–9 Differences in validity of HF discharge diagnoses reflect the fact that HF is a complex syndrome with clinical criteria that are less clear-cut compared to other diagnoses.
Almost 15% of the patients were diagnosed in the NRP as having HF without fulfilling the ESC criteria for HF. About one quarter of the patients diagnosed in the NRP as having HF were not examined by echocardiography and did not have any objective signs of dysfunction of the heart. Since these patients did not completely meet the ESC criteria for HF we classified the patients as having NHF. Although these patients in the NRP were classified as having HF none of these patients were followed in the OPC or HFC, fewer were treated with HF medication, fewer were readmitted during the 12-month period after discharge and their survival rate was significantly higher. However, a stratified analysis of NRP-HF patients without ESC-HF divided in groups with and without echocardiography performed revealed a significant lower survival rate among patients without echocardiography compared to patients who were examined by echocardiography. These findings indicate that the patients without echocardiography performed, were probably correctly classified as having HF although they did not have objective signs of cardiac dysfunction.
It was not possible to explore why some of the patients were not examined by an echocardiography. Symptoms and signs are important as they alert the observer to the possibility that heart failure exists. The clinical suspicion of heart failure must be confirmed by objective tests particularly aimed at assessing cardiac function and aetiology to HF and to direct treatment strategy. Confirmation by echocardiography of the diagnosis of HF is mandatory and should be performed shortly following suspicion of the diagnosis of HF.2 The rapid and dramatic decline in survival in the initial phase of the course among patients without echocardiography could indicate that some of the patients failed to get the examination due to early death. Whether the causes of death were related to cardiac disease or comorbidities is unknown.
Our findings may suggest that the use of hospital discharge registers might overestimate admissions for HF and the total burden of the disease. However, this study of admissions with hospitalization due to HF is only able to identify correctly coded cases and false-positive cases. We were not able to identify the false-negative cases in our department. A high specificity of the diagnosis of HF and low sensitivity values and signs of underestimation of the diagnosis of HF in administrative registries has been found in other studies.5–9 Since the codes underreport the magnitude of HF, discharge coding for HF is not suitable for use in studies of prevalence and incidence of HF.5
Our results have important implications. We found a relatively high PPV of the HF diagnosis in the NRP and the NRP can therefore be a valuable tool for identification of patients with HF. However, using the NRP alone will not give a true picture of the cost and total burden of the disease.
Certain limitations exist in this study of heart failure discharge diagnosis. First, our cohort was a group of patients admitted to a cardiac care unit. Others have shown variability in accuracy of a code for HF within different hospital departments, and therefore our results may not be representative for all patients admitted with suspicion of HF.5,7 Second, our study of a historic cohort is retrospective in nature and in some cases characterized by inadequate descriptions of symptoms and signs in the medical records. This might in some case have induced misclassification of the patients. Third, the echocardiographic examinations have mainly focussed on systolic cardiac function and valvular heart diseases. Diastolic parameters were not measured routinely and it could not be excluded that some of the patients classified as having no HF might have suffered diastolic dysfunction and therefore were misclassified.
Conclusion
Medical registries such as NRP are important tools in epidemiological and clinical research. We found a relatively high predictive value and therefore NRP can be a valuable tool for identification of patients with HF. However, a relatively large number of the patients were registered in the NRP as having HF without meeting the ESC criteria for HF. These patients were among others characterized by a better survival, a lower readmission rate, none were followed in the OPC, and they had a lower consumption of anticongestive medicine indicating that the NRP can not give a reliable picture of total burden and costs of the disease.
Footnotes
Disclosure
No conflicts of interest were declared in relation to this paper.
References
- 1.Swedberg K, Cleland J, Dargie H, et al. Guidelines for the diagnosis and treatment of chronic heart failure: executive summary (update 2005): The Task Force for the Diagnosis and Treatment of Chronic Heart Failure of the European Society of Cardiology. Eur Heart J. 2005;26(11):1115–1140. doi: 10.1093/eurheartj/ehi204. [DOI] [PubMed] [Google Scholar]
- 2.Dickstein K, Cohen-Solal A, Filippatos G, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: The Task Force for Diagnosis and Treatment of Acute and Chronic heart Failure 2008 of the European Society of Cardiology. Eur J Heart Fail. 2008:933–989. doi: 10.1016/j.ejheart.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 3.Mosterd A, Hoes AW. Clinical epidemiology of heart failure. Heart. 2007;93:1137–1146. doi: 10.1136/hrt.2003.025270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fonseca C, Sarmento PM, Marques F, Ceia F. Validity of a discharge diagnosis of heart failure: Implication of misdiagnosing. Congest Heart Fail. 2008;14:187–191. doi: 10.1111/j.1751-7133.2008.07752.x. [DOI] [PubMed] [Google Scholar]
- 5.Kümler T, Gislason GH, Kirk V, et al. Accuracy of a heart failure diagnosis in administrative registers. Eur J Heart Fail. 2008;10:658–660. doi: 10.1016/j.ejheart.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 6.Khand AU, Shaw M, Gemmel I, Cleland JGF. Do discharge codes underestimate hospitalisation due to heart failure? Validation study of hospital discharge coding for heart failure. Eur J Heart Fail. 2005;7:792–797. doi: 10.1016/j.ejheart.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 7.Ingelsson E, Ärnlöv J, Sundström J, Lind L. The validity of a diagnosis of heart failure in a hospital discharge register. Eur J Heart Fail. 2005;7:787–791. doi: 10.1016/j.ejheart.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 8.Austin PC, Daly PA, Tu JV. A multicenter study of the coding accuracy of hospital discharge administrative data for patients admitted to cardiac care units in Ontario. Am Heart J. 2002;144:290–296. doi: 10.1067/mhj.2002.123839. [DOI] [PubMed] [Google Scholar]
- 9.Lee DS, Donovan L, Austin P, et al. Comparison of coding of heart failure and comorbidities in administrative and clinical data for use in outcome research. Med Care. 2005;43:182–188. doi: 10.1097/00005650-200502000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Andersen TF, Madsen M, Jørgensen J, Mellemkjoer L, Olsen JH. The Danish National Hospital Register: A valuable source of data for modern health sciences. Dan Med Bull. 1999;46(3):263–268. [PubMed] [Google Scholar]