Abstract
Objective
To determine if trunk muscle attributes are associated with balance and mobility performance among mobility-limited older adults.
Design
Cross-sectional analysis of data from a randomized clinical trial.
Setting
Outpatient rehabilitation research center.
Participants
Community-dwelling older adults (N=70; mean age 75.9 y) with mobility limitations as defined by the Short Physical Performance Battery (SPPB).
Methods
Independent variables included physiologic measures of trunk extension strength, trunk flexion strength, trunk extension endurance, trunk extension endurance and leg press strength. All measures were well tolerated by the study subjects without the occurrence of any associated injuries or adverse events. The association of each physiologic measure with each outcome was examined, using separate multivariate models to calculate the partial variance (R2) of each trunk and extremity measure.
Main Outcome Measurements
Balance measured by the Berg Balance Scale (BBS) and Unipedal Stance Test (UST), and mobility performance as measured by the SPPB.
Results
Trunk extension endurance (partial R2=.14, p=.02), and leg press strength (partial R2=.14, p=.003) accounted for the greatest amount of the variance in SPPB performance. Trunk extension endurance (partial R2=.17, p=.007), accounted for the greatest amount of the variance in BBS performance. Trunk extension strength (R2=.09, p=.03), accounted for the greatest amount of the variance in UST performance. The variance explained by trunk extension endurance equaled or exceeded the variance explained by limb strength across all three performance outcomes.
Conclusions
Trunk endurance and strength can be safely measured in mobility-limited older adults, and are associated with both balance and mobility performance. Trunk endurance and trunk strength are physiologic attributes worthy of targeting in the rehabilitative care of mobility-limited older adults.
Keywords: Aged, Balance, Core, Impairments, Mobility, Rehabilitation, Trunk
Introduction
Mobility limitations affect over 25% of older adults, and are highly predictive of subsequent institutionalization, disability, and mortality.1–4 Balance problems are associated with risk of falls and fall related injury in older adults.5–7 The identification of impairments that are both relevant to functional decline and correctible through rehabilitative care are important goals of disability and falls research.8 Among older adults, associations between limb impairments and both mobility and balance are well established9, 10. Limb impairments are commonly the target of intervention studies for the treatment of balance and mobility problems.11 In contrast, the importance of trunk impairments such as decreased trunk strength or endurance is less clear. Therefore, it is not surprising that trunk muscle exercise is not prioritized by nationally advocated exercise programs.12
However, some studies have suggested a unique link between trunk muscle composition and both balance and mobility.13, 14 Among older adults, poor trunk muscle composition, as manifested by a higher degree of fat infiltration, is associated with both balance and mobility decline even after controlling for deficiencies in leg muscle composition13, 14. Impairments in trunk muscle attributes, such as decreased trunk strength or endurance, are a likely pathway by which these pathophysiologic changes influence balance and mobility status.
Among young adults, trunk impairments have been theorized to be closely linked to athletic performance15, 16. The authors hypothesized that trunk muscle attributes would be closely linked to both mobility and balance performance among older adults with poor mobility performance. To test this hypothesis, a cross-sectional analysis of a cohort of mobility-limited community-dwelling older adults participating in a clinical trial on the benefits of exercise training was conducted.
Methods
This study was an analysis of data collected as part of the InVEST (Increased Velocity Exercise Specific to Task) study, a single-blinded randomized controlled trial evaluating the benefits of two forms of exercise among community-dwelling, mobility limited older adults.17 The InVEST study was conducted at two outpatient rehabilitation centers in the greater Boston area (Hebrew SeniorLife, Roslindale, MA; Spaulding Cambridge Outpatient Center, Cambridge MA). The trunk measures utilized in this study were collected as part of an ancillary investigation conducted at the Cambridge site. Therefore, only the 70 individuals recruited at the Cambridge site were included in this investigation. The Institutional Review Board of Spaulding Rehabilitation Hospital approved the conduct of this study. The study methods have been detailed elsewhere9, but relevant aspects of the study will be summarized below.
Conceptual Model of Disablement
The conceptual model used in this study was characterized by Verbrugge and Jette18. This model of the disablement process describes a pathway proceeding from ‘pathology’ (diagnoses of disease, injury, or congenital/developmental condition) to ‘impairment’ (dysfunctions or structural abnormalities in specific body systems, including the musculoskeletal system) to ‘functional limitations’ (restrictions in basic physical or mental actions) to ‘disability’ (difficulty doing activities of daily life, or fulfilling societal roles). The Verbrugge model of disablement is based on the Nagi model19, which describes a closely related pathway proceeding from ‘active pathology’ (interruption or interference with normal processes) to ‘impairment’ (anatomical, physiological, mental, or emotional abnormality) to ‘functional limitation’ (limitation in performance at the level of the whole organism) to ‘disability’ (limitation in performance of socially defined roles and tasks within a sociocultural and physical environment). Within the conceptual framework of the disablement process, increased trunk muscle fat infiltration would constitute a pathophysiologic change, poor trunk muscle strength or endurance would constitute an impairment, and mobility limitations would constitute a functional limitation. The analyses performed in this study are concerned solely with the associations between trunk and limb impairments and functional limitations in older adults. Since accepted thresholds of normal for trunk and limb muscle strength and endurance do not exist, we will use the term trunk muscle attributes to refer to the range of strength and endurance over which impairment may occur.
Recruitment and Screening Process
Initially, 590 inquiries were solicited via advertising in newspapers, direct mailings, referrals from primary care providers and telephone screenings. These inquiries identified 260 potentially eligible subjects, who attended an initial screening assessment. Participants included in the study were community-dwelling older adults (age ≥ 65) with Short Physical Performance Battery (SPPB) scores between 4 and 10 who were able to climb a flight of stairs independently or while using an assistive device (e.g., cane). We used an upper threshold of 10 on the SPPB to ensure that our study subjects did indeed manifest mobility limitations, but also utilized a lower threshold of 4 to ensure they were not disabled and were physically able to undergo our extensive physical performance testing.
Exclusion criteria were unstable acute or chronic disease (e.g., abdominal aortic aneurysm, exertional angina, history of ventricular fibrillation, symptomatic valvular heart disease or uncontrolled diabetes), a score of less than 23 on the Folstein Mini-Mental State Examination20, a neuromuscular impairment limiting participation in further performance testing or participation in a resistance training program, and a submaximal treadmill exercise tolerance test (ETT) with positive findings for unstable cardiovascular disease.
After providing informed consent, participants underwent a comprehensive history and physical examination conducted by the study principal investigator (JFB), who is physiatrist with expertise in geriatric care. Of the 260 potentially eligible participants who attended an initial screening, 92 (35%) people could not participate in the study due to exclusion criteria, and 30 (11%) chose not to commit to the study, leaving 138 subjects. The first 68 subjects were recruited at the Roslindale site and completed the parent study before this ancillary investigation was initiated. Therefore, they were not included in this analysis. Testing was completed over 1–2 subsequent visits, depending on subject availability. If two visits were required, they were scheduled within one week of each other.
Limb and Trunk Attribute Measures
All 70 participants underwent baseline testing for leg press strength. Due to delays in equipment availability, trunk attribute testing was initiated after inception of the study. Therefore, 63 and 62 subjects underwent trunk extension and flexion endurance testing respectively, while 48 and 46 subjects underwent trunk extension and flexion strength testing respectively. No subject developed low back pain (LBP) or any other musculoskeletal injury as a result of testing.
Lower extremity strength was measured as the double leg press one repetition maximum (1RM) on customized leg press machines (Keiser Pneumatic Leg Press; Fresno, CA) as previously described9. The 1RM is a reliable and valid measurement of strength21. The 1RM is measured by progressively increasing resistance for successive repetitions until the subject can no longer move the lever arm through the full range of motion while maintaining proper form22. The highest resistance at which a full repetition could be completed is measured as the 1RM and recorded in Newtons.
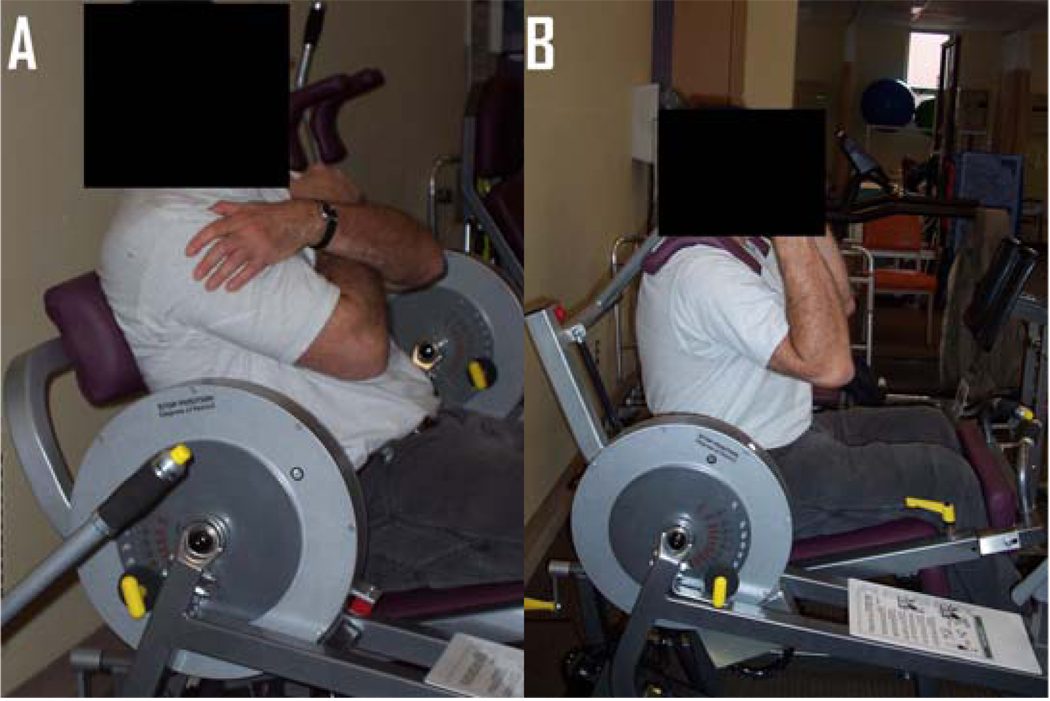
Trunk extension and flexion strength have been validated previously as measures for evaluating strength-function relationships among older adults 23, 24. Measures of trunk strength testing are illustrated in Figure 1. Trunk strength was measured as the 1RM on customized flexion and trunk extension machines (Keiser Sports Health Equipment Inc.; Fresno, CA), using similar methods to those used for leg strength. Each participant’s 1RM was determined within 6–12 repetitions in which resistance is incrementally progressed until the participant could no longer move the lever arm through the full range of motion. Trunk strength was recorded in Newtons. Subjects sat on both trunk strength testing machines in an upright position with 90 degrees of hip flexion and the knees also flexed and locked in place by a padded knee support. Trunk extension strength is measured by extending the spine against a lever arm positioned at the lumbar spine and trunk flexor strength is measured by a lever arm that is positioned over the shoulders and held down with the arms. For both methods of testing and safety, the testing range was limited to only 15 degrees of motion, centered on the initial resting position. For both flexion and extension, the participant initiated motion at 5 degrees behind the neutral position, and ended motion at a maximum excursion of 10 degrees beyond neutral.
Figure 1. Participant performing trunk extension strength and trunk flexion strength measures.
A) Trunk extension strength measure.
B) Trunk flexion strength measure.
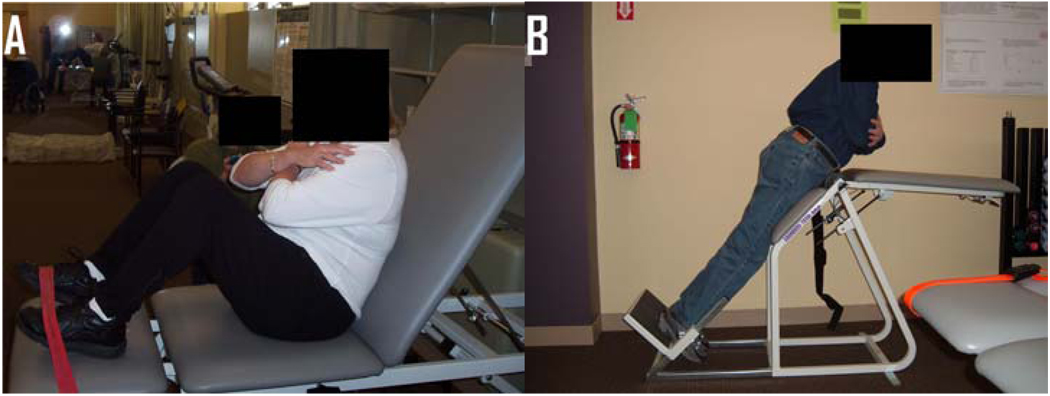
Trunk muscle endurance measures have been previously validated by McGill and colleagues, and have excellent reliability (r=.93–.99)25. To ensure safety of testing among older adults, a modified version of trunk extension testing from that which McGill originally described was used. Our test-retest reliability of trunk endurance testing among mobility limited older adults is excellent (r= .88–.91). Reliability was determined prior to initiating this ancillary study. Measures of trunk endurance testing are illustrated in Figure 2.
Figure 2. Participant performing trunk flexion endurance and trunk extension endurance measures.
A) Participant performing trunk flexion endurance measure. The pad has been removed.
B) Participant performing trunk extension endurance measure. The participant is not supporting the upper body on the plinth.
To measure trunk flexion endurance, each subject was seated in a semi-reclined position, on a horizontal exam table. Hips and knees were flexed to 90 degrees, and feet were supported and fixed in place on the table surface by a strap fixed to the table. The subject’s back rested against a 5 cm-deep firm pad that was positioned between the back and the exam table’s back support, which was positioned 30 degrees from vertical. Arms were held across the chest, with hands on opposite shoulders. When the subject was ready, the pad was slid out, while the subject was asked to maintain the position, unsupported, for as long as possible. Subjects were cued to maintain the original spine position. The test was terminated if the subject could no longer maintain the unsupported position, and this time was recorded in seconds up to 240 seconds, or 4 minutes.
To measure trunk extension endurance, each subject lay prone on a specialized plinth positioned 45 degrees from vertical. The subject’s feet were supported on a footplate, which was positioned such that the hips were even with the hinged portion of the table. A cushioned belt strap attached to the table was fastened around the subject’s pelvis. Subjects began testing with the torso portion of the table fixed at a horizontal position and the lower body portion of the table fixed at 45 degrees from horizontal. At rest, subjects were instructed to rest their arms on the torso portion of the table. When the subjects were ready, they were asked to raise their arms and fold them across their chest while maintaining their head and trunk position in line with their lower body. In this way when viewed from the side, the subject’s head, trunk and legs are in a straight line positioned 45 degrees from vertical. Subjects were asked to maintain this position, unsupported, for as long as possible. The test was terminated when the subject could no longer maintain the unsupported position, and this time was recorded in seconds. For both modes of trunk endurance testing subjects were encouraged during testing to avoid flexing or extending beyond a neutral alignment between the head, trunk and pelvis.
Outcome measures
Mobility performance and balance was measured for all 70 participants. Mobility was measured using the Short Physical Performance Battery (SPPB)26. The SPPB involves a timed assessment of standing balance, usual 4.0-m walk pace, and five repetitions of rising from a chair and sitting down. All times are measured to the nearest 0.01 second by using a stopwatch. Each test is scored between 0 and 4 and summed, for a total score ranging from 0 (low performance) to 12 (high performance). The SPPB is a reliable measure that captures a wide range of functional abilities. Summary scores are predictive of both activities of daily living (ADL) and mobility related disability, as well as mortality among both healthy and disabled older adults 3, 26. The SPPB was measured on two occasions during the baseline assessment, and the average of the two scores was used in this analysis.
Two measures of balance were performed, including the Berg Balance Scale (BBS) and the Unipedal Stance Time (UST). The BBS has demonstrated reliability and validity as a measure of dynamic balance5, 27–29. This commonly used composite balance test requires the patient to complete 14 tasks that are scored on a scale of 0 (unable to perform) to 4 (normal performance), with a maximum score of 56. The BBS includes normal functional activities such as sitting, standing, and leaning over5. The UST is a reliable and valid test of static balance that is a predictor of falls in older adults6, 7, 30. The UST measures the length of time that a person is able to maintain balance while standing on one leg. The single leg support time is measured to the nearest 0.01 second by using a stopwatch. The BBS was included because it is perhaps the most well-established fall-related balance scale in the literature. The UST was included because it is a component of the BBS which on its own represents a simple, clinically feasible balance test that is associated with falls.
Adjustment variables
Adjustment variables which were considered for inclusion in the final multivariate models included age, gender, height, weight, body mass index (BMI) and the number of active medical conditions. Standing height was measured in centimeters using a stadiometer. Weight was measured in kilograms using a calibrated scale. BMI was calculated by the formula: weight (kg)/height (m2). The examining physician recorded the total number of active medical conditions for each subject at the completion of the physical examination. Active medical conditions were defined as: (1) any condition for which a participant was currently receiving treatment, or (2) a condition requiring medical treatment within the past year. Medical records were requested from participants’ primary care physicians to corroborate these findings. The total number of active medical conditions at baseline was recorded for each subject.
Statistical Analysis
The following calculations were used to characterize the sample: means and standard deviations for continuous variables, and frequencies and proportions for categorical variables. Each variable was examined using descriptive statistics and graphic plots, applying log transformations for continuous predictors that were highly skewed. Both trunk endurance measures had skewed distributions and were therefore log transformed for statistical modeling. Simple correlations were determined between the limb and trunk attributes and the outcomes using Pearson correlation coefficients. Next, 15 separate multivariate linear regression models were created including each of the five limb and trunk attributes with each of the 3 outcome variables. Recognizing the limited sample size and the desire to use the same adjustment variables for all 15 models, adjustment variables for the final models were determined through an iterative process. For each outcome, successive models were evaluated using a maximum of 3 adjustment variables due to sample size limitations. The 3 adjustment variables chosen for the final models were those that were most consistently statistically significant among the respective models, had the least amount of covariance with each other and had the most meaningful influence on the total variance described by the resulting model. This method of selection of variables to be used in multivariate analyses has been well described.31 Statistical significance was determined if p-levels were <.05. All analyses were performed using SAS software, version 9.0 (SAS Institute., Cary, NC).
Results
Baseline characteristics, trunk and limb measures, and physical performance measures are presented in Table 1. The study population was predominantly female and mildly overweight. Subjects had a mean age ± standard deviation (SD) of 75.9 ± 7.3 years (range 65–94). Average height was 166.1 ± 10.5 cm, average weight was 76.3 ± 16.8 kg, and average body mass index (BMI) was 27.6 ± 5.1. Health status was characterized by a mean of 6.1 ± 2.6 active medical conditions. The mean SPPB was 8.8 ± 1.6. Baseline characteristics of the study sample were not materially different from those of individuals recruited at the Roslindale site of the InVEST study (data not shown), suggesting the absence of bias due to recruitment location.
Table 1.
Baseline Characteristics, Trunk and Extremity Measures, and Performance Measures of the Study Sample (n=70)
| Characteristic | Mean (S.D.) or N (%) | Range |
|---|---|---|
| Female Gender | 67.1% | n/a |
| Age (years) | 75.9 (7.3) | 65–94 |
| Height (cm) | 166.1 (10.5) | 144–190.5 |
| Weight (kg) | 76.3 (16.8) | 46.6–133.5 |
| BMI (ht/kg2) | 27.6 (5.1) | 19.8–41.5 |
| Number of Active Medical Conditions | 6.1 (2.6) | 2–14 |
| SPPB (0–12) | 8.8 (1.6) | 4.5–11 |
| BBS (0–28) | 50.6 (4.9) | 34–56 |
| Unipedal Stance Time (sec.) | 12.6 (17.8) | 0–82.4 |
| Trunk Extension Strength (Newtons) | 598.5 (242.0) | 187–1245 |
| Trunk Flexion Strength (Newtons) | 87.0 (47.2) | 27–334 |
| Trunk Extension Endurance (sec.) | 80.7 (65.6) | 1.3–240.0 |
| Trunk Flexion Endurance (sec.) | 54.0 (64.7) | 1.2–240.0 |
| Leg Press Strength (Newtons) | 1912 (658.0) | 881.0–3452.0 |
SPPB: Short Physical Performance Battery
BBS: Berg Balance Score
Correlations between physical performance measures are presented in Table 2. Significant (p<0.05) moderate to strong correlations were found for the association of trunk extension strength with leg press strength (r=.72), the association of trunk extension strength with trunk flexion strength (r=.52), and the association of trunk flexion strength with leg press strength (r=.37)32.
Table 2.
Associations of Trunk Measures, Extremity Measures and Performance Measures Using Pearson Correlation Coefficients*
| R | ExtSTR | FlexSTR | ExtEND | FlexEND | LegSTR | SPPB | BBS | UST |
|---|---|---|---|---|---|---|---|---|
| ExtSTR | 1.0 | .52* | .27 | .01 | .72* | .27 | .27 | .30* |
| FlexSTR | 1.0 | .26 | .18 | .36* | .24 | .15 | .20 | |
| ExtEND | 1.0 | .27* | .29* | .37* | .41* | .24 | ||
| FlexEND | 1.0 | .11 | .19 | .13 | .17 | |||
| LegSTR | 1.0 | .36* | .28* | .18 | ||||
| SPPB | 1.0 | .74* | .52* | |||||
| BBS | 1.0 | .64* | ||||||
| UST | 1.0 |
statistically significant p value <.05
ExtSTR: Trunk extension strength (Newtons)
FlexSTR: Trunk flexion strength (Newtons)
ExtEND: Log transformed Trunk Extension Endurance Test (sec)
FlexEND: Log transformed Trunk Flexion Test (sec)
LegSTR: Leg Press Strength (Newtons)
SPPB: Short Physical Performance Battery
BBS: Berg Balance Score
UST: Unipedal Stance Test
In examining bivariate associations between trunk and limb measures and physical performance measures, moderate correlations were found for the association of trunk extension strength with UST (r=.30). Trunk extension endurance was moderately correlated with SPPB (r=.37) and BBS (r=.41). Leg press strength was moderately correlated with SPBB (r=.36) and somewhat correlated with BBS (r=.28). In examining associations between performance outcomes, strong associations were found between BBS and both SPBB (r=.74) and UST (r=.64). Moderate associations were found between SPPB and UST (r=.52)
Table 3 presents the final multivariate models evaluating the association between each trunk or limb measure and the outcomes. All final models were statistically significant predictors of the outcomes (p≤.01). Age, gender, and BMI met criteria for inclusion as the adjustment variables for our final models. Height, weight, and number of active medical conditions were not found to be significant adjustment variables, and were excluded from the final multivariate models. Trunk extension strength (partial R2=.07, p=.01), trunk extension endurance (partial R2=.14, p=.02), and leg press strength (partial R2=.14, p=.003) were individual predictors significantly associated with SPPB performance. Trunk extension strength (partial R2=.07, p=.03), trunk extension endurance (partial R2=.17, p=.007), and leg press strength (R2=.10, p=.01) were also significantly associated with BBS score. Trunk extension strength was the only impairment which was significantly associated with performance on the UST (R2=.09, p=.03). Trunk extension endurance (R2=.06, p=.24) and leg press strength (R2=.05, p=.13) showed nonsignificant associations with performance on the UST.
Table 3.
Separate Multivariate Linear Models of Associations Between Trunk and Extremity Measures, and Mobility and Balance Performance*
| Outcome | Predictor | N | Parameter Estimate |
Estimate Significance |
Partial R2 | Model R2 |
|---|---|---|---|---|---|---|
| SPPB | ExtSTR | 48 | .004 | .01 | .07 | .32 |
| FlexSTR | 46 | .009 | .12 | .06 | .26 | |
| ExtEND | 63 | .34 | .02 | .14 | .33 | |
| FlexEND | 62 | .25 | .15 | .04 | .28 | |
| LegSTR | 70 | .001 | .003 | .14 | .29 | |
| BBS | ExtSTR | 48 | .01 | .03 | .07 | .38 |
| FlexSTR | 46 | .01 | .56 | .02 | .23 | |
| ExtEND | 63 | 1.26 | .007 | .17 | .47 | |
| FlexEND | 62 | .21 | .72 | .02 | .42 | |
| LegSTR | 70 | .003 | .01 | .10 | .37 | |
| UST | ExtSTR | 47 | .02 | .03 | .09 | .34 |
| FlexSTR | 45 | .04 | .26 | .04 | .25 | |
| ExtEND | 62 | 1.27 | .24 | .06 | .26 | |
| FlexEND | 61 | 1.89 | .12 | .03 | .26 | |
| LegSTR | 70 | .004 | .13 | .05 | .25 |
SPPB: Short Physical Performance Battery
UST: Unipedal Stance Test
BBS: Berg Balance Score
ExtSTR: Trunk extension strength (Newtons)
FlexSTR: Trunk flexion strength (Newtons)
ExtEND: Log transformed Trunk Extension Endurance Test (sec)
FlexEND: Log transformed Trunk Flexion Test (sec)
LegSTR: Leg Press Strength (Newtons)
All models adjusted for age, gender and BMI
Discussion
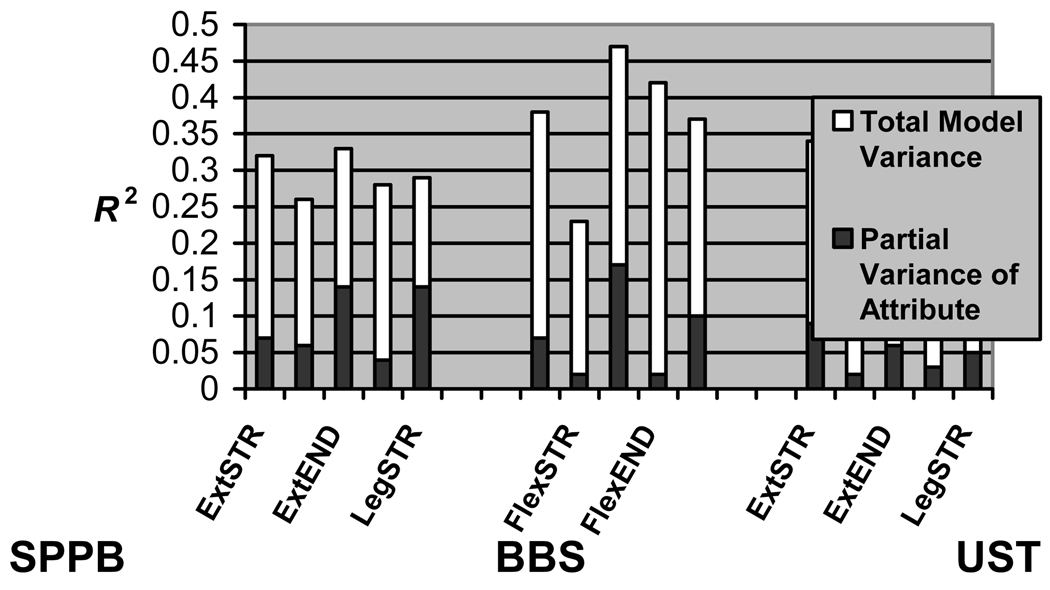
The most important finding of the present study is that trunk extension endurance and strength are associated with mobility and balance in older adults. Variance (R2) is a statistical term which may be used to describe the amount of variation in an outcome explained by a statistical model or independent variable. Model R2 values reflect the amount of variation described by all trunk or limb measures and covariates within a multivariate model. Partial R2 values are a reflection of the amount of variation attributed to a variable within the larger model. By observing the partial R2, the reader can better understand the portion of variation described by a trunk or limb measure in the context of the larger multivariate model. Prior studies examining the effects of physiologic attributes on performance have considered partial variances ranging from .05–.20 as statistically meaningful33. In this study, the authors found that trunk extension endurance (partial R2=.06–.17) explained as much or more of the variance in all performance outcomes, as compared to leg press strength (partial R2=.05–.14). In addition, trunk extension strength was significantly associated with all performance outcomes (partial R2=.07–.09). All measures were well tolerated by the study subjects, without the occurrence of associated injuries or adverse events, demonstrating that measures of trunk endurance and trunk strength can be safely measured in mobility limited older adults using simple equipment and protocols. In particular, this method of measuring trunk extension endurance may be quite easily administered in a clinical setting.
When viewed in the context of prior work, this study contributes to our understanding of the connection between trunk muscle pathoanatomy, trunk impairments, and functional limitations in older adults. A prior study by Sakari-Rantala et al. found significant associations between isometric trunk extension strength and mobility performance among a healthy elderly cohort.34 McGill et. al25 have instead emphasized the relative importance of trunk endurance, which is consistent with the findings in this study. More recent work by Hicks et al. 13, 14 reported that the pathoanatomical change of increased trunk muscle fat infiltration was associated with functional limitations in older adults, independent of limb muscle fat infiltration. Trunk muscle fat infiltration explained a relatively greater proportion of the variance in physical function as compared to limb muscle fat infiltration. Although this relationship was seen irrespective of LBP status, Hicks et al. demonstrated an association between severity of LBP and functional limitations that was graded by severity of LBP. They proposed that LBP due to deficiencies in spine stability from trunk muscle impairments was an important intermediary explaining the observed relationship between trunk muscle fat infiltration and physical function14. This current study did not focus upon patients with chronic low back pain. Nevertheless, these current findings suggest that trunk impairments may be the likely pathway by which changes in trunk muscle fat infiltration lead to functional limitations in older adults. The influence of LBP status on the association between trunk impairments and mobility limitations is worthy of investigation in a future study.
Relationships between trunk and extremity measures and performance measures are demonstrated in Figure 3, which depicts partial R2 values (dark bars) and total model R2 values (white bars). In most cases, trunk and limb measures with relatively high partial R2 values also had large model R2 values, underscoring the importance of these measures as related to performance outcomes. However, in some instances, two models with comparably large R2 values demonstrated partial R2 values for trunk or limb measures that differed substantially in magnitude. An example of this may be seen in the SPPB models, where total model R2 values were similar for models including trunk extension strength and trunk extension endurance, yet partial R2 values were higher for trunk extension endurance than trunk extension strength. The strength of the observed associations between trunk extension endurance and dynamic performance outcomes (SPPB and BBS), and the association between trunk extension strength and static balance (UST), can be explained mechanistically. The dynamic performance outcomes of SPPB and BBS are composite measures that each contain movement-related tasks, which require a changing base of support in order to ensure stability. In movement-related tasks, and specifically those that involve a component of forward motion in the sagittal plane, involvement of the trunk extensors may be necessary to stabilize the trunk35. During movement-related tasks, limb strength is essential, as reflected by the significance of leg press strength in the models for dynamic performance. The situation may be different in the case of the UST, due to the fact that the UST is a measure of static balance, and does not involve large amplitude movements of the base of support. In the UST, the ability to lock the knee in extension may for some individuals compensate for a degree of knee extension weakness, and may make the contributions of limb strength to balance relatively less important than in dynamic performance outcomes. In addition, much of the motor activity for maintaining balance during UST likely occurs at the ankle. Strength or endurance at this body segment was not measured as part of this study. Nevertheless, due to the position of the lumbar spine posterior to the ground reaction force vector in unipedal standing, activation of trunk extension musculature remains important. A final mechanistic explanation for the significance of trunk extension across all performance outcomes may be the influence of kyphosis in older adults. A kyphotic deformity would require increased activation of trunk extensor musculature in order to maintain stability during standing and ambulation35. Kyphosis has previously been associated with poor balance and mobility36. Because kyphosis was not measured in this study, the authors cannot support or refute this hypothesis. The influence of kyphosis on the association between trunk impairments and mobility limitations is worthy of further study.
Figure 3. Total Variance (R2) in Balance and Mobility Performance Described by Separate Multivariate Linear Regression Models*.
SPPB: Short Physical Performance Battery
BBS: Berg Balance Score
UST: Unipedal Stance Test
ExtSTR: Trunk extension strength (Newtons)
FlexSTR: Trunk flexion strength (Newtons)
ExtEND: Log transformed Trunk Extension Test (sec)
FlexEND: Log transformed Trunk Extension Test (sec)
LegSTR: Leg Press Strength (Newtons)
* All models adjusted for age, gender and BMI
This study has several limitations. First, the cross-sectional design utilized only allows identification of associations and does not permit identification of cause and effect relationships. Mechanistic explanations can only be speculative. Second, although leg press strength testing incorporates the components of strength at the hip and knee, it does not measure strength at the ankle. Ankle strength is an important factor related to both balance and mobility, and inclusion of an ankle strength measure might have altered these findings. Also, by it’s nature, impairment testing does not exclusively isolate the motor groups of interest; that is, leg press strength testing in the manner described above may depend on factors related to trunk strength, and trunk impairment testing as described may depend on aspects of lower limb strength. This may, in part, be reflected in the high level of correlation observed between the respective impairment measures in our study. The interdependence of muscle groups in this manner may also, to some extent, be a limitation of clinical muscle strength testing in general. However, interdependence of muscle groups would be expected, if anything, to bias the findings towards the null, and would not explain the observed differences between models. Future studies may choose to quantify the relative contributions of secondary muscle groups through techniques such as electromyography.
Third, trunk endurance testing in this study demonstrated a high level of variability. Other investigators performing related measures have suggested that normalization for upper body mass may help with decreasing the observed variability37. Normalization for upper body mass in theory would have been expected to decrease standard error and increase the significance of between group differences. This was not done in this current investigation, but would be worth considering in the future. Even so, the fact that significant associations between trunk extension endurance and both SPPB and BBS were observed even without normalization suggests that this mode of testing has merit sufficient to warrant further study.
Fourth, this study is limited by the high level of correlation observed among impairment measures, as well as the small sample size. Because of the high level of correlation, the authors were not able to adequately evaluate the relevance of one impairment measure versus the other in the same statistical model. It is for this reason that they were evaluated in separate models. The authors made a decision to include all available data on physiologic attributes in these models, which led to small variations in sample size across models. Small sample size may have resulted in increased type II error, such as in the case of the non-significant associations between trunk extension endurance, leg press strength, and performance on the UST. However, sample size limitations would not explain the significant associations which were found between trunk and extremity measures and performance measures.
Finally, a limitation of this study is potential bias due to the fact that subjects for this pilot study were older adults volunteering to participate in an exercise trial. These findings should be replicated in a cohort more representative of the population of mobility limited older adults. A future study of a larger and more diverse population would also allow for more thorough evaluation of both impairment-outcome relationships as well as the relevance of other potentially important covariates.
Despite these limitations, this study is one of the first to evaluate the relevance of different trunk measures to mobility status among older adults with underlying balance and mobility problems. These findings build upon the existing literature, and suggest that both trunk endurance and trunk strength may reflect important measures worthy of targeting in the rehabilitative care of mobility-limited older adults.
Acknowledgements
We wish to thank Dr. Manuel Monterro-Mondaso for his assistance with development of the trunk muscle strength and endurance protocols.
Funding sources and related paper presentations
Dr. Suri is funded by the Rehabilitation Medicine Scientist Training K12 Program (RMSTP) and the National Institutes of Health (K12 HD 01097).
Dr. Bean and the project were funded through the Dennis W. Jahnigen Scholars Career Development Award, American Geriatrics Society/Hartford Foundation, a NIH Mentored Clinical Scientist Development Award (K23AG019663-01A2) and by the department of PM&R, Harvard Medical School.
Footnotes
Clinical trials reg. # NCT00158119.
Aspects of this study were presented at the 2008 Annual Assembly of the American Geriatrics Society in Washington, D.C.
References
- 1.Fried LP, Bandeen-Roche K, Chaves PH, Johnson BA. Preclinical mobility disability predicts incident mobility disability in older women. J Gerontol A Biol Sci Med Sci. 2000;55:M43–M52. doi: 10.1093/gerona/55.1.m43. [DOI] [PubMed] [Google Scholar]
- 2.Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55:M221–M231. doi: 10.1093/gerona/55.4.m221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332:556–561. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liao Y, McGee DL, Cao G, Cooper RS. Recent changes in the health status of the older U.S. population: findings from the 1984 and 1994 supplement on aging. J Am Geriatr Soc. 2001;49:443–449. doi: 10.1046/j.1532-5415.2001.49089.x. [DOI] [PubMed] [Google Scholar]
- 5.Berg KO, Wood-Dauphinee SL, Williams JI, Maki B. Measuring balance in the elderly: validation of an instrument. Can J Public Health. 1992;83 Suppl 2:S7–S11. [PubMed] [Google Scholar]
- 6.Hurvitz EA, Richardson JK, Werner RA, Ruhl AM, Dixon MR. Unipedal stance testing as an indicator of fall risk among older outpatients. Arch Phys Med Rehabil. 2000;81:587–591. doi: 10.1016/s0003-9993(00)90039-x. [DOI] [PubMed] [Google Scholar]
- 7.Vellas BJ, Wayne SJ, Romero L, Baumgartner RN, Rubenstein LZ, Garry PJ. One-leg balance is an important predictor of injurious falls in older persons. J Am Geriatr Soc. 1997;45:735–738. doi: 10.1111/j.1532-5415.1997.tb01479.x. [DOI] [PubMed] [Google Scholar]
- 8.Bean JF, Kiely DK, LaRose S, Leveille SG. Which impairments are most associated with high mobility performance in older adults? Implications for a rehabilitation prescription. Arch Phys Med Rehabil. 2008;89:2278–2284. doi: 10.1016/j.apmr.2008.04.029. [DOI] [PubMed] [Google Scholar]
- 9.Mayson DJ, Kiely DK, LaRose SI, Bean JF. Leg strength or velocity of movement: which is more influential on the balance of mobility limited elders? Am J Phys Med Rehabil. 2008;87:969–976. doi: 10.1097/PHM.0b013e31818dfee5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Visser M, Goodpaster BH, Kritchevsky SB, et al. Muscle mass, muscle strength, and muscle fat infiltration as predictors of incident mobility limitations in well-functioning older persons. J Gerontol A Biol Sci Med Sci. 2005;60:324–333. doi: 10.1093/gerona/60.3.324. [DOI] [PubMed] [Google Scholar]
- 11.Bean JF, Vora A, Frontera WR. Benefits of exercise for community-dwelling older adults. Arch Phys Med Rehabil. 2004;85:S31–S42. doi: 10.1016/j.apmr.2004.03.010. quiz S3–4. [DOI] [PubMed] [Google Scholar]
- 12.NIA. Aging NIo. Bethesda: National Institute of Health; 1999. Exercise: A Guide from the National Institute on Aging. [Google Scholar]
- 13.Hicks GE, Simonsick EM, Harris TB, et al. Trunk muscle composition as a predictor of reduced functional capacity in the health, aging and body composition study: the moderating role of back pain. J Gerontol A Biol Sci Med Sci. 2005;60:1420–1424. doi: 10.1093/gerona/60.11.1420. [DOI] [PubMed] [Google Scholar]
- 14.Hicks GE, Simonsick EM, Harris TB, et al. Cross-sectional associations between trunk muscle composition, back pain, and physical function in the health, aging and body composition study. J Gerontol A Biol Sci Med Sci. 2005;60:882–887. doi: 10.1093/gerona/60.7.882. [DOI] [PubMed] [Google Scholar]
- 15.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. The American journal of sports medicine. 2005;33:492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 16.Leetun DT, Ireland ML, Willson JD, Ballantyne BT, Davis IM. Core stability measures as risk factors for lower extremity injury in athletes. Med Sci Sports Exerc. 2004;36:926–934. doi: 10.1249/01.mss.0000128145.75199.c3. [DOI] [PubMed] [Google Scholar]
- 17.Bean J, Kiely DK, LaRose S, O'Neil BS, Goldstein R, Frontera WR. Increased Velocity Exercise Specific to Task (InVEST) training vs. the National Institute on Aging’s (NIA) strength training program: changes in limb power and mobility. 2008 doi: 10.1093/gerona/glp056. In. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. 1994;38:1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- 19.Jette AM. Disablement outcomes in geriatric rehabilitation. Med Care. 1997;35:JS28–JS37. doi: 10.1097/00005650-199706001-00005. discussion JS8–44. [DOI] [PubMed] [Google Scholar]
- 20.Folstein MFFSFM P.R. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 21.Callahan D, Phillips E, Carabello R, Frontera WR, Fielding RA. Assessment of lower extremity muscle power in functionally-limited elders. Aging Clin Exp Res. 2007;19:194–199. doi: 10.1007/BF03324689. [DOI] [PubMed] [Google Scholar]
- 22.Cuoco A, Callahan DM, Sayers S, Frontera WR, Bean J, Fielding RA. Impact of muscle power and force on gait speed in disabled older men and women. J Gerontol A Biol Sci Med Sci. 2004;59:1200–1206. doi: 10.1093/gerona/59.11.1200. [DOI] [PubMed] [Google Scholar]
- 23.Sinaki M, Itoi E, Rogers JW, Bergstralh EJ, Wahner HW. Correlation of back extensor strength with thoracic kyphosis and lumbar lordosis in estrogen-deficient women. Am J Phys Med Rehabil. 1996;75:370–374. doi: 10.1097/00002060-199609000-00013. [DOI] [PubMed] [Google Scholar]
- 24.Sinaki M, Nwaogwugwu NC, Phillips BE, Mokri MP. Effect of gender, age, and anthropometry on axial and appendicular muscle strength. Am J Phys Med Rehabil. 2001;80:330–338. doi: 10.1097/00002060-200105000-00002. [DOI] [PubMed] [Google Scholar]
- 25.McGill SM, Childs A, Liebenson C. Endurance times for low back stabilization exercises: clinical targets for testing and training from a normal database. Arch Phys Med Rehabil. 1999;80:941–944. doi: 10.1016/s0003-9993(99)90087-4. [DOI] [PubMed] [Google Scholar]
- 26.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 27.Berg K, Wood-Dauphinee S, Williams JI. The Balance Scale: reliability assessment with elderly residents and patients with an acute stroke. Scand J Rehabil Med. 1995;27:27–36. [PubMed] [Google Scholar]
- 28.Cipriany-Dacko LM, Innerst D, Johannsen J, Rude V. Interrater reliability of the Tinetti Balance Scores in novice and experienced physical therapy clinicians. Arch Phys Med Rehabil. 1997;78:1160–1164. doi: 10.1016/s0003-9993(97)90145-3. [DOI] [PubMed] [Google Scholar]
- 29.Holbein-Jenny MA, Billek-Sawhney B, Beckman E, Smith T. Balance in personal care home residents: a comparison of the Berg Balance Scale, the Multi-Directional Reach Test, and the Activities-Specific Balance Confidence Scale. J Geriatr Phys Ther. 2005;28:48–53. [PubMed] [Google Scholar]
- 30.Giorgetti MM, Harris BA, Jette A. Reliability of clinical balance outcome measures in the elderly. Physiother Res Int. 1998;3:274–283. doi: 10.1002/pri.150. [DOI] [PubMed] [Google Scholar]
- 31.Sun GW, Shook TL, Kay GL. Inappropriate use of bivariable analysis to screen risk factors for use in multivariable analysis. J Clin Epidemiol. 1996;49:907–916. doi: 10.1016/0895-4356(96)00025-x. [DOI] [PubMed] [Google Scholar]
- 32.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale: Lawrence Erlbaum Associates, Inc.; 1988. [Google Scholar]
- 33.Bean JF, Kiely DK, Herman S, et al. The relationship between leg power and physical performance in mobility-limited older people. J Am Geriatr Soc. 2002;50:461–467. doi: 10.1046/j.1532-5415.2002.50111.x. [DOI] [PubMed] [Google Scholar]
- 34.Sakari-Rantala R, Era P, Rantanen T, Heikkinen E. Associations of sensory-motor functions with poor mobility in 75- and 80-year-old people. Scand J Rehabil Med. 1998;30:121–127. doi: 10.1080/003655098444237. [DOI] [PubMed] [Google Scholar]
- 35.Leteneur S, Gillet C, Sadeghi H, Allard P, Barbier F. Effect of trunk inclination on lower limb joint and lumbar moments in able men during the stance phase of gait. Clin Biomech (Bristol, Avon) 2009;24:190–195. doi: 10.1016/j.clinbiomech.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 36.Balzini L, Vannucchi L, Benvenuti F, et al. Clinical characteristics of flexed posture in elderly women. J Am Geriatr Soc. 2003;51:1419–1426. doi: 10.1046/j.1532-5415.2003.51460.x. [DOI] [PubMed] [Google Scholar]
- 37.Clark BC, Manini TM, Ploutz-Snyder LL. Derecruitment of the lumbar musculature with fatiguing trunk extension exercise. Spine. 2003;28:282–287. doi: 10.1097/01.BRS.0000042227.06526.A2. [DOI] [PubMed] [Google Scholar]