Abstract
Background
Health status is a key outcome for comparing treatments, particularly when mortality does not differ significantly.
Methods and Results
BARI 2D randomized 2368 patients with type 2 diabetes and stable ischemic heart disease to 1) prompt revascularization versus medical therapy and 2) insulin sensitization versus insulin provision. Randomization was stratified by the intended method of revascularization, coronary artery bypass graft surgery (CABG) or percutaneous coronary intervention (PCI). The Duke Activity Status Index (DASI) and RAND Energy, Health Distress and Self-rated Health were assessed at study entry and annually thereafter; linear mixed models were used to evaluate the effect of randomized treatment on these measures. Health status improved significantly from baseline to one-year (p<0.001) in each randomized treatment group. Compared with medical therapy, prompt revascularization was associated with significantly greater improvements in DASI (1.32 points, p<0.001), Energy (1.36 points, p=0.02) and Self-rated Health (1.77 points, p=0.007) but not Health Distress (−0.47, p=0.46). These treatment effects were largely maintained over four years of follow-up. The effect of revascularization on DASI was significantly larger in the subgroup of patients intended for CABG compared with the subgroup intended for PCI. Health status did not differ significantly on any of the four measures between the insulin provision and insulin sensitization strategies.
Conclusion
Prompt coronary revascularization was associated with small yet statistically significant improvements in health status compared with initial medical therapy among patients with diabetes and stable ischemic heart disease.
Keywords: coronary disease, diabetes mellitus, revascularization, health status
INTRODUCTION
Treatment of patients with the combination of ischemic heart disease and type 2 diabetes is undertaken to increase the length and the quality of the patient’s life. In prior trials of patients with stable symptoms and mild to moderate coronary disease, revascularization had little impact on the long-term risk of mortality or myocardial infarction but significantly mitigated angina symptoms and improved health status.1,2 It is not known whether the health status benefits seen with revascularization are shared by patients with type 2 diabetes and coronary artery disease. Moreover, there has been no large-scale randomized comparison of health status outcomes by diabetes treatment strategies aimed at insulin sensitization versus insulin provision.
The Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) clinical trial evaluated strategies to treat cardiac ischemia and control hyperglycemia among patients with type 2 diabetes and stable ischemic heart disease. As previously reported,3 mortality and major cardiovascular events were similar over five years for patients randomly assigned to insulin sensitization versus insulin provision and were also similar for those assigned to a strategy of prompt revascularization with intensive medical therapy versus intensive medical therapy alone. Among patients intended for CABG, prompt revascularization was associated with significantly lower rates of major cardiovascular events compared with intensive medical therapy, largely due to a reduction in the rate of documented myocardial infarction.3
In addition to comparing the effect of the randomized treatments on total mortality and major cardiovascular events, the BARI 2D trial was designed to assess the effect of treatment strategies on health status. This paper presents the health status outcomes by the assigned treatment strategies.
METHODS
The design, patient characteristics and primary results of the BARI 2D clinical trial have been described in detail.3–9 In brief, 2368 patients with type 2 diabetes mellitus and angiographically documented stable ischemic heart disease were enrolled from 49 clinical sites in 6 countries. Patients had at least one coronary lesion with ≥ 50% stenosis appropriate for elective revascularization and were excluded if they required immediate coronary revascularization, had left main disease, coronary revascularization within the previous 12 months, HbA1c level > 13.0%, or serum creatinine > 2.0 mg/dl. In a 2-by-2 factorial design, patients were randomly assigned to 1) a glycemic control strategy consisting of either insulin sensitization (IS) or insulin provision (IP) to achieve a target HbA1c < 7.0%, and 2) a myocardial ischemia management strategy consisting of either prompt coronary revascularization with intensive medical therapy (REV) or intensive medical therapy with revascularization used only to control progressive or unstable symptoms (MED). Prior to randomization, the enrolling cardiologist determined whether CABG or PCI was more suitable based on the patient’s coronary anatomy and clinical profile, and the randomization was stratified by the intended method of revascularization (CABG or PCI).4 The insulin sensitization strategy involved use of metformin, a thiazolidinedione or both while the insulin provision strategy relied on sulfonylurea, insulin or both.6 By protocol, all BARI 2D patients received intensive medical therapy to treat cardiac risk factors including hypertension, dyslipidemia, obesity and smoking.7 Clinic visits occurred on a monthly basis for the first 6 months and quarterly thereafter. BARI 2D was approved by the Internal Review Board at the coordinating center and each clinical site, and all participants gave informed consent.
Randomized patients completed self-administered questionnaires to evaluate health status at study entry and at annual intervals during follow-up. The primary health status domains were the Duke Activity Status Index (DASI)10, and the modified RAND instruments Energy/Fatigue, Health Distress and Self-rated Health.11,12 DASI is a 12-item index [0 (worst) – 58.2 (best)] that assesses the activities that one can do without difficulty such as walking a block or two on level ground or doing light house work.10 DASI has been correlated with peak oxygen intake10 and has been used to assess physical function in numerous cardiovascular clinical studies.13,14 Energy is a five-item scale [0 (worst) – 100 (best)] that measures the degree that a person has energy and feels full of pep, or alternatively feels tired and worn out, and Health Distress [0 (best) – 100 (worst)] is a four-item scale that assesses the amount of time one feels discouraged, frustrated or worried by their health status. These scales, derived from the RAND Medical Outcomes Study, have been validated and applied in clinical studies that evaluated medical interventions.11,12 Self-rated Health [0 (worst) – 100 (best)] is based on a single-item Likert scale, “In general, would you say your health is: Excellent, Very good, Good, Fair, Poor”.11,12 The smallest possible change for an individual patient is 1.75 points for DASI, 5.0 for Energy, 6.25 for Health Distress, and 25 for Self-rated Health, and between-group differences of 3 points for DASI and 5 points for Energy, Health Distress and Self-rated Health have been considered minimal “clinically meaningful” differences.14–15 In 2005, the Center for Epidemiologic Studies Depression Scale (CES-D), a screening measure that captures the number and severity of depressive symptoms, was added to the annual follow-up questionnaire.16
This analysis includes patients with at least one follow-up health status measure. Since patients with follow-up data at Years 5 and 6 were predominantly from the few clinical sites that were started enrolling patients early, follow-up information after Year 4 was truncated to minimize patient selection bias.
Statistical Methods
All analyses of treatment were based on the intention-to-treat principle. Baseline patient characteristics were compared by treatment assignment using t-tests and chi-square tests. Trends in longitudinal health-status measures were displayed by plotting the mean values. To measure improvement from study entry, longitudinal baseline and follow-up health status scores were analyzed with linear mixed models; follow-up time was coded as a categorical variable, and the parameter associated with each follow-up time-point was compared with the baseline parameter. The proportion of patients whose scores changed by defined levels were compared with Mantel-Haenszel chi-square statistics.
Longitudinal linear mixed models with restricted maximum likelihood were used to compare the follow-up health status scores by treatment assignment adjusting for follow-up year and the corresponding baseline health status measure. Generalized estimating equations (GEE) were used to model the odds of improvement (defined as any positive change coded as a binary variable). The effect of treatment assignment on a single CES-D measure per patient was evaluated using linear regression. Since the distribution of angina severity at baseline was not balanced by cardiac treatment groups, all models evaluating cardiac treatment were adjusted by baseline angina severity. The interactions between cardiac and glycemic randomized treatments and between randomized treatment and follow-up time were tested in each model and dropped if not statistically significant. Correlation within clinical sites was handled by including random site effects in mixed models and by incorporating a categorical country variable in GEE models.
The effect of randomized treatment was similarly assessed in subgroups defined by baseline characteristics. For cardiac treatment comparison, the pre-specified subgroups of interest were intended method of revascularization (CABG or PCI) and baseline angina severity (physician-assessed Canadian Cardiovascular Society (CCS) classification). For glycemic treatment comparison, the pre-specified subgroups of interest were insulin use at baseline and duration of diabetes.
Multivariable mixed models were constructed to model follow-up health status and assess independent effects of the two randomization assignments, the stratum of intended revascularization, and pre-selected baseline characteristics. We tested interactions between randomized cardiac treatment and strata of intended revascularization or baseline angina, between randomized diabetes treatment and baseline insulin use or duration of diabetes, and between randomized treatment, strata and time. An exploratory analysis was performed to investigate whether angina severity mediated the treatment effect on health status by adding follow-up angina status to the longitudinal mixed models.
Missing baseline data were imputed by the mean value in the designated intended revascularization stratum. Since mixed effects models account for “missing at random” data, missing outcomes were not imputed for the primary analyses. To control for potential “missing not at random” data, we applied pattern mixture model methods described by Hedeker and Gibbons17 by incorporating a categorical variable indicating three missing data patterns: completers (no missing), noncompliance (sporadic missing data) and dropouts (death, study withdrawal, or termination of health status information). In sensitivity analyses, multiple imputation was used to impute non-existent outcome values for every randomized BARI 2D patient.
Since there were five outcome variables in this analysis, alpha=0.01 (=0.05/5) was considered statistically significant. All analyses were performed using SAS 9.0.
RESULTS
Of the 2,368 patients enrolled in BARI 2D, 69 died during the first year, and 2163 (94.1%) of the remaining patients completed one or more follow-up health status assessment. The four health status outcomes (DASI, Energy, Health Distress, and Self-rated Health) were obtained from 2,130 of 2,163 (98.5%) patients who were alive and participating in the study at year one, 2,023 of the 2,114 (95.7%) participating at year two, 1,934 of 2,044 (94.6%) at year three, and 1,684 of 1,820 (92.5%) at year four. A follow-up CES-D measure was available for 1,647 of the 2,163 patients (76.1%). Details about missing data are presented in supplemental Tables S1 and S2. The baseline characteristics of the 2,163 patients were well-balanced by randomization with the exception of angina status (Table 1).
Table 1.
Baseline characteristics by assigned treatment and randomization strata for BARI 2D patients with follow-up health status data
| Insulin Sensitization (n=1080) | Insulin Provision (n=1083) | Revascularization (n=1059) | Medical Therapy (n=1104) | CABG-Intended |
PCI-Intended |
|||
|---|---|---|---|---|---|---|---|---|
| Revascularization (n=342) | Medical Therapy (n=359) | Revascularization (n=717) | Medical Therapy (n=745) | |||||
| Age (years) | 62.3 | 62.3 | 62.2 | 62.4 | 62.7 | 63.3 | 61.9 | 61.9 |
| Male (%) | 70.4 | 70.9 | 70.7 | 70.6 | 74.6 | 78.3 | 68.9 | 66.8 |
| Current Smoking (%) | 12.6 | 11.8 | 12.9 | 11.5 | 11.7 | 9.8 | 13.4 | 12.4 |
| Body Mass Index (kg/m2) | 31.8 | 31.7 | 31.6 | 31.9 | 30.0 | 30.8 | 32.4 | 32.5 |
| Prior Myocardial Infarction (%) | 32.4 | 30.9 | 30.5 | 32.7 | 33.5 | 39.6 | 29.0 | 29.4 |
| History of Heart Failure (%) | 5.7 | 6.7 | 6.6 | 5.8 | 4.7 | 3.4 | 7.6 | 6.9 |
| Angina (%) | ||||||||
| None | 38.5 | 40.9 | 37.8 | 41.5 | 33.6 | 42.9 | 39.8 | 40.8 |
| Stable CCS I/II | 43.4 | 42.6 | 41.8 | 44.2 | 42.1 | 47.6 | 41.6 | 42.6 |
| Stable CCS III/IV or Unstable | 18.1 | 16.5 | 20.4 | 14.3 | 24.3 | 9.5 | 18.6 | 16.6 |
| Duration of Diabetes (years) | 10.0 | 10.6 | 10.1 | 10.6 | 10.0 | 10.8 | 10.1 | 10.4 |
| Insulin Use (%) | 26.7 | 28.4 | 26.7 | 28.4 | 20.5 | 24.0 | 29.7 | 30.5 |
| DASI (score, 0–58.2) | 18.9 | 19.3 | 19.1 | 19.1 | 17.4 | 19.4 | 19.9 | 18.9 |
| Energy (score, 0–100) | 52.1 | 51.6 | 51.2 | 52.5 | 56.4 | 59.2 | 48.8 | 49.3 |
| Health Distress (score, 0–100) | 40.1 | 40.6 | 40.7 | 40.0 | 38.5 | 33.9 | 41.8 | 42.9 |
| Self-rated Health (score, 0–100) | 39.2 | 38.5 | 39.5 | 38.3 | 39.6 | 39.6 | 39.4 | 37.6 |
Overall, there was significant improvement in mean health status scores after study entry (Table 2) that was maintained through year three for DASI (2.34 from baseline to year 1, p<0.001, and 0.50 from baseline to year 4, p=0.10) and through year four for Energy, Health Distress, and Self-rated Health. One year after enrollment, the mean improvement was significant (p < 0.001) for the four health status measures within each of the randomized treatment groups.
Table 2.
Change in health status scores*
| DASI | Energy | Health Distress | Self-rated Health | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | SE | P | Estimate | SE | P | Estimate | SE | P | Estimate | SE | P | |
| Year 1 versus baseline | 2.34 | 0.27 | <0.001 | 5.32 | 0.43 | <0.001 | −8.71 | 0.51 | <0.001 | 8.06 | 0.49 | <0.001 |
| Year 2 versus baseline | 1.82 | 0.28 | <0.001 | 5.41 | 0.45 | <0.001 | −9.07 | 0.53 | <0.001 | 7.86 | 0.51 | <0.001 |
| Year 3 versus baseline | 1.03 | 0.29 | <0.001 | 5.21 | 0.45 | <0.001 | −9.28 | 0.54 | <0.001 | 8.25 | 0.52 | <0.001 |
| Year 4 versus baseline | 0.50 | 0.31 | 0.10 | 4.66 | 0.49 | <0.001 | −9.28 | 0.61 | <0.001 | 7.34 | 0.55 | <0.001 |
Based on linear mixed models
Revascularization Strategies
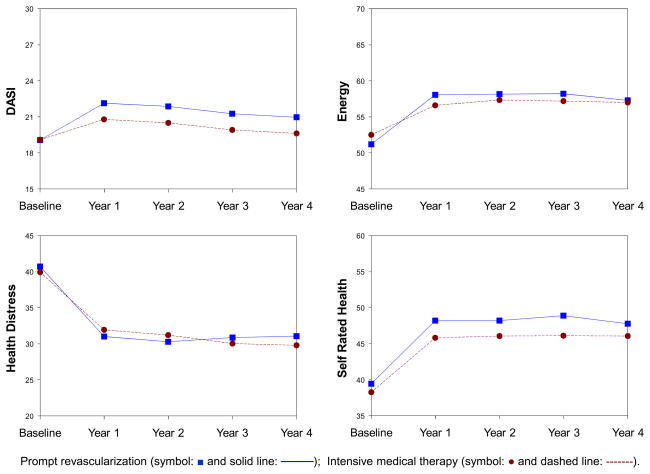
Patients randomized to prompt revascularization had greater improvements in average physical function, Energy, and Self-rated Health than patients randomized to medical therapy (Figure 1 and supplemental Table S3), and the two groups had similar reductions in Health Distress (p=0.49). The magnitude of the treatment difference did not vary significantly over the follow-up time period for any of the health status outcome measures. During the four-year follow-up, DASI scores were 1.32 points higher (p=0.001) among patients assigned to prompt revascularization compared with patients assigned to medical therapy; Energy was 1.36 points higher (p=0.02) and Self-rated Health was 1.77 points higher (p=0.007). Each health status score improved after study entry for approximately half of the patients (Table 3) and, patients assigned to prompt revascularization were significantly more likely to respond regarding DASI (OR=1.21, p=0.006) and Energy (OR=1.21, p=0.005) but not Self-rated Health or Health Distress. Patients assigned to prompt revascularization had similar mean CES-D scores as patients assigned to medical therapy (13.0 versus 12.6, p=0.40, Table S3).
Figure 1.
Health status by randomization to prompt revascularization (square symbol and solid line) versus medical therapy (circle symbol and dashed line). Points indicate mean scores in each group.
Table 3.
Improvement response in health status
| DASI |
Energy |
Health Distress |
Self-rated Health |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| REV | MED | P | REV | MED | P | REV | MED | P | REV | MED | P | |
| Year 1 versus baseline: N | 1039 | 1089 | 0.025 | 1038 | 1088 | 0.006 | 1037 | 1087 | 0.62 | 1039 | 1089 | 0.61 |
| Improvement % | 51.0 | 45.7 | 55.6 | 48.6 | 59.8 | 58.3 | 38.6 | 39.0 | ||||
| Neutral % | 16.5 | 18.5 | 16.4 | 19.9 | 13.5 | 14.5 | 48.2 | 45.8 | ||||
| Worsening % | 32.5 | 35.7 | 28.0 | 31.5 | 26.7 | 27.1 | 13.2 | 15.2 | ||||
| Year 2 versus baseline: N | 986 | 1034 | 0.044 | 987 | 1034 | 0.13 | 987 | 1033 | 0.55 | 986 | 1035 | 0.84 |
| Improvement % | 51.4 | 44.9 | 54.7 | 50.8 | 61.3 | 59.5 | 37.9 | 38.7 | ||||
| Neutral % | 13.3 | 17.5 | 15.3 | 17.1 | 12.3 | 13.5 | 47.4 | 45.1 | ||||
| Worsening % | 35.3 | 37.6 | 30.0 | 32.1 | 26.4 | 27.0 | 14.7 | 16.1 | ||||
| Year 3 versus baseline: N | 948 | 986 | 0.12 | 946 | 985 | 0.027 | 946 | 984 | 0.59 | 948 | 985 | 0.64 |
| Improvement % | 47.4 | 43.3 | 56.8 | 51.0 | 60.9 | 58.8 | 39.5 | 38.3 | ||||
| Neutral % | 14.2 | 16.0 | 14.7 | 17.4 | 12.6 | 14.5 | 46.3 | 47.2 | ||||
| Worsening % | 38.4 | 40.7 | 28.5 | 31.7 | 26.5 | 26.6 | 14.2 | 14.5 | ||||
| Year 4 versus baseline: N | 827 | 861 | 0.040 | 828 | 859 | 0.063 | 828 | 858 | 0.93 | 827 | 860 | 0.99 |
| Improvement % | 44.7 | 39.6 | 51.9 | 48.4 | 61.1 | 59.7 | 39.7 | 37.7 | ||||
| Neutral % | 13.7 | 16.3 | 18.5 | 17.5 | 11.2 | 13.8 | 43.3 | 47.2 | ||||
| Worsening % | 41.6 | 44.1 | 29.6 | 34.1 | 27.7 | 26.6 | 17.0 | 15.1 | ||||
| Improvement Response + | DASI Odds Ratio | P | Energy Odds Ratio | P | Health Distress Odds Ratio | P | Self-rated Health Odds Ratio | P | ||||
| REV vs MED (n=2163) | 1.21 | 0.006 | 1.21 | 0.005 | 1.05 | 0.53 | 0.99 | 0.88 | ||||
| By intended method of revasc. | 0.009 | 0.098 | 0.083 | 0.16 | ||||||||
| CABG: REV vs MED (n=701) | 1.52 | <0.001 | 1.41 | 0.006 | 1.20 | 0.16 | 1.12 | 0.39 | ||||
| PCI: REV vs MED (n=1462) | 1.07 | 0.40 | 1.12 | 0.17 | 0.97 | 0.69 | 0.92 | 0.36 | ||||
| IS vs IP (n=2163) | 1.06 | 0.49 | 0.93 | 0.26 | 1.00 | 0.97 | 1.08 | 0.31 | ||||
Odds of Improvement over four-year follow-up based on GEE models
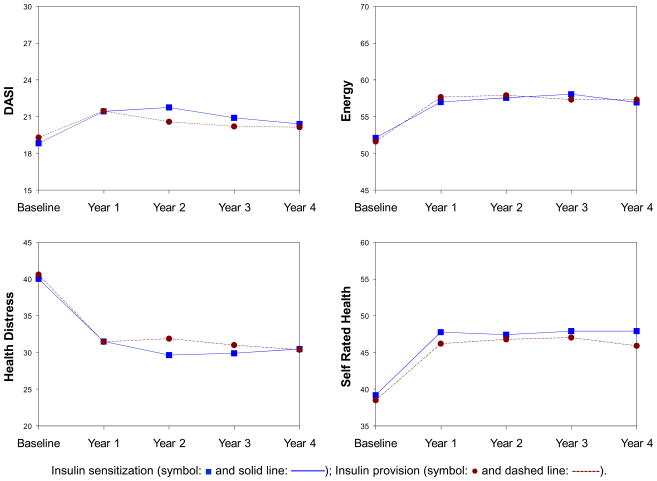
Glycemic Control Strategies
Health status during follow-up did not differ significantly by the randomized diabetes treatment strategy in any of the four health status domains (Figure 2). Mean CES-D also did not differ between patients assigned to insulin sensitization or insulin provision (p=0.90, Table S3).
Figure 2.
Health status by randomization to insulin sensitization (square symbol and solid line and solid line) versus insulin provision (circle symbol and dashed line). Points indicate mean scores in each group.
Subgroups
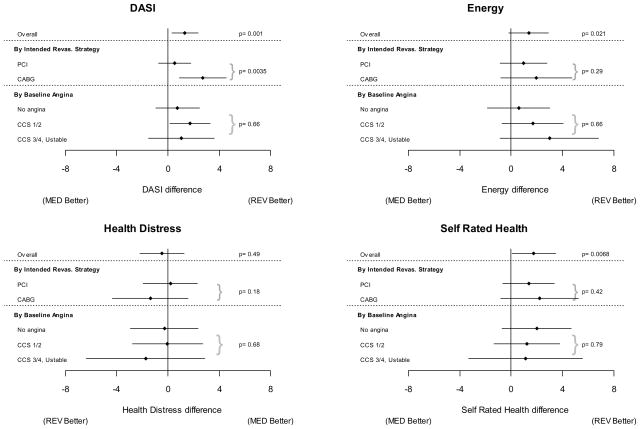
The randomized treatment comparisons in specified patient subgroups are shown in Figures 3 and 4. The effect of revascularization on DASI was significantly modified by the method of intended revascularization (interaction p=0.003). Within the stratum of patients identified for CABG, those randomized to prompt revascularization had significantly greater improvement in DASI scores compared with patients assigned to medical therapy (2.73 points, p<0.001). By contrast, within the stratum of patients identified for PCI, those randomized to prompt revascularization had an improvement in DASI that was similar to patients randomized to medical therapy (0.53 points, p=0.28). The magnitude of the randomized treatment effect did not vary significantly over the four year follow-up period in either stratum. The interaction between treatment assignment and stratum of intended revascularization was not significant for the other three health status outcomes (Figure 3). Mean health status stratified by intended method of revascularization is presented in supplemental Figure S1.
Figure 3.
Effect of randomization to prompt revascularization or medical therapy on health status overall and within subgroups. Estimates and 99% confidence intervals from mixed effects models.
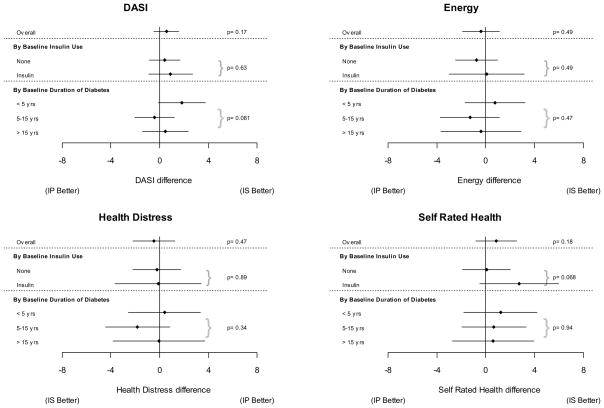
Figure 4.
Effect of randomization to insulin sensitization or insulin provision on health status overall and within subgroups. Estimates and 99% confidence intervals from mixed effects models.
The one-time depression score, CES-D, did not differ by the cardiac randomization in either the CABG (p=0.94) or PCI stratum (p=0.26). Patients with more severe angina at baseline experienced greater improvements in Energy after randomization to prompt revascularization (2.98 points higher with prompt revascularization among patients with Class III/IV angina, 1.67 points with Class I/II angina, and 0.58 points with no angina), but the interaction between angina severity and treatment was not statistically significant for Energy or for the other health status outcomes (Figure 3).
There was no significant interaction of baseline insulin use or duration of diabetes with the randomized glycemic treatment strategy (Figure 4).
Multivariable Analysis
In multivariable analysis, prompt revascularization was independently associated with higher Self-rated Health (1.68 points, p=0.0084) and marginally associated with higher Energy (1.17 points p=0.043), and this effect did not depend on intended method of revascularization (Table 4). For DASI, the effect of prompt revascularization differed according to the stratum of intended revascularization (interaction p=0.01) such that prompt revascularization with CABG was beneficial for physical function compared to initial medical therapy (2.63 points, p<0.001) while revascularization with PCI was not significantly different from initial medical therapy (0.57 points, p=0.22).
Table 4.
Multivariable models of follow-up health status scores
| DASI | Energy | Health Distress | Self-rated Health | |||||
|---|---|---|---|---|---|---|---|---|
| Estimate | p | Estimate | p | Estimate | p | Estimate | P | |
| Randomization | ||||||||
| Revascularization versus Medical in CABG stratum | 2.63 | <0.001 | 1.17 | 0.043 | −0.34 | 0.61 | 1.68 | 0.008 |
| Revascularization versus Medical in PCI stratum | 0.57 | 0.22 | ||||||
| Insulin sensitization versus Insulin provision | 0.50 | 0.19 | −0.33 | 0.57 | −0.52 | 0.43 | 0.96 | 0.13 |
| Covariates | ||||||||
| Baseline health status score | 0.53 | <0.001 | 0.43 | <0.001 | 0.41 | <0.001 | 0.40 | <0.001 |
| Follow up years in CABG stratum | −0.055 | 0.73 | −0.23 | 0.099 | −0.83 | 0.0052 | −0.21 | 0.19 |
| Follow up years in PCI stratum | −0.93 | <0.001 | 0.11 | 0.58 | ||||
| CABG stratum | −2.34 | 0.001 | 1.59 | 0.019 | −0.096 | 0.93 | 3.12 | <0.001 |
| Baseline angina status (reference: no angina) | ||||||||
| Stable CCS 1/2 | −0.45 | 0.31 | −2.65 | <0.001 | 1.64 | 0.028 | −2.29 | 0.001 |
| Stable CCS 3/4 or unstable | −0.64 | 0.29 | −1.82 | 0.043 | 1.60 | 0.12 | −1.59 | 0.11 |
| Insulin use at entry | −1.70 | <0.001 | −2.24 | 0.003 | 1.90 | 0.025 | −2.03 | 0.013 |
| Duration of diabetes | −0.083 | 0.001 | −0.11 | 0.004 | 0.14 | 0.0021 | −0.15 | <0.001 |
| Age | −0.20 | <0.001 | −0.11 | 0.003 | −0.071 | 0.091 | −0.032 | 0.43 |
| Male sex | 2.46 | <0.001 | 2.49 | <0.001 | −2.27 | 0.0039 | 1.84 | 0.015 |
| Body mass index | −0.17 | <0.001 | −0.17 | 0.001 | 0.19 | 0.002 | −0.27 | <0.001 |
| Current smoking | −2.97 | <0.001 | −5.37 | <0.001 | 5.30 | <0.001 | −6.87 | <0.001 |
| History of myocardial infarction | 0.025 | 0.95 | −1.57 | 0.015 | 1.02 | 0.16 | −1.32 | 0.063 |
| History of heart failure | −1.96 | 0.019 | −2.77 | 0.027 | 4.13 | 0.004 | −3.42 | 0.013 |
| Neuropathy | −1.38 | <0.001 | −1.50 | 0.016 | 1.40 | 0.049 | −1.56 | 0.023 |
| Missing status (reference: Completers ) | ||||||||
| Noncompliance | −2.10 | 0.052 | −2.28 | 0.16 | 3.20 | 0.084 | −3.73 | 0.045 |
| Dropout | −2.53 | <0.001 | −3.10 | <0.001 | 4.09 | <0.001 | −4.46 | <0.001 |
In multivariate-adjusted models, none of the health status measures differed by the randomly assigned diabetes treatment strategy. There was no evidence of interaction between the assigned cardiac and glycemic treatment strategies (p=0.62, DASI; p=0.41, Energy; p=0.44, Health Distress; p=0.74 Self-rated Health).
The interactions between randomized treatment and time were not significant indicating that the estimated treatment differences apply to all four years. However, there were significant interactions between the intended method of revascularization strata and time (p <0.001, DASI; p=0.009, Health Distress) such that health status benefits were better maintained in the CABG stratum than the PCI stratum for both the prompt revascularization and the medical therapy groups.
Male sex was independently associated with greater improvement in health status. Other baseline risk factors including older age, angina severity, insulin use, duration of diabetes, body mass index, smoking, history of heart failure and clinical evidence of neuropathy were independently associated with worse health status.
Adjusting for follow-up angina symptoms, the relationships between prompt revascularization and health status were modestly attenuated but did not disappear (supplemental Table S4). When all randomized BARI 2D patients were evaluated after imputation of missing outcome values, the results were consistent with those found among patients contributing follow-up data (supplement Table S5).
DISCUSSION
All patients in the BARI 2D randomized trial received intensive treatment for both diabetes and coronary disease, and on average, this patient cohort experienced a clinically meaningful and statistically significant improvement in health status after study enrollment. Compared with a strategy of intensive medical therapy, the strategy of prompt coronary revascularization with intensive medical therapy was associated with small or modest benefits in physical function, Energy, and Self-rated Health over the four years of follow-up although the revascularization benefit for physical function was significant among patients selected for CABG but not among those selected for PCI. Approximately half of the trial population had better health status scores during follow-up than at baseline, and prompt revascularization was associated with a greater likelihood of improvement for physical function and Energy compared with initial medical therapy. By contrast, none of the health status measures differed between patients assigned to a glycemic control strategy based on insulin sensitization or based on insulin provision. The degree and severity of depressive symptoms were not affected by the cardiac or diabetes randomized treatment strategies.
Consistent with other studies,1,2,13,14,18 BARI 2D demonstrates that the invasive approach conferred small, yet significant, benefits in physical function and perceived health status. In the COURAGE trial, patients randomized to PCI with optimal medical therapy had slightly better health status outcomes over the first three years compared with those randomized to optimal medical therapy alone.1 PCI with stenting was also shown to have small short-term advantages over medical therapy for physical function in the acute MI setting.11 The original BARI study established that CABG resulted in higher DASI scores than balloon angioplasty for the first three years but not thereafter.14 In BARI 2D, the differences between the randomized treatment groups were largely maintained over four years of follow-up. However, these statistically significant treatment differences did not reach the pre-defined thresholds of clinical significance. It is important to recognize that the medical treatment strategy included the use of revascularization when clinically indicated, and 19% of patients assigned to medical therapy received revascularization by one year and 38% by four years.3 In both treatment groups, the initial gains for DASI diminished over subsequent years. It is likely that the attenuation of physical function is due to the progressive nature of coronary atherosclerosis and to subsequent disease in vein grafts as well as restenosis after angioplasty or stents.
Previous clinical trials comparing revascularization and medical therapy reported that the observed improvement in health status may partly be attributed to the ability of revascularization to relieve angina.1,2,18 We assessed angina as a potential moderator and mediator. The impact of revascularization on health status was partially, but not completely, mediated through improvement in angina status. The severity of angina at study entry did not significantly modify the treatment effects, but most patients in this study had mild symptoms. In patients with both stable ischemic heart disease and type 2 diabetes, health status is influenced by the perceived burden of cardiac disease as well as diabetes (e.g. insulin use, neuropathy), and as a result, the influence of angina on health status may be weaker than what has been observed in cardiac patient populations.
In the BARI 2D trial, the method of revascularization, CABG or PCI, was selected before the patient was randomized. The effect of prompt revascularization on DASI was greater among those identified a priori as more suitable for CABG than among those identified for PCI. Participants selected for CABG were distinctly different from those selected for PCI. At baseline, patients in the CABG stratum were older, had more extensive coronary disease and more severe angina symptoms but were less likely to be taking insulin.9 Moreover, long-term survival rates were lower in the CABG stratum3 which may have resulted in stratum-specific survival biases. The advantage seen with CABG remained significant after adjustment for the differences in patient characteristics suggesting that the benefit was due, at least in part, to the CABG procedure itself, perhaps stemming from the degree of “complete revascularization” afforded with surgery. In contrast, the favorable Energy and Self-rated Health outcomes seen with prompt revascularization did not depend on the method of revascularization, and thus, revascularization with PCI conferred measurable health status benefits relative to medical therapy.
The health status outcomes were remarkably similar for patients treated with an insulin providing strategy and those treated with an insulin sensitizing strategy. Past observational studies have implicated the use of insulin with worse health status among patients with diabetes,19,20 but it has not been clear whether insulin treatment, per se, was detrimental, or whether insulin use was merely identifying patients who were more severely ill. Indeed in BARI 2D, patients receiving insulin at study entry had significantly worse physical function, Energy, Health Distress and Self-rated Health throughout the study compared with those not entering on insulin. Complications such as severe hypoglycemia, nephropathy and neuropathy have been associated with worse health status, and some studies indicate that glycemic control may be an important factor.20, 21 However, like UKPDS and several other randomized trials,21–23 BARI 2D shows that treatment strategies that rely on insulin provision therapy and those that avoid insulin provision lead to similar health status outcomes. At the three year follow-up, 61% of the BARI 2D patients in the insulin provision group were being treated with insulin compared with 29% in the insulin sensitization group. Thus, our data suggest that insulin treatment does not compromise health status among patients with advanced diabetes.
The BARI 2D trial was designed to compare treatment strategies in the setting of intensive coordinated care. Study patients were seen frequently during follow-up, and treatment strategies were employed to treat glycemia to a target HbA1c < 7.0%, reduce angina symptoms, treat hypertension and dyslipidemia, and actively encourage smoking cessation and weight loss when appropriate. Health status improved significantly between study entry and the first annual follow-up visit for patients regardless of randomized treatment assignment, and the marked reduction in Health Distress and improvements in Energy and Self-rated Health were maintained throughout follow-up. The “case-management” approach, with attentive care provided by BARI 2D medical staff and the opportunity to promptly address concerns about treatment and complications, may have contributed to desirable outcomes in both the psychosocial and medical domains. Furthermore, patients with advanced diabetes and cardiac risk factors at study entry experienced less improvement in health status which supports the concept that early detection and intervention for diabetes and cardiac disease are critical for achieving successful long-term outcomes.
This study has a number of limitations. In an effort to minimize participant burden, the BARI 2D battery was designed to include only a few measures focused on assessing the health status response to medical interventions. We therefore lack a broad profile of quality of life and patient-assessed angina burden, in particular. Since the BARI 2D randomized treatments were not masked, it is possible that health status was influenced by patient expectations of treatment effect. Health status was measured at the annual follow-up visits, and consequently, we have no information on short-term treatment response. Moreover, patients who died or withdrew during the first year of the trial did not contribute follow-up health status data and were excluded from the primary analyses. Our conclusions about health status apply to surviving patients; however, over 90% of the randomized patients completed a follow-up health status questionnaire, and the multiple imputation analyses suggest that our results persist when accounting for death and missing data.
The BARI 2D clinical trial illustrates that intensive coordinated care of diabetes and cardiac risk factors results in clinically meaningful and statistically significant improvement in aspects of health status for patients with type 2 diabetes and stable ischemic heart disease. The addition of prompt revascularization to intensive medical therapy resulted in small statistically significant benefits in physical function and Self-rated Health and marginally significant benefits in Energy. The effect of prompt revascularization on DASI was greater among patients selected for CABG than among those selected for PCI, while the benefits of prompt revascularization on Self-rated Health and Energy were evident irrespective of the method of revascularization. Health status outcomes were similar for patients treated with a strategy focused on insulin sensitization versus insulin provision.
Supplementary Material
Acknowledgments
Sources of Funding
The Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) is funded by the National Heart, Lung and Blood Institute and the National Institute of Diabetes and Digestive and Kidney Diseases (U01 HL061744, U01 HL061746, U01 HL061748, U01 HL063804).
BARI 2D receives significant supplemental funding from GlaxoSmithKline, and additional funding from Lantheus Medical Imaging, Inc. (formerly Bristol-Myers Squibb Medical Imaging, Inc.), Astellas Pharma US, Inc., Merck & Co., Inc., Abbott Laboratories, Inc. and Pfizer, Inc. Medications and supplies were donated by Abbott Laboratories Ltd., MediSense Products, Bayer Diagnostics, Becton, Dickinson and Company, J. R. Carlson Labs, Centocor, Inc., Eli Lilly and Company, LipoScience, Inc., Merck Sante, Novartis Pharmaceuticals Corporation, and Novo Nordisk, Inc.
Footnotes
Clinical Trials Registration Information -- URL: http://clinicaltrials.gov. Unique Identifier: NCT00006305.
Disclosures
Dr. Helmy reports serving as a consultant for Cordis and Abbott Vascular. Dr. Hillegass reports receiving lecture fees from Eli Lilly, Daishi Sankyo and Medicines Company. Ms Massaro reports receiving honoraria from Merck. The remaining authors report no conflicts.
References
- 1.Weintraub WS, Spertus JA, Kolm P, Maron DJ, Zhang Z, Jurkovitz C, Zhang W, Hartigan PM, Lewis C, Veledar E, Bowen J, Dunbar SB, Deaton C, Kaufman S, O’Rourke RA, Goeree R, Barnett PG, Teo KK, Boden WE COURAGE Trial Research Group. Effect of PCI on Quality of Life in Patients with Stable Coronary Disease. N Engl J Med. 2008;359:677–87. doi: 10.1056/NEJMoa072771. [DOI] [PubMed] [Google Scholar]
- 2.Pocock SJ, Henderson RA, Clayton T, Lyman GH, Chamberlain DA. Quality of life after coronary angioplasty or continued medical treatment for angina: three-year follow-up in the RITA-2 trial (Randomized Intervention Treatment of Angina) J Am Coll Cardiol. 2000;35:907–914. doi: 10.1016/s0735-1097(99)00637-3. [DOI] [PubMed] [Google Scholar]
- 3.BARI 2D Study Group. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med. 2009;360:2503–15. doi: 10.1056/NEJMoa0805796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brooks MM, Frye RL, Genuth S, Detre KM, Nesto RW, Sobel BE, Kelsey SF, Orchard TJ. Hypotheses, design, and methods for the Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) Trial. Am J Cardiol. 2006;97:9G–19G. doi: 10.1016/j.amjcard.2006.02.023. [DOI] [PubMed] [Google Scholar]
- 5.Barsness GW, Gersh BJ, Brooks MM, Frye RL. Rationale for the revascularization arm of the Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) Trial. Am J Cardiol. 2006;97:31G–40G. doi: 10.1016/j.amjcard.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 6.Magee MF, Isley WL. Rationale, design, and methods for glycemic control in the Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) Trial. Am J Cardiol. 2006;97:20G–30G. doi: 10.1016/j.amjcard.2006.02.024. [DOI] [PubMed] [Google Scholar]
- 7.Albu J, Gottlieb SH, August P, Nesto RW, Orchard TJ. Modifications of coronary risk factors. Am J Cardiol. 2006;97:41G–52G. doi: 10.1016/j.amjcard.2006.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bypass Angioplasty Revascularization Investigation 2 Diabetes Study Group. Baseline characteristics of patients with diabetes and coronary artery disease enrolled in the Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) trial. Am Heart J. 2008;156:528–36. doi: 10.1016/j.ahj.2008.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim LS, King SB, Kent K, Brooks MM, Kip KE, Abbott JD, Jacobs AK, Rihal C, Hueb WA, Alderman E, Pena Sing IR, Attubato MJ, Feit F. Factors related to the selection of surgical versus percutaneous revascularization in diabetic patients with multivessel coronary artery disease in the BARI 2D trial. JACC: Cardiovascular Interventions. 2009;2:384–392. doi: 10.1016/j.jcin.2009.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hlatky MA, Boineau RE, Higginbotham MB, Lee KL, Mark DB, Califf RM, Cobb FR, Pryor DB. A brief self-administered questionnaire to determine functional capacity (the Duke Activity Status Index) Am J Cardiol. 1989;64:651–654. doi: 10.1016/0002-9149(89)90496-7. [DOI] [PubMed] [Google Scholar]
- 11.Stewart AL, Ware JE, editors. Measuring Functioning and Well-being: The Medical Outcomes Study Approach. Duke University Press; Durham, NC: 1992. [Google Scholar]
- 12.Lorig K, Stewart A, Ritter P, González V, Laurent D, Lynch J. Outcome measures for health education and other health care interventions. Thousand Oaks, CA: Sage Publications; 1996. [Google Scholar]
- 13.Mark DB, Pan W, Clapp-Channing NE, Anstrom KJ, Ross JR, Fox RS, Devlin GP, Martin CE, Adlbrecht C, Cowper PA, Ray LD, Cohen EA, Lamas GA, Hochman JS Occluded Artery Trial Investigators. Quality of life after late invasive therapy for occluded arteries. N Engl J Med. 2009;360:774–83. doi: 10.1056/NEJMoa0805151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hlatky MA, Rogers WJ, Johnstone I, Boothroyd D, Brooks MM, Pitt B, Reeder G, Ryan T, Smith H, Whitlow P, Wiens R, Mark DB. Medical care costs and quality of life after randomization to coronary angioplasty or coronary bypass surgery. N Engl J Med. 1997;336:92–9. doi: 10.1056/NEJM199701093360203. [DOI] [PubMed] [Google Scholar]
- 15.Lorig KR, Sobel DS, Stewart AL, Brown BW, Jr, Bandura A, Ritter P, Gonzalez VM, Laurent DD, Holman HR. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: a randomized trial. Med Care. 1999;37:5–14. doi: 10.1097/00005650-199901000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 17.Hedeker D, Gibbons RD. Application of random-effects pattern-mixture models for missing data in longitudinal studies. Psychological Methods. 1997;2:64–78. [Google Scholar]
- 18.Kim J, Henderson RA, Pocock SJ, Clayton T, Sculpher MJ, Fox KA. Health-related quality of life after interventional or conservative strategy in patients with unstable angina or non-ST-segment elevation myocardial infarction: one-year results of the third Randomized Intervention Trial of unstable Angina (RITA-3) J Am Coll Cardiol. 2005;45:221–228. doi: 10.1016/j.jacc.2004.10.034. [DOI] [PubMed] [Google Scholar]
- 19.Redekop WK, Koopmanschap MA, Stolk RP, Rutten GE, Wolffenbuttel BH, Niessen LW. Health-related quality of life and treatment satisfaction in Dutch patients with type 2 diabetes. Diabetes Care. 2002;25:458–63. doi: 10.2337/diacare.25.3.458. [DOI] [PubMed] [Google Scholar]
- 20.Rubin RR, Peyrot M. Quality of life and diabetes. Diabetes Metab Res Rev. 1999;15:205–18. doi: 10.1002/(sici)1520-7560(199905/06)15:3<205::aid-dmrr29>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 21.U.K. Prospective Diabetes Study Group. Quality of life in type 2 diabetic patients is affected by complications but not by intensive policies to improve blood glucose or blood pressure control (UKPDS 37) Diabetes Care. 1999;22:1125–36. doi: 10.2337/diacare.22.7.1125. [DOI] [PubMed] [Google Scholar]
- 22.Vinik AI, Zhang Q. Adding insulin glargine versus rosiglitazone: health-related quality-of-life impact in type 2 diabetes. Diabetes Care. 2007;30:795–800. doi: 10.2337/dc06-1712. [DOI] [PubMed] [Google Scholar]
- 23.Lingvay I, Legendre JL, Kaloyanova PF, Zhang S, Adams-Huet B, Raskin P. Insulin-Based versus Triple Oral Therapy for Newly-Diagnosed Type 2 Diabetes: Which is Better? Diabetes Care. 2009;32:1789–95. doi: 10.2337/dc09-0653. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.