Abstract
Context
Patients with life-limiting illnesses, and their families, struggle with complex treatment decisions as these patients approach the last few years of life. Surrogates often do not clearly understand the patient's goals for future medical treatments.
Objectives
To determine if a disease-specific planning process can improve surrogate understanding of such patient goals for future, medical treatments.
Design, Setting, and Participants
A multisite randomized controlled trial conducted between January 1, 2004 and July 31, 2007 in 6 outpatient clinics of large community or university health systems in 3 Wisconsin cities. Subjects were patients with either chronic congestive heart failure or chronic renal disease and their surrogate decision makers. Participants had to be competent, English-speaking adults at least 18 years of age.
Intervention
Trained health professionals conducted a structured, patient-centered interview intended to promote informed decision making and to result in the completion of a document clarifying the goals of the patient with regard to four disease-specific health outcome situations and to the degree of decision-making latitude granted to the surrogate.
Measurements
Surrogate understanding of patient goals for care with regard to four expected, disease-specific outcomes situations and of the degree of surrogate latitude in decision making.
Results
Three hundred thirteen patient-surrogate pairs completed the study. As measured by Kappa (κ) scores and in all four situations and in the degree of latitude, intervention group surrogates demonstrated a significantly higher degree of understanding of patient goals than control group surrogates. Intervention group κ scores ranged from 0.61 to 0.78, while control group κ scores ranged from 0.07 to 0.28.
Conclusion
Surrogates in the intervention group had a significantly better understanding of patient goals and preferences than surrogates in the control group. This finding is the first step toward ensuring that patient goals for care are known and honored.
INTRODUCTION
Patients with chronic, life-limiting illnesses face serious and confusing health care decisions in the last years of life which are often complicated by documents such as “living wills”.1–3 A preferred approach involves legally appointing a health care agent or proxy4 but most efforts to prepare surrogates to make substituted decisions have been unsuccessful. In a systematic review on the accuracy of surrogate decision making, Shalowitz et al7 concluded that surrogates incorrectly predicted patients' treatment preferences in one-third of cases. Of the 16 articles reviewed, only two used an intervention intended to improve surrogate understanding of patient preferences. In these two articles, neither Ditto et al8 nor Matheis-Kraft et al9 showed significant improvement in surrogate understanding of patient's choices in their intervention groups.
Three recent pilot studies provide evidence that structured advance care planning (ACP) interventions to prepare patients and their surrogates to understand expected complications, make informed decisions prior to a medical crisis, and communicate patient goals may reduce conflict, relieve the family of the decision-making burden, and ensure that patient goals for care are known and honored.5 A randomized study of 61 geriatric patients,10 in which the intervention group received a Respecting Choices®–facilitated discussion, and two pilot studies that, like the current study, tested the Patient-Centered Advance Care Planning (PC-ACP) intervention have shown11,12 a significant increase in surrogate understanding of patient preferences (P = .01). Recently the intervention was used with adolescents living with human immunodeficiency virus (HIV) infection and their families, and researchers found increased congruence, decreased patient decisional conflict, and increased quality of communication.13 Little other research has been conducted concerning the effectiveness of interventions promoting ACP and advance directives (ADs).14
We report the results of a larger, randomized controlled trial examining the impact of PC-ACP on (1) surrogate understanding of patient goals for future medical care, (2) patient and surrogate knowledge of ACP, and (3) intervention patient and surrogate evaluation of the quality of communication regarding the structured interview. We hypothesize that a facilitated disease-specific planning discussion that includes the surrogate decision maker will favorably affect the surrogate decision-maker's understanding of the patient's wishes and both the patient's and the surrogate's knowledge about advanced care planning.
METHODS
Design and Setting
The study used a randomized controlled design. Patients with congestive heart failure (CHF) or end-stage renal disease (ESRD) and their surrogates were randomized to receive either the PC-ACP intervention (intervention group) or usual care (control group) using the sealed-envelope method within each setting and disease condition. The allocation sequence was generated by the project director using a computerized random number generator. The study was conducted in a similar fashion at medical centers headquartered in La Crosse and Madison, Wisconsin. The La Crosse center recruited CHF patients from an outpatient, multispecialty clinic, and recruited ESRD patients from two nephrology clinic/dialysis units. The Madison center recruited CHF patients from a cardiac rehabilitation clinic and from CHF clinics located in Madison and in Milwaukee; ESRD patients were recruited from two dialysis clinics. La Crosse has a long history of community-level ACP education, in contrast to the Madison center and sites, where no such organized community-level ACP education has taken place. The study was approved by the Health Sciences Institutional Review Board and Human Subjects Committee of the University of Wisconsin-Madison and of Gundersen Clinic, Ltd., as well as the IRBs of all the cooperating sites. It was registered at clinicaltrials.gov.
Participants
Patients and their designated surrogate decision makers were recruited as pairs. Patients with CHF and ESRD were chosen because these patient populations present both similarities and differences at the end-of-life. Individuals with both diagnoses have a chronic illness with a steady decline marked with exacerbations and incomplete recovery. Both groups are at high risk for sudden complications which may cause them to lose decision-making capacity and leave an unprepared surrogate. In addition, ESRD patients have the possibility of discontinuing a single technology supporting their life, which could result in a short end-of-life period. The selection of patients focused primarily on those who were receiving medical care, but had clinical signs and symptoms that indicated a risk of serious complication or death in the next two years. Patients with CHF had a New York Heart Association (NYHA) classification of II, III, or IV. Patients with ESRD had a serum albumin concentration < 3.7 g/dL (37 g/L) and a co-morbidity, such as diabetes, CHF, chronic obstructive pulmonary disease (COPD), a history of acute myocardial infarction (MI), or an above-the-knee amputation. Patients chose their surrogates, who agreed to make health care decisions should the patient become unable. Participants were 18 years of age or older, had decision making capacity, and were able to speak and understand English. Decision making capacity was determined by choosing patients who did not have an activated Power of Attorney for Healthcare and through consultation with the clinicians providing care to the patients. Patients were referred to the clinic social worker for assistance in completing a durable power of attorney for health care (DPOAHC) if they did not have a DPOAHC or if they wished to update their current DPOAHC.
Screening and Enrollment
Inservices were held to train clinic staff to screen participants. Clinic staff were given inclusion criteria and reviewed the medical records of patients scheduled for appointments to determine eligibility. Research staff met weekly with clinic staff to answer questions and ensure that all eligible patients were approached. Due to Health Insurance Portability and Accountability Act (HIPAA) and clinic rules, investigators could neither screen nor directly approach eligible patients. Clinical staff asked eligible patients if they were interested in more information about the study. If a patient was interested, a member of the research staff explained the study, determined if the patient had a surrogate decision maker, obtained informed consent, and enrolled the patient. If the surrogate was not present at that time, an appointment was made with the patient and surrogate for data collection.
Power Analysis
The projected sample size per treatment group was based on pilot data11 and previous research findings establishing a range of baseline congruence values (i.e., 35%–70% agreement).15, 16 The lower agreement figure of 35% was used in the power calculation, with the assumption that the value was constant. A moderate treatment effect of 71% increase in agreement (35% baseline increased to 60% post intervention) was assumed. Therefore, a total sample of approximately 560 patient-surrogate pairs evenly divided between the intervention group and the control group would be required to maintain a 0.10 β error level (power = .90). Patient-surrogate pairs were recruited from January 1, 2004, until July 31, 2007. Recruitment was halted due to expiration of funding.
Data Collection
All participants completed the measures on paper unless they had literacy or vision issues that precluded reading the forms. Any participants who expressed inability to read or who asked for assistance were offered the option of having the research assistant read the questions and answers aloud. Approximately 25% of the patients and no surrogates had the questions read to them. All patients and surrogates completed all measures separately. If they required assistance completing the forms, this was done in separate rooms. The research assistant assigned patient-surrogate pairs to the control group or an intervention group based on the sealed envelope method. Control pairs completed initial outcome measures upon entry into the study. Intervention pairs received the PC-ACP interview and completed outcome measures immediately afterward. Due to the nature of the intervention, the PC-ACP facilitator was not blinded to the group assignment.
Usual Care
All patients received care provided by their local health organization for the completion of ADs. For the La Crosse center, usual care includes ACP facilitation with the patient, but not the in-depth, patient-centered intervention in the presence of the surrogate decision-maker that is described in this study. For all sites, usual care included standard AD counseling, assessment of an AD on admission to the organization, and/or questions if they would like more information. If they desired assistance, they were referred per institutional protocol.
Intervention
The intervention was derived from previous work by Briggs and Hammes17, 18 and consisted of the PC-ACP structured interview delivered by a trained facilitator which resulted in documentation of patient goals for care in the medical record using a disease-specific Statement of Treatment Preferences (STP) form. The PC-ACP interview included the patient and the surrogate decision maker and lasted between 60 and 90 minutes. The purposes of the interview were: 1) to assess the patient and surrogate understanding of the patient's illness, experiences, hopes, fears, and concerns; 2) to provide individualized information about disease specific treatment choices and their benefit and burdens; 3) to assist in the documentation of disease-specific goals of care; and 4) to prepare the surrogate to understand the patient's choices and make future decisions to honor these choices (http://www2.edc.org/lastacts/archives/archivesmarch03/featureinn.asp). The first stage of the interview assesses the patient's understanding of the current medical condition, potential complications, hopes, fears, and perception of living well. The second stage of the interview explores experiences the patient may have had that have impacted their goals for future medical decision-making. Stage three of the interview assists the patient and surrogate to appreciate the value of discussing specific treatment choices the patient is likely to experience in the future, and how these discussions will prepare the surrogate to make substitute decisions based on a more thorough understanding of the patients' goals and preferences. Stage four of the interview uses a disease-specific Statement of Treatment Preference document to help the patient and surrogate to understand real scenarios that may occur due to illness complications, and to assist the patient to verbalize goals and values related to acceptable or unacceptable burdens and outcomes. This document allows the facilitator to introduce replacement information, such as why they are at risk for certain complications and the benefits and burdens of a particular life-sustaining treatment (e.g., CPR). Surrogates are encouraged to ask questions to help them better understand the patients' goals and to prepare for the types of decisions they may be asked to make if the patient cannot make their own decision. Stage five summarizes the value of the discussion for both the patient and surrogate, the need for future discussions as situations and preferences change and the expectation that the patient is more likely to have their wishes honored in the future. The interview was theoretically supported by the representational approach to patient education.19 Further information about the intervention can be found in Briggs, Kirchhoff, Hammes, Song, and Colvin (2004).11
PC-ACP Facilitator Training
The PC-ACP interview required professionals skilled in the content, techniques, and delivery of the intervention. A competency-based educational approach was used to train the six research staff (three nurses, two social workers, and a chaplain) who conducted the PC-ACP interviews. All interviewers successfully demonstrated predefined competencies after videotape review and individual feedback. One year after training, all facilitators were observed and given feedback. All demonstrated fidelity to the delivery of the PC-ACP interview and consistency at that time.
Instruments
Pre-intervention measures
Demographic Data Sheet (completed by patient and surrogate) included age, sex, race, marital status, education, and religious preference.
Outcome measures
Knowledge about Advance Care Planning (completed by patient and surrogate) developed for this study assessed understanding of the purposes of an AD, ACP, and issues such as the role of the surrogate. This is a 10-item, true/false/don't know questionnaire. Included were questions about whether ADs allow the patient to make different choices in the future and under what circumstances the surrogate may be asked to become involved in decision making. Higher scores indicated higher understanding of ACP. Two experts in ACP and one with expertise in psychometrics assisted with content validity of the instrument. Cronbach's α values were 0.76 (patients) and 0.79 (surrogates) in one study of 32 pairs in which the patients had undergone open heart surgery.12
Statement of Treatment Preferences (STP) (completed by patient and surrogate separately) was developed by Briggs and Hammes (2002, 2008)17. The STP form serves as a decision-aide/documentation tool to promote understanding of likely situations that could occur in the future and to express the patients' goals of treatment in light of acceptable and unacceptable burdens and outcomes. The first three situations in the STP described an outcome from a complication of the patient's illness after a trial of treatment was provided: (Situation 1) a prolonged hospital stay requiring ongoing medical interventions and with a low chance of survival (e.g., < 5%); (Situation 2) a good chance of survival, with permanent, severe functional impairment (could not walk, talk) requiring 24-hour nursing care; and (Situation 3) a good chance of survival, with permanent, severe cognitive impairment (did not know who I was or who I was with) requiring 24-hour nursing care. For each situation, after discussion and clarification of the meaning of the situation, patients were asked to choose one of three options: “continue all treatment,” “stop all treatment to prolong my life,” or “don't know.” Situation 4 described a sudden event causing the patient's heart and breathing to stop where the chance of recovery may be low and the burdens of treatment may be high, and the choices were “do not attempt resuscitation,” “attempt resuscitation,” or “do not attempt resuscitation if the treating physician believes the chance of survival is low.” An additional item, a latitude statement, clarified the decision-making authority a patient wished to grant the chosen surrogate (patient's form) and the surrogate's understanding of that authority (surrogate's form). From the following three options, surrogates were asked to choose the one that best described their understanding of their decision-making authority: to “strictly follow the wishes,” “do what the surrogate thinks is best at the time,” or “don't know.”
Quality of Patient-Clinician Communication about End-of-life Care (completed only by patients and surrogates in the intervention group) was developed by Engleberg, Downey, and Curtis,20 and consists of four items used to determine the quality of patient-facilitator communication about end-of-life care and a single generic-rating question. Items are rated on a 3-point scale from “no” to “definitely yes,” with higher scores indicating higher satisfaction with the quality of communication. Good internal consistencies have been reported in acquired immune deficiency syndrome (AIDS) patients (Cronbach's α = .81).21 In our pilot study, the internal consistencies for patients and surrogates were .87 and .88, respectively.11 This is reported only on the intervention group because the control group did not have conversations regarding future medical care with a PC-ACP facilitator.
Statistical Analysis
Chi-square and t-tests were used to compare demographic variables to ensure that the samples were comparable. Initially, Kappa (κ) statistics were used to estimate the surrogate understanding of the patient choices for each scenario presented. Logistic regression was used to determine the relationship of the surrogate's choices to those of the patient. These logistic regression models were constructed for each situation using the patient's choices as the reference. The models were then expanded to assess possible interactions between treatment and select covariates of patient age, patient knowledge, patient educational level, site, surrogate educational level, and surrogate knowledge.
For the secondary outcome of knowledge of ACP, the Knowledge About Advance Care Planning instruments were scored and the group scores compared using a Mann-Whitney U test. The quality of communication instrument was used only in the intervention group to provide the participant's assessment of the ACP facilitation session.
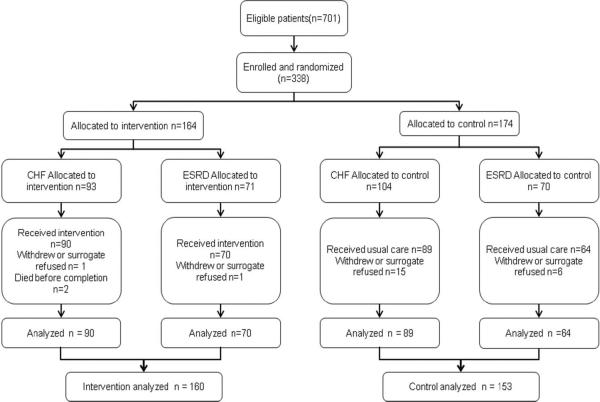
RESULTS
Out of 701 interested, eligible patients, 338 (48.2%) patients were enrolled. Reasons for interested, eligible patients not enrolling were not given consistently. Of the enrolled patients, 313 (92.6%) patients and their surrogates completed the study (Figure 1). Of those patients who were enrolled and did not complete the study: two (0.59% of enrolled) died or became too ill before data could be collected, two (0.59%) could not identify a surrogate, 14 (4.1% of enrolled) surrogates decided not to participate and seven (2.1% of enrolled) decided to withdraw with no further reason given. Although the power analysis indicated that 560 patient-surrogate pairs would be optimal, recruitment was halted with a total of 313 pairs (55.9% of projected) at the end of the funding period since it was not feasible to continue.
Figure 1.
Flow of Study Participants
Of those who completed the study, 179 had a diagnosis of end stage CHF (La Crosse, n=134; Madison n=45), and 134 had ESRD (La Crosse, n=98; Madison, n=36). A total of 313 patient/surrogate pairs were included in the analysis, which was an intent-to-treat analysis.
Control (n = 153) and intervention (n = 160) patients were both close to 70 years of age, usually married, white, and Protestant (Table 1). Patients' ages ranged from 37 to 93 years. Surrogates were on the average younger, predominately female, married, and Protestant.
Table 1.
Patient and Surrogate Baseline Demographic Information by Group
| Patient | Surrogate | |||||
|---|---|---|---|---|---|---|
| Characteristics | Control n = 153* | Intervention n = 160* | Statistical Significance | Control n = 153* | Intervention n = 160* | Statistical Significance |
| Mean age, y (SD) | 70.6 (11.61) | 71.4 (12.24) | t = −0.69, α =.49 | 57.41 (13.62) | 59.46 (13.94) | t = −1.27, α = .201 |
| No. (%) of Patients | No. (%) of Surrogates | |||||
| Men | 89 (58.2) | 96 (60.0) | χ2 = 0.1(df=1) | 41 (26.8) | 43 (26.9) | χ2 = 0.0002 (df=1) |
| White race | 146 (95.4) | 149 (93.1) | χ2 = 0.8(df=1) | 147 (96.0) | 153 (95.6) | χ2 = 0.03(df=1) |
| Marital status | n = 152 | χ2 = 2.6 (df=3) | n = 152 | n = 158 | χ2 = 0.5 (df=3) | |
| Married | 80 | 99 | 123 (80.4) | 130 (82.4) | ||
| Widowed | 14 | 12 | p = .470 | 13 (8.5) | 11 (7.0) | p = .929 |
| Divorced/Separated | 40 | 33 | 5 (3.3) | 4 (2.5) | ||
| Never married | 18 | 16 | 12 (7.8) | 13 (8.2) | ||
| Religious preference | n = 150 | n = 158 | χ2 = 2.6 (df=2) | n = 150 | n = 158 | χ2 = 1.6 (df=2) |
| Protestant | 98 (65.3) | 90 (57.0) | 95 (63.3) | 91 (56.9) | ||
| Catholic | 31 (20.7) | 44 (27.8) | p = .281 | 37 (24.7) | 49 (30.6) | p = .451 |
| Other | 21 (14.0) | 24 (15.2) | 18 (12.0) | 20 (12.5) | ||
| Education | χ2 = 4.1 (df=1) | n = 152 | n = 158 | χ2 = 0.1 (df=1) | ||
| High school or less | 105 (68.7) | 126 (78.7) | 82 (53.9) | 88 (55.7) | ||
| Beyond high school | 48 (31.3) | 34 (21.3) | p = .053 | 70 (46.1) | 70 (44.3) | p = .734 |
| Relationship of surrogate to patient | n = 151 | n = 157 | χ2 = 11.2 (df=7) | |||
| Spouse or partner | 66 (43.7) | 86 (54.8) | ||||
| Child | 48 (31.8) | 52 (33.1) | p = .115 | |||
| Sibling | 14 (9.3) | 7 (4.5) | ||||
| Other | 23 (15.2) | 12 (7.6) | ||||
| Recruitment site, No. (%) | ||||||
| Madison | 35 (22.9) | 46 (28.8) | χ2 = 1.4 (df=1) | |||
| La Crosse | 118 (77.1) | 114 (71.2) | ||||
unless otherwise noted. Missing data due to participant not responding.
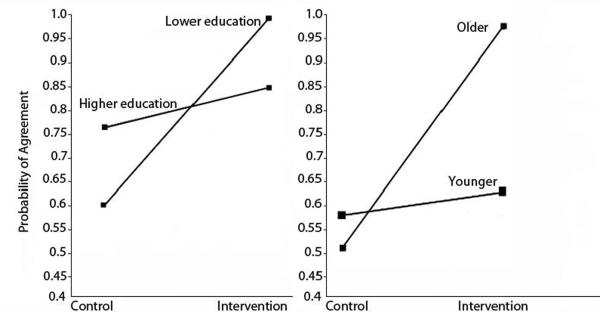
In all four expected outcome situations and in the latitude statement (amount of authority given to the surrogate) surrogates in the intervention group had significantly greater understanding of patient goals than those in the control group. The Kappas (κ) in the intervention group ranged from 0.61 to 0.78, while in the control group they ranged from 0.07 to 0.28. The odds ratio for surrogate understanding of patient goals in the expected outcome situations ranged from 2.04 to 5.57 (Table 2). For situation 1, the patient hospitalized with a serious complication and a low chance of survival, education was related to the probability of surrogate understanding of patient preferences, with those of lower educational attainment (high school education or less) having a significant increase in surrogate understanding for the intervention group over the control group (Figure 2). For situation 4, cardiopulmonary resuscitation, surrogate knowledge of ACP had an effect on surrogate knowledge of patient preferences, with surrogates with less knowledge of ACP receiving more benefit from the intervention.
Table 2.
Relationship Between Patient and Surrogate Responses on Goals of Treatment in Four Situations and Surrogate Decision-making Latitude
| Outcome Measure | Control Kappa(κ) (95% Confidence Interval) | Intervention κ (95% Confidence Interval) | Odds ratio | Probability |
|---|---|---|---|---|
| Situation | ||||
| 1. Low probability of survival | 0.28 (0.01–0.41) | 0.78 (0.67–0.89) | 5.57 | <0.001 |
| 2. Functional impairment | 0.27 (0.14–0.41) | 0.61 (0.50–0.73) | 2.04 | 0.01 |
| 3. Cognitive impairment | 0.26 (0.13–0.41) | 0.62 (0.45–0.78) | 3.34 | <0.001 |
| 4. Resuscitation | 0.26 (0.14–0.39) | 0.74 (0.65–0.83) | 4.32 | <0.001 |
| Surrogate decision-making latitude | 0.07 (−0.06–0.20) | 0.66 (0.54–0.78) | 5.41 | <0.001 |
Figure 2.
Effect of Patient Education and Patient Age on Surrogate Understanding of Patient Preferences (Agreement between Patient and Surrogate)
For situation 5, the amount of latitude in decision making that the patient wishes to give the surrogate, age was related to surrogate understanding, with older patients having a greater increase in surrogate understanding in the intervention group over the control group (Figure 3).
Knowledge of Advance Care Planning
Both patients (mean = 8.26, SD = 2.10) and surrogates (mean = 8.85, SD = 1.71) in the intervention group had significantly (p= 0.001) but only slightly higher scores in knowledge of ACP than the control patients (mean = 7.52, SD = 2.15) and surrogates (mean = 8.23, SD = 2.15).
Rating of Quality of Communication
The quality of communication tool has a 1 to 17 range. The mean intervention patient (n = 156) score was 15.9 (SD = 1.46) and the mean surrogate (n = 158) score was 16.1 (SD = 1.29).
There were no adverse effects reported by the intervention group.
DISCUSSION
A surrogate's understanding of a patient's informed choices for future medical care is critical for the surrogate to be able to make decisions that conform to the patient's goals of care. Surrogate understanding of patient goals is especially important for patients with chronic, life-limiting illnesses where critical and complex medical decision making can be expected for sudden, yet not surprising, complications.
The common ACP approach to the completion of traditional advance directives that is focused only on eliciting preferences for specific types of treatment modalities has been shown to be ineffective.22 Although it seems intuitive that the surrogates would have greater understanding of the patient's goals after an hour-long ACP discussion, most previous studies have not shown an improvement of the surrogates' understanding of the patient's preferences after a planning process.23 Those that have been effective have included elements that were incorporated into the PC-ACP interview. For example, recent research has indicated that interaction with a knowledgeable person, in this case the trained facilitator, and the opportunity to discuss individual concerns are critical to the effectiveness of ACP and AD interventions.24 Another recognized element of effective interventions, incorporated into the PC-ACP intervention, is the need for identification and correction of patient misconceptions regarding the results of treatment.25
This is the first large, multisite clinical trial that has shown a significant improvement in surrogate understanding of a patient's goals and preferences for future medical decisions. Such improved understanding is a necessary condition for better substituted decisions. Surrogate's lack of understanding of patient's preferences in the control group is of concern. For example, in the control group most surrogates did not understand the degree of latitude granted by the patient to the surrogate concerning decision making authority. Only 41.9% of the control surrogates knew the amount of latitude that the patient chose compared to 82.6% in the intervention group. Fins has found that patients often wish to give surrogates leeway in decision making and they do not always want surrogates to strictly follow their choices.26 This intervention clearly helped the surrogates to understand how the patient expects them to use the known goals and preference in decision-making. Such improvement of understanding in the intervention group was clearly superior in the other four situations as well.
Age, patient education, and surrogate knowledge of ACP had an effect on surrogate understanding of patient preferences. In situation 1, less educated patients in the intervention group demonstrated a significantly greater improvement in surrogate understanding than those in the control group, as did less knowledgeable surrogates and older patients in the intervention group in situation 5. This might indicate that older and less educated patients have a greater need for a facilitated and structured disease-specific planning discussion to improve surrogate understanding of patient goals for future medical care. It also suggests that this intervention might help address the problems of health literacy that may affect end-of-life choices.27
Finally, the quality of communication findings provide evidence that patients and surrogates in the intervention group were highly satisfied with the quality of communication in the PC-ACP interview, thus dispelling fears that these types of conversations will cause harm by creating anxiety or taking away hope.
There are several potential limitations in this study. One important limitation was the requirement that patients have a surrogate decision maker who could meet together with the facilitator. Those patients who did not have a surrogate decision maker and did not want to name a surrogate were not included. Patients who are not able to express their wishes directly and do not have a surrogate may express their wishes through a document such as a living will. Also, a number of patients agreed to participate but became too ill or died by the time an interview could be arranged with the surrogate. This group might have made different choices and had different conversations with their surrogates than those who were able to participate. We also do not know the total number of patients who might have been eligible but were not approached or refused to speak to research staff. The participants were predominantly white, so the findings cannot be generalized to other racial and ethnic groups. An additional limitation was that the La Crosse participants were in an environment in which advance care planning is standard, which may have diminished the size of the effect of the intervention on the La Crosse participants.28 There might also be regional differences in other parts of the country to which these results might not apply; patients in this study were primarily from Wisconsin and cities bordering the state. For the purposes of this study, participants chose among three options for each scenario presented. In real life, the situations are often not as clear and the options available are different from those presented. For research purposes, we could not capture such wide variation in preferences which might make a significant clinical difference. Finally, the achieved sample was only 55.9% of the projected sample needed in the power calculation. While this smaller sample did demonstrate statistically significant differences between the groups, a larger sample would be more compelling.
Patients with life-limiting illnesses, and their families who struggle with complex treatment decisions, would benefit from patient-centered, disease-specific planning. While the Statement of Treatment Preferences used in this study focused on specific scenarios and limited outcomes, the facilitated discussion provided an opportunity for the patient to express the values and beliefs that supported their choices. Surrogate knowledge of those underlying principles is an invaluable foundation for surrogate decision making using substituted judgment. It can help prepare both patients and their surrogates to better understand goals of care. This intervention shows that trained facilitators can assist patients with serious illness understand their treatment options and goals, make timely and proactive informed health care decisions, and prepare surrogates for future medical decision making, thus increasing the likelihood that a patient's goals and preferences are communicated and honored when complex treatment choices are faced.
Table 3.
Logistic Regression Models for Situation 1—Low Chance of Survival
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| Parameter (Standard Error) | Odds Ratio (Confidence Limits) | Parameter (Standard Error) | Odds Ratio (Confidence Limits) | |
| Intercept | −1.536 (1.253) | 0.22 (0.09, 2.51) | −1.194 (1.464) | 0.30 (0.02, 5.35) |
| Patient age | 0.004 (0.013) | 1.00 (0.98, 1.03) | 0.0007 (0.016) | 1.00 (0.97, 1.03) |
| Patient education level | −0.080 (0.354) | 0.92 (0.46, 1.85) | 0.457 (0.414) | 1.58 (0.70, 3.56) |
| Patient knowledge of ACP | 0.104 (0.075) | 1.11 (0.96, 1.29) | 0.080 (0.090) | 1.08 (0.91, 1.29) |
| Study site | 0.392 (0.380) | 1.48 (0.70, 3.11) | 0.374 (0.457) | 1.45 (0.59, 3.56) |
| Surrogate education | 0.062 (0.3197) | 1.06 (0.57, 1.99) | 0.121 (0.373) | 1.13 (0.54, 2.35) |
| Surrogate knowledge | 0.119 (0.074) | 1.13 (0.97, 1.30) | 0.108 (0.085) | 1.11 (0.94, 1.32) |
| Intervention group | *1.653 (0.346) | 5.22 (2.65, 10.28) | 0.123 (3.070) | 1.13 (0.003, 464.21) |
| Interaction | ||||
| Age × group | 0.015 (0.028) | 1.02 (0.96, 1.07) | ||
| Patient education × group | *−2.118 (0.808) | 0.12 (0.25, 0.59) | ||
| Patient knowledge × group | 0.040 (0.172) | 1.041 (0.74, 1.46) | ||
| Site × group | 0.104 (0.848) | 1.109 (0.21, 5.85) | ||
| Surrogate education × group | 0.115 (0.779) | 1.122 (0.24, 5.16) | ||
| Surrogate knowledge × group | 0.087 (0.177) | 1.091 (0.77, 1.54) | ||
P < .05
ACKNOWLEDGEMENTS
Financial disclosures: This study was supported by 1 R01 HS013374-01 from the Agency of Health care Research and Quality awarded to Dr. Kirchhoff. Dr. Hammes and Ms. Briggs are employed by the Gundersen Lutheran Medical Foundation, Inc. which owns the rights to the Respecting Choices® program. Dr. Kehl was supported by grant 1UL1RR025011 from the Clinical and Translational Science Award (CTSA) program of the National Center for Research Resources, National Institutes of Health during the final year of this project.
Footnotes
Presented at the 2008 National State of the Science Congress on Nursing Research, Washington, D.C. Sponsored by Council for the Advancement of Nursing Science.
Dr. Brown has no conflicts of interest. Drs. Kirchhoff, Kehl and Brown at the Madison site were responsible for data management and analysis. All authors participated in manuscript preparation and submission.
ClinicalTrials.gov Identifier: NCT00204802 http://clinicaltrials.gov/ct2/show/NCT00204802?term=advance+care+planning&rank=1
REFERENCES
- [1].Hickman SE, Hammes BJ, Moss AH, et al. Hope for the future: achieving the original intent of advance directives. Hastings Cent Rep. 2005;Spec No:S26–30. doi: 10.1353/hcr.2005.0093. [DOI] [PubMed] [Google Scholar]
- [2].Perkins HS. Controlling death: the false promise of advance directives. Ann Intern Med. 2007;147:51–57. doi: 10.7326/0003-4819-147-1-200707030-00008. [DOI] [PubMed] [Google Scholar]
- [3].Fagerlin A, Schneider CE. Enough. The failure of the living will. Hastings Cent Rep. 2004;34:30–42. [PubMed] [Google Scholar]
- [4].Jezewski MA, Brown J, Wu YW, et al. Oncology nurses' knowledge, attitudes, and experiences regarding advance directives. Oncol Nurs Forum. 2005;32:319–327. doi: 10.1188/05.onf.319-327. [DOI] [PubMed] [Google Scholar]
- [5].Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. J Am Med Assoc. 2008;300:1665–1673. doi: 10.1001/jama.300.14.1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Christakis NA. Prognostication and bioethics. Daedalus. 1999;128:197–214. [PubMed] [Google Scholar]
- [7].Shalowitz DI, Garrett-Mayer E, Wendler D. The accuracy of surrogate decision makers: a systematic review. Arch Intern Med. 2006;166:493–497. doi: 10.1001/archinte.166.5.493. [DOI] [PubMed] [Google Scholar]
- [8].Ditto PH, Danks JH, Smucker WD, et al. Advance directives as acts of communication: a randomized controlled trial. Arch Intern Med. 2001;161:421–430. doi: 10.1001/archinte.161.3.421. [DOI] [PubMed] [Google Scholar]
- [9].Matheis-Kraft C, Roberto KA. Influence of a values discussion on congruence between elderly women and their families on critical health care decisions. J Women Aging. 1997;9:5–22. doi: 10.1300/J074v09n04_02. [DOI] [PubMed] [Google Scholar]
- [10].Schwartz CE, Wheeler HB, Hammes B, et al. Early intervention in planning end-of-life care with ambulatory geriatric patients: results of a pilot trial. Arch Intern Med. 2002;162:1611–1618. doi: 10.1001/archinte.162.14.1611. [DOI] [PubMed] [Google Scholar]
- [11].Briggs LA, Kirchhoff KT, Hammes BJ, et al. Patient-centered advance care planning in special patient populations: a pilot study. J Prof Nurs. 2004;20:47–58. doi: 10.1016/j.profnurs.2003.12.001. [DOI] [PubMed] [Google Scholar]
- [12].Song MK, Kirchhoff KT, Douglas J, et al. A randomized, controlled trial to improve advance care planning among patients undergoing cardiac surgery. Med Care. 2005;43:1049–1053. doi: 10.1097/01.mlr.0000178192.10283.b4. [DOI] [PubMed] [Google Scholar]
- [13].Lyon ME, Garvie PA, McCarter R, et al. Who Will Speak for Me? Improving End-of-Life Decision-Making for Adolescents With HIV and Their Families. Pediatrics. 2009;123:e199–e206. doi: 10.1542/peds.2008-2379. [DOI] [PubMed] [Google Scholar]
- [14].Bravo G, Dubois MF, Wagneur B. Assessing the effectiveness of interventions to promote advance directives among older adults: a systematic review and multi-level analysis. Soc Sci Med. 2008;67:1122–1132. doi: 10.1016/j.socscimed.2008.06.006. [DOI] [PubMed] [Google Scholar]
- [15].Slomka J. The negotiation of death: Clinical decision making at the end of life. Soc Sci Med. 1992;35:251–259. doi: 10.1016/0277-9536(92)90021-h. [DOI] [PubMed] [Google Scholar]
- [16].Marbella AM, Desbiens NA, Mueller-Rizner N, et al. Surrogates' agreement with patients' resuscitation preferences: effect of age, relationship, and SUPPORT intervention. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. Journal of Critical Care. 1998;13:140–145. doi: 10.1016/s0883-9441(98)90018-1. [DOI] [PubMed] [Google Scholar]
- [17].Briggs L, Hammes B. Disease specific - Patient centered advance care planning (DS-ACP) manual. Gundersen Lutheran Medical Foundation, Inc.; La Crosse, WI: 2002. p. 2008. [Google Scholar]
- [18].Briggs L. Shifting the focus of advance care planning: using an in-depth interview to build and strengthen relationships. J Palliat Med. 2004;7:341–349. doi: 10.1089/109662104773709503. [DOI] [PubMed] [Google Scholar]
- [19].Donovan HS, Ward S. A representational approach to patient education. J Nurs Sch. 2001;33:211–216. doi: 10.1111/j.1547-5069.2001.00211.x. [DOI] [PubMed] [Google Scholar]
- [20].Engelberg R, Downey L, Curtis JR. Psychometric characteristics of a quality of communication questionnaire assessing communication about end-of-life care. J Palliat Med. 2006;9:1086–1098. doi: 10.1089/jpm.2006.9.1086. [DOI] [PubMed] [Google Scholar]
- [21].Curtis JR, Patrick DL, Caldwell E, et al. The quality of patient-doctor communication about end-of-life care: A study of patients with advanced AIDS and their primary care clinicians. AIDS. 1999;13:1123–1131. doi: 10.1097/00002030-199906180-00017. [DOI] [PubMed] [Google Scholar]
- [22].Rodriguez KL, Young AJ. Patients' and healthcare providers' understandings of life-sustaining treatment: are perceptions of goals shared or divergent? Social science & medicine (1982) 2006;62:125–133. doi: 10.1016/j.socscimed.2005.05.023. [DOI] [PubMed] [Google Scholar]
- [23].Wilkinson A, Wenger N, Shugaman L. Literature review on advance directives. US Department of Health and Human Services. 2007;Volume June 2007 [Google Scholar]
- [24].Jezewski MA, Meeker MA, Sessanna L, et al. The effectiveness of interventions to increase advance directive completion rates. J Aging Health. 2007;19:519–536. doi: 10.1177/0898264307300198. [DOI] [PubMed] [Google Scholar]
- [25].Fried TR, Bradley EH, Towle VR, et al. Understanding the treatment preferences of seriously ill patients. N Engl J Med. 2002;346:1061–1066. doi: 10.1056/NEJMsa012528. [DOI] [PubMed] [Google Scholar]
- [26].Fins JJ, Maltby BS, Friedmann E, et al. Contracts, covenants and advance care planning: an empirical study of the moral obligations of patient and proxy. J Pain Symptom Manage. 2005;29:55–68. doi: 10.1016/j.jpainsymman.2004.07.004. [DOI] [PubMed] [Google Scholar]
- [27].Volandes AE, Paasche-Orlow M, Gillick MR, et al. Health literacy not race predicts endof-life care preferences. J Palliat Med. 2008;11:754–762. doi: 10.1089/jpm.2007.0224. [DOI] [PubMed] [Google Scholar]
- [28].Hammes BJ, Rooney BL. Death and end-of-life planning in one midwestern community. Arch Intern Med. 1998;158:383–390. doi: 10.1001/archinte.158.4.383. [DOI] [PubMed] [Google Scholar]