Abstract
Introduction:
This study examines the relation between tobacco use and cessation with lifetime and past year mental illness in a nationally representative sample of Blacks.
Methods:
This cross-sectional study analyzed nationally representative data from 3,411 adult Blacks participating in the 2001–2003 National Survey of American Life. Smoking prevalence and quit rates according to lifetime and past year Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition mental disorders were assessed by a modified version of the Composite International Diagnostic Interview.
Results:
Compared with those without mental illness, respondents with a lifetime, past year, or past month mental illness had a higher smoking prevalence (20.6%, 35.6%, 36.0%, and 45.4%, respectively) and lower quit rate (40.5%, 31.2%, and 26.2%, respectively). The odds of being a current smoker among Blacks with mental illness in their lifetime, past year, and past month, after adjusting for age, gender, education, poverty, and marital status were 1.76 (95% CI = 1.39–2.22), 1.57 (95% CI = 1.22–2.03), and 2.20 (95% CI = 1.56–3.12), respectively. Mental illness also was associated with heavier smoking. Blacks with past year mental illness represented 18.1% of the sample, yet consumed 23.9% of cigarettes smoked by Black smokers. Past year (odds ratio [OR] = 0.72, 95% CI = 0.53–0.97) and past month (OR = 0.54, 95% CI = 0.29–0.98) mental illness were associated with a lower odds of quitting for at least 1 year.
Conclusions:
Findings indicate that mental illness is significantly associated with tobacco use in Blacks. Tobacco cessation interventions that address mental illness as a barrier to cessation are needed.
Introduction
Tobacco use remains a significant public health problem in the United States. Despite rates of tobacco use comparable to other ethnic groups, Blacks experience elevated risk for tobacco-related mortality (Centers for Disease Control and Prevention, 2009a; Horner et al., 2009; National Center for Health Statistics, 2008). The Healthy People 2010 goals for the nation are to eliminate health-related disparities that occur by race/ethnicity and reduce the prevalence of smoking to 12% by 2010 (U.S. Department of Health and Human Services, 2000). Declines in tobacco use among Blacks have stagnated, declining only 2% over the past ten years from a prevalence of 24.3% in 1999 to 22.0% in 2009 (Centers for Disease Control and Prevention, 2001, 2009b). Hence, there is a need to identify barriers to smoking cessation for Blacks.
In the general population, a strong relationship has been demonstrated between mental illness and tobacco use across a full range of psychiatric disorders (Colton & Manderscheid, 2006; Prochaska, Fromont, Hudmon, & Cataldo, 2009; Schroeder & Morris, 2010; Ziedonis et al., 2008). Epidemiological studies have documented a higher smoking prevalence, lower quit rates, and heavier smoking for persons with schizophrenia, major depression, bipolar disorder, anxiety disorder, panic attacks, posttraumatic stress disorder, alcohol abuse, and drug abuse relative to those without mental illness (Breslau, Davis, & Schultz, 2003; Grant, Hasin, Chou, Stinson, & Dawson, 2004; John, Meyer, Rumpf, & Hapke, 2009; Lasser et al., 2000). These studies have further estimated that nearly half the cigarettes sold in the United States are consumed by individuals with current mental illness (Grant et al.; Lasser et al., 2000). As a consequence, persons with mental illness are dying, on average, 25 years prematurely, with the major causes of death being tobacco-related chronic diseases (Colton & Manderscheid; Miller, Paschall, & Svendsen, 2006).
We are unaware of any epidemiological study examining the association of smoking with diagnosable psychiatric disorders by racial or ethnic group, in particular, among Blacks. The current study sought to examine the relationship between cigarette smoking and quitting among Blacks with and without mental disorders using national epidemiological data from the 2001–2003 National Survey of American Life (NSAL; Jackson, Neighbors, Nesse, Trierweiler, & Torres, 2004; Jackson, Torres, et al., 2004). The study aims were to (a) compare cigarette smoking prevalence and quit rates according to lifetime and past year Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) mental disorders in a nationally representative sample of Blacks; (b) compare the prevalence of heavier versus lighter smoking according to the number of mental disorders; and (c) examine the influence of gender, age, education, poverty status, and marital status on the relationship between mental illness and smoking. We hypothesized that Blacks with mental illness would have a higher smoking prevalence than those without mental illness, would smoke more cigarettes per day (CPD), and have lower quit rates.
Methods
Data Source
The NSAL was the first cross-sectional survey conducted to assess the national prevalence among Blacks of mental disorders, mental health service utilization, functional impairments, and protective and risk factors for mental disorders (Jackson, Neighbors, et al., 2004; Jackson, Torres, et al., 2004). Survey administration occurred between February 2, 2001 and June 30, 2003 in a random sample of households across the 48 contiguous states and the District of Columbia and became publicly available with personal identifiers removed in May 2007. The NSAL is part of the Collaborative Psychiatric Epidemiology Surveys initiative sponsored by the National Institute of Mental Health that also included the National Comorbidity Survey Replication (Kessler & Merikangas, 2004; Kessler et al., 2003; Kessler, Berglund, et al., 2004).
The NSAL includes a nationally representative sample of households, based on 2000 census data, with one self-identified Black adult aged 18 years or older collected using a stratified four-stage probability sampling method (Heeringa et al., 2004). Eligibility criteria for the NSAL included speaking and understanding English and scoring 4 or higher on the Short Portable Mental Status Questionnaire (Heeringa et al., 2004; Pennell et al., 2004; Pfeiffer, 1975). Persons recruited were community dwelling; the response rate was 71.5%. The NSAL interview averaged 145 min, and participants were compensated $50 for their time. Interviewers (N = 329, 62% Black) completed a mean of seven days of training (Pennell et al., 2004). The University of Michigan Institutional Review Board (IRB) approved the data collection, and the University of California, San Francisco IRB approved the data analyses in the current study.
The sample includes 3,411 Blacks aged 18–94 years assessed for cigarette smoking. The term “Blacks” refers to persons who self-identified as black, not Hispanic, were born in the Unites States, and had parents and grandparents also born in the United States (Jackson, Torres, et al., 2004).
Measures
Definition of Mental Disorders
Mental disorders were defined according to the DSM-IV (American Psychiatric Association, 1994). The World Health Organization’s Composite International Diagnostic Interview (CIDI) assessed mental disorders based on the diagnostic criteria in the DSM-IV (Kessler & Ustün, 2004; Kessler, Abelson, et al., 2004). The CIDI is a structured computer-delivered interview of mental disorders developed for administration by persons who are not mental health professionals (Kessler, Abelson, et al., 2004). Participants were assessed for 13 DSM-IV disorders in their lifetime, past year, and past month, including major depressive disorder, dysthymia, Bipolar I disorder, Bipolar II disorder, panic disorder, generalized anxiety disorder, posttraumatic stress disorder, agoraphobia without panic disorder, social phobia, alcohol abuse, alcohol dependence, drug abuse, and drug dependence. Too few participants met DSM-IV criteria for Bipolar II disorder for analysis by individual disorder; however, the categories for any mental illness include participants meeting criteria for Bipolar II disorder. Additionally, the NSAL did not assess the functional impairment criterion required for a DSM-IV psychotic disorder; therefore, we report on psychotic symptoms that include hallucinations and/or delusions unrelated to substance use or a medical condition. The number of lifetime disorders was tallied as none, one, two, three, or four or more. We followed the DSM-IV hierarchy criterion, which states that persons meeting criteria for alcohol abuse or drug abuse cannot also have a diagnosis of alcohol dependence or drug dependence, respectively; those meeting criteria for dysthymia or a generalized anxiety disorder cannot also have a diagnosis of a major depressive disorder; and those meeting criteria for a major depressive disorder cannot also have a diagnosis of bipolar disorder (American Psychiatric Association).
Definitions of Cigarette Smoking and Quit Rates
Never-smokers reported never having smoked 100 cigarettes. Lifetime smokers were defined as having smoked 100 or more cigarettes in one’s lifetime. Among lifetime smokers, current smokers responded affirmatively to the question, “Do you currently smoke?” and former smokers responded in the negative. Formers smokers were asked the age at which they quit smoking. Consumption was assessed by the question, “How many cigarettes per day (CPD) do you smoke?” Peak consumption was assessed by the question, “How many cigarettes did you smoke per day during the period when you were smoking the most?” Persons whose consumption was 10 or fewer CPD were classified as “lighter” smokers and those whose consumption was 11 or more CPD were classified as “heavier” smokers (Haiman et al., 2006). The quit rate was defined as the proportion of lifetime smokers who were not current smokers.
The proportion of all cigarettes smoked by Blacks with a past year mental disorder was calculated using the following formula: M1 × C1/(M2 × C2 + M1 × C1), where M1 = the number of current smokers with a past year mental disorder, C1 = the mean consumption of CPD by current smokers with a past year mental disorder, M2 = the number of current smokers without mental illness, and C2 = the mean consumption of CPD by current smokers without mental illness (Lasser et al., 2000). Values were weighted to be nationally representative. Proportions also were calculated using the CPD during peak consumption for both groups.
Analysis Strategy
We first examined the prevalence of lifetime and past year mental disorders according to demographic and socioeconomic variables. We then examined the prevalence of current smoking, lifetime smoking, and quit rates according to mental disorders and psychotic symptoms. Next, we examined the association between smoking intensity and lifetime mental disorders by comparing the prevalence of heavier and lighter smoking according to the number of lifetime mental disorders (range: none to four or more). Lastly, we ran logistic regression analyses to examine associations between lifetime, past year, and past month mental illness with current smoking status and former smoking or quit status after controlling for age, gender, poverty, education level, and marital status. We analyzed quit status for any duration and repeated the analysis for former smokers with prolonged abstinence of at least one year (Hughes et al., 2003). All logistic regression analyses controlled for gender, age, poverty status, education level, and marital status because epidemiological studies have found associations with cigarette smoking status (Centers for Disease Control and Prevention, 2009a; Tseng, Lin, Martin, Chen, & Partridge, 2010).
Prevalence estimates represent the Black adult population, and SE estimates account for the NSAL’s design-based clustering and stratification through application of weighted variables (Heeringa et al., 2004). Proc Surveyfreq and Proc Surveylogistic in SAS software version 9.2 (SAS Institute, Cary, NC) calculated weighted estimates and accounted for the design-based clustering and stratification.
Results
The prevalence of any lifetime, past year, and past month mental illness was 36.9%, 18.1%, and 4.7%, respectively. Persons with incomes below the poverty line; those with less than a high school degree; those who were divorced, separated, or widowed; and those living in the Northeast and Midwest had the highest prevalence of lifetime and past year mental illness relative to other groups (see Table 1).
Table 1.
Prevalence of DSM-IV Mental Disorders According to Demographics For Blacksa
| Demographic characteristics | Ns per demographic category | Any lifetime psychiatric disorder, % ± SE | Any past year psychiatric disorder, % ± SE |
| Total sample | 3,411 | 36.9 ± 1.2 | 18.1 ± 0.9 |
| Gender | |||
| Women | 2,202 | 38.1 ± 1.2 | 21.6 ± 1.1 |
| Men | 1,209 | 35.3 ± 1.8 | 13.6 ± 1.2 |
| Age, years | |||
| 18–24 | 473 | 36.0 ± 2.2 | 21.3 ± 2.4 |
| 25–34 | 730 | 35.5 ± 2.3 | 18.1 ± 1.9 |
| 35–44 | 810 | 39.1 ± 2.0 | 18.5 ± 1.9 |
| 45–54 | 622 | 44.0 ± 2.0 | 21.8 ± 1.6 |
| Highest education level | |||
| Some high school or less | 879 | 44.5 ± 2.0 | 24.8 ± 1.6 |
| High school degree or GED | 1,289 | 31.8 ± 1.8 | 15.8 ± 1.3 |
| Some college | 779 | 38.5 ± 2.2 | 16.5 ± 1.4 |
| College degree or greater | 464 | 34.3 ± 2.9 | 15.2 ± 2.4 |
| Federal poverty levelb | |||
| Below poverty | 642 | 43.5 ± 2.3 | 25.0 ± 1.7 |
| Above poverty | 2,769 | 35.3 ± 1.2 | 16.5 ± 0.9 |
| Marital status | |||
| Married/cohabiting | 1,174 | 31.5 ± 1.7 | 13.6 ± 1.1 |
| Divorced/separated/widowed | 1,106 | 44.9 ± 1.7 | 22.1 ± 1.4 |
| Never married | 1,131 | 37.2 ± 1.8 | 20.7 ± 1.4 |
| Region of residence | |||
| Northeast | 399 | 44.1 ± 1.7 | 20.8 ± 1.8 |
| Midwest | 542 | 45.1 ± 3.1 | 23.7 ± 3.4 |
| West | 231 | 38.4 ± 3.7 | 19.1 ± 3.1 |
| South | 2,239 | 32.0 ± 1.6 | 15.4 ± 0.9 |
Note. DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; GED = General Education Diploma.
Mental disorders are defined using the DSM-IV, as assessed by the Composite International Diagnostic Interview, administered in the National Survey of American (American Psychiatric Association, 1994; Jackson, Torres, et al., 2004; Kessler & Ustün, 2004). Estimates are weighted to be nationally representative of the Black adult population.
Federal poverty-level threshold is defined using the 2001 Federal Poverty Guidelines (U.S. Department of Health and Human Services, 2001).
For the total sample, the prevalence of current smoking was 27.7% and lifetime smoking was 42.6%. The current smoking prevalence for respondents with no mental illness was 20.6% compared with 35.6% for those with a lifetime mental illness, 36.0% for those with a past year mental illness, and 45.4% for those with a past month mental illness. The lifetime smoking prevalence for respondents with no mental illness was 34.6% compared with 51.7% for those with a lifetime mental illness, 48.8% for those with a past year mental illness, and 57.9% for those with a past month mental illness.
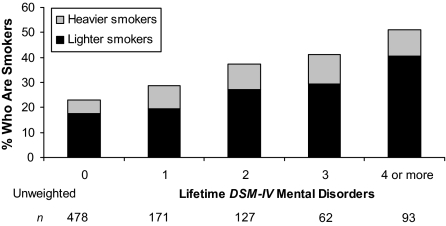
Table 2 summarizes the smoking prevalence and quit rates according to mental disorders in the lifetime and past year. Parallel analyses were not run for past month mental disorders given the small sample sizes. For all disorders assessed except lifetime dysthymia, meeting criteria for a mental disorder in one’s lifetime or past year was associated with higher current and lifetime smoking prevalence and lower quit rates relative to smokers with no mental illness. A dose–response relationship was found between the number of lifetime mental disorders and the prevalence of heavier and lighter smoking (see Figure 1).
Table 2.
Smoking Prevalence and Quit Rates According to Lifetime and Past Year DSM-IV Mental Disorders For Blacks (N = 3,411)a
| Smoking status according to lifetime disorders |
Smoking status according to past year disorders |
|||||
| Psychiatric disorders | Current smoker, % ± SE | Lifetime smokerb, % ± SE | Quit ratec, % ± SE | Current smoker, % ± SE | Lifetime smokerb, % ± SE | Quit ratec, % ± SE |
| No mental illness | 23.1 ± 1.2 | 37.2 ± 1.1 | 37.9 ± 2.1 | 25.9 ± 1.0 | 41.2 ± 1.0 | 37.2 ± 1.6 |
| Mood disorders | ||||||
| Major depressive disorder | 34.4 ± 2.6 | 48.7 ± 2.6 | 29.5 ± 4.5 | 33.4 ± 3.9 | 43.0 ± 4.1 | 22.1 ± 5.2 |
| Dysthymia | 32.3 ± 5.6 | 53.4 ± 5.4 | 39.6 ± 10.5 | 28.1 ± 4.4 | 41.8 ± 5.8 | 32.8 ± 10.8 |
| Bipolar I disorder | 71.2 ± 8.3 | 76.5 ± 6.5 | 7.0 ± 3.9 | 67.8 ± 10.0 | 73.5 ± 8.6 | 7.8 ± 5.4 |
| Anxiety disorders | ||||||
| Panic disorder | 43.5 ± 6.0 | 56.1 ± 5.2 | 22.4 ± 6.0 | 41.6 ± 6.4 | 55.7 ± 5.9 | 25.3 ± 7.8 |
| Generalized anxiety disorder | 40.8 ± 5.7 | 55.9 ± 5.6 | 27.1 ± 6.7 | 36.9 ± 8.1 | 54.0 ± 8.5 | 31.7 ± 9.8 |
| Posttraumatic stress disorder | 36.6 ± 3.7 | 50.6 ± 3.7 | 27.6 ± 4.8 | 40.8 ± 5.4 | 55.2 ± 5.8 | 26.1 ± 8.0 |
| Agoraphobia without panic disorder | 35.1 ± 8.0 | 50.2 ± 9.7 | 30.0 ± 6.6 | 42.8 ± 10.0 | 54.3 ± 8.6 | 21.2 ± 8.9 |
| Social phobia | 32.0 ± 3.3 | 46.5 ± 3.6 | 31.2 ± 5.5 | 34.1 ± 4.3 | 48.9 ± 4.5 | 30.2 ± 6.7 |
| Substance disorders | ||||||
| Alcohol abuse | 58.1 ± 4.5 | 81.0 ± 2.6 | 28.3 ± 4.5 | 61.5 ± 8.7 | 71.9 ± 8.7 | 14.4 ± 6.3 |
| Alcohol dependence | 55.5 ± 4.7 | 84.2 ± 3.0 | 34.1 ± 5.6 | 71.8 ± 5.3 | 81.3 ± 5.4 | 11.6 ± 4.6 |
| Drug abuse | 25.4 ± 0.9 | 85.3 ± 2.4 | 25.9 ± 3.3 | 50.6 ± 12.2 | 62.6 ± 12.6 | 19.0 ± 9.9 |
| Drug dependence | 61.3 ± 6.7 | 89.4 ± 3.2 | 31.4 ± 6.4 | 76.8 ± 9.3 | 81.3 ± 8.6 | 5.5 ± 5.4 |
| Psychotic symptoms | 33.0 ± 2.7 | 50.6 ± 3.3 | 34.7 ± 3.9 | 30.6 ± 3.8 | 48.5 ± 3.8 | 36.9 ± 5.7 |
| Any lifetime disorder | 35.6 ± 1.7 | 51.7 ± 1.5 | 31.2 ± 2.3 | 36.0 ± 2.0 | 48.8 ± 2.1 | 26.2 ± 2.9 |
Note. DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition.
Mental disorders are defined using the DSM-IV, as assessed by the Composite International Diagnostic Interview, administered in the National Survey of American Life (American Psychiatric Association, 1994; Jackson, Torres, et al., 2004; Kessler & Ustün, 2004). Estimates are weighted to be nationally representative of the Black adult population.
Lifetime smokers are defined as smoking more than 100 cigarettes in one’s lifetime.
Quit rate is the proportion of lifetime smokers who did not smoke when interviewed.
Figure 1.
Smoking prevalence and intensity according to the number of lifetime mental disorders for Blackss. Mental disorders are defined using the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), as assessed by the Composite International Diagnostic Interview, administered in the National Survey of American Life (American Psychiatric Association, 1994; Jackson, Torres, et al., 2004; Kessler & Ustun, 2004). Estimates are weighted to be nationally representative of the Black adult population. Heavier smokers are defined as smoking 11 or more cigarettes per day (CPD). Lighter smokers are defined as smoking 10 or fewer CPD (Haiman et al., 2006).
Current smokers with mental illness in the past year (weighted n = 1,420,284) had a mean consumption of 9.6 CPD and consumed 23.9% of cigarettes smoked by Black smokers. For current smokers, there was a positive correlation between current CPD and CPD during peak consumption, r = .42, n = 931, p < .001. To replicate the method of Lasser et al. (2000), the formula also was calculated using unweighted frequencies and CPD during peak consumption, yielding an estimate that those with past year mental illness consumed 28.2% of cigarettes smoked by Blacks.
Logistic regression analyses found that lifetime, past year, and past month mental illness were all significantly associated with current smoking status after controlling for age, gender, poverty, education level, and marital status (Table 3). The covariates of gender, education, and marital status also were significant; age and poverty were not significant.
Table 3.
Logistic Regression Analyses Predicting Current Smoking From Mental Illness For Blacks, Adjusting For Demographics
| Lifetime mental Illness |
Past year mental illness |
Past month mental illness |
||||
| ORs | 95% CI | ORs | 95% CI | ORs | 95% CI | |
| Any mental illnessa | ||||||
| No (reference) | 1.00 | 1.00 | 1.00 | |||
| Yes | 1.76 | 1.39–2.22 | 1.57 | 1.22–2.03 | 2.20 | 1.56–3.12 |
| Age, per year | 0.99 | 0.99–1.00 | 0.99 | 0.99–1.00 | 0.99 | 0.99–1.00 |
| Gender | ||||||
| Women (reference) | 1.00 | 1.00 | 1.00 | |||
| Men | 1.60 | 1.30–1.95 | 1.64 | 1.34–2.01 | 1.61 | 1.32–1.97 |
| Poverty | ||||||
| Above (reference) | 1.00 | 1.00 | 1.00 | |||
| Below | 0.81 | 0.61–1.06 | 0.80 | 0.61–1.04 | 0.77 | 0.60–1.02 |
| Education | ||||||
| College degree or more (reference) | 1.00 | 1.00 | 1.00 | |||
| No high school degree | 2.72 | 1.86–3.97 | 2.73 | 1.87–3.97 | 2.76 | 1.89–4.03 |
| High school degree or GED | 1.70 | 1.15–2.49 | 1.65 | 1.13–2.41 | 1.66 | 1.14–2.44 |
| Some college | 1.53 | 1.02–2.28 | 1.55 | 1.05–2.30 | 1.56 | 1.06–2.32 |
| Marital status | ||||||
| Never married (reference) | 1.00 | 1.00 | 1.00 | |||
| Married/cohabitating | 1.36 | 1.05–1.75 | 1.36 | 1.06–1.76 | 1.36 | 1.06–1.76 |
| Separated/divorced/widowed | 1.54 | 1.21–1.97 | 1.63 | 1.27–2.08 | 1.65 | 1.30–2.09 |
Note. DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; ORs = odds ratios; GED = General Education Diploma.
Consists of psychotic symptoms and the following DSM-IV disorders: major depressive disorder, dysthymia, bipolar disorder, panic disorder, generalized anxiety disorder, posttraumatic stress disorder, agoraphobia without panic disorder, social phobia, alcohol abuse, alcohol dependence, drug abuse, and drug dependence (American Psychiatric Association, 1994).
We ran a similar model to examine associations with quit status. For the full sample, former smokers reported being quit for an average of 13.6 years (SD = 0.68, range: <1 to 65 years). The majority of former smokers (91.7%) had quit for at least one year. Logistic regression analyses found that neither lifetime (odds ratio [OR] = 0.89, 95% CI = 0.67–1.20), past year (OR = 0.76, 95% CI = 0.54–1.07), or past month (OR = 0.58, 95% CI = 0.29–1.13) mental illness were significantly associated with quit status after controlling for age, gender, poverty, education level, and marital status. Only older age was significantly associated (OR = 1.05, 95% CI = 1.04–1.06) with an increased odds of quitting. We repeated the models defining quitting as being abstinent for ≥1 year and found that past year (OR = 0.72, 95% CI = 0.53–0.97) and past month mental illness (OR = 0.54, 95% CI = 0.29–0.98) were significantly associated with a lower odds of quitting, while lifetime mental illness was not associated with prolonged quit status (OR = 0.81, 95% CI = 0.62–1.07).
Discussion
The current findings indicate that Blacks with mental illness have a higher smoking prevalence and lower quit rate than Blacks with no mental illness, consistent with prior investigations in the general population (Grant et al., 2004; Lasser et al., 2000). Relative to those without mental illness, a higher smoking prevalence was found for 12 diagnosed mental disorders and psychotic symptoms, both assessed for lifetime and past year. Lower quit rates were found for all but one of the disorders (lifetime diagnosis of dysthymia). Furthermore, a dose–response relationship was found between the number of lifetime mental disorders and smoking prevalence as well as the prevalence of heavier smoking. That is, persons with multiple mental disorders had a higher smoking prevalence and were more likely to smoke heavily relative to those with none or only one mental disorder. Mental illness in one’s lifetime, past year, or past month remained significant correlates of current smoking after controlling for demographic characteristics.
We did not find an association between current quit status of any duration and lifetime mental illness, a finding consistent with meta-analysis of the literature of Hitsman, Borrelli, McChargue, Spring, and Niaura (2003), which found no differences in either short-term or long-term abstinence (defined as six months or greater) between smokers positive versus negative for a history of depression. In the current study, however, when prolonged quit status, defined as being quit for at least one year, was examined, both past month and past year mental illness were associated with a lower likelihood of being quit. Hughes and Kalman (2006) in their systematic review of the relationship between alcohol and tobacco use concluded that individuals with current and past alcohol problems were less likely to be former smokers.
The current study did not find an association between poverty with current smoking, which for a Black sample is not surprising. Other studies also have found no association between poverty and current smoking for Blacks (Kendzor et al., 2010; Klonoff & Landrine, 2001; Landrine & Klonoff, 2000). Furthermore, the lack of a relationship between poverty and smoking could have occurred because of the skewed distribution of Blacks with income above and below the federal poverty level; 81.2% of Blacks in our study had income above the federal poverty level. Fewer Blacks in our study (18.8%) had income below the federal poverty level compared with epidemiological data (24.7%) from the U.S. Census Bureau (DeNavas-Walt, Proctor, & Smith, 2009).
Several limitations warrant mention. The first is that findings may not generalize to all Blacks in the U.S. population because, like other large epidemiological studies (Grant et al., 2004; Lasser et al., 2000), the NSAL sampling method excluded Blacks who were homeless or living in institutional settings, such as jails, prisons, military bases, nursing homes, and long-term residential medical care facilities. In 2003, it was estimated that 10.4% of Black men aged 25–29 years were incarcerated in federal and state prisons (Harrison & Beck, 2004). Furthermore, Black men and women have served in the U.S. military in numbers greater than their percent of the population (U.S. Department of Defense, 2006). The second limitation, again similar to other epidemiological studies (Kessler, Berglund, et al., 2004; Lasser et al., 2000), is that the frequency of current cigarette consumption (i.e., daily vs. nondaily smoking) was not specified. Though the study had a large overall sample size, limited prevalence of Bipolar II and past month mental illness resulted in our not being able to examine associations with tobacco use and resulted in large SEs for estimates of dysthymia, which may account for the disparate finding of a higher tobacco quit rate for individuals with lifetime dysthymia.
The current study’s estimates of lifetime (36.9%), past year (18.1%), and past month (4.7%) mental illness are lower than those reported in the literature for the general U.S. population: 46.4%–48.0% for lifetime, 21%–29.5% for past year, and 17.1%–28.3% for past month (Kessler, Chiu, Demler, Merikangas, & Walters, 2005; Kessler et al., 1994; Kessler, Berglund, et al., 2005; Lasser et al., 2000; U.S. Department of Health and Human Services, 1999; WHO International Consortium in Psychiatric Epidemiology, 2000). The lower estimates in the current study may be due to either real or artifact racial differences. Studies of Kessler et al. have found that Blacks have a lower prevalence of lifetime and past year mental disorders than Whites (Kessler et al., 1994; Kessler, Chiu, et al., 2005).
We are unaware of prior studies examining smoking prevalence according to DSM-IV mental disorders using a nationally representative sample of Blacks. Blacks with mental illness had higher rates of smoking and lower quit rates. Black smokers with mental illness may be a particularly vulnerable group at risk for discrimination and stigma due to their race, use of tobacco, and mental illness. The cessation literature has reported challenges in obtaining long-term quit rates for Blacks (Froelicher, Doolan, Yerger, McGruder, & Malone, 2010; Webb, 2008; Webb, de Ybarra, Baker, Reis, & Carey, 2010). Effective tobacco cessation interventions are needed (Fagan et al., 2004). Traditional quit smoking programs generally have not addressed mental illness as a barrier to cessation (Fiore et al., 2008). Similarly, traditional mental health settings largely have ignored tobacco as a treatment target (Hall & Prochaska, 2009). The current findings underscore the need for greater integration.
Funding
This work was supported by the State of California Tobacco-Related Disease Research Program (grant number 13KT-0152), the National Institute on Drug Abuse (grant numbers K23 DA018691 and P50 DA09253), the National Institute of Mental Health (grant number R01 MH083684), and the National Cancer Institute (grant number 5R25 CA113710).
Declaration of Interests
None declared.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed., DSM-IV) Washington, DC: Author; 1994. [Google Scholar]
- Breslau N, Davis GC, Schultz LR. Posttraumatic stress disorder and the incidence of nicotine, alcohol, and other drug disorders in persons who have experienced trauma. Archives of General Psychiatry. 2003;60:289–294. doi: 10.1001/archpsyc.60.3.289. doi:10.1001/archpsyc.60.3.289. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Cigarette smoking among adults-United States, 1999. Morbidity and Mortality Weekly Report. 2001;50:1227–1232. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5040a1.htm. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Cigarette smoking among adults and trends in smoking cessation-United States, 2008. Morbidity and Mortality Weekly Report. 2009a;58:1227–1232. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5844a2.htm. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Prevalence of current smoking among adults aged 18 years and over: United States, 1997–June 2009. 2009b. Early release of selected estimates based on data from the January–June 2009 National Health Interview Survey. Retrieved from http://www.cdc.gov/nchs/data/nhis/earlyrelease/earlyrelease200912.pdf. [Google Scholar]
- Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Preventing Chronic Disease. 2006;3:1–14. Retrieved from http://www.cdc.gov/pcd/issues/2006/apr/05_0180.htm. [PMC free article] [PubMed] [Google Scholar]
- DeNavas-Walt C, Proctor BD, Smith JC. Income, poverty, and health insurance coverage in the United States: 2008. U.S. Census Bureau. Current Population Reports. 2009. pp. P60–P236. Retrieved from http://www.census.gov/hhes/www/poverty/data/incpovhlth/2008/highlights.html. [Google Scholar]
- Fagan P, King G, Lawrence D, Petrucci SA, Robinson RG, Banks D, et al. Eliminating tobacco-related health disparities: Directions for future research. American Journal of Public Health. 2004;94:211–217. doi: 10.2105/ajph.94.2.211. doi:10.2105/AJPH.94.2.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiore MC, Jaén CR, Baker TB, Bailey WC, Benowitz N, Curry SJ, et al. Treating tobacco use and dependence: 2008 Update. Quick reference guide for clinicians. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service; 2009. [Google Scholar]
- Froelicher ES, Doolan D, Yerger VB, McGruder CO, Malone RE. Combining community participatory research with a randomized clinical trial: The Protecting the Hood Against Tobacco (PHAT) smoking cessation study. Heart Lung. 2010;39:50–63. doi: 10.1016/j.hrtlng.2009.06.004. doi:10.1016/j.hrtlng.2009.06.004. [DOI] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Chou SP, Stinson FS, Dawson DA. Nicotine dependence and psychiatric disorders in the United States: Results from the national epidemiologic survey on alcohol and related conditions. Archives of General Psychiatry. 2004;61:1107–1115. doi: 10.1001/archpsyc.61.11.1107. doi:10.1001/archpsyc.61.11.1107. [DOI] [PubMed] [Google Scholar]
- Haiman CA, Stram DO, Wilkens LR, Pike MC, Kolonel LN, Henderson BE, et al. Ethnic and racial differences in the smoking-related risk of lung cancer. New England Journal of Medicine. 2006;354:333–342. doi: 10.1056/NEJMoa033250. doi:10.1056/NEJMoa033250. [DOI] [PubMed] [Google Scholar]
- Hall SM, Prochaska JJ. Treatment of smokers with co-occurring disorders: Emphasis on integration in mental health and addiction treatment settings. Annual Review of Clinical Psychology. 2009;5:409–431. doi: 10.1146/annurev.clinpsy.032408.153614. doi:10.1146/annurev.clinpsy.032408.153614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison PM, Beck AJ. Prisoners in 2003. Bureau of Justice Statistics Bulletin, NCJ 205335, 1-12. 2004. Retrieved from http://bjs.ojp.usdoj.gov/content/pub/pdf/p03.pdf. [Google Scholar]
- Heeringa SG, Wagner J, Torres M, Duan N, Adams T, Berglund P. Sample designs and sampling methods for the Collaborative Psychiatric Epidemiology Studies (CPES) International Journal of Methods in Psychiatric Research. 2004;13:221–240. doi: 10.1002/mpr.179. doi:10.1002/mpr.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hitsman B, Borrelli B, McChargue DE, Spring B, Niaura R. History of depression and smoking cessation outcome: A meta-analysis. Journal of Consulting & Clinical Psychology. 2003;71:657–663. doi: 10.1037/0022-006x.71.4.657. doi:10.1037/0022-006X.71.4.657. [DOI] [PubMed] [Google Scholar]
- Horner MJ, Ries LAG, Krapcho M, Neyman N, Aminou R, Howlader N, et al. SEER cancer statistics review, 1975–2006. Bethesda, MD: National Cancer Institute; 2009. Retrieved from http://seer.cancer.gov/csr/1975_2006/ [Google Scholar]
- Hughes JR, Kalman D. Do smokers with alcohol problems have more difficulty quitting? Drug and Alcohol Dependence. 2006;82:91–102. doi: 10.1016/j.drugalcdep.2005.08.018. doi:10.1016/j.drugalcdep.2005.08.018. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Keely JP, Niaura RS, Ossip-Klein DJ, Richmond RL, Swan GE. Measures of abstinence in clinical trials: Issues and recommendations. Nicotine & Tobacco Research. 2003;5:13–25. doi:10.1080/1462220031000070552. [PubMed] [Google Scholar]
- Jackson JS, Neighbors HW, Nesse RM, Trierweiler SJ, Torres M. Methodological innovations in the National Survey of American Life. International Journal of Methods in Psychiatric Research. 2004;13:289–298. doi: 10.1002/mpr.182. doi:10.1002/mpr.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson JS, Torres M, Caldwell CH, Neighbors HW, Nesse RM, Taylor RJ, et al. The national survey of American life: A study of racial, ethnic and cultural influences on mental disorders and mental health. International Journal of Methods in Psychiatric Research. 2004;13:196–207. doi: 10.1002/mpr.177. doi:10.1002/mpr.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John U, Meyer C, Rumpf HJ, Hapke U. Nicotine dependence criteria and nicotine withdrawal symptoms in relation to pain among an adult general population sample. European Journal of Pain. 2009;13:82–88. doi: 10.1016/j.ejpain.2008.03.002. doi:10.1016/j.ejpain.2008.03.002. [DOI] [PubMed] [Google Scholar]
- Kendzor DE, Businelle MS, Costello TJ, Castro Y, Reitzel LR, Cofta-Woerpel LM, et al. Financial strain and smoking cessation among racially/ethnically diverse smokers. American Journal of Public Health. 2010;100:702–706. doi: 10.2105/AJPH.2009.172676. doi:10.2105/ajph.2009.172676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Abelson J, Demler O, Escobar JI, Gibbon M, Guyer ME, et al. Clinical calibration of DSM-IV diagnoses in the World Mental Health (WMH) version of the World Health Organization (WHO) Composite International Diagnostic Interview (WMHCIDI) International Journal of Methods in Psychiatric Research. 2004;13:122–139. doi: 10.1002/mpr.169. doi:10.1002/mpr.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Chiu WT, Demler O, Heeringa S, Hiripi E, et al. The US National Comorbidity Survey Replication (NCS-R): Design and field procedures. International Journal of Methods in Psychiatric Research. 2004;13:69–92. doi: 10.1002/mpr.167. doi:10.1002/mpr.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, et al. The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R) Journal of the American Medical Association. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. doi:10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. doi:10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. doi:10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Archives of General Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Merikangas KR. The National Comorbidity Survey Replication (NCS-R): Background and aims. International Journal of Methods in Psychiatric Research. 2004;13:60–68. doi: 10.1002/mpr.166. doi:10.1002/mpr.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Ustün TB. The World Mental Health (WMH) Survey Initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) International Journal of Methods in Psychiatric Research. 2004;13:93–121. doi: 10.1002/mpr.168. doi:10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klonoff EA, Landrine H. Depressive symptoms and smoking among US Black Adults: Absence of a Relationship. Journal of Health Psychology. 2001;6:645–649. doi: 10.1177/135910530100600603. doi:10.1177/135910530100600603. [DOI] [PubMed] [Google Scholar]
- Landrine H, Klonoff EA. Racial segregation and cigarette smoking among blacks: Findings at the individual level. Journal of Health Psychology. 2000;5:211–219. doi: 10.1177/135910530000500211. doi:10.1177/135910530000500211. [DOI] [PubMed] [Google Scholar]
- Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: A population-based prevalence study. Journal of the American Medical Association. 2000;284:2606–2610. doi: 10.1001/jama.284.20.2606. doi:10.1001/jama.284.20.2606. [DOI] [PubMed] [Google Scholar]
- Miller BJ, Paschall CB, III, Svendsen DP. Mortality and medical comorbidity among patients with serious mental illness. Psychiatric Services. 2006;57:1482–1487. doi: 10.1176/ps.2006.57.10.1482. doi:10.1176/appi.ps.57.10.1482. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. Health, United States, 2008, with chartbook on trends in the health of Americans. Hyattsville, MD: Government Printing Office; 2008. Retrieved from http://www.cdc.gov/nchs/data/hus/hus08.pdf. [Google Scholar]
- Pennell BE, Bowers A, Carr D, Chardoul S, Cheung GA, Dinkelmann K, et al. The development and implementation of the National Comorbidity Survey Replication, the National Survey of American Life, and the National Latino and Asian American Survey. International Journal of Methods in Psychiatric Research. 2004;13:241–269. doi: 10.1002/mpr.180. doi:10.1002/mpr.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. Journal of American Geriatrics Society. 1975;23:433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- Prochaska JJ, Fromont SC, Hudmon KS, Cataldo JK. Designing for dissemination: Development of an evidence-based tobacco treatment curriculum for psychiatry training programs. Journal of the American Psychiatric Nurses Association. 2009;15:24–31. doi: 10.1177/1078390308329536. doi:10.1177/1078390308329536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schroeder SA, Morris CD. Confronting a neglected epidemic: Tobacco cessation for persons with mental illness and substance abuse problems. Annual Review of Public Health. 2010;31:16.1–16.8. doi: 10.1146/annurev.publhealth.012809.103701. doi:10.1146/annurev.publhealth.012809.103701. [DOI] [PubMed] [Google Scholar]
- Tseng TS, Lin HY, Martin MY, Chen T, Partridge EE. Disparities in smoking and cessation status among cancer survivors and non-cancer individuals: A population-based study from National Health and Nutrition Examination Survey. Journal of Cancer Survivorship. 2010 doi: 10.1007/s11764-010-0127-9. Epub ahead of print May 13; doi:10.1007/s11764-010-0127-9. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Defense. Population representation in the military services: Fiscal Year 2004. Washington, DC: Office of the Under Secretary of Defense, Personnel and Readiness; 2006. Retrieved from http://prhome.defense.gov/MPP/ACCESSION%20POLICY/poprep2004/download/2004report.pdf. [Google Scholar]
- U.S. Department of Health and Human Services. Mental health: A report of the Surgeon General-executive summary. Rockville, MD: Author, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health; 1999. [Google Scholar]
- U.S. Department of Health and Human Services. Healthy People 2010. With understanding and improving health objectives for improving health. 2nd ed. Washington, DC: Government Printing Office; 2000. Retrieved from http://www.healthypeople.gov/Document/tableofcontents.htm#parta. [Google Scholar]
- U.S. Department of Health and Human Services. The 2001 HHS poverty guidelines. Federal Register. 2001;66:10695–10697. Retrieved from http://aspe.hhs.gov/poverty/01poverty.htm. [Google Scholar]
- Webb MS. Treating tobacco dependence among African Americans: A meta-analytic review. Health Psychology. 2008;27(3 Suppl):S271–S282. doi: 10.1037/0278-6133.27.3(suppl.).s271. doi:10.1037/0278-6133.27.3(Suppl.).S271. [DOI] [PubMed] [Google Scholar]
- Webb MS, de Ybarra DR, Baker EA, Reis IM, Carey MP. Cognitive- behavioral therapy to promote smoking cessation among African American smokers: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 2010;78:24–33. doi: 10.1037/a0017669. doi:10.1037/a0017669. [DOI] [PubMed] [Google Scholar]
- WHO International Consortium in Psychiatric Epidemiology. Cross-national comparisons of the prevalences and correlates of mental disorders. Bulletin of the World Health Organization. 2000;78:413–426. [PMC free article] [PubMed] [Google Scholar]
- Ziedonis D, Hitsman B, Beckham JC, Zvolensky M, Adler LE, Audrain-McGovern J, et al. Tobacco use and cessation in psychiatric disorders: National Institute of Mental Health report. Nicotine & Tobacco Research. 2008;10:1691–1715. doi: 10.1080/14622200802443569. doi:10.1080/14622200802443569. [DOI] [PubMed] [Google Scholar]