Abstract
Introduction:
This study, informed by ecological frameworks, compared the prevalence, predictors, and association of home smoking restrictions with secondhand smoke exposure (SHSe) between Koreans in Seoul, South Korea, and Korean Americans in California, United States.
Methods:
A cross-sectional survey was drawn from telephone interviews with Korean adults in Seoul (N = 500) and California (N = 2,830) during 2001–02. Multivariable regressions were used for analyses.
Results:
Koreans, compared with Korean Americans, had significantly fewer complete home smoking bans, 19% (95% CI: 16–23) versus 66% (95% CI: 64–68), and were more likely to not have a home smoking restriction, 64% (95% CI: 60–69) versus 5% (95% CI: 4–6). Home smoking restrictions were associated with lower home SHSe; however, the impact was consistently larger among Korean Americans. Households with more SHSe sources were less likely to have the strongest home smoking restrictions, where the difference in complete bans among Korean Americans versus Koreans was largely among those at low risk of SHSe, 82% (95% CI: 76–86) versus 36% (95% CI: 17–57), while high-risk Korean American and Koreans had similar low probabilities, 10% (95% CI: 7–13) versus 7% (95% CI: 3–13).
Conclusions:
Consistent with ecological frameworks, exposure to California’s antismoking policy and culture was associated with stronger home smoking restrictions and improved effectiveness. Interventions tailored to Korean and Korean American SHSe profiles are needed. Behavioral interventions specifically for high-risk Korean Americans and stronger policy controls for Koreans may be effective at rapidly expanding home smoking restrictions.
Introduction
Ecological frameworks assume that societal structures have mediating and moderating, in addition to direct, impacts on secondhand smoke exposure (SHSe; Bronfenbrenner, 1977; Glass & McAtee, 2006; Hovell & Hughes, 2009; McLeroy, Bibeau, Steckler, & Glanz, 1988). Exposure to formal tobacco control policies and antismoking cultures may promote home smoking restrictions (mediation), and where in place, restrictions may be more effective when embedded in antitobacco social structures (moderation). These ecologic deductions are exemplified through comparison of the disparate tobacco control and smoking cultures among Koreans in Seoul, South Korea, and Korean Americans in California, United States.
The South Korean tobacco market originated in government monopolies, where most of the market remains and few policies restrict consumption (Corrao, Guindon, Sharma, & Shokoohi, 2000; Do & Park, 2009; Kang et al., 2003). Smoking is often a status symbol among Koreans, especially men (Cho, Khang, Jun, & Kawachi, 2008; Lee, 2003). California, on the other hand, has been at the forefront of antismoking activism beginning in 1977 (Bayer & Colgrove, 2002) developing into the California Tobacco Control Program (CTCP; Gilpin et al., 2004). Californians are also considered the most hostile to smoking in the United States (Alamar & Glantz, 2006).
The mediation ecological deduction suggests that the larger environment alters the occurrence of proximal determinants—those occurring conceptually closer to the individual. South Korean sociopolitical norms may place nonsmokers, mostly women and children, in positions where they cannot protect themselves. About 54% of Korean nonsmoking women had smoking husbands, and these women developed lung cancer at double the rates of those married to never-smokers (Jee, Ohrr, & Kim, 1999), likely a reflection of limited smoking restrictions. Estimates suggest that 65% of Korean homes have no home smoking restriction, and only 19% have a complete home smoking ban (Hughes, Hovell, et al. 2008; Hughes et al. 2009). Taking on California norms likely increases the focus on self-preservation, encourages equitable relationships (Markus & Kitayama, 1991; Min, 2001), and renders smoking less common (Ji et al., 2005; Zhu, Wong, Tang, Shi, & Chen, 2007). In the context of California’s antismoking culture, instituting home smoking restrictions may be easier. We hypothesize (H1) that home smoking policies will be more restrictive among Korean Americans than among Koreans.
Research among diverse populations documents a consistent association between harsher home smoking restrictions and lower SHSe (Martinez-Donate, Johnson-Kozlow, Hovell, & Gonzalez Perez, 2009; Pizacani et al., 2003), particularly among children (Spencer, Blackburn, Bonas, Coe, & Dolan, 2005); this relationship appears to hold for Koreans (Hughes et al., 2008; Hughes et al., 2008) and Korean Americans (Hughes, Corcos, Hofstetter, Hovell, & Irvin, 2008). However, the relative effectiveness of home smoking restrictions may be contingent on the social structures they are embedded in, the moderating ecologic deduction. Asian cultures are hierarchical (Markus & Kitayama, 1991), and smoking men often have power over nonsmokers (Jee et al., 1999). Immigration may empower Korean Americans to enforce smoking restrictions. Some of our earlier analyses allude to this dynamic: Korean male smokers are very resistant to others’ requests to limit smoking (Ayers, Hofstetter, Hughes, et al., 2010), while Korean American men expect and cease in the face of social reprimand (Hofstetter, Hovell, et al., 2010). Similarly, strong tobacco control policies, largely enforced by peers and not the police (Jacobson & Wasserman, 1999), provide a set of models Korean Americans can imitate in their home. We hypothesize (H2) that home smoking restrictions will be more effective at reducing SHSe among Korean Americans than among Koreans.
The patterns between home smoking restrictions and SHSe are complicated by suggestions that home smoking restrictions arise from microsocial contexts where smoking is rare and individuals need less protection (Hughes et al., 2009; Ji et al., 2009; Winickoff et al., 2009). Unfortunately, most prior work focused on the head of household or the study subject’s smoking. In this report, we document a more complete perspective of these processes using social network data on familial smoking and descriptors of friends’ smoking to evaluate the relative presence of the harshest home smoking restrictions across levels of SHSe risk. These analyses inform our earlier hypotheses of which Korean and Korean Americans uptake home smoking restrictions by investigating the SHSe risk of those with and without restrictions.
Methods
The survey instruments were developed in English and translated into Korean with the assistance of coinvestigators in Seoul and California. The English–Korean translation process was repeated, including formative focus groups, to assess translations and optimize isomorphism between concepts.
Random digit dialing procedures were used in Seoul with telephone interviews administered to 500 adults stratified by telephone district. California interviews were based on all residential telephones linked to Korean surnames. Numbers were purchased from a firm that aggregated from a variety of sources that included listed, unlisted, and cell phone numbers. The list was purged of persons who had Asian but not Korean first names with Anglicized first names retained (N = 108,843). The list was sorted into random order before calling began, and 2,830 interviews were administered. In both the Seoul and the California samples, respondents within households were randomly selected using the “most recent birthday” procedure (Frey, 1983) and filtered to ensure they were Korean.
Seoul interviews were conducted by trained graduate students at Myongi University under the supervision of a project coinvestigator during Summer and Fall of 2002. Up to five callbacks were made to each residence until interviews were completed, the targeted respondent refused the interview, or the number was found to be nonresidential. The cooperation rate, 41%, was comparable with meta-analysis, suggesting a mean cooperation rate of 48% (SD = 20; Baruch, 1999). All Seoul interviews were conducted in Korean.
California interviews were conducted by professional interviewers who were bilingual in English and Korean under the supervision of the interview supervisor at the Center for Behavioral Epidemiology and Community Health. Interviewers keyed on the phone answering language, which was very often Korean, but asked language preference before initiating interviews. Up to seven callbacks were used and a specially trained skilled interviewer attempted to convert refusals. The cooperation rate was high, with approximately 86% of all eligible respondents completing interviews. About 85% of interviews were conducted in Korean. Figure 1A and 1B show the sample dispositions. The Institutional Review Boards at San Diego State and Myongji University approved study procedures.
Figure 1.
(A) California Sample. (B) Seoul Sample. Disposition of the samples ineligible includes non-Koreans, business numbers, and persons who speak neither English nor Korean. Other includes disconnected numbers, machines, no answer after seven attempts (five in Seoul, Korea), and line busy through seven (five) attempts.
Measures
Adult and Childrens’ SHSe
Respondents estimated the number of cigarettes to which they and their “most exposed” child were exposed in the home on a “typical day,” dummy coded into any exposure. Similar measures have demonstrated satisfactory validity (Hovell, Zakarian, Wahlgren, Matt, & Emmons, 2000; Wagenknecht, Burke, Perkins, Haley, & Friedman, 1992).
Home Smoking Restrictions
Responses to “How is cigarette smoking handled as far as your home is concerned? Is no one allowed to smoke in your home, only special guests are allowed to smoke, people are allowed to smoke only in certain areas of your home, or are people allowed to smoke anywhere in your home?” were coded into three dummy indicators for no smoking restriction, a partial smoking ban, or a complete smoking ban.
Family Smoking Models
The survey instruments included questions to collect egocentric social network data on familial ties and general descriptors of friends’ smoking (Smith & Christakis, 2008). Respondents were presented with a list of familial relationships and asked about the traits of that person. This network approach treats the individual as the wheel hub where respondents are asked about alters, persons with whom the respondent has a relationship, particularly if these alters smoked.
Family smoking models were measured by counting the number of the persons (spouse, parents, grandparents, aunts/uncles, siblings, and children) that respondents reported “ … smokes cigarettes” and dividing by the total number of observed familial ties. The units are interpreted as the percent of smoking familial ties.
Dyadic Patterns of Family Smoking
Specific smoking relationships were computed by creating dummy variables by relationship type (spouse, parents, grandparents, aunts/uncles, siblings, and children) that indicated if the alter smoked.
Friends’ Smoking
Responses to “How many of your friends who you see regularly are cigarette smokers? All, most, some, a few, or none” was coded into three dummy variables representing none, some/few, or most/all.
Respondent's Smoking Status
Current smoking status was computed using Centers for Disease Control and Prevention criteria; persons who reported having smoked 100 cigarettes in their lifetime and currently smoke everyday or some days (U.S. Department of Health and Human Services, 1996).
Covariates
Education and age were measured in years. Gender and having any children at home were dummy coded.
Analysis Plan
Significant differences in home smoking restrictions between Koreans and Korean Americans, consistent with H1, were estimated by chi-square tests of deviation from independence followed by two-sample t tests to estimate differences in proportion within categories of restriction (Freedman, Pisani, & Purves, 2007). The association of restrictions with SHSe was appraised by entering home smoking restrictions into a logistic regression equation (Long, 1997) predicting any SHSe at home by sample, including adjustment for sociodemographics (gender, having any children [adult only], education, and age in the regression equation). Analysis of children’s home SHSe was restricted to households with at least one child under the age of 18 years and adjusted for adult characteristics. To test for differences in the association between smoking restrictions and SHSe, consistent with H2, a single equation for Seoul and California was specified, including an interaction term of country with home smoking restrictions (Brambor, Clark, & Golder, 2006).
To further understand, the patterns in H1 predictors of having a complete home smoking ban were appraised. The choice of analyzing tendencies toward a complete home smoking ban was informed by preliminary analysis, demonstrating that those with a partial ban and no smoking restriction had equivalent distributions of familial smokers, friends smoking, and respondents smoking (Seoul: z = .59, p < .55 and California: z = .05, p < .963) based on the null hypothesis that none of these varied across a partial ban and no smoking restriction using a joint linear combination test. Predictors of a complete home smoking ban using smoking risk indicators for the respondent, their familial network, and friends including sociodemographics used logistic regression. The association between dyadic occurrences of smoking in specific relationships and having a complete home smoking ban were assessed using logistic regression by relationship and sample, including adjustment for friends’ smoking and sociodemographics.
Predicted probabilities from the regression analyses, instead of odds ratios, are reported to improve clarity, so absolute differences as well as relative differences can be observed (King, Tomz, & Wittenberg, 2000). Graphical presentation followed methods described by Kastellec and Leoni (2007). All tests were two tailed, p < .05.
Results
On average, Koreans were younger, less educated, and more likely to have children or smoke than Korean Americans (Table 1). Koreans had more opportunities for SHSe as indicated by more familial smokers and smoking friends. For example, about 45% (95% CI: 43–48) of Korean family members smoked compared to 29% (95% CI: 27–30) among Korean Americans. Similarly, about 34% (95% CI: 30–38) of Koreans reported most/all their friends smoked compared with 13% (95% CI: 12–14) among Korean Americans. Koreans were significantly more likely to have any SHSe at home, 43% (95% CI: 38–47), compared with Korean Americans, 17% (95% CI: 16–19), as were Korean children, 59% (95% CI: 53–65) versus 13% (95% CI: 12–25).
Table 1.
Sample characteristicsa
| Seoul, South Korea |
California, United States |
|||||
| M | 95% CI | N | M | 95% CI | N | |
| Any SHSe adultb | 0.427 | 0.383–0.471 | 494 | 0.174 | 0.160–0.188 | 2,830 |
| Any SHSe childrenb | 0.591 | 0.534–0.648 | 286 | 0.134 | 0.115–0.154 | 1,177 |
| Home smoking policy | — | — | — | — | — | — |
| No policyb | 0.644 | 0.601–0.686 | 494 | 0.054 | 0.045–0.063 | 2,498 |
| Partial banb | 0.166 | 0.133–0.199 | 494 | 0.287 | 0.269–0.304 | 2,498 |
| Complete banb | 0.190 | 0.156–0.225 | 494 | 0.659 | 0.641–0.678 | 2,498 |
| Smoking modelsb | 0.454 | 0.427–0.482 | 499 | 0.309 | 0.298–0.319 | 2,827 |
| Spouseb | 0.278 | 0.228–0.329 | 309 | 0.161 | 0.145–0.176 | 2,172 |
| Siblingb | 0.573 | 0.528–0.617 | 475 | 0.441 | 0.423–0.460 | 2,687 |
| Grandparentb | 0.573 | 0.518–0.628 | 314 | 0.350 | 0.327–0.373 | 1,669 |
| Parentb | 0.537 | 0.492–0.582 | 471 | 0.369 | 0.350–0.388 | 2,509 |
| Son/daughterb | 0.220 | 0.172–0.268 | 291 | 0.154 | 0.139–0.170 | 2,029 |
| Friends smoking | — | — | — | — | — | — |
| Noneb | 0.243 | 0.205–0.281 | 498 | 0.395 | 0.377–0.413 | 2,811 |
| A few/someb | 0.418 | 0.374–0.461 | 498 | 0.474 | 0.455–0.492 | 2,811 |
| Most/allb | 0.339 | 0.298–0.381 | 498 | 0.131 | 0.119–0.144 | 2,811 |
| CDC smokerb | 0.332 | 0.291–0.373 | 500 | 0.172 | 0.159–0.186 | 2,830 |
| Any childrenb | 0.572 | 0.528–0.616 | 500 | 0.416 | 0.398–0.434 | 2,830 |
| Male | 0.496 | 0.452–0.540 | 500 | 0.471 | 0.453–0.490 | 2,830 |
| Years of educationb | 12.998 | 12.723–013.273 | 495 | 14.862 | 14.753–014.971 | 2,732 |
| Ageb | 38.342 | 37.029–039.655 | 500 | 46.948 | 46.377–047.520 | 2,828 |
Note. CDC = Centers for Disease Control and Prevention; SHSe = secondhand smoke exposure.
Numbers in cells are means, associated 95% CIs, and useful sample size for each concept. SHSe for adults and children were based on self-reports of the typical number of cigarettes exposed to at home.
Indicates significant differences in means between Seoul, South Korea, and California, United States, using a two sample t test assuming unequal variances; p < .05.
Korean Americans Have Harsher Smoking Restrictions
Consistent with expectations under H1, Korean Americans were significantly more likely to have a complete home smoking ban, 66% (95% CI: 64–68) versus 19% (95% CI: 16–23), and less likely to not have any smoking restriction, 5% (95% CI: 4–6) versus 64% (95% CI: 60–69), than Koreans. Among those with any smoking restrictions, Korean Americans were also significantly (t = 4.19, p < .01) more likely to have a complete rather than partial home smoking ban, 70% (95% CI: 46–68) versus 53% (95% CI: 46–61), than Koreans.
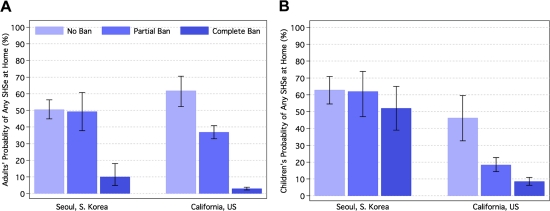
Korean Americans Were Afforded More Protection for the Same Home Smoking Restriction
Consistent with expectations under H2, the negative associations between smoking restrictions and any home SHSe were stronger among Korean Americans than among Koreans for both adults and children. For example, among Koreans, the probability of any SHSe at home without a home smoking restriction was 50% (95% CI: 45–56) compared with 49% (95% CI: 38–61) with a partial ban and 10% (95% CI: 5–18) with a complete smoking ban (Figure 2A). Among Korean Americans, the trends for SHSe were 62% (95% CI: 52–70) without a home smoking restriction compared with 37% (95% CI: 33–41) with a partial and 3% (95% CI: 2–4) with a complete smoking ban. The absolute difference between a complete ban versus no ban was 40% compared with a 59% reduction in the probability of any home SHSe for Korean and Korean Americans, respectively; this translates into relative within-group differences [(SHSe(ban) − SHSe(no ban))/SHSe(no ban)] of 80% for Koreans versus 95% for Korean Americans. Among children, the absolute difference in probability of any home SHSe, by ban versus no ban, was 12% for Koreans versus 38% for Korean Americans; with the relative within-group differences being 17% for Koreans versus 83% for Korean Americans (Figure 2B).
Figure 2.
Home smoking restrictions differentially protect against secondhand smoke exposure (SHSe) at home in Seoul and California. (A) shows the predicted probability of any SHSe at home for the respondent, and (B) their children, with 95% CIs by home smoking policy in Seoul, South Korea, and California, United States. Estimates were produced from a logistics regressions (by country) adjusting for gender, education, and age of the household respondent. Predictions were produced by simulation, using 1,000 randomly drawn estimates from the coefficient covariance matrix, with other predictors held at their mean. Trends of increased SHS exposure were statistically significant for all associations, except children in Seoul, South Korea.
High-Risk Koreans and Korean Americans Were Similarly Unlikely to Have the Harshest Smoking Restrictions
Part of the difference in the presence of complete home smoking bans between Korean and Korean Americans was a function of Korean Americans with lower risk profiles being more likely to have a complete ban. For example, the probability of having a complete home smoking ban among Korean Americans was 13% (95% CI: 8–18) lower when a few/some friends smoked and 25% (95% CI: 17–33) lower when most/all of their friends smoked, while Koreans were not significantly more or less likely to have a complete home smoking ban as a function of their friends smoking (Figure 3A). Respondents’ smoking was associated with a 40% (95% CI: 33–45) and 12% (95% CI: 3–20) lower probability of a complete home smoking ban among Koreans and Korean Americans, respectively, with the former significantly larger than the later (z = 2.69, p < .01). As 50% more of a respondent's family smoked, Korean Americans had a 15% (95% CI: 11–20) and Koreans a 11% (95% CI: 6–17) lower probability of a complete home smoking ban; though the difference was practically large, it was not statistically significant (z = 0.86, p < .38).
Figure 3.
Who has the harshest home smoking restrictions? (A) shows the change in predicted probability of a complete home smoking ban with 95% CIs after entering all predictors into a single logistic regression equation. An overlapping CI with zero indicates statistical insignificance. (B) shows the predicted probability of a home smoking ban for high-risk and low-risk profile respondents using estimates from the logistic equation described in A. Low risk was indicated by 25% of familial alters smoking, no smoking friends, not smoking, and 16 years of education. High risk was indicated by 75% of familial alters smoking, most/all smoking friends, smoking, and 12 years of education. In both profiles, age was fixed at 30, gender as male, and they had children. All predictions were produced by simulation using 1,000 randomly drawn estimates from the coefficient covariance matrix.
Four more years of formal education was associated with a 6% (95% CI: 1–14) higher probability of a complete home smoking ban among Korean Americans, but education was not significantly associated with a ban among Koreans. Each additional 10 year age increase after 40 years was associated with a 7% (95% CI: 4–10) and 5% (95% CI: 3–7) higher probability of having a complete home smoking ban among Koreans and Korean Americans, respectively, with neither association significantly distinguishable from the other (z = 0.87, p < .39). Having any children was associated with a 12% (95% CI: 7–16) lower probability and male gender a 12% (95% CI: 7–17) higher probability of having a complete home smoking ban among Korean Americans, while these were not significantly associated with a complete home smoking ban among Koreans.
To clarify SHSe between risk patterns and their association with home smoking restrictions, probabilities were produced under the counterfactual of low and high-risk profiles using estimates from the above regression. Low-risk profiles assumed that the respondent did not smoke, 25% of their familial alters smoked, none of their friends smoked, and they had 16 years of education. High-risk profiles assumed that the respondent smoked, 75% of their familial alters smoked, most/all of their friends smoked, and they had 12 years of education. In both profiles, age was fixed at 30, gender as male, and they were parents. Korean Americans at low risk were significantly more likely than Koreans at low risk to have a complete home smoking ban, 82% (95% CI: 76–86) versus 36% (95% CI: 17–57; Figure 3B). On the other hand, Korean Americans at high risk were no more likely to have a complete home smoking ban than Koreans at high risk, 10% (95% CI: 7–13) versus 7% (95% CI: 3–13), with the probability of having a complete ban of either quite low.
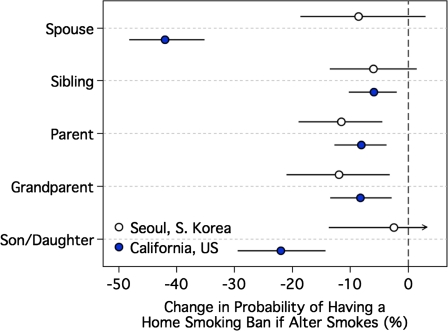
Dyadic associations between smoking by familial relationship and complete home smoking ban provided additional evidence for differences in SHSe risk between Koreans and Korean Americans (Figure 4). For example, a smoking spouse was associated with a 42% (95% CI: 35–48) lower probability of having a complete home smoking ban among Korean Americans compared with 9% (95% CI: 3–18) among Koreans, a more than fourfold stronger association (z = 2.26, p < .01). This pattern was similar for smoking husbands or wives modeled separately. A smoking son or daughter was associated with a 22% (95% CI: 14–29) lower probability of a complete home smoking ban compared with an insignificant association for Koreans, −2% (95% CI: −14 to 12), with these associations borderline significantly different (z = 1.61, p < .10). These patterns suggest that for Korean Americans, any smoking relationship in the home was associated with greater reductions in the probability of having a complete ban than for Koreans.
Figure 4.
Within household models prevent home smoking restrictions. The above shows the change in predicted probability of a complete home smoking ban with 95% CIs. Predictions were produced by simulating the probabilities for a change in smoking status (from nonsmoking to smoking) with the use of 1,000 randomly drawn secondhand smoke of estimates from the coefficient covariance matrix adjusting for friends’ smoking, respondents’ smoking, gender, the presence of children, education, and age. An overlapping CI with zero indicates statistical insignificance.
Discussion
Consistent with ecological frameworks, mediating and moderating processes occurred on both sides of the Pacific where tobacco control and antismoking cultures were weak, as in Seoul, versus strong, as in California. Korean Americans had harsher home smoking restrictions than Koreans, and for the same level of restriction, restrictions were more protective against SHSe at home among adults and their children. Respondents who did not smoke, had few smoking family members, few smoking friends, and higher education were more likely to have the most restrictive smoking policies on both sides of the Pacific. However, these patterns also differed in that the higher prevalence of complete smoking bans in California, relative to Seoul, was among those at low risk of SHSe, though being at lower risk was more common in California than in Seoul.
Strengths and Limitations
The strengths of this study include a multisite design consistent with ecological frameworks to assess variability in distal sociopolitical structures, particularly for home smoking restrictions and SHSe where these have been the least explored (Hovell & Hughes, 2009). Interviews were conducted in respondents’ language of preference, and measures included details of SHSe risk from friends and family who smoked. Limitations included self-reported data subject to recall and reporting biases from a single household informant, although such biases are not fatal to tobacco studies of this kind (SRNT Subcommittee on Biochemical Verification, 2002). Some features of the data collection also posed limitations. The response rate in Seoul was modest, though the sample characteristics, including smoking status, were similar to those known of the population, suggesting that the data still closely represented the respective population. The collection of the data differed only in the number of callbacks to no answers, five in Seoul versus seven in California. Dunkelberg and Day (1973) shows that respondents reached on the fifth versus seventh attempt do not differ practically or statistically; suggesting that this difference in method may not alter our conclusions.
The assumption that the two-sample design allowed variation in policy/culture among similar populations may be problematic. Koreans who immigrate likely differ from other Koreans, even though these differences may be partially controlled for by sampling in Seoul, the primary source of Korean immigration, and adjusting for sociodemographic characteristics. It remains unclear what specific aspects of the distal environment altered home smoking restrictions and restrictions’ association with SHSe. Among the possible explanations, three predominate: It may be the harsher smoking culture, CTCP, or the shifting cultural norms toward equitable individualism. More complete measures of the distal environment may address this but it is likely that all three factors work in combination (Link & Phelan, 1995).
It is also possible that difference in cooperation rates across study sites limit the generalizability of the findings reported herein, where noncooperators could differ from cooperators in smoking restrictions, SHSe and their joint association. Despite the disproportionate cooperation rates in Seoul and California, the surveys closely represented population characteristics. Neither sample differed significantly from age by gender population distributions, and sample smoking prevalences approximated those in other studies, as described in Hofstetter et al. (2004, 2006). Still, the results should be interpreted with caution, and further investigation should be used to assess the quality of our inferences.
Implications
Engel (1977, 1980) provided early critiques of the biomedical model, which focused on already diseased individuals in isolation of factors outside the individual. Extensions of his logic (Bronfenbrenner, 1977; Glass & McAtee, 2006; Hovell, Wahlgren, & Adams, 2009; McLeroy et al., 1988) have brought attention to extraindividual determinants, but their inclusion in research remains shallow with many researchers treating these frameworks as little more than a reminder to consider investigating everything (McHugh, 1992). This may be changing, especially in tobacco research where advances in policy, social context, and individual research are more prominent (Samet & Wipfli, 2009). Hovell and Hughes (2009) have taken these frames to their next logical extension with application to SHSe where more specific and testable deductions may be made. Herein, we extended these deductions by applying the logic of distal and proximal mediation and moderation to Koreans and Korean Americans, and their home smoking restrictions. Our findings provide a framework for their continued application. For example, studies have found strong associations between the CTCP and restrictive home smoking policies (Norman, Ribisl, Howard-Pitney, Howard, & Unger, 2000), but these only considered the direct effects of CTCP on home smoking restrictions and did not consider the possible pathways responsible or how individuals are differentially impacted by CTCP as ecological frameworks would suggest.
It is difficult to apply our findings to situations where there may be more nuanced contrasts in distal determinants. However, we have found similar patterns in South Korea between genders where women faced more criticism for, and the same level of criticism had a stronger association with, smoking than among men (Ayers, Hofstetter, Hughes, et al., 2010). Martinez-Donate et al. (2009, 2008) found that exposure to the California smoking climate was associated with a lower smoking prevalence 1,500 miles south of the Mexican border. These analyses were able to observe patterns of mediation and moderation with less extreme variability in distal determinants than presented here, suggesting that ecological frameworks may be pursued in more nuanced cases.
At the time these data were collected, South Korea was undergoing many tobacco control reforms. In 2003, the South Korea government signed and in 2005 ratified the World Health Organization Framework Convention on Tobacco Control (FCTC; K. S. Cho, 2006; Fong et al., 2006). To be consistent with FCTC, reforms of the original 1995 National Health Promotion Act expanded antismoking campaigns, restrictions on tobacco advertising, and obvious warning labels on cigarettes and made clean indoor air laws more restrictive. Our findings suggest that these policies may promote home smoking restrictions and thereby reductions in SHSe at home. These policies may also cause South Korea to resemble California where there are fewer smokers and numerous models of how to enforce public restrictions that may be translated to the home, resulting in greater effectiveness for restrictions. Application of additional policy interventions to South Korea should be foremost on the prevention agenda.
In California, home smoking restrictions appear mostly in effect among low-risk households; suggesting that direct interventions are needed unlike the policy provisions prescribed for Koreans. California’s policy environment likely selects from Korean Americans most susceptible to taking on a complete home smoking ban, leaving those at the greatest risk unchanged. These data provide details on which Korean Americans are in the category of greatest risk. It may be advisable to approach clinicians who service Korean Americans and ask if they screen and prescribe home smoking restrictions to their patients in the high-risk profile. Similar strategies among U.S. teens have reduced smoking initiation when prescribed by their orthodontist (Hovell et al., 1996). Since health care access may be limited among immigrants, community interventions that reach Korean Americans where they cluster, such as Christian churches (Ayers et al., 2009; Ayers, Hofstetter, Irvin, et al., 2010; Hofstetter, Ayers, et al., 2010), may also be useful for promoting secondary and tertiary prevention. Targeted interventions developed in the United States will be applicable to South Korea as policy changes there likely impact those with low risk of SHSe, leaving a pool of high risk Koreans to be directly intervened on.
Future Research
It is no longer sufficient to focus on a single level of measurement given the strong claims by ecological frameworks and our results. Studies need to maximize variability among distal determinants to detect the upstream factors responsible for the proximal risks most often observed. What remains to be studied is how similar mediating and moderating processes impact other smoking behaviors and how application of ecological frameworks to interventions moves the promotion of home smoking restrictions away from their individual focus.
Funding
This research was supported by California’s Tobacco-Related Disease Research Program (9RT-0073) and the National Institutes of Health (R01CA105199-01A1) to C. Richard Hofstetter.
Declaration of Interests
None declared.
References
- Alamar B, Glantz SA. Effect of increased social unacceptability of cigarette smoking on reduction in cigarette consumption. American Journal of Public Health. 2006;96:1359–1363. doi: 10.2105/AJPH.2005.069617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayers JW, Hofstetter CR, Hughes SC, Irvin VL, Sim DE, Hovell MF. Exploring religious mechanisms for healthy alcohol use: Religious messages and drinking among Korean women in California. Journal of Studies on Alcohol and Drugs. 2009;70:890–898. doi: 10.15288/jsad.2009.70.890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayers JW, Hofstetter CR, Hughes SC, Park HR, Paik HY, Song YJ, et al. Gender modifies the relationship between social networks and smoking among adults in Seoul, South Korea. International Journal of Public Health. 2010 doi: 10.1007/s00038-010-0126-7. doi:10.1007/s00038-010-0126-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayers JW, Hofstetter CR, Irvin V, Song YJ, Park HR, Paik HY, et al. Can religion help prevent obesity? Religious messages and the prevalence of overweight and/or obesity among Korean women in California. Journal for the Scientific Study of Religion. 2010;49:536–549. doi: 10.1111/j.1468-5906.2010.01527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baruch Y. Response rate in academic studies—A comparative analysis. Human Relations. 1999;52:421–438. [Google Scholar]
- Bayer R, Colgrove J. Science, politics, and ideology in the campaign against environmental tobacco smoke. American Journal of Public Health. 2002;92:949–954. doi: 10.2105/ajph.92.6.949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brambor T, Clark WR, Golder M. Understanding interaction models: Improving empirical analyses. Political Analysis. 2006;14:63–82. [Google Scholar]
- Bronfenbrenner H. Toward an experimental ecology of human development. American Psychologist. 1977;32:513–531. [Google Scholar]
- Cho HJ, Khang YH, Jun HJ, Kawachi I. Marital status and smoking in Korea: The influence of gender and age. Social Science & Medicine. 2008;66:609–619. doi: 10.1016/j.socscimed.2007.10.005. [DOI] [PubMed] [Google Scholar]
- Cho KS. FCTC and tobacco control policy in Korea. Health Welfare Policy Forum. 2006;116:7–23. [Google Scholar]
- Corrao MA, Guindon GE, Sharma N, Shokoohi DF. Tobacco control country profiles. Atlanta, GA: American Cancer Society; 2000. [Google Scholar]
- Do YK, Park K. Local governments’ dependence on tobacco tax revenue: A deterrent to tobacco control in the Republic of Korea. Bulletin of the World Health Organization. 2009;87:692–699. doi: 10.2471/BLT.08.056051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunkelberg WC, Day GS. Nonresponse bias and callbacks in sample surveys. Journal of Marketing Research. 1973;10:160–168. [Google Scholar]
- Engel GL. The need for a new medical model: A challenge for biomedicine. Science. 1977;196:129–136. doi: 10.1126/science.847460. [DOI] [PubMed] [Google Scholar]
- Engel GL. The clinical application of the biopsychosocial model. American Journal of Psychiatry. 1980;137:535. doi: 10.1176/ajp.137.5.535. [DOI] [PubMed] [Google Scholar]
- Fong GT, Cummings KM, Borland R, Hastings G, Hyland A, Giovino GA, et al. The conceptual framework of the International Tobacco Control (ITC) policy evaluation project. Tobacco Control. 2006;15(Suppl. 3):iii3–iii11. doi: 10.1136/tc.2005.015438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman D, Pisani R, Purves . Statistics. 4th ed. New York: W.W. Norton; 2007. [Google Scholar]
- Frey JH. Survey research by telephone. Beverly Hills, CA: Sage Publications; 1983. [Google Scholar]
- Gilpin E, White M, White V, Distefan JM, Trinidad DR, James L. Tobacco control successes in California: A focus on young people, results from the California Tobacco Control Surveys, 1999–2002. San Diego, CA: University of California; 2004. [Google Scholar]
- Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: Extending horizons, envisioning the future. Social Science & Medicine. 2006;62:1650–1671. doi: 10.1016/j.socscimed.2005.08.044. [DOI] [PubMed] [Google Scholar]
- Hofstetter CR, Ayers JW, Irvin VL, Kang Sim DE, Hughes SC, Reighard F, et al. Does church participation facilitate tobacco control? A report on Korean immigrants. Journal of Immigrant and Minority Health/Center for Minority Public Health. 2010;12:187–197. doi: 10.1007/s10903-009-9228-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofstetter CR, Hovell MF, Irvin VL, Ayers JW, Hughes S, Kang S. It's others, not the police: Smoking, reprimand, and fines among adults of Korean descent in California. Health Psychology. 2010;29:255–261. doi: 10.1037/a0018166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofstetter CR, Hovell MF, Irvin VL, Ledet R, Ni R, Jung KR, et al. Demography of exercise: Koreans residing in Seoul. Asian Journal of Health and Information Sciences. 2006;1:136–151. [Google Scholar]
- Hofstetter CR, Hovell MF, Lee J, Zakarian J, Park H, Paik HY, et al. Tobacco use and acculturation among Californians of Korean descent: A behavioral epidemiological analysis. Nicotine & Tobacco Research. 2004;6:481–489. doi: 10.1080/14622200410001696646. [DOI] [PubMed] [Google Scholar]
- Hovell MF, Hughes SC. The behavioral ecology of secondhand smoke exposure: A pathway to complete tobacco control. Nicotine & Tobacco Research. 2009;11:1254–1264. doi: 10.1093/ntr/ntp133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hovell MF, Slymen DJ, Jones JA, Hofstetter CR, Burkham-Kreitner S, Conway TL, et al. An adolescent tobacco-use prevention trial in orthodontic offices. American Journal of Public Health. 1996;86:1760–1766. doi: 10.2105/ajph.86.12.1760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hovell MF, Wahlgren DR, Adams MA. The logical and empirical basis for the behavioral ecological model. In: Ciclemente RJ, Crosby RA, Kegler M, editors. Emerging theories in health promotion practice and research. San Francisco, CA: Jossey-Bass; 2009. pp. 347–385. [Google Scholar]
- Hovell MF, Zakarian JM, Wahlgren DR, Matt GE, Emmons KM. Reported measures of environmental tobacco smoke exposure: Trials and tribulations. Tobacco Control. 2000;9(3 Suppl.):ii23–ii28. doi: 10.1136/tc.9.suppl_3.iii22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes SC, Corcos IA, Hofstetter RC, Hovell MF, Irvin VL. Environmental tobacco smoke exposure among Korean American nonsmokers in California. Nicotine & Tobacco Research. 2008;10:663–670. doi: 10.1080/14622200801978748. [DOI] [PubMed] [Google Scholar]
- Hughes SC, Corcos IA, Hofstetter CR, Hovel MF, Irvin VL, Park HR, et al. Children's exposure to secondhand smoke at home in Seoul, Korea. Asian Pacific Journal of Cancer Prevention. 2008;9:491–495. [PubMed] [Google Scholar]
- Hughes SC, Corcos IA, Hofstetter CR, Hovell MF, Irvin VL, Park HR, et al. Home smoking restrictions among Koreans in Seoul. Asia-Pacific Journal of Public Health. 2009;21:63–70. doi: 10.1177/1010539508327029. [DOI] [PubMed] [Google Scholar]
- Hughes SH, Hovell MF, Hofstetter CR, Irvin VL, Park HR, Paik HY. Home smoking policy and environmental tobacco smoke exposure among Koreans in Seoul. Tobacco Control. 2008;17:71–72. doi: 10.1136/tc.2007.022244. [DOI] [PubMed] [Google Scholar]
- Jacobson PD, Wasserman J. The implementation and enforcement of tobacco control laws: Policy implications for activists and the industry. Journal of Health Politics, Policy and Law. 1999;24:567–598. doi: 10.1215/03616878-24-3-567. [DOI] [PubMed] [Google Scholar]
- Jee SH, Ohrr H, Kim IS. Effects of husbands’ smoking on the incidence of lung cancer in Korean women. International Journal of Epidemiology. 1999;28:824–828. doi: 10.1093/ije/28.5.824. [DOI] [PubMed] [Google Scholar]
- Ji M, Ding D, Hovell MF, Xia X, Zheng P, Fu H. Home smoking bans in an urbanizing community in china. American Journal of Preventive Medicine. 2009;37:132–136. doi: 10.1016/j.amepre.2009.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji M, Hofstetter CR, Hovell M, Irvin V, Song YJ, Lee J, et al. Smoking cessation patterns and predictors among adult Californians of Korean descent. Nicotine & Tobacco Research. 2005;7:59–69. doi: 10.1080/14622200412331328493. [DOI] [PubMed] [Google Scholar]
- Kang HY, Kim HJ, Park TK, Jee SH, Nam CM, Park HW. Economic burden of smoking in Korea. Tobacco Control. 2003;12:37–44. doi: 10.1136/tc.12.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kastellec JP, Leoni EL. Using graphs instead of tables in political science. Perspectives on Politics. 2007;5:755–771. [Google Scholar]
- King G, Tomz M, Wittenberg J. Making the most of statistical analyses: Improving interpretation and presentation. American Journal of Political Science. 2000;44:341–355. [Google Scholar]
- Lee SW. The effects of the smoking and drinking on TV on health related behavior. Seoul, Korea: Kwan Dong University Press; 2003. [Google Scholar]
- Link BG, Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior. 1995;35:80–94. [PubMed] [Google Scholar]
- Long JS. Regression models for categorical and limited dependent variables. London: Sage Publications; 1997. [Google Scholar]
- Markus HR, Kitayama S. Culture and the self: Implications for cognition, emotion, and motivation. Psychological Review. 1991;98:224–253. [Google Scholar]
- Martínez-Donate AP, Hovell MF, Hofstetter CR, González-Pérez GJ, Kotay A, Adams MA. Crossing borders: The impact of the California tobacco control program on both sides of the US-Mexico border. American Journal of Public Health. 2008;98:258–267. doi: 10.2105/AJPH.2006.097998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez-Donate AP, Johnson-Kozlow M, Hovell MF, Gonzalez Perez GJ. Home smoking bans and secondhand smoke exposure in Mexico and the US. Preventive Medicine. 2009;48:207–212. doi: 10.1016/j.ypmed.2008.12.011. [DOI] [PubMed] [Google Scholar]
- McHugh PR. A structure for psychiatry at the century's turn—The view from Johns Hopkins. Journal of the Royal Society of Medicine. 1992;85:483. doi: 10.1177/014107689208500819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Education & Behavior. 1988;15:351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- Min PG. Changes in Korean immigrants’ gender role and social status, and their marital conflicts. Sociological Forum. 2001;16:301–320. [Google Scholar]
- Norman GJ, Ribisl KM, Howard-Pitney B, Howard KA, Unger JB. The relationship between home smoking bans and exposure to state tobacco control efforts and smoking behaviors. American Journal of Health Promotion. 2000;15:81–88. doi: 10.4278/0890-1171-15.2.81. [DOI] [PubMed] [Google Scholar]
- Pizacani BA, Martin DP, Stark MJ, Koepsell TD, Thompson B, Diehr P. Household smoking bans: Which households have them and do they work? Preventive Medicine. 2003;36:99–107. doi: 10.1006/pmed.2002.1123. [DOI] [PubMed] [Google Scholar]
- Samet JM, Wipfli H. Unfinished business in tobacco control. Journal of the American Medical Association. 2009;302:681–682. doi: 10.1001/jama.2009.1155. [DOI] [PubMed] [Google Scholar]
- Smith KP, Christakis NA. Social networks and health. Annual Review of Sociology. 2008;34:405–429. [Google Scholar]
- Spencer N, Blackburn C, Bonas S, Coe C, Dolan A. Parent reported home smoking bans and toddler (18–30 month) smoke exposure: A cross-sectional survey. Archives of Disease in Childhood. 2005;90:670–674. doi: 10.1136/adc.2004.054684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SRNT Subcommittee on Biochemical Verification. Biochemical verification of tobacco use and cessation. Nicotine & Tobacco Research. 2002;4:149–159. doi: 10.1080/14622200210123581. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. National center for health statistics. NHANES III reference manuals and reports (CD-ROM) Hyattsville, MD: Centers for Disease Control and Prevention; 1996. [Google Scholar]
- Wagenknecht LE, Burke GL, Perkins LL, Haley NJ, Friedman GD. Misclassification of smoking status in the CARDIA study: A comparison of self-report with serum cotinine levels. American Journal of Public Health. 1992;82:33–36. doi: 10.2105/ajph.82.1.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winickoff JP, Friebely J, Tanski SE, Sherrod C, Matt GE, Hovell MF, et al. Beliefs about the health effects of “thirdhand” smoke and home smoking bans. Pediatrics. 2009;123:e74–e79. doi: 10.1542/peds.2008-2184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu SH, Wong S, Tang H, Shi CW, Chen MS. High quit ratio among Asian immigrants in California: Implications for population tobacco cessation. Nicotine & Tobacco Research. 2007;9(3 Suppl.):S505–S14. doi: 10.1080/14622200701587037. doi:10.1080/14622200701587037. [DOI] [PubMed] [Google Scholar]