Abstract
Introduction:
The incidence of quit attempts is often used to measure the effects of tobacco control interventions. Many surveys of quit attempts require that the attempt last ≥24 hr, presumably to provide a more objective definition and to eliminate less serious attempts; however, this criterion may bias outcomes by excluding the more dependent quitters who cannot stop for 1 day despite a serious quit attempt.
Methods:
We examined the 2003 and the 2006–2007 Tobacco Use Supplements to the Current Population Survey to determine the prevalence of quit attempts that did and did not last 24 hr, both in the last 12 months and in one's lifetime among current daily smokers. We also tested the hypothesis that those unable to quit for 24 hr were the more dependent smokers.
Results:
Requiring quit attempts to last 24 hr excluded 6%–17% of smokers who stated they made a quit attempt. Whether smokers who could not quit for more than 24 hr were more dependent varied across survey, recall duration, and measure.
Conclusions:
We conclude restricting quit attempts to those who have quit for 24 hr underestimates the prevalence of attempts. Whether those unable to quit for 24 hr are the more dependent smokers is unclear. Empirical tests of whether the addition of a 24-hr criterion increases reliability or validity are needed.
Introduction
A major focus of most tobacco control interventions (e.g., taxation, media, work-site restrictions) in adults is to motivate current smokers to attempt to stop smoking; thus, the incidence of quit attempts is often used as a measure of the success of tobacco control efforts (National Cancer Institute [NCI], 2000). In epidemiological, policy, and treatment surveys, a quit attempt is often defined as an attempt to stop smoking that lasted 1 day or 24 hr (Starr et al., 2005). Why the additional criterion that an attempt must last 24 hr is often added is unclear. One possibility is that it is to provide a more standard and objective measure than a smoker's opinion of what was versus was not a quit attempt, which could vary across smokers and attempts. Another possibility is that it is to exclude “nonserious” or “less motivated” quit attempts. Whether adding the 24-hr criterion improves reliability or validity has not been tested.
Two prior studies have examined how many quit attempts do not last for 24 hr. In a study of volunteers for a clinical trial, we found that excluding quit attempts <24 hr would miss 21% of quit attempts (Carpenter & Hughes, 2004). In addition, an analysis of the population-based U.S. 2003 Tobacco Use Supplement to the Current Population Survey (TUS-CPS) that was focused on the prevalence of treatment use, provided data that one can use to calculate that excluding quit attempts <24 hr would have missed 13% of quit attempts (Shiffman, Brockwell, Pillitteri, & Gitchell, 2008).
One potential problem with the 24-hr definition is that it may miss true quit attempts that do not last for 24 hr (Hughes, Keely, & Naud, 2004) due to several factors, including high levels of nicotine dependence (U.S. Department Health and Human Services, 1988). If so, then a tobacco control activity (e.g., increased taxation) could truly increase quit attempts in heavy dependent smokers, but if few such smokers were able to abstain for 24 hr, then the 24-hr definition could cause one to falsely conclude taxes have little effect on dependent smokers. Although the proposition that the ≥24-hr definition excludes dependent smokers is face valid, our earlier study did not find this (Carpenter & Hughes, 2004). Given the limited data on the concordance of ≥24 hr versus any quit attempts, and whether the former excludes the more dependent smokers, we undertook a more detailed analysis of this using the more recent TUS-CPS surveys.
Methods
The TUS-CPS is an NCI-sponsored survey of tobacco use that has been administered as part of the U.S. Census Bureau's Current Population Survey every 2–3 years (http://riskfactor.cancer.gov/studies/tus-cps). The most recent surveys were completed in February/June/November of 2003 and May 2006/August 2006/January 2007. The TUS-CPS recruits a nationally representative sample of about 240,000 noninstitutionalized individuals who are ≥15 years old. Most (70%) surveys were conducted via phone and the remainder via in person interviews. More information on the TUS-CPS can be obtained at the Web site cited above.
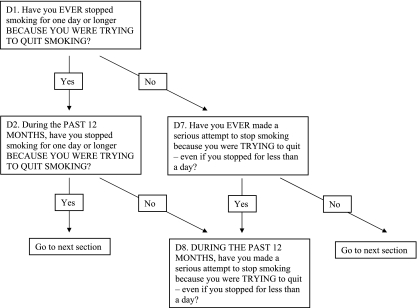
The 2003 and 2006–2007 surveys asked several questions about quit attempts (a) in the past 12 months and (b) in one's lifetime, among current daily smokers who were also daily smokers 1 year ago. Respondents were first asked about any quit attempts over a lifetime and, if some occurred, whether any were in the last year (Figure 1). Importantly, respondents were first asked about quit attempts ≥24 hr and, only if they reported no such attempts, were asked about quit attempts <24 hr. This hierarchy has implications for the many smokers who made more multiple quit attempts in their lifetime or even in the last year (e.g., in the 2006 TUS-CPS, among those who attempted to quit in the last year, 62% attempted to quit more than once). Thus, among those with multiple quit attempts, those who reported a quit attempt of ≥24 hr had at least one quit attempt that lasted ≥24 hr and may have had one or more quit attempts that lasted <24 hr as well. Also, among those with multiple attempts, those who reported a quit attempt of <24 hr are actually stating that all their quit attempts lasted <24 hr. Finally, we did not include nondaily smokers because the TUS-CPS did not ask questions about ≥24-hr versus <24-hr quit attempts among current nondaily smokers, plus we worried that nondaily smokers would have difficulty in discriminating 24 hr periods of abstinence due to quitting versus due to their usual pattern of smoking.
Figure 1.
Hierarchy of questions on quit attempts in the 2006–2007 Tobacco Use Supplement to the Current Population Survey (TUS-CPS). The hierarchy for the 2003 TUS-CPS is similar.
To test whether quit attempts <24 hr are associated with high nicotine dependence we compared <24-hr versus ≥24-hr quitters on age-of-onset of smoking, cigarettes/day, and time to first cigarette (TTFC), all of which have been used as proxy measures of dependence with some evidence of validity (Piper, McCarthy, & Baker, 2006). We also compared the groups on four demographics: age, sex, race, and education. We considered comparing groups on motivation; however, the motivation measures in the TUS-CPS asked about current motivation, not motivation at the time of the quit attempt. We believed it was plausible that motivation had changed after prior failed quit attempts and thus may not reflect motivation prior to the quit attempt; thus, we did not include measures of motivation in our analyses. The TUS-CPS also only asked about current dependence; however, we included dependence results because we believed they were less likely to change after a failed quit attempt; however, we have no data to support or refute this belief.
Our analysis can be conceptualized as comparing quit attempts with versus without the 24-hr criteria in four datasets representing a 2 × 2 design with factors of (a) 2006–2007 versus 2003 survey and (b) over the last 12 months versus over a lifetime. The very large sample sizes of the two CPS surveys allow trivial differences to be statistically significance; thus, instead of using statistical significance to conclude differences, the analysis used the relative magnitude of the difference. We thought a 15% increase or decrease to be the smallest difference worth discussing; however, all the estimates are reported for those who wish to focus on smaller or larger differences. Means, medians, and percentages were weighted to represent the civilian noninstitutionalized U.S. population age 18+ years.
Results
Prevalence of quit attempts
In the 2006–2007 TUS-CPS, 35% of current daily smokers who were also daily smokers 12 months ago reported a quit attempt in the last 12 months and 71% reported a quit attempt in their lifetime. Of those who had ever tried to quit, 50% tried in the last 12 months. Similar results occurred with the 2003 TUS-CPS. Among smokers in the 2006–2007 dataset who attempted to quit in the last 12 months, 17% of attempters reported none of their quit attempts lasted ≥24 hr; thus, excluding attempts lasting <24 hr would miss 17% of those who made a quit attempt. The corresponding incidence of missed quit attempters with the 24 hr criterion for lifetime quitting was 6% of attempters. In the 2003 CPS, the corresponding rates of missed quit attempters for last 12 months and lifetime quit attempters were 11% and 6% of all quit attempters.
The above analyses are based on current daily smokers who were also daily smokers 1 year ago. If we included last year quitters in the denominator (i.e., based on all last-year smokers), then excluding quit attempts that lasted <24 hr would have missed a smaller percent of all quit attempts in the past year; that is, 12% in the 2006–2007 and 9% in the 2003 TUS-CPS.
Across the four datasets, those who quit for <24 hr and those who quit for ≥24 hr did not differ on any demographic (Table 1). They also did not differ on age of onset of smoking. In two of the four analyses, those not able to quit for ≥24 hr smoked more cigarettes/day, and in three of the four analyses, they had a shorter TTFC.
Table 1.
Characteristics of Smokers by Quit History for TUS-CPSa
| 2006–07 survey |
2003 survey |
|||||||
| Quit in last 12 months |
Ever quit |
Quit in last 12 months |
Ever quit |
|||||
| Attempt lasted <24 hr | Attempt lasted ≥24 hr | Attempt lasted <24 hr | Attempt lasted ≥24 hr | Attempt lasted <24 hr | Attempt lasted ≥24 hr | Attempt lasted <24 hr | Attempt lasted ≥24 hr | |
| Demographics | ||||||||
| Age | 44 | 41 | 43 | 43 | 44 | 40 | 42 | 43 |
| % Men | 47 | 53 | 49 | 52 | 46 | 52 | 49 | 52 |
| % Whiteb | 78 | 76 | 79 | 81 | 76 | 77 | 76 | 82 |
| % ≥HS | 81 | 83 | 76 | 83 | 78 | 83 | 76 | 83 |
| Dependence | ||||||||
| Age of onset | 17 | 18 | 17 | 17 | 17 | 17 | 17 | 17 |
| Cigarettes/dayc | 15 | 15 | 20 | 17 | 20 | 15 | 20 | 20 |
| TTFCc | 30 | 30 | 15 | 30 | 20 | 30 | 15 | 30 |
Note. HS = high school education; TTFC = time to first cigarette, in minutes.
All data weighted (see text). Values in bold indicate where difference is greater than 15% for <24 hr versus ≥24 hr comparison.
Non-Hispanic also.
Median.
Discussion
The current results replicate our prior finding that requiring 24 hr of abstinence misses a substantial minority of past quit attempts among current smokers who made a quit attempt; that is, 6%–17% in the current survey versus 21% in our prior study (Carpenter & Hughes, 2004) and 13% in the prior 2003 CPS paper (Shiffman et al., 2008). These results are generally consistent with prospective studies that about 20% of smokers who try to quit are not able to remain abstinent for a day (Hughes et al., 2004). Thus, measures of quit attempts that require 24 hr of abstinence underestimate quit attempts.
Smokers who were versus were not able to quit for 24 hr did not differ on demographics. This finding was consistent across durations of recall and is consistent with the findings of our prior study (Carpenter & Hughes, 2004). In our prior study, those able to quit for <24 hr did not appear to be more dependent on either of two measures. In the current analyses, those not able to quit for <24 hr were more dependent on 5 of 12 tests. Several lines of evidence suggest that the validity of dependence measures is TTFC > cigarettes/day > age of onset (Piper et al., 2006). In the current analyses, the <24-hr quitters were more likely to be more dependent on TTFC (3/4 tests), than on cigarettes/day (2/4 tests) than on age of onset (0/4 tests).
The major methodological asset of the current analyses was its use of a large, population-based sample and the ability to test for differences across a range of surveys, recall durations and measures to assess convergent validity. Major methodological liabilities of the current analyses include the hierarchal structure of questions about quit attempts in the TUS-CPS and its resultant lack of clarity about multiple quit attempts. A clearer method would have been to ask specifically about the most recent quit attempt. In addition, the TUS-CPS records current dependence and motivation, not dependence and motivation at the time of the quit attempt. It is plausible that a failed quit attempt could change dependence or motivation, and thus, current measures may be inadequate proxies for prequit attempt dependence and motivation. Another liability is that memory causes many quit attempts to be forgotten or reported inaccurately and shorter quit attempts are less likely to be remembered (Berg et al., 2010; Gilpin & Pierce, 1994).
In conclusion, the current results suggest excluding quit attempts that last <24 hr underestimates the prevalence of quit attempts. Our results also suggest this may be due to the elimination of quit attempts by more dependent smokers; however, given our results differed by dependence measure, this latter result clearly requires replication. However, if replicated, this finding would suggest using the 24-hr quit attempt could underestimate the effect of tobacco control activities to motivate more dependent smokers to try to quit.
Several questions remain unanswered about the reliability and validity of the two definitions of quit attempts. Retrospective data suggest shorter quit attempts are more often forgotten (Gilpin & Pierce, 1994); thus, one would expect the test–retest reliability of ≥24-hr quit attempts to be better than that for quit attempts without this criterion. A test of this is needed. Whether the less or more restrictive definition of a quit attempt is more valid is unknown. Typically less restrictive definitions increase sensitivity (i.e., decrease false negatives) but decrease specificity (i.e., increase false positives). Studies comparing the specificity and sensitivity of the ability of the two definitions to predict later cessation are needed. Finally, one possible rationale for the 24-hr quit attempt definition was to eliminate “nonserious” or “low-motivation” quit attempts; thus, studies comparing the a priori “motivation,” “seriousness,” etc., of quit attempts that did versus did not last <24 hr are needed.
Funding
U.S. National Institute on Drug Abuse (Senior Scientist Award, DA000490).
Declaration of Interests
In the last 3 years, Dr Hughes has received research grants from the U.S. National Institutes of Health and Pfizer Pharmaceuticals. He has received consulting and speaking fees from multiple governmental, nonprofit, and for-profit organizations or companies that develop, sell, or promote smoking cessation products and services. Dr Callas has no disclosures.
Acknowledgments
We thank Anne Hartman for help with these analyses.
References
- Berg C, An L, Kirch M, Guo H, Thomas J, Patten C, et al. Failure to report attempts to quit smoking. Addictive Behaviors. 2010;35:900–904. doi: 10.1016/j.addbeh.2010.06.009. [DOI] [PubMed] [Google Scholar]
- Carpenter MJ, Hughes JR. Defining quit attempts: What difference does a day make? Addiction. 2004;100:257–259. doi: 10.1111/j.1360-0443.2004.00952.x. [DOI] [PubMed] [Google Scholar]
- Gilpin E, Pierce JP. Measuring smoking cessation: Problems with recall in the 1990 California Tobacco Survey. Cancer Epidemiology, Biomarkers & Prevention. 1994;3:613–617. [PubMed] [Google Scholar]
- Hughes JR, Keely J, Naud S. Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction. 2004;99:29–38. doi: 10.1111/j.1360-0443.2004.00540.x. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute. Population-based smoking cessation. Proceedings of a conference on What Works to Influence Cessation in the General Population, Smoking and Tobacco Control Monograph No. 12. Bethesda, MD: U.S. Public Health Service; 2000. [Google Scholar]
- Piper ME, McCarthy DE, Baker TB. Assessing tobacco dependence: A guide to measure evaluation and selection. Nicotine and Tobacco Research. 2006;8:339–351. doi: 10.1080/14622200600672765. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Brockwell SE, Pillitteri JL, Gitchell JG. Use of smoking-cessation treatments in the United States. American Journal of Preventive Medicine. 2008;34:102–111. doi: 10.1016/j.amepre.2007.09.033. [DOI] [PubMed] [Google Scholar]
- Starr G, Rogers T, Schooley M, Porter S, Wiesen E, Jamison N. Key outcome indicators for evaluating comprehensive tobacco control programs. Atlanta, GA: Centers for Disease Control and Prevention; 2005. [Google Scholar]
- U.S. Department Health and Human Services. The health consequences of smoking: Nicotine addiction: A report of the U.S. surgeon general. Washington, DC: U.S. Govt Printing Office; 1988. [Google Scholar]