Abstract
Objective
To examine the extent to which drivers with hemianopia or quadrantanopia display safe driving skills when evaluated on-road, as compared to drivers with normal visual fields.
Method
22 persons with hemianopia, 8 with quadrantanopia, and 30 with normal vision were evaluated for driving skills under in-traffic conditions by an experienced occupational therapist who used a set of six 5-point rating scales.
Results
Over 90% of drivers with normal vision drove flawlessly or had only minor errors. Although drivers with hemianopia were more likely to receive poorer ratings for all skills evaluated, 59.1% to 81.8% performed without obvious errors (depending on the skill evaluated) or had only minor errors. The skill most commonly problematic for hemianopic drivers was lane keeping (40.9% of drivers exhibiting this problem). Seven of 8 (87.5%) quadrantanopic drivers drove without obvious errors or exhibited only minor errors.
Conclusions
This study on persons with hemianopia or quadrantopia with no lateral spatial neglect and MMSE scores of ≥ 24, highlights the need to individually provide them the opportunity for an on-road driving evaluation under a variety of natural traffic conditions if they are motivated to return to driving following brain injury.
Keywords: low vision, visual perception, sensory disorders, task performance analysis
Driving is an important instrumental activity of daily living since it is the primary mode of personal transportation in many parts of the world including the U.S. (Hu & Young, 1999). Access to driving facilitates the performance of routine tasks of daily life including those related to employment, and provides opportunities for social interaction. Safe driving depends heavily on vision, yet much is unknown about the degree of vision that is required for safe driving performance (Owsley & McGwin, 1999). One group of visually impaired persons who are categorically denied licensure in many jurisdictions are those with homonymous hemianopia or quadrantanopia. In addition, ophthalmologists and neurologists commonly recommend driving cessation for their patients diagnosed with these conditions. Homonymous visual field defects occur when field loss is in the same relative position in visual space in each eye. The term hemianopia is used if one half of the field is involved, and quadrantanopia if only one quadrant is affected. These conditions result from damage to the post-chiasmal portion of the visual pathways, with the most common etiology being stroke, with other causes including traumatic brain injury and tumor (Cassidy, Bruce, & Gray, 2001; Townend, et al., 2006; Zhang, Kedar, Lynn, Newman, & Biousse, 2006). While homonymous hemianopia and quadrantanopia are not highly prevalent conditions, they are a relatively common consequence of brain injury. The prevalence of homonymous hemianopic visual field defects was recently estimated to be 0.8% within a community-dwelling population ≥ 49 years old, with 52% of these reporting a history of stroke (Gilhotra, Mitchell, Healey, Cumming, & Currie, 2002).
Preventing a person from driving has potentially serious consequences for quality of life in that it has been linked to depression, social isolation, employment challenges, and increased risk for placement in long term care (Fonda, Wallace, & Herzog, 2001; Freeman, Munoz, Turano, & West, 2006; Marottoli, et al., 2000). Therefore policies that deny licensure to persons with functional impairments must be evidence based. That is, if the driver’s license is going to be denied to applicants with certain types of functional impairments, there should be clear evidence that persons driving with these problems are unsafe to drive. Few previous studies have examined the impact of hemianopia and quadrantanopia on driver performance. One recent study (Tant, Brouwer, Cornelissen, & Kooijman, 2002) found problems with on-road steering stability in a group of 28 patients with homonymous hemianopia. This study specifically recruited persons with hemianopia whose driving was suspected to be unsafe. A study using an interactive driving simulator (Szlyk, Brigell, & Seiple, 1993) reported similar findings, specifically that the six persons with hemianopia due to stroke in their sample had more lane boundary crossings than those without the condition. Hemianopes were tested within two months of their stroke so it is highly likely that the recovery process was still ongoing (Zhang, et al., 2006). A retrospective chart review (Racette & Casson, 2005) examined occupational therapists’ assessments of the on-road driving of persons with visual field impairment, including a subgroup of 20 drivers with hemianopia or quadrantanopia. This study found that localized visual field loss in the left hemifield and diffuse loss in the right hemifield were associated with impaired driving performance in this subgroup. As acknowledged by the authors, this study had several methodological limitations such as a retrospective design, lack of a standardised driving route, and no reference group of drivers with normal visual fields to serve as a basis of comparison.
In the study described here, an occupational therapist who was also a certified driving rehabilitation specialist (CDRS) with 8 years of clinical experience in the assessment and rehabilitation of drivers, conducted on-road driving assessments for a group of persons with hemianopia or quadrantanopia. These assessments were conducted on a standardized driving route in everyday traffic conditions, using a rating instrument typical of those used by driving specialists in that ratings are provided both for specific skills and for a global impression of driving (Fox, Bowden, & Smith, 1998; Hunt, et al., 1997; Justiss, Mann, Stav, & Velozo, 2006; Kay, Bundy, Clemson, & Jolly, 2008). For comparison purposes, an age-matched group of drivers with full visual fields (i.e., normal peripheral vision) were also assessed on the road. We were interested in the extent to which drivers with hemianopia and quadrantanopia would display safe driving skills.
Methods
Participants
Participants with hemianopia or quadrantanopia were recruited through the Neuro-Ophthalmology service at the University of Alabama at Birmingham. Persons with normal visual fields and in the same age range were recruited from a list of volunteers interested in research participation. Inclusion criteria for all participants were: aged ≥ 19 years old, visual acuity of 20/60 or better in at least one eye (the vision requirement for licensure in Alabama) and a current driver’s license in the State of Alabama. If a potential participant had not driven in the past 2 years but had an interest in returning to driving, that person was considered eligible as long as the driver’s license had not expired. Exclusion criteria were diagnoses of Parkinson’s disease, multiple sclerosis, Alzheimer’s disease, hemiparesis and other types of paralysis, ophthalmic or neurologic condition characterized by visual field impairment (other than hemianopia or quadrantanopia for the visual field loss group), the requirement for adaptive equipment in a vehicle in order to drive, and lateral spatial neglect as determined by the Stars test (Halligan, Cockburn, & Wilson, 1991).
Additional inclusion criteria for participants with hemianopia or quadrantaopia were a homonymous hemianopic or quadrantanopic visual field defect as indicated by the most recent visual field assessment in the medical record and ≥ 6 months from the brain injury date. Those persons in the age-matched reference group were required to have normal visual fields (see below), and no history of brain injury (e.g., stroke, trauma, tumor, arteriovenous malformation).
The protocol was approved by the Institutional Review Board for Human Use at the University of Alabama at Birmingham. After the purpose of the study was explained, participants were asked to sign a document of informed consent before enrolling.
Procedures
The following information was obtained through interview: (1) Demographic information (age, gender, race/ethnicity); (2) The number of co-morbid medical conditions was estimated using a general health questionnaire which has been used extensively in previous studies (Owsley, McGwin, Phillips, McNeal, & Stalvey, 2004); (3) The Driving Habits Questionnaire (Owsley, Stalvey, Wells, & Sloane, 1999) was used to confirm driving status and licensure and estimate driving exposure (days/week, miles/week driven) in the recent past.
Visual acuity was assessed binocularly using the standard protocol of the Early Treatment for Diabetic Retinopathy Study chart (Ferris, Kassoff, Bresnick, & Bailey, 1982) and expressed as logMAR. Binocular letter contrast sensitivity was measured using the Pelli-Robson chart (Pelli, Robson, & Wilkins, 1988) under the recommended testing conditions, and scored by the letter-by-letter method (Elliott, Bullimore, & Bailey, 1991). Visual acuity and contrast sensitivity were evaluated with the spectacle prescription normally worn for driving, if any. All participants had undergone a comprehensive eye examination within the past year.
Visual fields were assessed by automated static perimetry (Humphrey Field Analyzer Model 750i, Carl Zeiss Meditec, California, USA). The monocular field for each eye was measured using the central threshold 24-2 test with the SITA standard testing strategy. Results were used to confirm the presence of homonymous hemianopia, quadrantanopia, or normal visual fields. The Esterman (binocular) field test (Humphrey Field Analyzer Model 750i, Carl Zeiss Meditec, California, USA) was also used to confirm these diagnoses. For hemianopes, field loss was classified as left side versus right, complete versus incomplete, and whether or not macular sparing was present as per standard clinical definitions (Kline, 2008). For quadrantanopes, field loss was classified by left side versus right, complete versus incomplete, and superior versus inferior. Classifications were made by a rater masked to all other clinical and driving performance characteristics of participants.
Several cognitive screening tests commonly used in driving evaluations by driving specialists were also administered (McKnight & McKnight, 1999; Odenheimer, et al., 1994; Rizzo, Reinach, McGehee, & Dawson, 1997; Worringham, Wood, Kerr, & Silburn, 2006). General cognitive status was screened using the Mini-Mental Status Examination (MMSE) (Folstein, Folstein, & McHugh, 1975). Processing speed, short-term memory and attention switching were measured using the Digit Symbol Substitution Test (Wechsler, 1981), which is part of the Wechsler Adult Intelligence Scale. Trails A and B (Reitan, 1955) were used to examine visual search, processing speed, mental flexibility, and executive function. Medical record review also identified if participants had undergone scanning training during previous occupational therapy. The useful field of view test (UFOV®) was not administered (even though it is commonly used in driving assessment clinics to evaluate divided attention) because when taking the UFOV® test, the person fixates on the center of the screen and the peripheral target duration is so brief there is no opportunity to scan; thus a person with hemianopia would by definition miss all targets in their affected field, not because of an attention problem but because they are not visible to the person.
On-road driving performance was evaluated under in-traffic conditions in a dual-brake vehicle (Chevrolet Impala 2007 with automatic transmission) using the same route for each participant. The same occupational therapist did all of the evaluations; this person has 8 years of clinical experience in the assessment and rehabilitation of drivers with a wide variety of medical conditions including brain injury, neurological diseases, vision impairment, and cognitive impairment. She sat in the front passenger seat, had access to the dual brake, and was responsible for monitoring driving safety. The design of the route was based on our previous research with functionally impaired drivers (Bowers, Peli, Elgin, McGwin, & Owsley, 2005; Wadley, et al., 2009; Wood, Anstey, Kerr, Lacherez, & Lord, 2008). The route covered 14.1 miles with 6.3 miles of non-interstate driving in residential and commercial areas of a city and 7.8 miles of interstate driving in a city. It included both simple and complex intersections and encompassed a broad range of traffic densities and operational maneuvers.
Before beginning the on-road assessment, the occupational therapist asked participants to carry out a series of basic driving maneuvers in a parking lot, devoid of other traffic, to ensure they had adequate vehicle control and to allow them to become familiar with the vehicle. Once the occupational therapist was satisfied that a participant exhibited adequate control, the on-road driving evaluation began. It started in low traffic city streets in a residential neighborhood and proceeded to busier roads, then interstate driving, and finally city non-interstate driving in a commercial area. Driving evaluations were held between 9am and 3pm to avoid rush hour traffic and were cancelled if there was precipitation or the road was wet. If a participant did not wish to drive on the interstate, that portion of the route was omitted.
The occupational therapist used a rating system for evaluating driving performance that had five skill components that were each rated on a five-point scale: interaction/communication with other road users and pedestrians; driving style (margin of anticipation); vehicle control skills (smoothness), adjustment to traffic speed conditions, reaction to unexpected events, and unusually bad driving maneuvers (e.g., stopping in a lane on the interstate, turning the wrong way on a one-way street). The five-point scale was: 1 = driving was so unsafe that the drive was terminated (i.e., the occupational therapist asked the driver to pull-over and the evaluation stopped); 2 = exhibited a couple of unsafe maneuvers but did not reach the level of drive termination; 3 = driving was unsatisfactory but not unsafe at that time given traffic circumstances; 4 = driver exhibited a few minor driving errors (e.g., some drift within the lane); 5 = there were no obvious driving errors. The occupational therapist used the same scale to generate a rating of overall driving performance. In addition, the therapist made a clinical judgment as to whether the driver had the potential for safe driving (response options: yes with no restrictions; yes with some restrictions; no). All the above ratings were completed for non-interstate driving and interstate driving separately. Each time the occupational therapist made a verbal intervention (i.e., correction or recommendation) to the driver (e.g., “slow down,” “watch where you are in your lane”) or a physical intervention (applying the dual brake or taking the wheel), it was recorded on the score sheet.
As is standard in clinical practice, the occupational therapist was aware of the medical and functional characteristics of the clients she was evaluating on the road. However, because of the potential of bias and its impact on interpreting the results, we were interested in the extent to which the therapist’s ratings about quality of driving would be in agreement with a person in the backseat masked with respect to the medical and functional characteristics of the driver. The backseat evaluator also rated the quality of driving on a five-point scale. This evaluator was not a driving rehabilitation specialist but had extensive training in using the rating scale. Comparison of the ratings from the occupational therapist and backseat evaluator was designed to provide some information for research purposes about the reliability of the occupational therapist’s judgments with respect to safe driving (the main dependent variable in the study).
Statistical Analysis
Participants with hemianopia and quadrantanopia were compared to participants with normal visual fields with respect to demographic, medical/cognitive, functional, and driving characteristics using t- and chi-square tests for continuous and categorical variables, respectively. When appropriate the Wilcoxon rank sum test and Fisher’s exact test were used. P-values of ≤ 0.05 (two-sided) were considered statistically significant.
Results
There were 22 participants with hemianopia, 8 with quadrantanopia, and 30 participants with normal visual fields, making a total of 60 participants. Their demographic, health, and functional characteristics are in Table 1. Both the group with hemianopia and the group with quadrantanopia were similar to the group having normal visual fields with respect to the distributions of age, race, and MMSE (all had MMSE scores ≥ 24). The drivers with hemianopia or quadrantanopia were more likely to be men than those with normal visual fields. The number of chronic medical conditions was significantly higher in the field loss groups compared to the controls. Although persons in the hemianopia group had slightly worse visual acuity and contrast sensitivity than those in the normal visual field group, their visual acuity was still at a high level, averaging 20/25 or better, as was their contrast sensitivity (averaging 1.7–1.8). There was no difference between the quadrantanopic group and the normals on either acuity or contrast sensitivity. Scores for visual processing speed and attentional skills as assessed by Trails A, Trails B, and the DSST were worse in those with hemianopia compared to the normal visual field group. Participants with quadrantanopia had worse Trails A and DSST scores than did those with normal fields, but their Trails B scores were not different to those of the normal group.
Table 1.
Characteristics of drivers with normal visual fields, hemianopia, and quadrantanopia.
| Normal Visual Fields N =30 | Hemianopia N = 22 | p-value normal visual field vs. hemianopia | Quadrantanopia N = 8 | p-value normal visual field vs. quadrantanopia | |
|---|---|---|---|---|---|
| Age, years, mean (SD) | 52 (19) | 52 (20) | .8922 | 55 (22) | .7121 |
| Gender, n (%) | |||||
| Female | 20 (67) | 9 (41) | .0647 | 2 (25) | .0339 |
| Male | 10 (33) | 13 (59) | 6 (75) | ||
| Race, n (%) | |||||
| African American | 5 (17) | 2 (9) | .3832 | 0 (0) | .2153 |
| White, non-Hispanic | 25 (83) | 19 (86) | 8 (100) | ||
| Other1 | 0 (0) | 1 (5) | 0 (0) | ||
| # Chronic Medical Conditions, mean (SD) | 2.2 (1.5) | 5.5 (3.2) | < .0001 | 4.8 (1.8) | .0003 |
| MMSE score, M (SD) | 29.0 (1.4) | 28.4 (1.6) | .1871 | 28.6 (.7) | .5131 |
| Visual acuity, logMAR, M (SD) | −0.13 (.27) | 0.08 (.32) | .0121 | −0.02 (.32) | .3445 |
| Contrast sensitivity, log sensitivity, M(SD) | 1.83 (.12) | 1.73 (.19) | .0273 | 1.79 (.13) | .3669 |
| Trails A, time to complete, seconds, M (SD) | 33 (11) | 51 (30) | .0027 | 45 (19) | .0215 |
| Trails B, time to complete, seconds, M (SD) | 81 (37) | 127 (93) | .0185 | 106 (48) | .1231 |
| Digit Symbol Substitution, # correct, M (SD) | 54.2 (12.8) | 40.7 (14.2) | .0008 | 42.4 (11.6) | .0242 |
One participant chose not to respond to this item.
The most common cause of hemianopia or quadrantanopia was cerebral vascular accident (CVA), with the balance attributable to trauma, tumor, arteriovenous malformation, or presumed congenital abnormalities (Table 2). Of those with hemianopia, most had left hemianopia (17 of 22, 77%) compared to 23% with right hemianopia, and for nine of 22 hemianopes the field loss was complete. Eight of 22 hemianopes had macular sparing. For the quadrantanopes, the quadrant with loss was half the time on the right versus left. Five of eight had field loss in quadrants in the superior field with the balance in the inferior field. Two of eight quadrantanopes had field loss in the affected quadrant that was complete. The time passed since brain injury was highly variable, but all participants except for one were ≥ 1 year from the date of injury and almost half (14 of 30) were ≥ 4 years from injury.
Table 2.
Brain injury and field loss characteristics of patients with hemianopia and quadrantanopia
| Hemianopic Participants (N=22) | n (%) |
|---|---|
| Etiology of brain injury, n (%) | |
| Cerebrovascular accident (CVA) | 12 (54.6) |
| Tumor | 2 (9.1) |
| Trauma | 5 (22.7) |
| Arteriovenous malformation | 2 (9.1) |
| Congenital brain abnormality | 1 (4.5) |
| Laterality of field loss, n (%) | |
| Right | 5 (22.7) |
| Complete | 1 (4.5) |
| Incomplete | 4 (18.2) |
| Left | 17 (77.3) |
| Complete | 8 (36.4) |
| Incomplete | 9 (40.9) |
| Macular sparing, n (%) | |
| Yes | 8 (36.4) |
| No | 14 (63.6) |
| Quadrantanopic Participants (N=8) | n (%) |
| Etiology of brain injury, n (%) | |
| Cerebrovascular accident (CVA) | 6 (75.0) |
| Tumor | 1 (12.5) |
| Congenital brain abnormality | 1 (12.5) |
| Quadrant of field loss, n (%) | |
| Right superior | 3 (37.5) |
| Complete | 2 (25) |
| Incomplete | 1 (12.5) |
| Right inferior | 1 (12.5) |
| Complete | 0 (0) |
| Incomplete | 1 (12.5) |
| Left superior | 2 (25) |
| Complete | 0 (0) |
| Incomplete | 2 (25) |
| Left inferior | 2 (25) |
| Complete | 0 (0) |
| Incomplete | 2 (25) |
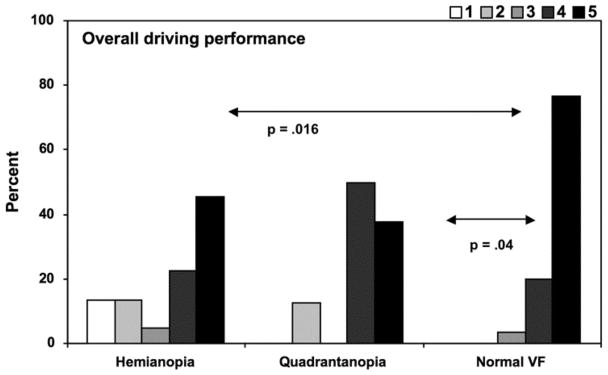
The occupational therapist’s ratings for overall driving performance on the non-interstate portion of the route are in Figure 1. For drivers with normal visual fields, the vast majority (> 90%), although not all, drove with no obvious driving errors (rating 5) or had only a few minor driving errors (rating 4) in all skills evaluated including overall driving performance scores. For drivers with hemianopia, about 2/3 to 3/4 drove with no obvious driving errors or had only a few minor errors on all skills evaluated (range 59.1–81.8%). When the distribution of ratings is compared for drivers with hemianopia versus those with normal fields, those with hemianopia were more likely to receive lower (poorer) ratings (p = .016). For drivers with quadrantanopia under non-interstate conditions, 7 of 8 (87.5%) drivers drove with no obvious driving errors or had only a few minor errors. One of 8 drivers (12.5%) had problems with all skills evaluated (scoring ≤ 3). The distribution of ratings for quadrantanopic drivers is displaced to lower ratings as compared to those with normal visual fields (p=.04).
Figure 1.
Non-interstate driving: Percent of each group rated by the occupational therapist as 1 through 5 for overall driving performance. 1 = terminate the drive, 2 = unsafe driving, 3 = unsatisfactory driving, 4 = a few minor errors, 5 = no obvious errors. See text for further explanation. Group comparisons indicated by horizontal lines labeled with p-values.
It is useful to consider which specific driving skills were problematic for hemianopic and quadrantanopic drivers for non-interstate driving (Table 3). The distribution of ratings for hemianopic drivers are lower for all skills evaluated as compared to drivers with normal fields, except for interaction/communication with other road users, which was similar between the two groups. The percentage of hemianopic drivers exhibiting problems (defined as scores of ≤ 3) for all skills evaluated was greater than the percentage of drivers with normal visual fields exhibiting these problems. For example, 40.9% of hemianopic drivers exhibited difficulty with vehicle control skills, 36.3% for adjustment to traffic speed conditions, 27.3% for reaction to unexpected events, and 27.3% for unusually bad driving maneuvers. The corresponding percentages for drivers with normal visual fields were 6.7%, 6.7%, 0%, and 0%, respectively. With respect to quadrantanopic drivers, their distribution of ratings for non-interstate driving, compared to drivers with normal fields was displaced to lower ratings for driving style (margin of anticipation), adjustment to traffic speed conditions, and unusual bad driving behaviors (p < .05). However, this difference was largely due to one quadrantanopic driver who had serious problems on the road.
Table 3.
Non-interstate driving: Number and percent in each group rated by the occupational therapist as 1 through for specific driving skills: 1 = terminate drive, 2 = unsafe driving, 3 = unsatisfactory driving, 4 = a few minor flaws, and 5 = flawless. See text for further explanation.
| Ratings for each skill evaluated | Drivers with Normal Fields | Hemia-nopia | p-value normal visual field vs. hemianopia | Quadrant-anopia | p-value normal visual field vs. quadrantanopia |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | |||
| N=30 | N=22 | N=8 | |||
| Driving style: margin of anticipation | |||||
| 1 | 0 (0) | 1 (4.6) | .0037 | 0 (0) | .0237 |
| 2 | 0 (0) | 0 (0) | 1 (12.5) | ||
| 3 | 0 (0) | 3 (13.6) | 0 (0) | ||
| 4 | 1 (3.3) | 4 (18.2) | 2 (25) | ||
| 5 | 29 (96.7) | 14 (63.6) | 5 (62.5) | ||
| Interaction with other road users | |||||
| 1 | 0 (0) | 1 (4.5) | .3010 | 0 (0) | .3086 |
| 2 | 0 (0) | 4 (18.2) | 1 (12.5) | ||
| 3 | 1 (3.3) | 2 (9.1) | 0 (0) | ||
| 4 | 8 (26.7) | 5 (22.7) | 3 (37.5) | ||
| 5 | 21 (70) | 10 (45.5) | 4 (50) | ||
| Vehicle control skills (smoothness) | |||||
| 1 | 0 (0) | 1 (4.5) | .0257 | 0 (0) | .0534 |
| 2 | 0 (0) | 4 (18.2) | 1 (12.5) | ||
| 3 | 2 (6.7) | 4 (18.2) | 0 (0) | ||
| 4 | 6 (20.0) | 3 (13.6) | 4 (50) | ||
| 5 | 22 (73.3) | 10 (45.5) | 3 (37.5) | ||
| Adjustment to traffic speed conditions | |||||
| 1 | 0 (0) | 1 (4.5) | .0115 | 0 (0) | .0495 |
| 2 | 0 (0) | 4 (18.2) | 1 (12.5) | ||
| 3 | 2 (6.7) | 3 (13.6) | 0 (0) | ||
| 4 | 3 (10) | 4 (18.2) | 3 (37.5) | ||
| 5 | 25 (83.3) | 10 (45.5) | 4 (50) | ||
| Reaction to unexpected events | |||||
| 1 | 0 (0) | 1 (4.5) | .0116 | 0 (0) | .0528 |
| 2 | 0 (0) | 1 (4.5) | 1 (12.5) | ||
| 3 | 0 (0) | 4 (18.2) | 0 (0) | ||
| 4 | 2 (6.7) | 2 (9.1) | 2 (25.0) | ||
| 5 | 28 (93.3) | 14 (63.7) | 5 (62.5) | ||
| Unusually bad driving maneuvers | |||||
| 1 | 0 (0) | 1 (4.6) | .0021 | 0 (0) | .0237 |
| 2 | 0 (0) | 4 (18.2) | 1 (12.5) | ||
| 3 | 0 (0) | 1 (4.6) | 0 (0) | ||
| 4 | 1 (3.3) | 2 (9.0) | 2 (25) | ||
| 5 | 29 (96.7) | 14 (63.6) | 5 (62.5) |
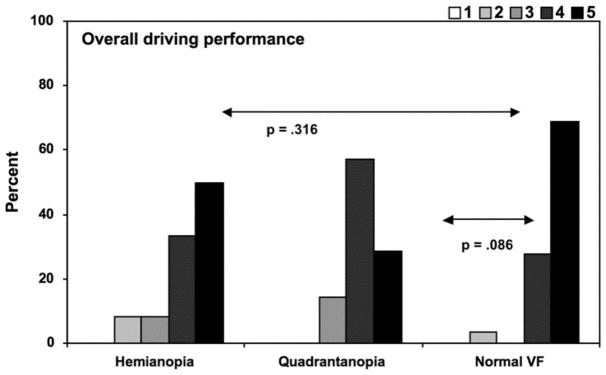
In evaluating the results for interstate driving, it is important to keep in mind that in order for a driver to be evaluated on the interstate, two criteria had to be met. First, the occupational therapist judged that the non-interstate driving was at a safe standard such that interstate driving was appropriate. Second, the participant had to choose to drive on the interstate, as some of the field loss group reported that they usually avoided interstate driving. Meeting these criteria were 12 of 22 persons with hemianopia and 7 of 8 persons with quadrantanopia. Although all 30 participants with normal visual fields met these criteria, one person was not evaluated on the interstate since as soon as she entered the interstate, a severe traffic jam was encountered (so the driver left the interstate at the next exit). Results were that for interstate driving there were no differences in the distribution of the ratings for specific skills for participants with normal fields versus those participants with hemianopia or quadrantanopia who met the criteria for going on the interstate portion of the route.
Table 4 displays the occupational therapist’s clinical judgment with respect to each driver’s potential for safe driving. On the non-interstate, 100% of drivers with normal visual fields were judged by the occupational therapist to have the potential for safe driving with no restrictions. Compared to drivers with normal visual fields, a lower percentage of drivers with hemianopia (17 of 22, 77.3%) – 16 with no restrictions and 1 with restrictions -- were judged to have the potential for safe driving. Seven of 8 (87.5%) persons with quadrantanopia were judged by the occupational therapist to have the potential for safe driving on the non-interstate. With respect to interstate driving, it is important to keep in mind when viewing Table 3 that some drivers were not evaluated on the interstate because they preferred not to drive on the interstate or the occupational therapist did not permit interstate driving. All drivers with normal visual fields except one (28 of 29, 96.6%) were judged to have the potential for safe driving with no restrictions on the interstate. Of those with hemianopia or quadrantanopia who drove on the interstate, the vast majority (91.7% and 85.7 respectively) were judged to have the potential for safe driving with no restrictions.
Table 4.
Potential for safe driving as judged by the occupational therapist
| Drivers with Normal Fields | Hemianopia | p-value normal visual field vs. hemianopia | Quadrantanopia | p-value normal visual field vs. quadrantanopia | |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | |||
| Non-interstate driving | N=30 | N=22 | .0098 | N=8 | .0497 |
| Yes, with no restrictions | 30 (100) | 16 (72.7) | 7 (87.5) | ||
| Yes, but with restrictions | 0 (0) | 1 (4.6) | 0 (0) | ||
| No | 0 (0) | 5 (22.7) | 1 (12.5) | ||
| Interstate driving1 | N=29 | N=12 | .5049 | N = 7 | .356 |
| Yes, with no restrictions | 28 (96.6) | 11 (91.7) | 6 (85.7) | ||
| Yes, but with restrictions | 0 (0) | 0 (0) | 1 (14.3) | ||
| No | 1 (3.4) | 1 (8.3) | 0 (0) |
10 hemianopic drivers, 1 quadrantanopic drivers, and 1 driver with normal visual fields were not evaluated on the interstate.
Agreement (weighted kappa) between the occupational therapist’s rating of overall driving performance on the 5-point scale and that rating by the backseat evaluator who was masked to the clinical characteristics of drivers was 0.79 on the non-interstate and 0.73 on the interstate. Agreement between the occupational therapist and the backseat evaluator was also evaluated for “pass” (scores of 3, 4 or 5 on overall driving performance) versus “fail” (scores of 1 or 2 on overall driving performance). For non-interstate driving, agreement was 1.0; for interstate driving, agreement was .79 (although there was only 1 driver out of 48 where there was disagreement).
The occupational therapist was more likely to make verbal interventions for drivers with hemianopia and quadrantanopia as compared to drivers with normal visual fields (Table 5). Specifically, about half of the hemianopic (45.5%) or quadrantanopic drivers (50%) received verbal feedback (e.g., “slow down,” “watch where you are in your lane”), as compared to 16.7% (5 of 30) of drivers with normal visual fields. In terms of physical interventions, the therapist made corrections for 40.9% (9 of 22) of hemianopic drivers but only 1 driver with normal visual fields. These physical interventions consisted of using the dual brake to slow the vehicle and briefly taking the wheel because the driver was drifting in the lane. There was no difference in the percentage of interventions between the quadrantanopic drivers and those with normal visual fields.
Table 5.
Number of participants where the occupational therapist had to verbally or physically make corrections at any time during the drive (regardless of whether on the non-interstate or not).
| Drivers with Normal Fields N = 30 | Hemianopia N = 22 | p-value normal visual field vs. hemianopia | Quadrantanopia N = 8 | p-value normal visual field vs. quadrantanopia | |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | |||
| Verbally intervene | .0236 | .0488 | |||
| Yes | 5 (16.7) | 10 (45.5) | 4 (50) | ||
| No | 25 (83.3) | 12 (54.5) | 4 (50) | ||
| Physically intervene | .0007 | .3022 | |||
| Yes | 1 (3.3) | 9 (40.9) | 1 (12.5) | ||
| No | 29 (96.7) | 13 (59.1) | 7 (87.5) |
We were interested in which of the in-clinic tests and other patient characteristics (i.e., as listed in Tables 1 and 2) were associated with the occupational therapist’s judgment that there was a potential for safe driving with no restrictions, since these characteristics might provide information about prognostic indicators for a return to driving following brain injury causing hemianopia or quadrantopia. Better performance on the following in-clinic tests was associated with the therapist’s judgment that there was a potential for safe driving: contrast sensitivity (p=.003), average visual field sensitivity in the intact field (p=.016), and Trails A (p=.0036). Other characteristics of the hemianopia or quadrantanopia (visual field side or quadrant affected, whether field loss in the affected area was complete, whether there was macular sparing) were not associated with the therapist’s judgment of potential for safe driving (all p >.15). Six of 22 participants with hemianopia or quadrantanopia had undergone in-clinic scanning training by an occupational therapist as part of their post-brain injury rehabilitation, but having had the training was not associated with the therapist’s rating of whether there was potential for safe driving (p=.3021).
Discussion
We embarked on this study to address the stereotypic notion held by licensing jurisdictions, as well as many health care providers, that drivers with hemianopic or quadrantanopic field defects are unfit to drive. Our results indicate that although drivers with hemianopia and quadrantanopia were more likely to receive lower skill ratings from the occupational therapist than drivers with normal visual fields, some drivers with hemianopia and quadrantanopia received good driving performance ratings similar to those received by persons with normal visual fields. Up to two-thirds of the drivers in our study with hemianopia and quadrantanopia drove with no obvious driving errors or had only a few minor errors on non-interstate roads as assessed by the driving specialist and were judged to have the potential for safe driving. These results are consistent with an earlier report (Racette & Casson, 2005). It is important to emphasize that we did not enroll patients with lateral spatial neglect. There is little or no controversy that hemianopic or quadrantanopic clients with lateral spatial neglect should not drive since they behave as if objects in the affected field area do not exist. In addition, all drivers in our sample had MMSE scores ≥ 24.
Our findings provide strong evidence that some persons with hemianopia and quadrantanopia can demonstrate that they are fit to drive if given the opportunity to undergo a standardized on-road evaluation by an occupational therapist who specializes in driving. These specialists are specifically trained to evaluate drivers who have functional impairments that could potentially interfere with safe driving skills. The occupational therapist’s ratings were in good agreement with those of the backseat evaluator who was masked to drivers’ medical and functional characteristics, implying that the results are not attributable to the therapist’s bias based on knowledge of each driver’s medical history. In addition to on-road driving evaluations, driving specialists administer in-clinic screening tests and assessments of visual, cognitive, and motor skills used in driving. Our data suggest that drivers with better contrast sensitivity and average light sensitivity in the remaining areas of visual field and those with faster processing speeds were more likely to be judged as safe drivers. However, these findings are preliminary and await confirmation through larger sample studies. Ultimately, it is critical to have an in-clinic battery that is evidence-based so that its tests and assessments efficiently focus on those skills that are established prognostic indicators of driving fitness.
One might question, if about 40% of the hemianopic drivers had verbal or physical interventions from the occupational therapist, how could she judge about 75% of hemianopic drivers as having the potential for safe driving? First, interventions are not only carried out for egregious behaviors but also for the mere suspicion that a dangerous maneuver may occur and provide the opportunity for the therapist to provide immediate feedback to their client regarding their driving. Thus, they are basically preventative actions, but in many cases may not have been needed. Second, the therapist’s judgment about the potential for safe driving is based on all aspects of the driving performance, not just single snapshots in time. Previous research confirms that judgments of overall driving fitness, although related to evaluations of specific driving behaviors, are not synonymous with them (Di Stefano & MacDonald, 2003; Kay, et al., 2008).
These results raise important questions regarding the fairness of governmental policies that categorically deny licensure of persons with hemianopia or quadrantanopia. This study and that of Racette and Casson (2005) suggest a more rational and fair policy would be to allow for an individualized assessment of driving fitness for persons with these conditions, conducted by an occupational therapist who specializes in driving assessment and rehabilitation.
For those drivers with hemianopia who received ratings of unsatisfactory or worse (≤3), the most noteworthy problem area as rated by the occupational therapist was vehicle control skills (e.g., staying in one’s lane), with about 40% of drivers exhibiting this problem to varying degrees. The finding of vehicle control skill problems is consistent with previous research involving on-road assessment or performance on a driving simulator, which has noted that hemianopic drivers often have difficulty with steering steadiness (Szlyk, et al., 1993; Tant, et al., 2002). What remains to be determined is whether a driving rehabilitation program (e.g., scanning or visual search training while driving, practice in lane-keeping) could improve driving skills in problem drivers with hemianopia or quadrantanopia. This is an important issue since many persons with field impairment secondary to brain injury want to eventually return to driving. Persons with hemianopia are sometimes prescribed spectacles that provide a prismatic correction to re-locate or expand the field (Bowers, Keeney, & Peli, 2008; Perez & Jose, 2003; Smith, Weiner, & Lucero, 1982). At present there is no evidence that such optical devices improve on-road driving performance or driver safety in persons with hemianopia (Szlyk, Seiple, Stelmack, & McMahon, 2005). It is important to note that none of our hemianopic or quadrantanopic drivers, including those who were judged by the occupational therapist to have good overall driving performance, wore prismatic devices for the driving assessments. This suggests that hemianopic drivers have strategies that they use to compensate for their field loss during driving, and that a prismatic correction is not a necessary condition for safe driving in this population. It is important to understand what these strategies are so that they can be incorporated into evidence-based driving rehabilitation programs.
We designed our study so that it could focus on a specific subpopulation of drivers with hemianopia or quadrantanopia, as a starting point for beginning an exploration of the issue. Excluded from the sample were persons with lateral spatial neglect as mentioned earlier, since there is little disagreement that clinicians appropriately recommend no driving to such persons. We also excluded persons who had no interest in returning to driving, since motivation to be a driver is required to carry out the skill effectively. Persons with hemiparesis were excluded, many of whom may have the potential for safe driving if adaptive vehicular controls were made available. Future research should address driving fitness in persons with the combined impairments of hemianopia and hemiparesis. In addition, in our study design, we are unable to dissociate the impact of the brain injury per sé from the impact of the visual field impairment on driving performance, since the two co-occur in all the drivers with hemianopia and quadrantanopia.
In summary, this study has highlighted the need to provide the opportunity for individual driving evaluations for persons with hemianopia and quadrantanopia who want to return to driving following brain injury. Denying these persons the opportunity to demonstrate driving fitness as part of the rehabilitation process is inappropriate since some persons with hemianopia and quadrantanopia display acceptable driving skills that are indistinguishable from drivers with no field loss. Our results also suggest that policies categorically prohibiting persons with these functional impairments from holding a driver’s license without the opportunity to demonstrate driving fitness need to be re-evaluated. These results underscore the importance of driving assessment and rehabilitation services as part of a comprehensive rehabilitation program following a brain injury that impairs vision.
Figure 2.
Interstate driving: Percent of each group rated by the occupational therapist as 1 through 5 for overall driving performance. 1 = terminate the drive, 2 = unsafe driving, 3 = unsatisfactory driving, 4 = a few minor errors, 5 = no obvious errors. See text for further explanation. Group comparisons indicated by horizontal lines labeled with p-values. Some participants did not go on the interstate if they did not typically drive on the interstate or the therapist did not allow interstate driving based on non-interstate driving performance.
Acknowledgments
This research was funded by National Institutes of Health grants P30-AG22838 and R21-EY14071, EyeSight Foundation of Alabama, Research to Prevent Blindness Inc., and a QUT PDL grant.
References
- Bowers A, Peli E, Elgin J, McGwin G, Owsley C. On-road driving with moderate visual field loss. Optometry and Vision Science. 2005;82(8):657–667. doi: 10.1097/01.opx.0000175558.33268.b5. [DOI] [PubMed] [Google Scholar]
- Bowers AR, Keeney K, Peli E. Commuity-based trial of a peripheral prism visual field expansion device for hemianopia. Archives of Ophthalmology. 2008;126:657–664. doi: 10.1001/archopht.126.5.657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassidy TP, Bruce DW, Gray CS. Visual field loss after stroke: Confrontation and perimetry in the assessment of recovery. Journal of Stroke and Cerebrovascular Diseases. 2001;10(3):113–117. doi: 10.1053/jscd.2001.25457. [DOI] [PubMed] [Google Scholar]
- Di Stefano M, MacDonald W. Assessment of older drivers: Relationships among on-road errors, medical conditions and test outcome. Journal of Safety Research. 2003;34:415–429. doi: 10.1016/j.jsr.2003.09.010. [DOI] [PubMed] [Google Scholar]
- Elliott DB, Bullimore MA, Bailey IL. Improving the reliability of the Pelli-Robson contrast sensitivity test. Clinical Vision Science. 1991;6:471–475. [Google Scholar]
- Ferris FL, Kassoff A, Bresnick GH, Bailey I. New visual acuity charts for clinical research. American Journal of Ophthalmology. 1982;94:91–96. [PubMed] [Google Scholar]
- Folstein MF, Folstein SW, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Fonda SJ, Wallace RB, Herzog AR. Changes in driving patterns and worsening depressive symptoms among older adults. Journal of Gerontology: Social Sciences. 2001;56B(6):S343–S351. doi: 10.1093/geronb/56.6.s343. [DOI] [PubMed] [Google Scholar]
- Fox GK, Bowden SC, Smith DS. On-road assessment of driving competence after brain impairment: Review of current practice and recommendations for a standardized examination. Archives of Physical Medicine and Rehabilitation. 1998;79:1288–1296. doi: 10.1016/s0003-9993(98)90277-5. [DOI] [PubMed] [Google Scholar]
- Freeman EE, Munoz B, Turano KA, West SK. Measures of visual function and their association with driving modification in older adults. Investigative Ophthalmology & Visual Science. 2006;47(2):514–520. doi: 10.1167/iovs.05-0934. [DOI] [PubMed] [Google Scholar]
- Gilhotra JS, Mitchell P, Healey PR, Cumming RG, Currie J. Homonymous visual vield defects and stroke in an older population. Stroke. 2002;33:2417–2420. doi: 10.1161/01.str.0000037647.10414.d2. [DOI] [PubMed] [Google Scholar]
- Halligan PW, Cockburn J, Wilson BA. The behavioural assessment of visual neglect. Neuropsychological Rehabilitation. 1991;1:5–32. [Google Scholar]
- Hu PS, Young JR. Summary of Trends. 1995 Nationwide Personal Transportation Survey (No. FHWA-PL-00–006) Washington, DC: U.S. Department of Transportation, Federal Highway Administration; 1999. [Google Scholar]
- Hunt LA, Murphy CF, Carr D, Duchek JM, Buckles V, Morris JC. Reliability of the Washington University road test: A performance-based assessment for drivers with dementia of the Alzheimer type. Archives of Neurology. 1997;54:707–712. doi: 10.1001/archneur.1997.00550180029008. [DOI] [PubMed] [Google Scholar]
- Justiss MD, Mann WC, Stav W, Velozo C. Development of a behind-the-wheel driving performance assessment for older adults. Topics in Geriatric Rehabilitation. 2006;22:121–128. [Google Scholar]
- Kay L, Bundy A, Clemson L, Jolly N. Validity and reliability of the on-road driving assessment with senior drivers. Accident Analysis & Prevention. 2008;40:751–759. doi: 10.1016/j.aap.2007.09.012. [DOI] [PubMed] [Google Scholar]
- Kline LB. Visual fields. In: Kline LB, editor. Neuro-Ophthalmology Review Manual. Thorofare NJ: Slack Inc; 2008. pp. 1–44. [Google Scholar]
- Marottoli RA, de Leon CFM, Glass TA, Williams CS, Cooney LM, Jr, Berkman LF. Consequences of driving cessation: Decreased out-of-home activity levels. Journal of Gerontology: Social Sciences. 2000;55B(6):S334–S340. doi: 10.1093/geronb/55.6.s334. [DOI] [PubMed] [Google Scholar]
- McKnight AJ, McKnight AS. Multivariate analysis of age-related driver ability and performance deficits. Accident Analysis and Prevention. 1999;31:445–454. doi: 10.1016/s0001-4575(98)00082-7. [DOI] [PubMed] [Google Scholar]
- Odenheimer GL, Beaudet M, Jette AM, Albert MS, Grande L, Minaker KL. Performance-based driving evaluation of the elderly driver: Safety, reliability, and validity. Journal of Gerontology: Medical Sciences. 1994;49(4):M153–M159. doi: 10.1093/geronj/49.4.m153. [DOI] [PubMed] [Google Scholar]
- Owsley C, McGwin G., Jr Vision impairment and driving. Survey of Ophthalmology. 1999;43(6):535–550. doi: 10.1016/s0039-6257(99)00035-1. [DOI] [PubMed] [Google Scholar]
- Owsley C, McGwin G, Phillips JM, McNeal SF, Stalvey BT. Impact of an educational program on the safety of high-risk, visually impaired, older drivers. American Journal of Preventive Medicine. 2004;26(3):222–229. doi: 10.1016/j.amepre.2003.12.005. [DOI] [PubMed] [Google Scholar]
- Owsley C, Stalvey B, Wells J, Sloane ME. Older drivers and cataract: Driving habits and crash risk. Journal of Gerontology: Medical Sciences. 1999;54A(4):M203–M211. doi: 10.1093/gerona/54.4.m203. [DOI] [PubMed] [Google Scholar]
- Pelli DG, Robson JG, Wilkins AJ. The design of a new letter chart for measuring contrast sensitivity. Clinical Vision Science. 1988;2(3):187–199. [Google Scholar]
- Perez AM, Jose RT. The use of Fresnel and ophthalmic prisms with persons with hemianopic visual field loss. Journal of Visual Impairment and Blindness. 2003;97:173–176. [Google Scholar]
- Racette L, Casson EJ. The impact of visual field loss on driving performance: evidence from on-road driving assessments. Optometry and Vision Science. 2005;82(8):668–674. doi: 10.1097/01.opx.0000174719.25799.37. [DOI] [PubMed] [Google Scholar]
- Reitan R. The relation of the Trail Making Test to organic brain damage. Journal of Consulting Psychology. 1955;19:393–394. doi: 10.1037/h0044509. [DOI] [PubMed] [Google Scholar]
- Rizzo M, Reinach S, McGehee D, Dawson J. Simulated car crashes and crash predictors in drivers with Alzheimer disease. Archives of Neurology. 1997;54:545–551. doi: 10.1001/archneur.1997.00550170027011. [DOI] [PubMed] [Google Scholar]
- Smith JL, Weiner IG, Lucero AJ. Hemianopic Fresnel prisms. Journal of Clinical Neuro-ophthalmology. 1982;2:19–22. [PubMed] [Google Scholar]
- Szlyk JP, Brigell M, Seiple W. Effects of age and hemianopic visual field loss on driving. Optometry and Vision Science. 1993;70(12):1031–1037. doi: 10.1097/00006324-199312000-00007. [DOI] [PubMed] [Google Scholar]
- Szlyk JP, Seiple W, Stelmack J, McMahon T. Use of prisms for navigation and driving in hemianopic patients. Ophthalmic & Physiological Optics. 2005;25:128–135. doi: 10.1111/j.1475-1313.2004.00265.x. [DOI] [PubMed] [Google Scholar]
- Tant M, Brouwer W, Cornelissen F, Kooijman A. Driving and visuospatial performance in people with hemianopsia. Neuropsychological rehabilitation. 2002;12(5):419–437. [Google Scholar]
- Townend BS, Sturm JW, Petsoglou C, O’Leary B, Whyte S, Crimmins D. Perimetric homonymous visual field loss post-stroke. Journal of Clinical Neuroscience. 2006;2(22):1–3. doi: 10.1016/j.jocn.2006.02.022. [DOI] [PubMed] [Google Scholar]
- Wadley VG, Okonkwo O, Crowe M, Vance DE, Ball KK, Owsley C. Mild cognitive impairment and everyday function: investigation of driving performance. Journal of Geriatric Psychiatry and Neurology. 2009 doi: 10.1177/0891988708328215. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Adult Intelligence Scale-Revised Manual. San Antonio TX: Psychological Corporation; 1981. [Google Scholar]
- Wood JM, Anstey KJ, Kerr GK, Lacherez PF, Lord S. A multidomain approach for predicting older driver safety under in-traffic toad conditions. Journal of the American Geriatrics Society. 2008;56:986–993. doi: 10.1111/j.1532-5415.2008.01709.x. [DOI] [PubMed] [Google Scholar]
- Worringham C, Wood JM, Kerr G, Silburn P. Predictors of driving assessment outcome in Parkinson’s disease. Movement Disorders. 2006;21:230–235. doi: 10.1002/mds.20709. [DOI] [PubMed] [Google Scholar]
- Zhang X, Kedar S, Lynn MJ, Newman NJ, Biousse V. Homonymous hemianopias. Neurology. 2006;66:906–910. doi: 10.1212/01.wnl.0000203913.12088.93. [DOI] [PubMed] [Google Scholar]