Abstract
Purpose
The purpose of this study is to describe the diagnosis, course, and outcome of a case of Acanthamoeba and Stenotrophomonas keratitis with a fungal keratitis in the contralateral eye.
Methods
A case of Acanthamoeba and Stenotrophomonas keratitis was diagnosed with confocal microscopy and cultures with confocal diagnosis of fungal keratitis in the fellow eye.
Results
During the initial treatment of the Acanthamoeba and Stenotrophomonas keratitis, the contralateral eye developed a keratitis that demonstrated hyphae in the corneal stroma with confocal microscopy consistent with fungal keratitis.
Conclusions
Bilateral chronic keratitis cannot be assumed to be caused by the same organism and independent cultures, and confocal microscopy needs to be performed to direct appropriate therapy.
Keywords: Acanthamoeba, Stenotrophomonas, confocal, fungus, keratitis
Introduction
Contact lens-induced infectious keratitis may be caused by a multitude of organisms. Acanthamoeba and fungi may infect the cornea separately or together.1–3 Acanthamoeba may cause bilateral keratitis.4,5 A case of contralateral fungal keratitis has not been described.
Case report
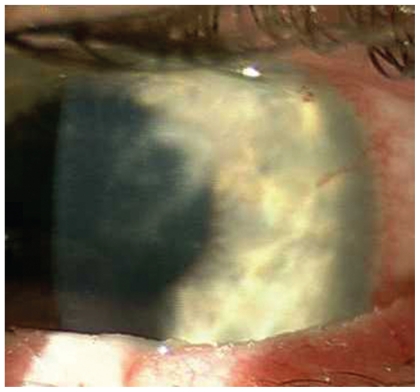
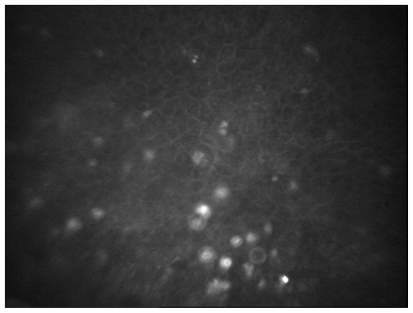
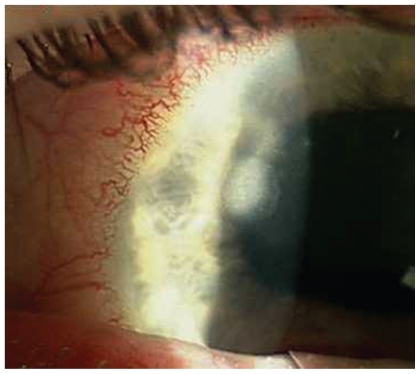
A 42-year-old male physician was referred for the evaluation of a keratitis in the left eye. He had presented to the referring ophthalmologist 2 weeks earlier with pain, photophobia, and reduced vision in his left eye, which had progressed over 2 weeks. He was a rigid gas-permeable contact lens wearer who had rinsed his contact lens and case with tap water on a regular basis. The patient had self-prescribed Tobradex® ophthalmic solution for several days before presenting to the ophthalmologist. The ophthalmologist discontinued the Tobradex and treated with Vigamox® (moxifloxacin). After several days, prednisolone actetate was started. The patient was referred 1 week later when the condition had shown no improvement. Visual acuity with correction was 20/20 in the right eye and 20/80 in the left eye. Intraocular pressures were 16 mmHg in each eye. The right cornea was clear. The left cornea showed multiple stromal infiltrates (Figure 1). Confocal microscopy of the left eye showed multiple cyst structures consistent with Acanthamoeba (Figure 2). Cultures were performed of the cornea. Scrapings of the cornea were evaluated with calcofluor white and no organisms were seen. The patient was requested to bring his contact lens case in for culturing. The patient was started on atropine 1% twice/day, Neosporin® every hour, Brolene® every hour, polyhexamethylene biguanide (PHMB) 0.02% every hour, and clotrimazole 1% every hour in the left eye. The patient showed significant improvement over 1 week with visual acuity improving to 20/40 in the left eye. One week later, the patient returned with new symptoms of pain and photophobia in his right eye. The cornea showed stromal infiltrates (Figure 3). Confocal microscopy did not demonstrate any cystic structures but did show evidence of hyphae (Figure 4). The right cornea was cultured, and the right eye was started on the same regiment as was used on the left. The contact lens case was sent for culturing. In addition, both eyes were started on natamycin 5% every hour because of the suspicion of fungal keratitis in the right eye. The corneal cultures showed no growth of bacteria, fungus, or Acanthamoeba. The left cell of the contact lens case did grow Acanthamoeba as well as Stenotrophomonas maltophilia. The right cell was culture negative. Both eyes were treated with natamycin, clotrimazole, Brolene, Neopsorin, and PHMB four times per day for 3 months. Both corneas showed complete resolution of the infiltrates and corrected vision returned to 20/20.
Figure 1.
Multiple corneal infiltrates of the left cornea.
Figure 2.
Acanthamoeba cysts in the left cornea by confocal microscopy.
Figure 3.
Multiple corneal infiltrates of the right cornea.
Figure 4.
Fungal hyphae in right cornea by confocal microscopy.
Discussion
Keratitis resulting from coinfections with Acanthamoeba and fungus or bacteria has been described.1–3 Bilateral Acanthamoeba has also been well described.4,5 We believe that this is the first case of presumed Acanthamoeba and fungal keratitis reported on contralateral eyes. This case is also the second reported case of presumed coinfection of Stenotrophomonas maltophilia and Acanthamoeba.3 Confocal microscopy has been shown to be a reliable method of detecting Acanthamoeba and fungal elements in infected corneas.6 The possibility exists that one or both of the corneas could have had combined Acanthamoeba and fungal keratitis. This case emphasizes the importance of evaluating both corneas independently when there are similar clinical presentations bilaterally. This case also illustrates the importance of employing as many modalities as possible in approaching an atypical corneal infection.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Froumis NA, Mondino BJ, Glasgow BJ. Acanthamoeba keratitis associated with fungal keratitis. Am J Ophthalmol. 2001;131(4):508–509. doi: 10.1016/s0002-9394(00)00827-8. [DOI] [PubMed] [Google Scholar]
- 2.Rumelt S, Cohen I, Lefler E, Rehany U. Corneal co-infection with Scedosporium apiospermum and Acanthamoeba after sewage-contaminated ocular injury. Cornea. 2001;20(1):112–116. doi: 10.1097/00003226-200101000-00022. [DOI] [PubMed] [Google Scholar]
- 3.Mauger TF, Craig E. Combined Acanthamoeba and Stenotrophomonas maltophilia keratitis treated with a conjunctival flap followed by penetrating keratoplasty. Cornea. 2006;25(5):631–633. doi: 10.1097/01.ico.0000214214.45070.b6. [DOI] [PubMed] [Google Scholar]
- 4.Wilhelmus KR, Jones DB, Matoba AY, Hamill MB, Pflugfelder SC, Weikert MP. Bilateral Acanthamoeba keratitis. Am J Ophthalmol. 2008;145(2):193–197. doi: 10.1016/j.ajo.2007.09.037. [DOI] [PubMed] [Google Scholar]
- 5.Voyatzis G, McElvanney A. Bilateral Acanthamoeba keratitis in an experienced two-weekly disposable contact lens wearer. Eye Contact Lens. 2007;33(4):201–202. doi: 10.1097/01.icl.0000252567.06446.7b. [DOI] [PubMed] [Google Scholar]
- 6.Parmar DN, Awwad ST, Petroll WM, Bowman RW, McCulley JP, Cavanagh HD. Tandem scanning confocal corneal microscopy in the diagnosis of suspected Acanthamoeba keratitis. Ophthalmology. 2006;113(4):538–547. doi: 10.1016/j.ophtha.2005.12.022. [DOI] [PubMed] [Google Scholar]