Abstract
Objectives
Delays in colorectal cancer (CRC) diagnosis related to colonoscopy referrals are not well studied. We tested whether certain details of information transmitted through computerized provider order entry (CPOE)-based referrals affected timeliness of diagnostic colonoscopy for patients with newly diagnosed colorectal cancer (CRC).
Methods
We studied a 6-year cohort of all newly diagnosed patients with CRC at a large tertiary care Veterans Affairs hospital and its affiliated multispecialty clinics. Referring providers included primary care clinicians, resident trainees, and other specialists. From the colonoscopy referral preceding CRC diagnosis, we determined request date, type and frequency of diagnostic clues provided (symptoms, signs, test results), notation of urgency, and documented evidence of verbal contact between referring provider and consultant to expedite referral. We compared distributions of proportions of diagnostic clues between patients with > 60 and ≤ 60 day lag and examined predictors of lag time.
Results
Of 367 electronic referrals identified with a median lag of 57 days, 178 (48.5%) had lag > 60 days. Referrals associated with longer lag times included those with “positive fecal occult blood test” (92 days, P<0.0001), “hematochezia” (75 days, P=0.02), “history of polyps” (221 days, P=0.0006), and when “screening” (versus specific symptoms) was given as reason for diagnostic colonoscopy (203 days, P=0.002). Independent predictors of shorter wait times included 3 diagnostic clues, notation of urgency, and documentation of verbal contact.
Conclusions
Attention to certain details of diagnostic information provided to consultants through CPOE-based referrals may help reduce delays in CRC diagnosis.
Keywords: delayed cancer diagnosis, colorectal cancer, colonoscopy referrals, computerized order entry, electronic medical records, primary care
INTRODUCTION
Delayed CRC diagnosis is one of the most common reasons for ambulatory diagnostic malpractice claims in the United States.1,2 Contributing factors in delayed CRC diagnosis include patient-related delays in seeking care and scheduling procedures, provider-related delays in ordering tests, and limited endoscopic capacity.3,4,4–7 We recently described the prevalence and types of missed opportunities for detecting and investigating clues that could have led to an earlier referral for colonoscopy.8 When we examined determinants of wait time between referral and diagnosis of CRC in a large tertiary care facility, we found that patients with symptoms related to CRC, abnormal lab tests, or abnormal imaging studies had a shorter lag time between referral and diagnosis compared to patients who had a positive screening test.9 These data suggest that the nature of referral information provided to the gastroenterologist could influence lag time between referral and colonoscopy performance.
In many integrated electronic medical records (EMRs), practitioners use computerized provider order entry (CPOE) to generate referral requests and relay relevant clinical information to the consultant. Studies of non-CPOE referrals have shown that providers do not consistently provide accurate clinical information on referral requests.10–12 Whether the nature and amount of information influences the outcome of the referral is not clear. For instance, the documentation of certain diagnostic clues or flagging referrals as “urgent” may be associated with shorter lag times for colonoscopy. We sought to determine the association between the quality and quantity of information transmitted in colonoscopy requests using CPOE and the timeliness of colonoscopy performance. We also examined the characteristics of referral requests associated with time lags of greater than 60 days from initial request to colonoscopy performance.
METHODS
We studied a cohort of all newly diagnosed patients with confirmed primary CRC diagnosed between June 2001 and June 2007 at a tertiary care Veterans Affairs facility. Colonoscopy referrals are entered through a CPOE system, which has been used in the VA setting for close to a decade (Figure 1). Most outpatient referrals are initiated by approximately 50 primary care providers who practice at the facility or at one of its five community-based satellite clinics. Other referring providers include resident trainees and specialists. Most inpatient referrals are initiated by residents on medical or surgical floors. Requests are then screened by several gastroenterologists on rotating basis. At this institution and many others, endoscopic capacity is limited by the number of endoscopy rooms, preparation and recovery space, and availability of gastroenterologists.
Figure 1.
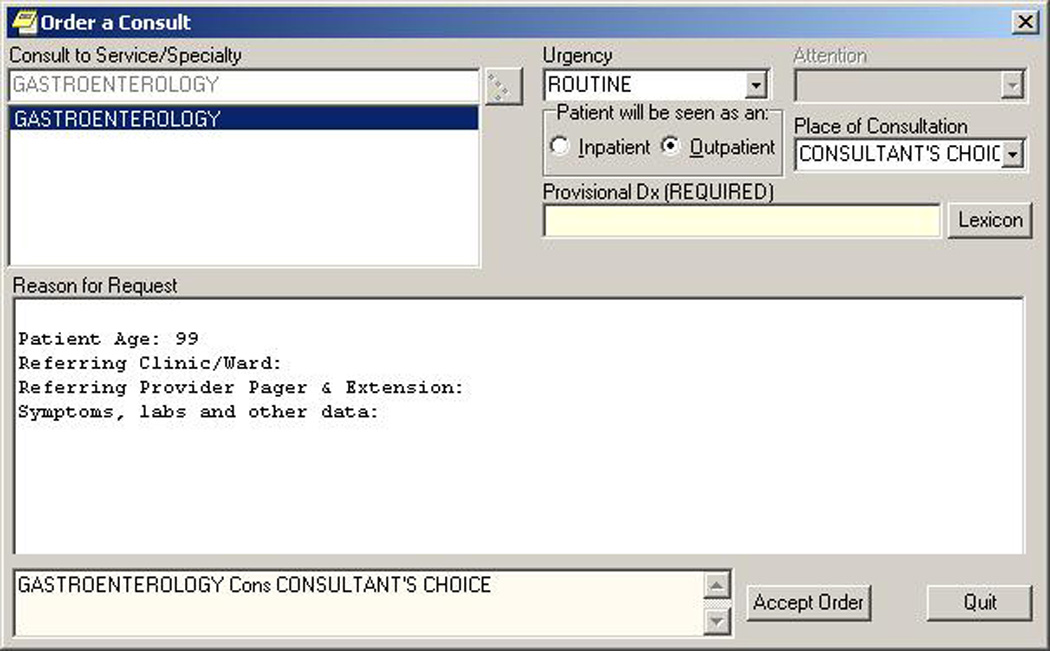
Order entry template for colonoscopy referrals
We examined referrals that requested a diagnostic colonoscopy or sigmoidoscopy or requested the consultant to address certain diagnostic clues suggestive of CRC. We thus focused our study only on patients for whom the referring physician requested a diagnostic colonoscopy or screening for high risk individuals. The primary modality of CRC screening in the VA is fecal occult blood test (FOBT) and only a small proportion of colonoscopies requested are related to screening in average risk individuals. 13,14
We excluded patients diagnosed (or who received their CRC diagnosis care) outside the institution and those with recurrent CRC. We also excluded CRC diagnosed by colonoscopy requested solely for screening in otherwise asymptomatic patients. Using the integrated EMR, we conducted a detailed review of information contained in the electronic referral request, as well as colonoscopy performance and patient characteristics. Currently the only information templated is patient age, referring clinic/ward, details of referring provider and their contact information, and free-text information about symptoms, labs, and other data. For patients with more than one referral, we examined only the first request. The study was approved by the local Institutional Review Board.
Data Collection Procedures
Prior to the study we designed and pilot tested a data collection instrument for the variables of interest. The study team supervised and trained reviewers to ensure reliable and consistent data collection. Reviewers documented the following:
Referral request information: Date of request; type of information provided in the request (i.e., diagnostic clues such as symptoms, signs, test results); referral origin (inpatient or outpatient); notation of urgency (< 7 days, < 30 days, next available, or routine); specialty of the referring provider; and documented evidence of verbal contact between referring provider and consultant to expedite referral. Based on our previous work,8 we started with a list of diagnostic clues a priori but further developed it as we gathered new information. To evaluate the quantity of information provided to the consultant, we documented the number of diagnostic clues provided in the referral request.
Outcome: We recorded whether an appointment for colonoscopy was generated subsequent to the referral, and if so, the date colonoscopy was performed and any patient non-adherence (no show, cancellation).
Data Analysis
Our primary outcome was the median number of days between first colonoscopy referral and colonoscopy performance. A VA directive recommends a colonoscopy completion time of 60 days after a positive FOBT.15 Therefore, we also analyzed wait times as a binary variable (≤ 60 days or > 60 days from referral to colonoscopy). We used several methods to determine the relationship of referral characteristics to lag time. We used chi-square tests for categorical variables, Fisher’s exact test when the assumptions for chi-square were not met, and non-parametric quantile regression for models with median wait time as the outcome. Quantile regression is used when parametric assumptions cannot be met and is a more robust analogue of least-squares regression under conditions of non-normality and heterogenous variability.16,17 Quantile regression models the relation between a set of independent variables and specific percentiles or quantiles of the outcome variable. Because the distribution of wait times was highly skewed, we used a median (a quantile describing the central location of the distribution) regression model to specify the changes in median wait times as a function of the predictor variables.
Predictor variables included the frequency of diagnostic clues (symptoms, signs, test results), referral origin (inpatient or outpatient), marking of urgency (< 7 days, < 30 days, next available, or routine), the specialty of the requesting provider (primary care vs. subspecialist) and documented evidence of verbal contact between referring provider and consulting services to expedite referral. We also tested patient demographics (age, gender, race) and clinical factors (e.g., comorbid medical or psychiatric disorder) as predictors of wait time. Potential predictor variables were examined in an unadjusted model and those with P<0.1 were included in a multivariate model. Only covariates with significant (P<0.1) as well as stable risk estimates were kept in the final model. Data were analyzed using SAS software (SAS Institute Inc., Cary, NC, version 9.1.3).
RESULTS
Between June 2001 and June 2007, 367 patients with CRC fulfilled selection criteria and had electronic referral requests for colonoscopy/sigmoidoscopy prior to CRC diagnosis. The median wait time between referral and colonoscopy performance was 57 days. Almost half (48.5%) of patients had wait times > 60 days.
Table 1 shows the distribution of median wait times by patient characteristics. Patients with congestive heart failure, coronary artery disease, and diabetes had significantly longer median wait times to colonoscopy than patients without these disorders (P values ≤ .02). Patients with depression and posttraumatic stress disorder also had significantly greater wait times (P=0.006 and P=0.04, respectively). Demographic variables were not associated with differences in median wait times. Demographic and health characteristics were similar at the beginning and end of the study period, with the exception that hypertension was more prevalent in 2007 (77.8%) than in 2001 (54.3%) P=.02. However, when we collapsed medical and psychiatric conditions across subcategories, we found that the presence of any psychiatric condition was more frequent in 2001 (P=.09).
Table 1.
Distribution of median wait times between referral and performance of colonoscopy for several patient characteristics; results of univariate analyses. Data shown for 367 patients diagnosed with colorectal cancer in one tertiary center from Jun 2001 to Jun 2007.
| N (%) | Median time | Quantile Regression | ||||
|---|---|---|---|---|---|---|
| Coefficient | Std error | T value | P-value | |||
| Age | ||||||
| <65 | 143 (39.0) | 50.0 | referent | |||
| 65–74 | 108 (29.4) | 63.0 | 13.0000 | 16.3631 | 0.79 | 0.43 |
| >75 | 116 (31.6) | 57.0 | 7.0000 | 16.0384 | 0.44 | 0.66 |
| Race | ||||||
| White Caucasian | 187 (57.0) | 57.0 | referent | |||
| Black | 112 (34.2) | 45.0 | −19.3445 | 14.5651 | −1.33 | 0.18 |
| Hispanic, other | 29 (8.8) | 61.0 | −3.7262 | 24.8619 | −0.15 | 0.88 |
| Gender | ||||||
| Male | 364 (99.2) | 56.5 | −9.2321 | 76.6343 | −0.12 | 0.90 |
| Female | 3 (0.8) | 66.0 | referent | |||
| Medical disorders | ||||||
| Congestive heart failure | 29 (7.9) | 114.0 | 58.0000 | 24.5427 | 2.36 | 0.02 |
| Coronary artery disease | 83 (22.6) | 88.0 | 36.0000 | 15.7661 | 2.28 | 0.02 |
| Hypertension | 244 (66.5) | 64.5 | 23.0620 | 14.6306 | 1.58 | 0.12 |
| Diabetes | 99 (27.0) | 88.0 | 36.0000 | 14.2310 | 2.53 | 0.01 |
| Chronic obstructive pulmonary disease | 47 (12.8) | 70.0 | 18.0000 | 21.2238 | 0.85 | 0.40 |
| Any medical condition | 281 (76.6) | 193.0 | 28.0000 | 16.2706 | 1.72 | 0.09 |
| Psychiatric disorders | ||||||
| Depression | 47 (12.8) | 108.0 | 55.1083 | 20.0249 | 2.75 | 0.006 |
| Anxiety | 17 (4.6) | 118.0 | 62.0000 | 33.2869 | 1.86 | 0.06 |
| Dementia | 10 (2.7) | 21.5 | −24.8090 | 42.4349 | −0.58 | 0.56 |
| Posttraumatic stress disorder | 18 (4.9) | 115.0 | 67.0759 | 31.9511 | 2.10 | 0.04 |
| Schizophrenia | 3 (0.8) | 179.0 | 122.2794 | 75.5686 | 1.62 | 0.11 |
| Bipolar disorder | 5 (1.4) | 53.0 | −4.0000 | 59.5244 | −0.07 | 0.95 |
| Alcohol | 66 (18.0) | 53.5 | −2.5543 | 17.9672 | −0.14 | 0.89 |
| Any mental disorder | 120 (32.9) | 226.0 | 15.5027 | 14.8695 | 1.04 | 0.30 |
Table 2 shows median wait times for patients with diagnostic clues provided in the referral request and compares the proportions of diagnostic clues between patients with ≤ 60 and > 60 day wait times. Referrals with longer wait times contained positive FOBT, rectal bleeding, history of polyps, and requests for “screening” in the presence of other diagnostic clues.
Table 2.
Waiting times between referral to and performance of colonoscopy presented for several diagnostic clues. Data for 367 patients diagnosed with colorectal cancer in one tertiary care center from Jun 2001 to Jun 2007
| All Patients (n=367) |
Wait > 60 days (n=178) |
Wait ≤60 days (n=189) |
P-value | ||
|---|---|---|---|---|---|
| Clues (n=634) | Median wait in days |
n (%) | |||
| Iron deficiency anemia (n=47) | 14.0 | 14 (4.6) | 33 (9.9) | 0.01 | |
| FOBT positive (n=150) | 92.0 | 95 (31.5) | 55 (16.6) | <.0001 | |
| Abnormal CT scan (n=20) | 4.0 | 2 (0.7) | 18 (5.4) | 0.0006 | |
| Suspected mass (n=11) | 10.0 | 1 (0.3) | 10 (3.0) | 0.01 | |
| Hematochezia (n=100) | 75.0 | 58 (19.2) | 42 (12.7) | 0.02 | |
| Constipation (n=14) | 36.5 | 5 (1.7) | 9 (2.7) | 0.37 | |
| Abdominal pain (n=14) | 4.0 | 1 (0.3) | 13 (3.9) | 0.002 | |
| Weight loss (n=15) | 31.0 | 4 (1.3) | 11 (3.3) | 0.10 | |
| Melena (n=12) | 26.0 | 4 (1.3) | 8 (2.4) | 0.32 | |
| History of polyps (n=26) | 221.0 | 21 (7.0) | 5 (1.5) | 0.0006 | |
| Obstruction (n=22) | 0.0 | 1 (0.3) | 21 (6.3) | <.0001 | |
| Other lower GI symptoms (n=24) | 47.0 | 10 (3.3) | 14 (4.2) | 0.55 | |
| Flex sigmoidoscopy positive (n=12) | 43.5 | 5 (1.7) | 7 (2.1) | 0.68 | |
| Barium enema positive (n=24) | 16.5 | 6 (2.0) | 18 (5.4) | 0.02 | |
| Colon cancer screening (n=23) | 203.0 | 18 (6.0) | 5 (1.5) | 0.003 | |
| Anemia (n=59) | 69.0 | 32 (10.6) | 27 (8.1) | 0.29 | |
| Ileocolitis/fissure/Crohn’s disease (n=3) |
2.0 | 0 (0.0) | 3 (0.9) | 0.25 | |
| Surgical Indications (ano-rectal stricture, diverticulitis/abscess etc.) (n=33) |
114.0 | 19 (6.3) | 14 (4.2) | 0.24 | |
Table 3 shows univariate associations between referral request characteristics and wait time to colonoscopy. Referrals that originated in the inpatient setting were associated with shorter wait times than outpatient referrals. Approximately half of referrals were marked as “routine”; all others were associated with shorter wait times, particularly those marked as needed in less than 1 week. In approximately 12% of outpatient referrals, providers documented additional verbal contact with the gastroenterology service, and these requests were also associated with shorter wait times. Referrals followed by one or more episodes of patient non-adherence were associated with the longest median wait time.
Table 3.
Association between referral request characteristics and time to colonoscopy using univariate quantile regression for all patients (n=367) diagnosed with colorectal cancer in one tertiary care center from Jun 2001 to Jun 2007
| Independent Variable | n (%) | Median time | |||
|---|---|---|---|---|---|
| days | Coefficient | Std error | P-value | ||
| Model 1 | |||||
| Provisional diagnosis (clue codes) | |||||
| 1clue | 166 (45.2) | 54.5 | referent | ||
| 2 clues | 145 (39.5) | 83.0 | 28.8448 | 12.1326 | 0.02 |
| 3 clues | 46 (12.5) | 36.5 | −15.2789 | 17.7847 | 0.39 |
| 4+ clues | 10 (2.7) | 4.0 | −50.1552 | 34.7546 | 0.15 |
| Model 2 | |||||
| Inpatient | |||||
| Yes | 84 (22.9) | 2.0 | referent | <.0001 | |
| No | 283 (77.1) | 84.0 | 82.0000 | 5.4216 | |
| Model 3 | |||||
| Urgency marked | |||||
| Routine | 184 (50.1) | 107.5 | referent | ||
| Next available | 16 (4.4) | 84.0 | −18.8797 | 9.7942 | 0.05 |
| < 30 days | 44 (12.0) | 69.0 | −37.7064 | 6.3060 | <.0001 |
| < 1 week | 123 (33.5) | 3.0 | −104.471 | 4.3765 | <.0001 |
| Model 4 | |||||
| Specialty of provider | |||||
| Primary care | 277 (75.5) | 70.0 | referent | ||
| Non primary care | 90 (24.5) | 14.0 | −56.0000 | 13.3429 | <.0001 |
| Model 5 | |||||
| Non-electronic contact | |||||
| Inpatient contact | 84 (22.9) | 2.0 | −97.0000 | 5.3366 | <.0001 |
| Outpatient contact | 42 (11.4) | 20.0 | −75.8811 | 7.0426 | <.0001 |
| No contact | 241 (65.7) | 99.0 | referent | ||
| Model 6 | |||||
| Patient adherent to 1st referral | |||||
| Yes | 313 (85.3) | 41.0 | referent | <.0001 | |
| No | 53 (14.4) | 308.0 | 267.0000 | 15.5598 | |
Table 4 shows results from the final multivariable quantile regression model. The following variables were significant independent predictors of shorter wait times: referrals with 3 clues, inpatient referrals, referrals with urgency marked for <1 week or <30 days, referrals marked “next available,” and outpatient referrals in which verbal discussion with a consultant was documented. A gradient effect for the number of clues may not be evident due to sample size limitations, as the majority of referrals documented 1 or 2 clues. Only 46 referrals had 3 documented clues, and 10 referrals had 4 or more clues.
Table 4.
Potential predictors of wait times between referral and performance of colonoscopy in 367 patients diagnosed with colorectal cancer during Jun 2001 to Jun 2007: results of multivariable quantile regression.
| Independent Variable | N (%) | Median time | Coefficient | Std error | P-value |
|---|---|---|---|---|---|
| Number of Clues | |||||
| 1 clue | 166 (45.2) | 54.5 | referent | ||
| 2 clues | 145 (39.5) | 83.0 | 1.0000 | 3.3057 | 0.76 |
| 3 clues | 46(12.5) | 36.5 | −21.0000 | 4.8109 | <.0001 |
| 4+ clues | 10 (2.7) | 4.0 | 0.0000 | 9.4250 | 1.00 |
| Inpatient | |||||
| Yes | 84 (22.9) | 2.0 | referent | ||
| No | 283 (77.1) | 84.0 | 55.6704 | 6.5823 | <.0001 |
| Urgency Marked | |||||
| Routine | 184 (50.1) | 107.5 | referent | ||
| Next available | 16 (4.4) | 84.0 | −32.4893 | 7.4358 | <.0001 |
| < 30 days | 44 (12.0) | 69.0 | −37.0555 | 4.8338 | <.0001 |
| < 1 week | 123 (33.5) | 3.0 | −21.0000 | 5.5868 | 0.0002 |
| Specialty of Provider | |||||
| Primary care | 277 (75.5) | 70.0 | referent | ||
| Non primary care | 90 (24.5) | 14.0 | −1.0000 | 3.8892 | 0.80 |
| Non-electronic (verbal) contact | |||||
| Inpatient referrals (always require additional verbal contact) |
84 (22.9) | 2.0 | −760.000 | 17.7711 | <.0001 |
| Outpatient verbal contact | 42 (11.4) | 20.0 | −60.0000 | 5.8490 | <.0001 |
| No contact | 241 (65.7) | 99.0 | referent | ||
| Patient adherent to 1st referral | |||||
| Yes | 313 (85.3) | 41.0 | referent | ||
| No | 53 (14.4) | 308.0 | 231.0000 | 4.3617 | <.0001 |
DISCUSSION
We evaluated referrals for 367 patients diagnosed with CRC over a 6-year period to determine if the timeliness of diagnostic colonoscopy was associated with the quality and quantity of information transmitted via the CPOE-generated referral request. Our findings suggest that in a system with limited endoscopic capacity, both quality and quantity of information transmitted to the consultant affected the wait time between referral and colonoscopy. Shorter wait times were associated with referral requests that documented three diagnostic clues versus one clue, originated in the inpatient setting, were marked as urgent or next available (versus routine), and documented a verbal discussion with a consultant. Clues such as iron deficiency anemia, abnormal CT scan or barium enema, suspected mass on physical examination, abdominal pain, and obstruction were significantly associated with wait times of <60 days. Conversely, other clues such as positive FOBT, hematochezia, and history of polyps were associated with >60 day wait times. Longer wait times were also more likely for referrals that requested colonoscopy for “screening” despite the presence of other diagnostic clues.
The use of CPOE-generated referrals has potential for overcoming several types of communication failures between the PCP and specialist. Breakdowns in referral communication due to inadequate or absent information transmission have been previously described in health care systems without CPOE-generated referral requests.10,18–20 In one study from Brigham and Women's Hospital in Boston prior to use of computerized referral requests, almost 68% of specialists reported not receiving any information from the PCP prior to the referral visit.18 Other studies have described communication breakdowns where the consultant and the PCP do not agree for the reason for referral.21 An added benefit of using CPOE is provision of templates or checkboxes to the referring physician when requesting a colonoscopy. This information can potentially be used to generate a likelihood score for CRC from an evidence-based algorithm, which can rationally inform colonoscopy scheduling.
We found that several diagnostic clues were associated with shorter wait times to diagnostic colonoscopy, suggesting the presence of some prioritization mechanism to schedule procedures. However, seemingly logical prioritization strategies may not be supported by current evidence. For example, a recent meta-analysis concluded that most “alarm” features such as anemia, change in bowel habits, and weight loss have poor sensitivity and specificity for the diagnosis of CRC.22 Shorter wait times for referrals documenting obstruction and abdominal pain occurred because the majority (74.3%) of these were emergent inpatient referrals. Additionally, clues suggesting the presence of a tumor, such as abnormal imaging or mass, were associated with short wait times. Contrary to what we expected, clues that signified bleeding, such as positive FOBT and hematochezia, were associated with a greater than 60 day wait time.
Consistent with previous literature, we found patient non-adherence to play a significant role in timeliness of diagnostic colonoscopy procedures.3,23,24 Our findings underscore the need for future efforts to improve adherence to diagnostic colonoscopies. This is especially important in systems with constrained endoscopic capacity, where there may be lengthy delays before procedures can be rescheduled. Most of the work on improving patient adherence is mostly focused on screening colonoscopy25,26 and could potentially be applied to diagnostic procedures, where the yield of the procedure is expected to be higher.
Our findings suggest that timeliness may relate to “how you ask” through CPOE.27 For instance, we observed longer wait times when providers inappropriately listed “screening” as the reason for the diagnostic colonoscopy despite the presence of other diagnostic clues in the patient’s record. Similarly, using an unqualified diagnosis of “anemia” was associated with a longer lag time than when “iron deficiency anemia” was used. Consultants may find it cumbersome to perform additional chart reviews to look for clues other than those provided in the referral request. Thus, effective electronic communication using CPOE requires providers to receive proper training on how best to use referral templates. Obligatory fields in referral templates may also help but do not guarantee the accuracy of information. Work on use and acceptability of templates for gastroenterology referrals at this institution is ongoing. Future research, preferably using prospective studies, is also needed to confirm our findings in other health care systems that use CPOE.
According to a recent Cochrane review, interventions to improve outpatient referrals from primary care to secondary care are needed, and only a limited number of rigorous evaluations exist to inform policy.28 To our knowledge, this is the first study that evaluates how characteristics of CPOE-generated referral content affect the timeliness of referral completion. Our study involved several satellite clinics, a large study sample, and a large number of referring providers. Providers in the VA are trained and well versed with CPOE, which has been used in most VA facilities since before 2002.
Our study had several limitations. The study population included only patients who were eventually diagnosed with CRC. Therefore, the findings may not apply to the vast majority of requests for colonoscopy in which CRC is not found, and any selection bias resulting from our methods is difficult to detect. Additionally, the study population (predominantly male veterans), and the VA setting may make our findings less generalizable to other practices, especially those that do not use electronic referrals. We also did not collect data on clinical outcomes related to delays in CRC diagnosis. Previous studies of the association between diagnostic delays and CRC outcomes have yielded conflicting results.29–31 Although the precise definition of a meaningful delay is unclear, delays in care are relevant facets of patient safety and satisfaction.
In conclusion, we found several referral characteristics were associated with lag times for diagnostic colonoscopy in CRC patients, including the type as well as frequency of diagnostic clues provided to the consultants (more than one clue is better than one or no clues), flagging of urgency, and documenting verbal discussions with consultants to expedite referrals. In systems with limited endoscopic capacity, attention to these aspects of diagnostic information transmitted through CPOE based referrals may help reduce delays in CRC diagnosis.
Acknowledgments
Funding Source
The study was supported by an NIH K23 career development award (K23CA125585) to Dr. Singh, the VA National Center of Patient Safety, and in part by the Houston VA HSR&D Center of Excellence (HFP90-020). These sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Data
All authors had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Conflicts of Interest
None
Licence for Publication:
The Corresponding Author has the right to grant on behalf of all authors and does grant on behalf of all authors, an exclusive licence (or non exclusive for government employees) on a worldwide basis to the BMJ Publishing Group Ltd to permit this article (if accepted) to be published in QSHC and any other BMJPGL products and sublicences such use and exploit all subsidiary rights, as set out in our licence. (http://qshc.bmj.com/ifora/licence.pdf)
Reference List
- 1.Gandhi TK, Kachalia A, Thomas EJ, et al. Missed and delayed diagnoses in the ambulatory setting: A study of closed malpractice claims. Ann Intern Med. 2006;145:488–496. doi: 10.7326/0003-4819-145-7-200610030-00006. [DOI] [PubMed] [Google Scholar]
- 2.Phillips RL, Jr, Bartholomew LA, Dovey SM, Fryer GE, Jr, Miyoshi TJ, Green LA. Learning from malpractice claims about negligent, adverse events in primary care in the United States. Qual Saf Health Care. 2004;13:121–126. doi: 10.1136/qshc.2003.008029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fisher DA, Jeffreys A, Coffman CJ, Fasanella K. Barriers to full colon evaluation for a positive fecal occult blood test. Cancer Epidemiol Biomarkers Prev. 2006;15:1232–1235. doi: 10.1158/1055-9965.EPI-05-0916. [DOI] [PubMed] [Google Scholar]
- 4.Yabroff K, Washington KS, Leader A, Neilson E, Mandelblatt J. Is the Promise of Cancer-Screening Programs Being Compromised? Quality of Follow-Up Care after Abnormal Screening Results. Med Care Res Rev. 2003;60:294–331. doi: 10.1177/1077558703254698. [DOI] [PubMed] [Google Scholar]
- 5.Freeman HP, Muth BJ, Kerner JF. Expanding access to cancer screening and clinical follow-up among the medically underserved. Cancer Pract. 1995;3:19–30. [PubMed] [Google Scholar]
- 6.Young CJ, Sweeney JL, Hunter A. Implications of delayed diagnosis in colorectal cancer. Aust N Z J Surg. 2000;70:635–638. doi: 10.1046/j.1440-1622.2000.01916.x. [DOI] [PubMed] [Google Scholar]
- 7.Singh H, Sethi S, Raber M, Petersen LA. Errors in cancer diagnosis: current understanding and future directions. J Clin Oncol. 2007;25:5009–5018. doi: 10.1200/JCO.2007.13.2142. [DOI] [PubMed] [Google Scholar]
- 8.Singh H, Daci K, Petersen LA, et al. Missed opportunities to initiate endoscopic evaluation for colorectal cancer diagnosis. Am J Gastroenterol. 2009 doi: 10.1038/ajg.2009.324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wattacheril J, Kramer JR, Richardson P, et al. Lagtimes in diagnosis and treatment colorectal cancer: determinants and association with cancer stage and survival. Aliment Pharmacol Ther. 2008 doi: 10.1111/j.1365-2036.2008.03826.x. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jiwa M, Mathers N, Walters S. Quality of information on referrals to colorectal surgeons: towards consensus. Curr Med Res Opin. 2002;18:72–77. doi: 10.1185/030079902125000309. [DOI] [PubMed] [Google Scholar]
- 11.Jumah KB, Gordon-Harris L, Agahowa JI. Common faults in filling of radiological request forms. East Afr Med J. 1995;72:744–745. [PubMed] [Google Scholar]
- 12.Jenkins RM. Quality of general practitioner referrals to outpatient departments: assessment by specialists and a general practitioner. Br J Gen Pract. 1993;43:111–113. [PMC free article] [PubMed] [Google Scholar]
- 13.Singh H, Kadiyala H, Bhagwath G, et al. Using a multifaceted approach to improve the follow-up of positive fecal occult blood test results. Am J Gastroenterol. 2009;104:942–952. doi: 10.1038/ajg.2009.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.El-Serag HB, Petersen L, Hampel H, Richardson P, Cooper G. The Use of Screening Colonoscopy for Patients Cared for by the Department of Veterans Affairs. Arch Intern Med. 2006;166:2202–2208. doi: 10.1001/archinte.166.20.2202. [DOI] [PubMed] [Google Scholar]
- 15.VHA Directive 2007-004: Colorectal Cancer Screening. Department of Veterans Affairs and Veterans Health Administration. 2007 Dec 1; Ref Type: Report. [Google Scholar]
- 16.Koenker R. Quantile Regression. Cambridge: Cambridge University Press; 2005. [Google Scholar]
- 17.Hao L, Naiman DQ. Quantile Regression. Thousand Oaks, Ca: Sage Publications; 2007. [Google Scholar]
- 18.Gandhi TK, Sittig DF, Franklin M, Sussman AJ, Fairchild DG, Bates DW. Communication breakdown in the outpatient referral process. J Gen Intern Med. 2000;15:626–631. doi: 10.1046/j.1525-1497.2000.91119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stille CJ, McLaughlin TJ, Primack WA, Mazor KM, Wasserman RC. Determinants and Impact of Generalist-Specialist Communication About Pediatric Outpatient Referrals. Pediatrics. 2006;118:1341–1349. doi: 10.1542/peds.2005-3010. [DOI] [PubMed] [Google Scholar]
- 20.Stille CJ, Primack WA, Savageau JA. Generalist-Subspecialist Communication for Children With Chronic Conditions: A Regional Physician Survey. Pediatrics. 2003;112:1314–1320. doi: 10.1542/peds.112.6.1314. [DOI] [PubMed] [Google Scholar]
- 21.Lee T, Pappius EM, Goldman L. Impact of inter-physician communication on the effectiveness of medical consultations. Am J Med. 1983;74:106–112. doi: 10.1016/0002-9343(83)91126-9. [DOI] [PubMed] [Google Scholar]
- 22.Ford AC, Veldhuyzen van Zanten SJO, Rodgers CC, Talley NJ, Vakil N, Moayyedi P. Diagnostic Utility of Alarm Features for Colorectal Cancer: Systematic Review and Meta-analysis. Gut. 2008;57:1545–1553. doi: 10.1136/gut.2008.159723. [DOI] [PubMed] [Google Scholar]
- 23.Zheng YF, Saito T, Takahashi M, Ishibashi T, Kai I. Factors associated with intentions to adhere to colorectal cancer screening follow-up exams. BMC Public Health. 2006;6:272. doi: 10.1186/1471-2458-6-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Denberg TD, Melhado TV, Coombes JM, et al. Predictors of nonadherence to screening colonoscopy. J Gen Intern Med. 2005;20:989–995. doi: 10.1111/j.1525-1497.2005.00164.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Coombes JM, Steiner JF, Bekelman DB, Prochazka AV, Denberg TD. Clinical outcomes associated with attempts to educate patients about lower endoscopy: a narrative review. J Community Health. 2008;33:149–157. doi: 10.1007/s10900-007-9081-5. [DOI] [PubMed] [Google Scholar]
- 26.Denberg TD, Coombes JM, Byers TE, et al. Effect of a mailed brochure on appointment-keeping for screening colonoscopy: a randomized trial. Ann Intern Med. 2006;145:895–900. doi: 10.7326/0003-4819-145-12-200612190-00006. [DOI] [PubMed] [Google Scholar]
- 27.Goldman L, Lee T, Rudd P. Ten commandments for effective consultations. Arch Intern Med. 1983;143:1753–1755. [PubMed] [Google Scholar]
- 28.Akbari A, Mayhew A, Al-Alawi MA, et al. Interventions to improve outpatient referrals from primary care to secondary care. Cochrane Database Syst Rev. 2008 doi: 10.1002/14651858.CD005471.pub2. CD005471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gonzalez-Hermoso F, Perez-Palma J, Marchena-Gomez J, Lorenzo-Rocha N, Medina-Arana V. Can Early Diagnosis of Symptomatic Colorectal Cancer Improve the Prognosis? World Journal of Surgery. 2004;28:716–720. doi: 10.1007/s00268-004-7232-8. [DOI] [PubMed] [Google Scholar]
- 30.Korsgaard M, Pedersen L, Sorensen HT, Laurberg S. Delay of treatment is associated with advanced stage of rectal cancer but not of colon cancer. Cancer Detect Prev. 2006;30:341–346. doi: 10.1016/j.cdp.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 31.Ramos M, Esteva M, Cabeza E, Campillo C, Llobera J, Aguilo A. Relationship of diagnostic and therapeutic delay with survival in colorectal cancer: a review. Eur J Cancer. 2007;43:2467–2478. doi: 10.1016/j.ejca.2007.08.023. [DOI] [PubMed] [Google Scholar]


