Abstract
BACKGROUND
Alcohol use disorders (AUD), i.e., alcohol dependence and abuse are major contributors to burden of disease. A large part of this burden is due to disability. However, there is still controversy about the best disability weighting for alcohol use disorders. The objective of this study was to provide an overview of alcohol-related disabilities.
METHODS
Systematic literature review and expert interviews.
RESULTS
There is heterogeneity in experts’ descriptions of disabilities related to AUD. The major core attributes of disability related to AUD are changes of emotional state, social relationships, memory and thinking. The most important supplementary attributes are anxiety, impairments of speech and hearing.
CONCLUSIONS
This review identified the main patterns of disability associated with alcohol use disorders. However, there was considerable variability, and data on less prominent patterns were fragmented. Further and systematic research is required for increasing the knowledge on disability related to alcohol use disorders and for application of interventions for reducing the associated burden.
OBJECTIVE
To provide an overview of disabilities associated with AUD.
Keywords: alcohol abuse, alcohol dependence, alcohol use disorders, disability, global burden of disease
INTRODUCTION
Alcohol use disorders (AUD) are a highly prevalent category of mental disorders with a global 12-month prevalence of 3.6% for adults up to 65 years of age; 6.3% among men and 0.9% among women (Rehm et al., 2009a; WHO 2008). The prevalence is even higher in high income countries such as the US. Based on the results of the US National Epidemiologic Survey on Alcohol and Related Conditions, the 12-month prevalence of AUD was 8.5% among all adults, 4.7% with alcohol abuse and 3.8% with alcohol dependence, with higher AUD prevalence among men (12.4%), Native Americans (12.1%) and young adults [16.2% in the age group 18–29; (Hasin et al., 2007)]. AUD have been associated with considerable burden of disease (WHO 2001). Technically, burden of disease is measured in disability-adjusted life years (DALYs), which are estimated as the sum of two components, years of life lost due to premature mortality and years of life lost due to disability (Murray and Lopez, 1996). As AUD are often non fatal, the disability component of DALYs is more important than that of the mortality for these disorders (Rehm et al., 2003; WHO 2008). To operationalize the level of disability, disability weights are used (Murray, 1996), which vary between 0 (perfect health = no disability at all) and 1 (death), and then combined with incidence and average duration (Murray and Lopez, 1996).
Disability weights are usually derived from valuations of short descriptions of the disease condition under consideration. These vignettes can be either unstructured and idiosyncratic for the disease condition (i.e., alcohol use dependence is a disease, which is characterized by loss of control of one drinking, tolerance, withdrawal, etc.) or through the use of the same set of attributes for each condition [see Table 2 below for one set of attributes widely used (McIntosh et al., 2007); for more background see (Langlois et al., in press; Rehm and Frick, 2010). The latter approach allows for the calculation of disability weights for any disease condition once the vector of attributes is known (McIntosh et al., 2007; Rehm and Frick, 2010).
TABLE 2.
COMPARISON OF DISABILITIES ATTRIBUTABLE TO ALCOHOL USE DISORDERS MADE BY EXPERTS AND BASED ON CLINICAL DESCRIPTIONS IN REVIEWED ARTICLES
Score 1 - no problem; Scores 4 or 5 - the highest levels of disability
We will use this approach here and describe alcohol abuse and dependence in terms of a standard set of attributes which can later be combined to derive disability weights.
MATERIAL AND METHODS
CLASSIFICATION OF DISABILITIES ATTRIBUTABLE TO ALCOHOL-USE DISORDERS
There are several definitions of disability (Üstün et al., 2001). For this contribution, we rely on the definition of disability from the International Classification of Functioning, Disability and Health (ICF) by the World Health Organization (available from http://www.who.int/classifications/icf/en/). As defined by the ICF, disability covers a spectrum of various levels of functioning at the body level, person level and societal level and includes impairments in body functions and structures, and limitations in activity and in participation (WHO 2001). This definition and its qualifiers are comprehensive, complementary to International Classification of Diseases (ICD) version 10, and relevant to clinical and public health needs. To operationalize the most important capacity limitations congruent with this general concept, we used the dimensions of the Classification and Measurement System of Functional Health (CLAMES) developed by Statistics Canada.
The CLAMES includes 6 core (pain or discomfort, physical functioning, emotional state, fatigue, memory and thinking, social relationships) and 5 supplementary attributes [anxiety, speech, hearing, vision, use of hands and fingers; cf. (McIntosh et al., 2007)]. Each attribute in CLAMES is scaled from 1 (no problem) to 4 or 5, the highest level of disability (Table 1).
TABLE 1.
LIST OF ATTRIBUTES TO CHARACTERIZE EACH HEALTH STATES BASED ON THE CLAMES SYSTEM (MCINTOSH ET AL., 2007)
| Attribute | Level | Description |
|---|---|---|
| Core Attributes | ||
| Pain or discomfort | 1 | Generally free of pain and discomfort |
| 2 | Mild pain or discomfort | |
| 3 | Moderate pain or discomfort | |
| 4 | Severe pain or discomfort | |
| Physical functioning | 1 | Generally no limitations in physical functioning |
| 2 | Mild limitations in physical functioning | |
| 3 | Moderate limitations in physical functioning | |
| 4 | Severe limitations in physical functioning | |
| Emotional state | 1 | Happy and interested in life |
| 2 | Somewhat happy | |
| 3 | Somewhat unhappy | |
| 4 | Very unhappy | |
| 5 | So unhappy that life is not worthwhile | |
| Fatigue | 1 | Generally no feelings of tiredness, no lack of energy |
| 2 | Sometimes feel tired and have little energy | |
| 3 | Most of the time feel tired and have little energy | |
| 4 | Always feel tired and have no energy | |
| Memory and thinking | 1 | Able to remember most things, think clearly and solve day-to-day problems |
| 2 | Able to remember most things but have some difficulty when trying to think and solve day-to-day problems | |
| 3 | Somewhat forgetful, but able to think clearly and solve day-to-day problems | |
| 4 | Very forgetful, and have great difficulty when trying to think or solve day-to-day problems | |
| Social relationships | 1 | No limitations in the capacity to sustain social relationships |
| 2 | Mild limitations in the capacity to sustain social relationships | |
| 3 | Moderate limitations in the capacity to sustain social relationships | |
| 4 | Severe limitations in the capacity to sustain social relationships | |
| 5 | No capacity or unable to relate to other people socially | |
| Supplementary attributes | ||
| Anxiety | 1 | Generally not anxious |
| 2 | Mild levels of anxiety experienced occasionally | |
| 3 | Moderate levels of anxiety experienced regularly | |
| 4 | Severe levels of anxiety experienced most of the time | |
| Speech | 1 | Able to be understood completely when speaking with strangers or friends |
| 2 | Able to be understood partially when speaking with strangers but able to be understood completely when speaking with people who know you well | |
| 3 | Able to be understood partially when speaking with strangers and people who know you well | |
| 4 | Unable to be understood when speaking to other people | |
| Hearing | 1 | Able to hear what is said in a group conversation, without a hearing aid, with at least 3 other people |
| 2 | Able to hear what is said in a conversation with 1 other person in a quiet room, with or without a hearing aid, but require a hearing aid to hear what is said in a group conversation with at least 3 other people | |
| 3 | Able to hear what is said in a conversation with 1 other person in a quiet room, with or without a hearing aid, but unable to hear what is said in a group conversation with at least 3 other people | |
| 4 | Unable to hear what others say, even with a hearing aid | |
| Vision | 1 | Able to see well enough, with or without glasses or contact lenses, to read ordinary newsprint and recognize a friend on the other side of the street |
| 2 | Unable to see well enough, even with glasses or contact lenses, to recognize a friend on the other side of the street but can see well enough to read ordinary print | |
| 3 | Unable to see well enough, even with glasses or contact lenses, to read ordinary newsprint or to recognize a friend on the other side of the street | |
| Use of hands and fingers | 1 | No limitations in the use of hands and fingers |
| 2 | Limitations in the use of hands and fingers but do not require special tools or the help of another person | |
| 3 | Limitations in the use of hands and fingers, independent with special tools and do not require the help of another person | |
| 4 | Limitations in the use of hands and fingers, require the help of another person for some tasks | |
| 5 | Limitations in the use of hands and fingers, require the help of another person for most tasks | |
Score 1 - no problem; Scores 4 or 5 - the highest levels of disability
Attributes and scales were taken from three leading general health status instruments: the Health Utilities Index Mark III [HUI3; (Feeny et al., 2002; Furlong et al., 2001)], the Medical Outcomes Study Short-Form 36 [SF-36; (Ware and Sherbourne, 1992)]; and the European Quality of Life Five-Dimensions Index Plus [EQ-5D; (Brooks and EuroQoL Group, 1996; EuroQoL Group, 1990; Rabin and de Charro, 2001)]. Further reasoning for the selection of the CLAMES can be found in (Rehm and Frick, 2010).
SYSTEMATIC LITERATURE SEARCH
A systematic literature search on alcohol-related disabilities was performed in multiple electronic bibliographic databases, including: Ovid MEDLINE, PubMed, EMBASE, Web of Science (including Science Citation Index, Social Sciences Citation Index, Arts and Humanities Citation Index), and PsycINFO, Google Scholar and the Cochrane Database of Systematic Reviews. The available published literature was searched from the earliest publications to March 2010 inclusive. The search was conducted using multiple combinations of the following key words: alcohol, use, abuse, dependence, alcoholism, disability, drinking, comorbid states, comorbidity, physical functioning, social relationships, pain, mood, emotional state, anxiety, depression, memory, thinking, cognitive functions, hearing, vision, speech, fine motor functions. In addition, manual reviews of the content pages of the major epidemiological journals and citations in any of the relevant articles were conducted. The search was not limited either geographically or to English language publications.
Inclusion criteria:
Article focused on disability associated with AUD as primary condition;
Article contained clear and generalized description of one or several core or supplementary attributes of disability included into CLAMES.
Exclusion criteria:
AUD were secondary to another disease condition (i.e., AUD secondary to depression or anxiety);
Information presented in the article referred to specific conditions subpopulation (e.g alcohol consumption increases hearing threshold in persons exposed to loud noise).
Information was not extractable or not compatible with CLAMES.
DATA EXTRACTION
Data were extracted using the clinical description of each rank of core and supplementary attributes of CLAMES. Extraction was performed independently by two medical doctors (AVS and SP). Training of coders to achieve sufficient (> 0.80) interrater reliability (IRR) was conducted. IRR, a statistical measure for the degree of agreement among raters that gives a score of how much homogeneity, or consensus there is in the ratings given by different raters, was calculated by Fleiss’ kappa statistics using attribute agreement analytic method. Discrepancies were reconciled by a third investigator (JR), independent of the first process. Incorporation of the data was possible only if all three reviewers were in agreement.
EXPERTS’ ESTIMATES
We supplemented the systematic literature review with data from expert interviews and other expert judgments. The first set of expert judgments were the CLAMES descriptions for AUD from Statistics Canada as part of the overall description of more than 300 health states (McIntosh et al., 2007). Secondly, as part of the US study on estimating alcohol-attributable burden of disease (contract # HHSN267200700041C “Alcohol- and Drug-Attributable Burden of Disease and Injury in the US” to the last author), 5 experts in total from NIAAA, CDC, Atlanta and CAMH classified alcohol dependence using the CLAMES system. In addition, we interviewed two addiction experts from the Institute of Neurology, Psychiatry and Narcology of Academy of Medical Sciences of Ukraine (Kharkiv, Ukraine). The latter experts were asked to fill in a table and provide scores based on their best knowledge for mild, moderate and severe alcohol abuse and dependence separately using CLAMES. Estimates given by the various experts were then compared and tabulated.
RESULTS
The electronic searches on alcohol-related disabilities studies yielded a total of 3,751 publications (Figure 1).
Figure 1.
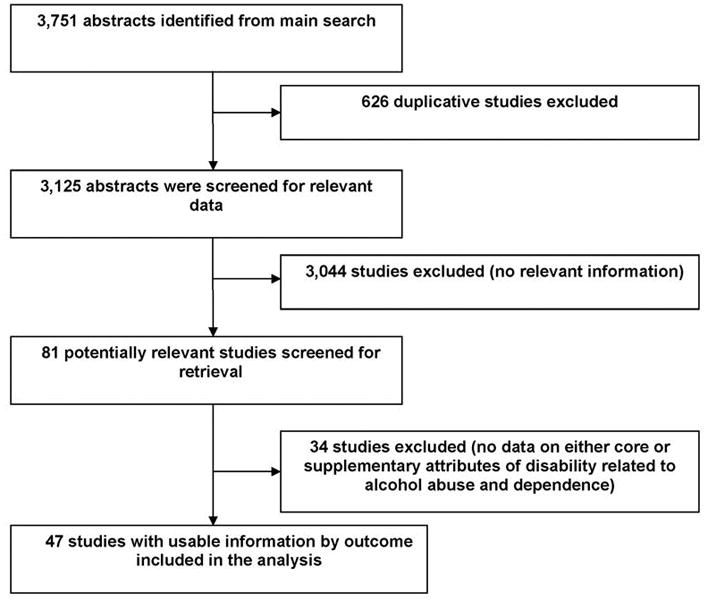
Flow diagram describing selection of studies for a systematic review on core and supplementary attributes of disability related to alcohol abuse and dependence
After 626 duplicate articles were removed, 3,125 were screened using titles and abstracts. Eighty one full-text articles were retrieved for further consideration. Cross-checking of references did not yield any additional studies for inclusion. In total, 47 studies met the inclusion criteria. There was a high IRR (kappa = 0.92; p<0.0001) among reviewers across all variables. Most of the studies (44) were in English, with the exception of single articles in French, one in Russian and one in Spanish. Studies were found from the following countries: USA (14), Germany (6), UK (4), Australia (3), Austria (3), Brazil (2), Switzerland (2), and other countries contributed single articles only.
In the systematic search, we did not find any single study which empirically described or quantified all aspects of disability related to AUD, although it should be noted that there is a chance of missing some studies that did not fall into our search algorithm. One major problem in the descriptions of disability associated with AUD concerned the high co-morbidity of AUD with other substance use and/or mental disorders (Üstün et al., 2001). In addition, AUD are associated with somatic disorders such as liver cirrhosis (Rehm et al., 2010a) or infectious diseases such as tuberculosis (Rehm et al., 2009b); see (Rehm et al., 2010a) an overview). It was not always clear from the literature reviewed whether the disabilities were associated with the AUD, or only with the co-morbid condition.
Core attributes
even though AUDs are typically associated with a number of comorbidities causing pain and discomfort, most of the reviewed articles were considered alcohol for its analgesic properties with the exception of a few studies that described mild to moderate pain and physical discomfort in alcohol abusers and addicts (Dooldeniya et al., 2007; Fink and Beck, 2005; Sheu et al., 2008). Pain and discomfort were closely related to another core disability attribute, physical functioning, in terms of results of our search – mild to moderate decrease of physical functioning were described (Burger et al., 2003; Johnson et al., 1995; Wells et al., 1990). A search for both attributes was complicated by involvement of comorbid conditions.
Emotional state, or especially depressive symptoms, as a consequence of AUD was extensively described in scientific literature. After exclusion of AUD secondary to depression and other emotional conditions several studies describing predominantly moderate levels of depression in alcohol users and moderate-to-severe levels in alcohol addicts were found (Conner et al., 2009; Fergusson et al., 2009; Hasin and Grant 2002; Manninen et al., 2006; Olgiati et al., 2007; Rupp et al., 2008; Saatcioglu et al., 2008; Uekermann et al., 2003). We were able to locate three articles on higher fatigue levels corresponding to blood alcohol concentration levels (Dawson and Reid, 1997; Maruff et al., 2005; Williamson et al., 2001). Problems in cognitive functioning in AUD were described in multiple studies covering various AUD-related conditions, including intoxication, hangovers, withdrawal states and Korsakoff’s syndrome (Chelune and Parker, 1981; Farr et al., 2005; Kopelman et al., 2009; Labudda et al., 2008; Liraud et al., 1999; Loeber et al., 2009; McKinney and Coyle, 2004; Postma et al., 2006; Rupp et al., 2004; Rupp et al., 2008; Seifert et al., 2003; Todor, 2007; Uekermann et al., 2003). We managed to find only one article clearly describing social functioning in alcohol-dependent individuals (Günther et al., 2007), albeit indicating high levels of disability on this dimension.
Supplementary attributes
Most of the studies found on anxiety and AUD considered AUD as a secondary or comorbid condition to anxiety disorders, though the attribute of anxiety was the best described of all supplementary attributes for both alcohol abuse and dependence in the literature (Allan, 1995; Blume et al., 2009; Halsband, 2004; Liappas et al., 2003; Olgiati et al., 2007; Saatcioglu et al., 2008; Todor, 2007). Despite the fact that speech impairments are traditionally associated with acute alcohol intoxication we were able to find only three studies describing specific speech impairments in AUD (Hollien et al., 2001; Pisoni and Martin, 1989; Pisoni et al., 1991). Chronic and excessive alcohol consumption were found to have some ototoxic effects in several studies (Bellé et al., 2007; Niedzielska et al., 2001; Ribeiro et al., 2007; Shore et al., 2006; Verma et al., 2006), though they were inconclusive. Also several experimental studies showed some visual impairment in alcohol abusers and addicts, namely, color vision impairment and deterioration of visuospatial perception (Kapitany et al., 1993; Mergler et al., 1988; Shore et al., 2006; Skripnichenko, 1987; Vanlith and Henkes, 1979). A search for description of disability related to use of hands and fingers in patients with AUD yielded three articles (De Wilde et al., 2007; Mangold et al., 1996; McKinney and Coyle 2004)
Table 2 compares the result of the literature review with the expert judgments. Despite the heterogeneity, the most important core attributes of disability related to alcohol abuse and dependence appeared to be changes of emotional state, social relationships, and memory and thinking. The most important supplementary attributes of disability associated with AUD were anxiety and impairments of speech and hearing.
DISCUSSION
Overall, given the high prevalence of AUD and their importance for public health, especially in developed countries, it is surprising that relatively few studies have looked at associated disability. In the studies systematically reviewed we find a surprising level of heterogeneity regarding both patterns and levels of disability. Additionally, the heterogeneity within the experts’ opinions, as well as between their estimations and the clinical descriptions presented in reviewed publications, makes information fragmented and hardly comparable.
The diversity in results and views is in part due to differing perspectives. The clinical perspective tends to be formed from the very severe and often quite disabled cases that are treated in specialist services for alcohol dependence or comorbid problems including dependence. These cases are often socially marginalized – not in the workforce, not in an intact family, and in trouble with the police, as well as disabled with comorbid physical or mental illness. While a substantial proportion in many general populations drink enough to qualify for an alcoholic dependence diagnosis or to have adverse effects on their health, these more socially integrated persons with AUD will present a starkly different picture from the clinical populations – a difference that has been described in terms of “the two worlds of alcohol problems” (Room, 1977; Storbjörk and Room, 2008). Disability weights derived from clinical samples thus cannot validly be applied to the whole of the group qualifying for AUDs in psychiatric epidemiological surveys of the general population. The disability associated with AUD is also likely to vary between cultures according not only to variations in patterns of very heavy drinking but also to variations in the social response to and derogation of AUD (Room et al., 2001).
There is also the problem of proper clinical description of alcohol abuse and dependence and related disabilities. Due to the sporadic and unpredictable clinical course of alcohol abuse and dependence we can describe several potential states and several degrees of severity within the course of these disorders. This is one of the major problems in disability scoring for alcohol abuse and dependence – unlike the pattern for most somatic diseases, the symptoms of alcohol abuse and dependence vary significantly depending on the functional state of individual, e.g., intoxication and withdrawal will have markedly different scores of disability, and an alcohol dependence case with intermittent drinking bouts may show little disability between bouts. This makes it difficult to integrate disability of AUD over time. One solution would be to differentiate by and measure the number of intoxications and add up the resulting disabilities, assuming no disabilities are present during the sober times. This is an approach which falls outside the usual assumptions both of the disability field, which tends to think in terms of lasting rather than transient attributes, and of psychiatric thinking, which focuses on presumed underlying conditions rather than transitory states. It is presumably these habits of thought which explain, for instance, the lack of discussion of speech impairments in connection with AUDs in the literature. It would be interesting to conduct a study of the hour-to-hour disablement of chronic heavy drinkers (Bruun, 1969 was a pioneer study with a methodology adaptable for this purpose), while measuring separately any longer-lasting disabilities which are not attributable to diseases which are consequences of heavy drinking. Such a model in terms of cumulative intoxication disability-hours probably could be realistic for the disabilities of AUD in late adolescents and early adulthood, which as mentioned are prominent in those identified with AUDs in population surveys, though it might not capture the disabilities of the above described clinical cases with AUD in later adulthood.
Another way would be to separate two or more severity levels of AUD with different vectors of disability attributes. This could be done by separating people with AUD into those attending vs. those not attending treatment, and the resulting estimate of severe AUD in the US would then be around 10%–15% (Cohen et al., 2007; Hasin et al., 2007). Given different treatment systems in other countries (Klingemann et al., 1992), the proportions of people with severe AUD could vary considerably around the world. Two additional problems of disability estimation concern the strong pathogenic link between alcohol and attributable disorders such as liver cirrhosis or cancer (Rehm et al., 2010b) and the psychiatric comorbidity associated with AUD (Kessler, 2004). It has been shown that the majority of DALYs associated with alcohol are not related to AUD [Table 3 in (Room et al., 2005)] and a notable/serious(used majority just before) problem of the Global Burden of Disease estimates is the exclusion of the disability of comorbid states (Mathers et al., 2006), e.g. AUD and other mental disorders. As alcohol has a causal impact on more disease and injury conditions than any other risk factor (Ezzati et al., 2004), and there is a high comorbidity between AUD and other mental conditions (Kessler, 2004), the challenges for estimating disability of AUD are immense. It is thus no surprise, that the disability profiles given by experts and in the literature vary, as their judgments may be based on different assumptions.
CONCLUSIONS
This review identified the main patterns of disability associated with AUD. However, there was considerable variability, and data on less prominent disablements were fragmented. Further and systematic qualitative as well as quantitative research is required for increasing the knowledge on disability related to alcohol use disorders and for application of interventions for reducing the associated burden.
Acknowledgments
NIAAA (contract # HHSN267200700041C “Alcohol- and Drug-Attributable Burden of Disease and Injury in the US” to the last author), and the Global Burden of Disease and Injury 2005 Project provided financial and/or technical support for this study. With regard to the contributions by Dr. Rehm, support to Centre for Addiction and Mental Health for salary of scientists and infrastructure has been provided by the Ontario Ministry of Health and Long Term Care. The views expressed in this paper do not necessarily reflect those of the Ministry of Health and Long Term Care or other funders. We would like to thank Fotis Kanteres for helpful comments on earlier versions of the manuscript.
Reference List
- Allan CA. Alcohol problems and anxiety disorders: A critical review. Alcohol Alcohol. 1995;30:145–151. [PubMed] [Google Scholar]
- Bellé M, Sartori SA, Rossi AG. Alcoholism: effects on the cochleo-vestibular apparatus. Braz J Otorhinolaryngol. 2007;73:110–116. doi: 10.1016/S1808-8694(15)31132-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blume AW, Resor MR, Villanueva MR, Braddy LD. Alcohol use and comorbid anxiety, traumatic stress, and hopelessness among Hispanics. Addict Behav. 2009;34:709–713. doi: 10.1016/j.addbeh.2009.03.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks R EuroQoL Group. EuroQoL: The current state of play. Health Policy. 1996;37:53–72. doi: 10.1016/0168-8510(96)00822-6. [DOI] [PubMed] [Google Scholar]
- Bruun K. The actual and registered frequency of drunkenness in Helsinki. Br J Addict. 1969;64:3–8. doi: 10.1111/j.1360-0443.1969.tb01103.x. [DOI] [PubMed] [Google Scholar]
- Burger M, Mensink GBM, Bergmann E, Pietrzik K. Characteristics associated with alcohol consumption in Germany. J Stud Alcohol. 2003;64:262–269. doi: 10.15288/jsa.2003.64.262. [DOI] [PubMed] [Google Scholar]
- Chelune GJ, Parker JB. Neuropsychological deficits associated with chronic alcohol abuse. Clinical Psychology Review. 1981;1:181–195. [Google Scholar]
- Cohen E, Feinn R, Arias A, Kranzler HR. Alcohol treatment utilization: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend. 2007;86:214–221. doi: 10.1016/j.drugalcdep.2006.06.008. [DOI] [PubMed] [Google Scholar]
- Conner KR, Pinquart M, Gamble SA. Meta-analysis of depression and substance use among individuals with alcohol use disorders. J Subst Abuse Treat. 2009;37:127–137. doi: 10.1016/j.jsat.2008.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson D, Reid K. Fatigue, alcohol and performance impairment. Nature. 1997;388:235. doi: 10.1038/40775. [DOI] [PubMed] [Google Scholar]
- De Wilde B, Dom G, Hulstijn W, Sabbe B. Motor functioning and alcohol dependence. Alcohol Clin Exp Res. 2007;31:1820–1825. doi: 10.1111/j.1530-0277.2007.00484.x. [DOI] [PubMed] [Google Scholar]
- Dooldeniya MD, Khafagy R, Mashaly H, Browning AJ, Sundaram SK, Biyani CS. Lower abdominal pain in women after binge drinking. BMJ. 2007;335:992–993. doi: 10.1136/bmj.39247.454005.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EuroQoL Group. EuroQoL - A new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- Ezzati M, Lopez A, Rodgers A, Murray CJL. Comparative quantification of health risks. Global and regional burden of disease attributable to selected major risk factors. Geneva, Switzerland: WHO; 2004. [Google Scholar]
- Farr SA, Scherrer JF, Banks WA, Flood JF, Morley JE. Chronic ethanol consumption impairs learning and memory after cessation of ethanol. Alcohol Clin Exp Res. 2005;29:971–982. doi: 10.1097/01.alc.0000171038.03371.56. [DOI] [PubMed] [Google Scholar]
- Feeny D, Furlong W, Torrance GW, Goldsmith CH, Zhu Z, DePauw S, Denton M, Boyle M. Multiattribute and single-attribute utility functions for the health utilities index mark 3 system. Med Care. 2002;40:113–128. doi: 10.1097/00005650-200202000-00006. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Boden JM, Horwood LJ. Tests of causal links between alcohol abuse or dependence and major depression. Arch Gen Psychiatry. 2009;66:260–266. doi: 10.1001/archgenpsychiatry.2008.543. [DOI] [PubMed] [Google Scholar]
- Fink A, Beck JC. The problem drinking pain paradox. Addiction. 2005;100:731–732. doi: 10.1111/j.1360-0443.2005.01115.x. [DOI] [PubMed] [Google Scholar]
- Furlong WJ, Feeny DH, Torrance GW, Barr RD. The Health Utilities Index (HUI) system for assessing health-related quality of life in clinical studies. Ann Med. 2001;33:375–384. doi: 10.3109/07853890109002092. [DOI] [PubMed] [Google Scholar]
- Günther O, Roick C, Angermeyer MC, König HH. The EQ-5D in alcohol dependent patients: relationships among health-related quality of life, psychopathology and social functioning. Drug Alcohol Depend. 2007;86:253–264. doi: 10.1016/j.drugalcdep.2006.07.001. [DOI] [PubMed] [Google Scholar]
- Halsband S. Ansiedad y alcoholismo. Vertex. 2004;15:16–20. [PubMed] [Google Scholar]
- Hasin DS, Grant BF. Major depression in 6050 former drinkers: association with past alcohol dependence. Arch Gen Psychiatry. 2002;59:794–800. doi: 10.1001/archpsyc.59.9.794. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Grant BF. Prevalence, correlates, disability and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Hollien H, De Jong G, Martin CA, Schwartz R, Lijegren K. Effects of ethanol intoxication on speech suprasegmentals. J Acoust Soc Am. 2001;110:3198–3206. doi: 10.1121/1.1413751. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Spitzer RL, Williams JB, Kroenke K, Linzer M, Brody D, deGruy F, Hahn S. Psychiatric comorbidity, health status, and functional impairment associated with alcohol abuse and dependence in primary care patients: findings of the PRIME MD-1000 study. J Consult Clin Psychol. 1995;63:133–140. doi: 10.1037//0022-006x.63.1.133. [DOI] [PubMed] [Google Scholar]
- Kapitany T, Dietzel M, Grunberger J, Frey R, Koppensteiner L, Schleifer G, Marx B. Color vision deficiencies in the course of acute alcohol withdrawal. Biol Psychiatry. 1993;33:415–422. doi: 10.1016/0006-3223(93)90169-e. [DOI] [PubMed] [Google Scholar]
- Kessler RC. The epidemiology of dual diagnosis. Biol Psychiatry. 2004;56:730–737. doi: 10.1016/j.biopsych.2004.06.034. [DOI] [PubMed] [Google Scholar]
- Klingemann H, Takala J-P, Hunt G. Cure, care, or control: alcoholism treatment in sixteen countries. Albany, NY: State University of New York Press; 1992. [Google Scholar]
- Kopelman MD, Thomson AD, Guerrini I, Marshall EJ. The Korsakoff Syndrome: Clinical Aspects, Psychology and Treatment. Alcohol Alcohol. 2009;44:148–154. doi: 10.1093/alcalc/agn118. [DOI] [PubMed] [Google Scholar]
- Labudda K, Todorovski S, Markowitsch HJ, Brand M. Judgment and memory performance for emotional stimuli in patients with alcoholic Korsakoff syndrome. J Clin Exp Neuropsychol. 2008;30:224–235. doi: 10.1080/13803390701363811. [DOI] [PubMed] [Google Scholar]
- Langlois KA, Samokhvalov AV, Rehm J, Spence ST, Gorber SK. Health state descriptions for Canadians: Mental illnesses. Ottawa, ON: Statistics Canada; (in press) [Google Scholar]
- Liappas J, Paparrigopoulos T, Tzavellas E, Christodoulou G. Alcohol detoxification and social anxiety symptoms: a preliminary study of the impact of mirtazapine administration. J Affect Disord. 2003;76:279–284. doi: 10.1016/s0165-0327(02)00094-0. [DOI] [PubMed] [Google Scholar]
- Liraud F, Lespinet V, N’Kaoua B, Fleury B, Claverie B. A multifactor analysis of the effects of chronic alcoholism on memory. Revue de neuropsychologie. 1999;9:61–82. [Google Scholar]
- Loeber S, Duka T, Welzel H, Nakovics H, Heinz A, Flor H, Mann K. Impairment of cognitive abilities and decision making after chronic use of alcohol: the impact of multiple detoxifications. Alcohol Alcohol. 2009;44:372–381. doi: 10.1093/alcalc/agp030. [DOI] [PubMed] [Google Scholar]
- Mangold S, Laeubli T, Krueger H. Effects of a low alcohol dose on static balance, fine motor activity, and mental performance. Neurotoxicol Teratol. 1996;18:547–554. doi: 10.1016/0892-0362(96)00063-3. [DOI] [PubMed] [Google Scholar]
- Manninen L, Poikolainen K, Vartiainen E, Laatikainen T. Heavy drinking occasions and depression. Alcohol Alcohol. 2006;41:293–299. doi: 10.1093/alcalc/agh246. [DOI] [PubMed] [Google Scholar]
- Maruff P, Falleti MG, Collie A, Darby D, McStephen M. Fatigue-related impairment in the speed, accuracy and variability of psychomotor performance: comparison with blood alcohol levels. J Sleep Res. 2005;14:21–27. doi: 10.1111/j.1365-2869.2004.00438.x. [DOI] [PubMed] [Google Scholar]
- Mathers CD, Iburg KM, Begg S. Adjusting for dependent comorbidity in the calculation of healthy life expectancy. Popul Health Metr. 2006;4:4. doi: 10.1186/1478-7954-4-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntosh CN, Connor Gorber S, Bernier J, Berthelot JM. Eliciting Canadian population preferences for health states using the Classification and Measurement System of Functional Health (CLAMES) Chronic Dis Can. 2007;28:29–41. [PubMed] [Google Scholar]
- McKinney A, Coyle K. Next day effects of a normal night’s drinking on memory and psychomotor performance. Alcohol Alcohol. 2004;39:509–513. doi: 10.1093/alcalc/agh099. [DOI] [PubMed] [Google Scholar]
- Mergler D, Blain L, Lemaire J, Lalande F. Colour vision impairment and alcohol consumption. Neurotoxicol Teratol. 1988;10:255–260. doi: 10.1016/0892-0362(88)90025-6. [DOI] [PubMed] [Google Scholar]
- Murray CJL. Rethinking DALYs. In: Murray CJL, Lopez A, editors. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. Boston: Harvard School of Public Health; 1996. pp. 1–98. [Google Scholar]
- Murray CJL, Lopez AD. The global burden of disease. Cambridge, MA: Harvard School of Public Health (on behalf of the WHO and World Bank); 1996. [PMC free article] [PubMed] [Google Scholar]
- Niedzielska G, Katska E, Kusa W. Hearing loss in chronic alcoholics. Annales Universitatis Mariae Curie-Sklodowska. Sectio D: Medicina. 2001;56:99–101. [PubMed] [Google Scholar]
- Olgiati P, Liappas I, Malitas P, Piperi C, Politis A, Tzavellas EO, Zisaki A, Ferrari B, De Ronchi D, Kalofoutis A, Serretti A. Depression and social phobia secondary to alcohol dependence. Neuropsychobiology. 2007;56:111–118. doi: 10.1159/000112952. [DOI] [PubMed] [Google Scholar]
- Pisoni BP, Martin CS. Effects of alcohol on the acoustic-phonetic properties of speech: perceptual and acoustic analyses. Alcohol Clin Exp Res. 1989;13:577–587. doi: 10.1111/j.1530-0277.1989.tb00381.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pisoni DB, Johnson K, Bernali RH. Effects of alcohol on speech. Proceedings of the Human Factors Society. 1991;1:694–698. [Google Scholar]
- Postma A, Van Asselen M, Keuper O, Wester AJ, Kessels RPC. Spatial and temporal order memory in Korsakoff patients. J Int Neuropsychol Soc. 2006;12:327–336. doi: 10.1017/s1355617706060449. [DOI] [PubMed] [Google Scholar]
- Rabin R, de Charro F. EQ-5D: A measure of health status from the EuroQoL group. Ann Med. 2001;33:337–343. doi: 10.3109/07853890109002087. [DOI] [PubMed] [Google Scholar]
- Rehm J, Baliunas D, Borges GLG, Graham K, Irving HM, Kehoe T, Parry CD, Patra J, Popova L, Poznyak V, Roerecke M, Room R, Samokhvalov AV, Taylor B. The relation between different dimensions of alcohol consumption and burden of disease - an overview. Addiction. 2010a;105:817–843. doi: 10.1111/j.1360-0443.2010.02899.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J, Frick U. Valuation of health states in the U.S. study to establish disability weights: lessons from the literature. Int J Methods Psychiatr Res. 2010;19:18–33. doi: 10.1002/mpr.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009a;373:2223–2233. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- Rehm J, Room R, Monteiro M, Gmel G, Graham K, Rehn N, Sempos C, Jernigan D. Alcohol as a risk factor for global burden of disease. Eur Addict Res. 2003;9:157–164. doi: 10.1159/000072222. [DOI] [PubMed] [Google Scholar]
- Rehm J, Samokhvalov AV, Neuman MG, Room R, Parry CD, Lönnroth K, Patra J, Poznyak V, Popova S. The association between alcohol use, alcohol use disorders and tuberculosis (TB). A systematic review. BMC Public Health. 2009b;9:450. doi: 10.1186/1471-2458-9-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J, Taylor B, Mohapatra S, Irving H, Baliunas D, Patra J, Roerecke M. Alcohol as a risk factor for liver cirrhosis - a systematic review and meta-analysis. Drug Alcohol Rev. 2010b doi: 10.1111/j.1465-3362.2009.00153.x. [Epub ahead of print January 20] [DOI] [PubMed] [Google Scholar]
- Ribeiro SBA, Jacob LCB, Alvarenga K, Marques JM, Camplo RM, Tschoeke SN. Auditory assessment of alcoholics in abstinence. Braz J Otorhinolaryngol. 2007;73:452–462. doi: 10.1016/S1808-8694(15)30097-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Room R, Babor T, Rehm J. Alcohol and public health: a review. Lancet. 2005;365:519–530. doi: 10.1016/S0140-6736(05)17870-2. [DOI] [PubMed] [Google Scholar]
- Room R, Rehm J, Trotter RI, Paglia A, Üstün T. Cross-cultural views on stigma, valuation, parity, and societal values towards disability. In: Üstün T, Chatterji S, Bickenbach J, Trotter RI, Room R, Rehm J, Saxena S, editors. Disability and Culture: Universalism and Diversity. Seattle: Higrefe and Huber; 2001. pp. 247–291. [Google Scholar]
- Room R. Measurement and distribution of drinking patterns and problems in general populations. In: Edwards G, Gross MM, Keller M, Moser J, Room R, editors. Alcohol-related disabilities. Geneva, Switzerland: WHO; 1977. pp. 61–87. [Google Scholar]
- Rupp CI, Fleischhacker WW, Drexler A, Mair D, Hausmann A, Hinterhuber H, Kurz M. Olfactory, executive and memory functions in alcoholism. Alcohol Clin Exp Res. 2004;28:23A. [Google Scholar]
- Rupp CI, Norcia E, Kurz M, Fleischhacker WW. Cognitive functioning and depressive symptoms in alcohol dependence. Alcohol Clin Exp Res. 2008;32:176. [Google Scholar]
- Saatcioglu O, Yapici A, Cakmak D. Quality of life, depression and anxiety in alcohol dependence. Drug Alcohol Rev. 2008;27:83–90. doi: 10.1080/09595230701711140. [DOI] [PubMed] [Google Scholar]
- Seifert J, Seeland I, Borsutzky M, Passie T, Rollnik JD, Wiese B, Emrich HM, Schneider U. Effects of acute alcohol withdrawal on memory performance in alcohol-dependent patients: a pilot study. Addiction Biology. 2003;8:75–80. doi: 10.1080/1355621031000069918. [DOI] [PubMed] [Google Scholar]
- Sheu R, Lussier D, Rosenblum A, Fong C, Portenoy J, Joseph H, Portenoy RK. Prevalence and characteristics of chronic pain in patients admitted to an outpatient drug and alcohol treatment program. Pain Med. 2008;9:911–917. doi: 10.1111/j.1526-4637.2008.00420.x. [DOI] [PubMed] [Google Scholar]
- Shore JH, Beals J, Orton H, Buchwald D. Comorbidity of alcohol abuse and dependence with medical conditions in 2 American Indian reservation communities. Alcohol Clin Exp Res. 2006;30:649–655. doi: 10.1111/j.1530-0277.2006.00076.x. [DOI] [PubMed] [Google Scholar]
- Skripnichenko ZML. Alcohol adverse effect on the organ of vision. Vestnik Oftalmologii. 1987;3:73–75. [PubMed] [Google Scholar]
- Storbjörk J, Room R. The two worlds of alcohol problems: who is in treatment and who is not? Addict Res Theory. 2008;16:67–84. [Google Scholar]
- Todor I. Memory distortions and anxiety in alcoholism: a directed-forgetting investigation. J Psychol. 2007;141:229–239. doi: 10.3200/JRLP.141.3.229-240. [DOI] [PubMed] [Google Scholar]
- Uekermann J, Daum I, Schlebusch P, Wiebel B, Trenckmann U. Depression and cognitive functioning in alcoholism. Addiction. 2003;98:1521–1529. doi: 10.1046/j.1360-0443.2003.00526.x. [DOI] [PubMed] [Google Scholar]
- Üstün TB, Chatterji S, Bickenbach J, Trotter RI, Room R, Rehm J, Saxena S. Disability and culture: universalism and diversity. Seattle: Hogrefe and Huber; 2001. [Google Scholar]
- Vanlith GHM, Henkes HE. Low vision in alcohol abuse. Doc Ophthalmol. 1979;46:333–338. doi: 10.1007/BF00142623. [DOI] [PubMed] [Google Scholar]
- Verma RK, Panda NK, Basu D, Meena R. Audiovestibular dysfunction in alcohol dependence. Are we worried? A J Otolaryngol. 2006;27:225–228. doi: 10.1016/j.amjoto.2005.09.005. [DOI] [PubMed] [Google Scholar]
- Ware J, Sherbourne C. The MOS 36-item short form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- Wells KB, Burnam MA, Benjamin B, Golding GM. Alcohol use and limitations in physical functioning in a sample of the Los Angeles general population. Alcohol Alcohol. 1990;25:673–684. doi: 10.1093/oxfordjournals.alcalc.a045065. [DOI] [PubMed] [Google Scholar]
- WHO. International classification of functioning, disability and health. Geneva, Switzerland: WHO; 2001. [Google Scholar]
- WHO. The global burden of disease: 2004 update. Geneva, Switzerland: WHO; 2008. [Google Scholar]
- Williamson AM, Feyer AM, Mattick RP, Friswell R, Finlay-Brown S. Developing measures of fatigue using an alcohol comparison to validate the effects of fatigue on performance. Accid Anal Prev. 2001;33:313–326. doi: 10.1016/s0001-4575(00)00045-2. [DOI] [PubMed] [Google Scholar]


