Abstract
Background
Familial loading for alcoholism is an important marker of risk for early onset alcohol problems, but the early expression of this risk in community samples of children is understudied.
Methods
This study tested, for 452 eight- and ten-year old children, whether density of alcohol problems in their biological relatives was associated with externalizing behaviors that are risk factors for later alcohol problems.
Results
Density of alcohol problems in first- and second-degree biological relatives was associated with behavioral disinhibition (BD; e.g., poor inhibitory control, attentional shifting, β=.10, p=.04) and conduct problems (CP; i.e., defiance, aggression, delinquency, β=.18, p=.00). These relations were moderated by parenting practices (parental warmth, discipline consistency, and parental monitoring). The density-behavior association lost statistical significance when at least two of three parenting practices were rated above median levels for the sample (p=.67 to .36). The density-behavior association was mediated by current demographic advantage, (p=.00 for BD, p=.00 for CP), current maternal mental health, (p=.01 for BD, p=.00 for CP), and current maternal deviant behavior (for CP only, p=.01).
Conclusions
Findings support previously proposed but untested pathways in etiologic models of alcoholism and show the potentially important role of active parenting in reducing the expression of inherited vulnerability to alcoholism in childhood.
Keywords: family history, child behavior, alcoholism, density of alcoholism, disinhibition
Introduction
Evidence for the familial transmission of alcoholism is well-established in the empirical literature. The heritability of alcohol use disorders is high, generally around 50% (for review, see Schuckit, 2009), and figures prominently in widely cited discussions of the etiologic pathways into problematic drinking (Leonard and Blane, 1999; Sher, 1991; Tarter and Vanyukov, 1994; Zucker, 2006). Both twin and adoption studies support the heritability of alcoholism for both men and women (Heath et al., 1997; Kendler et al., 2003). Among adolescents, heritability estimates are higher for males than for females (Han et al., 1999; Rhee et al., 2003). Genetic influences may also explain greater proportions of the variance in substance use over the course of adolescence in contrast to environmental influences which appear to be more important in early adolescence (Derringer et al., 2008).
Recent years have seen an increasing appreciation for a developmental systems approach to the study of alcoholism etiology (Zucker, 2006). This conceptual shift has resulted in more research on the mechanisms through which familial vulnerability operates and includes prospective studies of children in families with an alcoholic parent. A major focus of this research is to uncover the phenotypic manifestations of risk in childhood which may permit the development of more refined explanatory models and earlier prevention efforts. Prospective longitudinal studies of families with an alcoholic parent have shown that the children in these families are at risk for early, heavy, or problem drinking at young ages, and that externalizing behavior problems (conduct problems, attentional difficulties, defiant behavior) commonly characterize these highest-risk youth (Chassin et al., 2002; Martel et al., 2009).
Greater density of familial alcoholism, as indicated by the occurrence of the condition in multiple biological relatives beyond the parents, is also potentially important (Aston and Hill, 1990; Yuan et al., 1996). Such quantitative estimates of familial loading may be more sensitive indicators of alcoholism vulnerability than the presence or absence of the disorder in a parent (Hill et al., 2000). Milne and colleagues (2009) found that individuals with the highest family density of alcoholism were most likely to receive a diagnosis of alcoholism, to be diagnosed with alcoholism at multiple times, to report greater impairment due to their alcoholism, and to utilize treatment. Therefore, the occurrence of alcoholism in multiple biological relatives may identify a particularly potent and highly heritable form of the disorder. The most severe and chronic form of alcoholism (e.g., Type II or Type B alcoholism) is described as starting at a young age, as being coupled with externalizing behavior problems, and as reflecting a dense family history (Babor, 1996; Cloninger, 1987; Zucker, 1987). Unfortunately, the manner in which this inherited liability is expressed phenotypically prior to the onset of alcoholism is not well documented. To the extent that alcoholism is the outcome of a developmental process in which inherited vulnerability is manifested early in childhood and shaped by experience as the child ages (Zucker, 2006), documentation of the early presentation of vulnerability in children at high-risk should prove fruitful both conceptually and practically.
Expressions of disinhibited child behavior, variously referred to as “difficult temperament,” “behavioral disinhibition,” or “behavioral undercontrol,” have figured prominently in the alcoholism literature as potential mediators of genetic risk that are measurable in childhood (Sher et al., 1999; Tarter and Vanyukov, 1994; Zucker, 2006; Zucker and Gomberg, 1986). Impulsivity, novelty seeking, inattention, hyperactivity, and under-socialized behaviors such as aggression and conduct problems are commonly studied as indicators of this construct. These correlated behaviors have demonstrated heritability (Price et al., 2001; Rose et al., 1997; Slutske et al., 1997), they are more common among children of alcoholics than among children of non-alcoholics (Carbonneau et al., 1998; Chassin et al., 1991; Jester et al., 2005), and they predict adolescent alcohol use and adult alcoholism (Caspi et al., 1996; Fergusson et al., 1995; Masse and Tremblay, 1997; Nigg et al., 2006). Moreover, they are potentially indicative of underlying genetic influences common to the early onset and highly heritable form of alcoholism typically associated with chronicity and antisociality (Dick et al., 2008; Iacono et al., 1999; Zucker et al., 1995). Broadly speaking, disinhibited child behavior is an excellent candidate for the phenotypic expression of inherited alcoholism risk in childhood (Windle and Davies, 1999).
Some research has demonstrated an association between alcoholism in multiple biological relatives and offspring behavior. Research on families with at least two brothers having alcohol use disorder found that such heavy familial loading for alcoholism is associated with extraversion and with alcohol use in youth 8 to 18 years old (Hill and Yuan, 1999). However, “extraversion” only partially overlaps with the larger concept of behavioral disinihibition and among teenagers may include normative socially-mediated drinking experiences. Fuller and colleagues (2003), in contrast, focused on aggression in childhood and found higher scores in the presence of grandparent and parent alcohol problems. Although their assessments of behavior were limited (i.e., neither study assessed the full range of undercontrolled behaviors that are implicated in alcoholism theory), these studies suggest that a quantitative index of family alcohol problems (i.e., density) might predict aspects of behavior in childhood that tap the larger construct of behavioral undercontrol.
In such research, several measurement issues require attention. First, longitudinal studies often rely solely on youth self-reports of behavioral deviance which likely underestimate important aspects of behavioral disinhibition. This bias may be most problematic for the very youth at highest risk for alcoholism and for measurement of traits that require subjective judgment. It is well-documented that behaviorally disinhibited youth characteristically lack insight (e.g. Barkley et al., 2002; Hoza et al., 2002). Thus, parent and teacher ratings of child behavior are preferred in clinic-based studies of children with behavior problems.
Second, it is important to recognize the heterogeneity that exists within the higher-level construct of behavioral undercontrol (Windle, 1990). Lower-level constructs reflecting heritable traits such as “reactive control” (Martel et al., 2009) or “behavioral disinhibition” (inhibitory control problems, difficulty sustaining attention, etc.) may be distinguished from behavioral violations of social norms (i.e., conduct problems such as defiance of authority, rule breaking, etc.). The latter have also been shown to be heritable (e.g., Slutske et al., 1997) but are usually understood to result more strongly from socialization failure (Dishion and Patterson, 2006). These constructs have been distinguished from one another in many factor analytic studies and found to be differentially predictive of outcomes that increase alcoholism risk (e.g., social functioning, academic problems, aggression; Flanagan et al., 2003). Moreover, behavioral disinhibition can occur in the absence of conduct problems, and studies have demonstrated that an underlying genetic predisposition toward behavioral disinhibition in childhood can manifest as alcohol dependence in adulthood (Dick et al., 2006). However, questions continue to be raised in the literature about the extent to which family density of alcohol problems influences behavioral disinhibition in children. Capone and Wood (2008) found that the association between family density and young adult alcohol problems was mediated by impulsivity and the willingness to take risks. However, these traits were self-reported in adulthood. Thus, to determine whether familial alcoholism operates through one or more domains of behavioral undercontrol in children, more work is needed with multiple reporter data that considers the possible disaggregated structure of the larger behavioral construct.
A major influence on the expression of behavioral difficulties in high risk children that is also included in models of alcoholism etiology is the parenting environment (Sher, 1991). There is strong empirical evidence that multiple aspects of the parent-child relationship (e.g., warmth, support, low levels of conflict) and the effectiveness of parents’ child management efforts (e.g., consistency of discipline, monitoring child’s whereabouts) play an important role in minimizing or preventing behavior problems in youth, including substance use and abuse (Dishion et al., 1988; Hawkins et al., 1992). For example, parental monitoring moderates the level of genetic and environmental influences on adolescent smoking behavior. At high levels of parental monitoring, the environment accounts for 80% of the variance in adolescent smoking; at low levels of parental monitoring, genetics assume a greater importance and account for 60% of the variance in adolescent smoking (Dick et al., 2007). There is also evidence that parental monitoring mediates the impact of parent alcoholism on offspring outcome. Latendresse and colleagues (2008) found that parental monitoring partially mediated the association between alcohol use by parents (frequency of use, intoxication, and problems) and by their teenaged children (frequency of use and intoxication) in a large epidemiologic sample in Finland. Greater parental discipline, however, predicted more frequent alcohol use. This association may have reflected parental reaction to adolescent alcohol use rather than proactive child management. Chassin and colleagues (1996), studying adolescent offspring of alcoholics, found that parental monitoring partially mediated the association between paternal alcoholism and growth in child’s substance use over time. Thus, there is reason to believe from these findings and from the findings of others (Lamborn et al., 1991; Mounts and Steinberg, 1995) that the adverse effects of a high family density of alcoholism might be either exacerbated (moderated) or partially explained (mediated) by lower-quality parenting practices. Either finding would have important implications for the development of intervention strategies to minimize risk for early drinking in a highly vulnerable subgroup.
Finally, assuming there is an association between the density of alcohol problems in the family and offspring behavior in childhood, research on other mediators and moderators of this association is also needed. Parent alcohol use and mental health problems, known to affect child adjustment, may partially reflect transgenerational alcoholism and mediate the association between density of alcohol problems and child behavior. Along these lines, parental antisociality and depression have helped to explain the relation between parent alcohol problems and offspring externalizing behavior in community samples of children and adolescents (Chassin et al., 1991; El-Sheikh and Flanagan, 2001). Assortative mating among alcoholics (Merikangas and Brunetto, 1996) also increases the likelihood of such psychopathology in the family. Each of these familial adversities, including tendencies toward marital disruption and lower education, may mediate the effects of heavy familial loading for alcoholism (Zucker, 2006).
In the current study, density of alcohol problems in community children’s biological relatives was examined as a predictor of child behavior – in this case, behaviors reflecting either disinhibition or conduct problems – using data from the Tween to Teen Project of 452 children in Allegheny County, Pennsylvania. Child behavior was assessed comprehensively using parent and teacher reports for a circumscribed elementary-school age range. Thus, this study provides the first test of the association between family density of alcoholism and expressed behavioral risk in childhood in a community sample of children ascertained before the onset of alcohol use (Donovan and Molina, 2008). Moderators and mediators of this association were tested with special attention to parenting efficacy as a potentially protective moderating factor.
MATERIALS AND METHODS
Data were drawn from the first wave of an ongoing longitudinal study of the risk factors for early onset of alcohol use (the Tween to Teen Project). Human subject procedures were approved by the University of Pittsburgh Institutional Review Board. A Certificate of Confidentiality was provided by the National Institute on Alcohol Abuse and Alcoholism to help protect the identities of participants in the research.
Procedures
Families were selected for participation using targeted-age directory and random digit dialing (RDD) sampling of families in Allegheny County, Pennsylvania (population 1.3 million) which includes the city of Pittsburgh. Directory listings were provided by Survey Sampling Inc. (Fairfield, CT) and RDD lists were provided by Genesys Sampling Systems (Ft. Washington, PA). Recruitment goals included equal numbers of 8- and 10-year-olds (half of each age cohort female) and the child’s biological mother, and over-sampling of single-mother-headed and African-American families (Allegheny County is 13% African-American based on data from the U.S. Census; U.S. Census Bureau, 2007). Cohorts of 8- and 10-year old children were recruited to capture children before they had initiated regular alcohol use and to establish an accelerated longitudinal design.
Initial phone screening was conducted in 2001–2002 by the Survey Research Center of the University Center for Social and Urban Research (UCSUR) at the University of Pittsburgh. Mothers were asked about their interest in being contacted to participate in a study involving regular interviews with their 8- or 10-year old child, with them, and with their partner (if present). Tween to Teen project staff subsequently re-contacted potential participants to further assess eligibility, to determine if families met recruitment quotas, and to schedule a computer-assisted interview in participants’ homes or at our research offices.
After complete description of the study to the participants, written informed consent (assent for minors) was obtained. Computer-assisted interviews were read to the children who responded using the computer mouse. Parent computer-assisted interviews were completed independently in separate rooms. Teachers completed measures by mail.
Participants
The Tween to Teen staff identified 804 eligible families. Of these, 504 (63%) agreed to participate and 452 completed the Wave 1 interview (90% of those who agreed and 56% of those eligible). Participants did not differ significantly from non-participants on race, age-cohort, or mother’s education (see Donovan & Molina, 2008). Recruitment quotas for a diverse community sample of families were met: 92 eight-year-old boys, 118 eight-year-old girls, 122 ten-year-old boys, and 120 ten-year-old girls; 73% (331/452) were European-American; 24% (110/452) were African-American; 2% (11/452) were Other. Biological mothers participated in all families; 23% (n=106) of them were single; 92% (320/346) of household fathers/partners participated. The diversity of the sample was reflected in mother’s education: 2% had partial high school education; 20% graduated from high school; 11% had vocational-technical training; 25% had partial college education; 31% graduated from college; 10% had post-graduate education. Demographic advantage was calculated for modeling purposes, with advantage = two-parent family and/or mother having received at least some college education (n=237/452 or 52.4%). Additional details regarding recruitment of participants may be found in Donovan and Molina (2008).
Measurement of Density of Familial Alcohol Problems
Mothers completed the Mann Family Tree (Mann et al., 1985), a measure of lifetime history of alcohol problems, for themselves, for the child’s biological father, and for their own and the father’s biological siblings and parents (i.e., the child’s first- and second-degree biological relatives, excluding his/her siblings). Ratings were made on a four-point scale from 1) never drank alcohol to 4) was a definite problem drinker (had received treatment for alcohol problems or experienced alcohol-related negative consequences). An alcohol problem was defined as a rating of three (possible problem drinker) or four which is more reliable than requiring the presence of alcohol-related consequences, especially for second-degree relatives (Mann et al., 1985). Consistent with prior practice (Baer et al., 2003), density was calculated as a weighted average of: 1) the proportion of first-degree relatives (mothers/fathers only) with an alcohol problem in the lifetime; and 2) the proportion of second-degree relatives with an alcohol problem in the lifetime (M=0.16, S.D.=0.16, range=0.00 to 0.67). Density did not differ between boys and girls (p=.38). Density was higher among African-Americans than among European-Americans (M=0.21, S.D.=0.17, vs. M=0.14, S.D.=0.16), but not after controlling for maternal education and marital status, F(1, 423)=3.29, p=.07. Density was higher for children of non-married mothers (p=.000), not unexpected given the higher rates of antisocial behavior in father-absent families (Pfiffner et al., 2001). As expected, alcohol problems were more common among the fathers (33.7%) than among the mothers (4.0%). It was rare that both parents were affected (1.4% of families).
Measurement of Behavioral Disinhibition (BD) and Conduct Problems (CP)
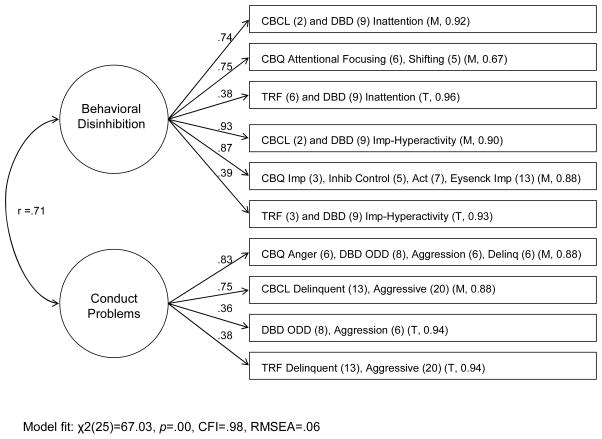
Items were selected from the larger battery to comprehensively assess the two constructs of interest, BD and CP, which have been frequently identified in prior factor analytic studies of behavioral undercontrol. Mothers completed the Child Behavior Questionnaire (CBQ; Rothbart et al., 2001), an abridged version of the Eysenck Impulsivity Scale (Eysenck et al., 1984), the Child Behavior Checklist (CBCL; Achenbach, 1991a), the Disruptive Behavior Disorders Scale (DBD; Pelham et al., 1992), a 6-item measure of Aggression (e.g., frequency of biting, pinching, pushing, or shoving other children), and a 6-item measure of delinquent behavior (e.g., “Has your child ever taken something from a store without paying for it?”). Teachers completed the Teacher Report Form (TRF; Achenbach, 1991b) and the Disruptive Behavior Disorders Scale (DBD; Pelham et al., 1992). The individual subscales, their respective numbers of items, and reporter (mother, teacher) are identified in the boxes on the right side of Figure 1. Subscale scores (means or, in the case of the Achenbach measures, T-scores divided by 10 to reduce variance for modeling purposes) were z-scored and averaged within reporter to yield six observed variable indicators for BD and four observed variable indicators for CP (see Figure 1). Confirmatory factor analysis using MPlus Version 5.1 (Muthen & Muthen, 1998–2007) was conducted to test the fit of the Figure 1 two factor model of BD and CP. This two factor model (including correlated errors to accommodate method variance) best fit the data well: χ2(25)=67.03, p=.00, CFI=.98, RMSEA=.06. Standardized factor loadings are shown in Figure 1. Mother-rated variables loaded more strongly; all factor loadings were statistically significant at p<.001 or less. As expected (Waschbusch, 2002), BD and CP were significantly correlated (r=.71). A one factor model did not fit the data better: χ2(26)=191.95, p=.00, CFI=.94, RMSEA=.12 (χ2diff (1)=124.92, p<.001). Despite their lower factor loadings, teacher reports were retained to improve the estimation of behavior cross-situationally (at home and at school). The two factor measurement model was retained and incorporated within all subsequent structural models. Factor loadings and the BD-CP intercorrelation were similar across all models.
Figure 1.
Two factor measurement model of child behavior. Note. All factor loadings are standardized and were statistically significant at p<.001 or less. Measured indicators and the bundled items are in boxes on the right; subscales are followed by their respective number of items and (M, α) indicating mother report and the associated Cronbach’s alpha, (T, α) for teacher report and the associated Cronbach’s alpha. For the CBCL and TRF, items were selected from the larger “Attention problems” subscale for their specificity (e.g., “can’t concentrate” and “daydreams” for Inattention, and “can’t sit still” and “impulsive” for Impulsivity-Hyperactivity). For ease of presentation, errors and their correlations are excluded from the diagram.
Measurement of Parenting Practices
Parenting practices were measured with child report because parents often exaggerate their behavior, and child perceptions may be just as important as actual parent behavior (Steinberg et al., 1992). Indeed, most parents rated themselves at the adaptive ends of the scales, while the children’s ratings showed greater variability.
Children reported parental discipline consistency and follow-through (Loeber et al., 1998) with eight items (e.g., “Does your mother sometimes punish you for something and at other times not punish you for the same thing?”; α = .65). Response options ranged from (1) “almost always” to (3) “never.” Parental monitoring was assessed with four items (e.g., “How much do your parents try to know about what you do with your free time?” and “How much do your parents really know about what you do with your free time?”) from the Behavioral Supervision and Strictness subscale of the Authoritative Parenting measure (Steinberg et al., 1992; α = .65). Response options ranged from (1) “don’t try” to (3) “try a lot” and (1) “don’t know” to (3) “know a lot.” Parent-child warmth was assessed with three items (e.g., “My parents like to talk with me and be with me much of the time.”) from the Parent-Child Warmth subscale of the Personal Data Form (Emery and O’Leary, 1982), α = .56. Response options ranged from (1) “not true” to “true.” Following previous work (Steinberg et al., 1992), the three subscale means were dichotomized (0, 1) near the median and summed. Parents with a sum score of 0 (11.7%) or 1 (35.6%), indicating that their child rated them above the sample median on none or on only one of three dimensions, received a parenting practice score of zero. Parents with a sum score of 2 (35.0%) or 3 (17.7%) received a parenting practice score of one.
Measurement of Parental Functioning
Current mother and father alcohol use were each composites of five variables indexing self-reported alcohol use and alcohol-related negative consequences in the past six months (Donovan, 1993). These included 1) the summed frequency of beer, wine, and liquor use, with item responses ranging from (1) did not drink (this beverage) to (11) every day; 2) the highest typical quantity of alcohol use (i.e., across beer, wine, and liquor); 3) frequency of consuming 5+ drinks in one sitting; 4) frequency of being drunk or “very, very high” on alcohol; and 5) the mean frequency of 11 alcohol-related negative consequences (e.g., “In the past six months, how many times have you missed work or had to call in sick because you had been drinking?”). These five variables were each z-scored and averaged for mothers (α=.80) and for fathers (α=.83). Current mother and father mental health were measured using the Brief Symptom Inventory (BSI; Derogatis and Melisaratos, 1983; Derogatis and Savitz, 2000), a 53-item self-report measure on which each parent indicated the presence of distress from symptoms of psychiatric disorders in the past six months (somatization, obsession-compulsion, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism subscales). These nine subscales were averaged separately for mother (α=.93) and for father (α=.94). Current mother and father deviant behavior were each measured with 11 self-report items (General Deviant Behavior Scale; Jessor et al., 1991) about general (non-substance) norm violations in the past six months (e.g., “How many times have you… taken something from a store without paying for it?”). Items were averaged within reporter.
RESULTS
Behavioral Characteristics of the Children
As expected for a community sample, the average ratings of behavior by mothers and by teachers indicated an absence of difficult temperament and externalizing behavior overall. For example, CBCL and TRF scores were near the U.S. normative averages for these scales (as indicated by T-scores in the low 50s). Also as expected, boys were usually rated higher than girls. For example, for CBCL Inattention, M=.50, S.D.=.52, for boys and M=.36, S.D.=.48 for girls, p<.01. Numbers of children with inattention, impulsivity-hyperactivity, and oppositional-defiant symptoms based on parent and teacher report with the DBD were comparable to studies using similar methods (endorsements of rating scale items and not clinical interview): 11.7% (53/452) with 6+ inattention and/or 6+ impulsivity-hyperactivity symptoms, 4.4% (20/452) with 5+ symptoms of oppositionality (Wolraich et al., 1996). A minority (28.3% or 128/452) of the sample had some conduct problems based on mother’s report on the 6-item delinquency measure (e.g., repeatedly pushing/shoving, lying, or stealing).
Association Between Density and Child Behavior
A latent variable structural equation model (SEM) was used to test the association between family density of alcoholism (one manifest continuous variable) and child behavior (the two latent variables, BD and CP, described above). The model was estimated using Maximum Likelihood and full information maximum likelihood missing data estimation in MPlus (Muthén and Muthén, 1998–2007). These estimation methods were used for all remaining structural models unless otherwise noted. The fit of the structural model was good: χ2(33)=71.30, p<.01, CFI=.99, RMSEA=.05. Statistically significant associations were found between density and BD (β=.10, p=.04) and between density and CP (β=.18, p=.00), indicating small but significant positive associations between density of alcohol problems in the family and ratings of these behaviors for children (betas are standardized). Variances explained for BD (R2=.01) and for CP (R2=.03) were small. When tested separately by gender (using a multiple-group SEM model), the fit was marginally improved by freeing the path between density and CP [χ2difference(1)=2.71, p=.10] such that density predicted CP better for boys (β=.25, p=.00) than for girls (β=.12, p=.09).
Moderation of Density-Behavior Association by Parenting Practices
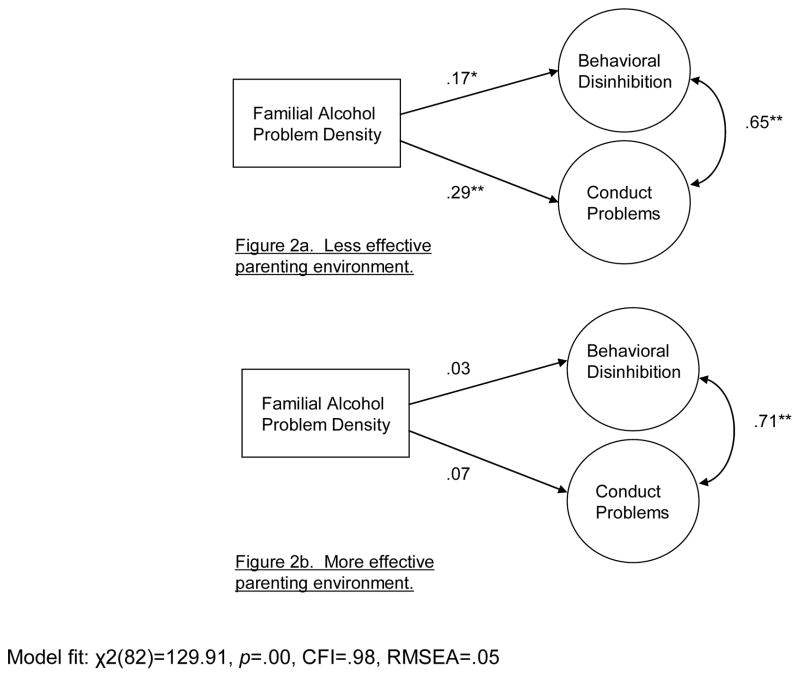
The parenting variable was tested as a moderator of the density associations with child behavior. Parenting was not tested as a mediator because it did not correlate with density (r = −.01, p=.82) which is a requirement of mediation. A multiple-group SEM analysis was conducted in which the associations between family density and child behavior were compared between children in the less effective parenting environments (n=214) and children in the more effective (n=238) parenting environments (see Figures 2a and 2b). Model fit was good with the two structural parameters (paths from density to child behavior) constrained to be equal, χ2(84)=134.78, p=.00, CFI=.98, RMSEA=.05. Model fit was marginally improved by freeing the two structural parameters [difference χ2(2)=4.87, p<.10] to result in a final model fit of χ2(82)=129.91, p=.00, CFI=.98, RMSEA=.05. As may be seen in the figures, there were large differences in the magnitude and significance of the density effects between the two groups of children. Alcohol problem density was positively and significantly associated with BD (p=.02) and with CP (p=.00) in the less effective, but not in the more effective, parenting group (p=.67 for BD, and p=.36 for CP). This pattern of effects was not changed appreciably by controlling for demographic advantage. Magnitude of effects were small to medium in size (3% to 8% of the variance in BD and in CP accounted for, respectively, in the less effective parenting environment versus 0–1% in the more effective parenting environment).
Figure 2.
Moderation of density-behavior association by parenting practices. Note. All parameters are standardized parameter estimates. For the less effective parenting environment (Figure 2a), R2 for BD=.03; R2 for CD=.08. For the more effective parenting environment (Figure 2b), R2 for BD=.00; R2 for CD=.01. *p<.05. **p<.01.
Because the grouping variable for parenting behaviors was calculated using a median-split approach, a k-means cluster analysis of the parenting variables (original continuous scores) was conducted to verify that we did not create artificial subgroupings. A two group solution resulted in two clusters of parents that significantly overlapped with the original subgroupings based on median splits, χ2(1)=151.68, p=.000. Like our original groupings, cluster 1 (n=303) had parenting subscale scores that were higher (better) than those of cluster 2 (n=149) by .54 to 1.70 standard deviations. Parenting subscale score means were nearly identical to the means for the original subgroups (e.g., for discipline, M=2.24 and 2.48 for the original parenting subgroups; M=2.24 and 2.43 for the k-means clusters). Parental monitoring was an exception, where the mean was lower for cluster 2, M=1.94, than for the parallel parenting subgroup from the original analysis, M=2.21. The moderation model was re-analyzed with the new cluster analysis subgroupings and forcing the structural parameters to be equal across groups. The fit was good: χ2 (84)=138.79, p<.001, CFI=.98, RMSEA=.05. Model fit was marginally improved by freeing the path coefficient between density and CP, χ2(1)=2.90, p<.10, resulting in model fit of χ2 (83)=135.89, p<.001, CFI=.98, RMSEA=.05. A similar pattern of parenting subgroup differences in associations between density and CP was found: β =.28, p=.001 and β =.11, p=.09 for the less and for the more effective parenting subgroups, respectively. The associations between density and BD were β =.09, p=.06, and β =.10, p=.06, for the same parenting subgroups, respectively. Given the more balanced distribution of participants across subgroups in the original analysis, and therefore more balanced power, we opted to retain the original subgroupings based on the median splits.
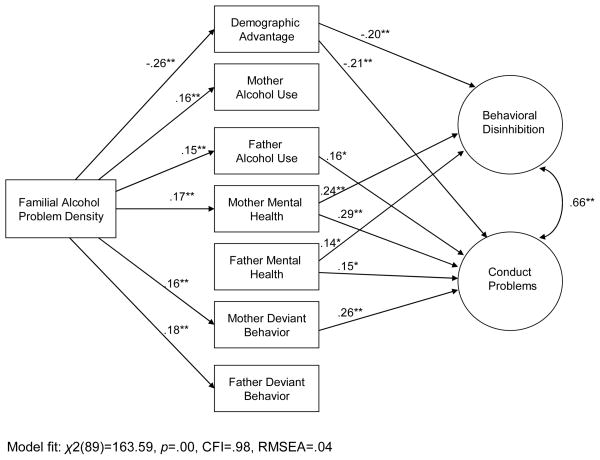
Mediation by Demographic Risk, Parent Mental Health, and Parent Alcohol Use
Figure 3 shows the mediational model in which current demographic advantage, current mother/father mental health, current deviance, and current alcohol use were tested as mediators of the association between family density of alcoholism and child behavior. The fit of the model was good: χ2(89)=163.59, p=.00, CFI=.98, RMSEA=.04. With the exception of one marginally significant association (density to father mental health, β=.11, p=.05), density was significantly associated with all of the proposed mediators, one of the requirements of a mediational model (MacKinnon et al., 2002). All but two of the proposed mediators (mother alcohol, father deviance) were associated with one or both of the dependent measures, another requirement of mediation. With these mediators included, the effect of family density diminished to nonsignificance for both BD (β=−.04, p=.45) and CP (β=−.01, p=.92). Model-produced intercorrelations among the mediators are displayed in Table 1. Table 2 shows the total effects disaggregated into direct and indirect effects. All associations between density and child behavior were mediated by current parent functioning with no direct effects of density on child behavior remaining.
Figure 3.
Mediational pathways from familial alcohol problem density to child behavior through demographic advantage and current parent functioning. Note. For ease of presentation, only statistically significant paths (p<.05) are presented, and correlations among the mediators are shown in Table 1. All parameters are standardized parameter estimates. R2 for BD=.17; R2 for CD=.35. *p<.05. **p<.01.
Table 1.
Correlations among mediators in Figure 3.
| Demographic Advantage | Mother Alcohol Use | Father Alcohol Use | Mother Mental Health | Father Mental Health | Mother Deviant Behavior | |
|---|---|---|---|---|---|---|
| Mother Alcohol Use | −.07 | |||||
| Father Alcohol Use | −.04 | .28** | ||||
| Mother Mental Health | −.10 | .18* | .04 | |||
| Father Mental Health | −.05 | −.01 | .03 | .18* | ||
| Mother Deviant Behavior | −.08 | .25** | .04 | .39** | .07 | |
| Father Deviant Behavior | .04 | .08 | .12* | .10 | .22* | .08 |
Note.
p<.05.
p<.01.
Table 2.
Total, total indirect, specific indirect, and direct effects for mediational model.
| Estimates | S.E. | Est./S.E. (mediation z-score) | Two-tailed p-value | |
|---|---|---|---|---|
| Effects from Density to BD | ||||
| Total | .35 | .20 | 1.76 | .08 |
| Total indirect | .51 | .11 | 4.54 | .00 |
| Specific indirect | ||||
| Demographic Advantage | .21 | .06 | 3.35 | .00 |
| Mother Alcohol Use | −.01 | .03 | −0.05 | .96 |
| Father Alcohol Use | .02 | .04 | 0.46 | .65 |
| Mother Mental Health | .16 | .06 | 2.76 | .01 |
| Father Mental Health | .06 | .04 | 1.54 | .12 |
| Mother Deviant Behavior | .04 | .04 | 1.18 | .24 |
| Father Deviant Behavior | .02 | .04 | 0.45 | .65 |
| Direct | ||||
| Density | −.16 | .20 | −0.76 | .45 |
| Effects from Density to CP | ||||
| Total | .60 | .21 | 2.89 | .00 |
| Total indirect | .62 | .13 | 4.81 | .00 |
| Specific indirect | ||||
| Demographic Advantage | .20 | .06 | 3.38 | .00 |
| Mother Alcohol Use | −.02 | .03 | −0.57 | .57 |
| Father Alcohol Use | .09 | .05 | 1.78 | .08 |
| Mother Mental Health | .18 | .06 | 2.96 | .00 |
| Father Mental Health | .06 | .04 | 1.49 | .14 |
| Mother Deviant Behavior | .16 | .06 | 2.65 | .01 |
| Father Deviant Behavior | −.05 | .05 | −1.10 | .27 |
| Direct | ||||
| Density | −.02 | .20 | −0.10 | .92 |
Mediation was tested using the multivariate delta method of calculating the standard error of the indirect effect (Sobel, 1982). The associated mediation z-scores are provided in Table 2, and the statistical significance of the mediation is based on bias-corrected bootstrap confidence intervals (MacKinnon et al., 2004). The 95% confidence intervals not including zero were interpreted as statistically significant. We found significant mediation of the family density effect on BD through demographic advantage (z=3.35) and through mother mental health (z=2.76). Mediation of the family density effect on CP was through demographic advantage (z=3.38), mother mental health (z=2.96), and mother deviance (z=2.65). The paths to and from father alcohol use were each statistically significant, but the mediation was marginally significant (z=1.78) and the 95% CI included zero. As a check on these findings that relied on missing data estimation, the model was run using only data from the 320 families in which two parents participated. The results [χ2(89)=155.48, p=.00, CFI=.97] were virtually identical to those found using the full sample.
We considered the possibility that parenting effectiveness should directly affect child behavior and might explain the associations between current parent characteristics and BD/CP. Thus, we added the parenting effectiveness variable as a downstream mediator between each of the current parent characteristics and BD/CP while retaining density as the upstream exogenous predictor (density→current parent characteristics→parenting effectiveness→BD and CP). The model fit the data well: χ2 (98)=183.86, p=.00, CFI=.97, RMSEA=.04. However, there were few associations between parenting and upstream (with mother alcohol use, β= −.13, p<.05) or downstream (with BD, β= −.11, p<.05) variables. No statistically significant mediation occurred to explain any of the associations between the parent characteristics and child behavior. A deconstruction of the parenting variable back to its summed form (prior to dichotomizing, in which the score ranged from 0 to 3) increased its associations with child behavior (with BD, β= −.18, p<.01; with CP, β= −.14, p<.05) but did not lead to statistically significant mediation of parent characteristic effects. Thus, parenting effectiveness appeared to operate more successfully as a moderator than as a mediator of the associations between density of alcohol problems and child behavior.
Mediated Associations for the Two Parenting Subgroups
Finally, to determine whether differential mediation of the density-to-child behavior association between the two parenting subgroups explained the greater magnitude of the density effect in the less effectively parented subgroup, we conducted a multiple group analysis of the mediated model in Figure 3 comparing the two parenting subgroups. All structural paths were constrained to be equal across the groups. This resulted in a model that fit the data well: χ2 (217)=330.191, p=.00, CFI=.96, RMSEA=.05. When the structural paths were freed across groups, model fit was marginally improved, χ2 (23)=33.69, p<.10. The individual standardized path coefficients are shown in Table 3. There were individual paths from density to the mediators, and from the mediators to child behavior, that were appreciably different across groups. For example, density and mother alcohol use were significantly associated for the less effective parenting subgroup but not for the more effective parenting subgroup. Father mental health was significantly associated with BD and with CP for the more effective, but not for the less effective, parenting subgroups. However, these differences were not reflected in mediation z-scores because group differences were not apparent in both upstream and downstream paths for individual mediators. Thus, although the main effect of family density of alcoholism on BD and CP was somewhat stronger for the less effective parenting subgroup, mediated associations between density and child behavior through current parent characteristics appeared to be similar between the subgroups.
Table 3.
Path coefficients for mediation model by parenting subgroup.
| Paths from density to mediators | Paths from mediators to BD | Paths from mediators to CP | ||||
|---|---|---|---|---|---|---|
| Parenting Effectiveness | Parenting Effectiveness | Parenting Effectiveness | ||||
| Less | More | Less | More | Less | More | |
| Demographic Advantage | −.24** | −.28** | −.23** | −.19* | −.19** | −.22** |
| Mother Alcohol Use | .22** | .09 | −.06 | .01 | −.03 | −.05 |
| Father Alcohol Use | .11 | .19* | .05 | .06 | .20* | .17* |
| Mother Mental Health | .19** | .15* | .23** | .23** | .30** | .26** |
| Father Mental Health | .10 | .13 | .03 | .31** | .05 | .24** |
| Mother Deviant Behavior | .22** | .11 | .07 | .07 | .11 | .42** |
| Father Deviant Behavior | .09 | .23** | .12 | −.06 | .01 | −.14 |
Note. Paths are standardized regression coefficients and associated p-values.
p<.05;
p<.01.
DISCUSSION
This is the first study of a community sample to examine the association between density of alcohol problems in the biological family and multiple childhood externalizing behaviors in the offspring. We found small but statistically significant associations between family density and two components of externalizing behavior: one composite variable reflecting difficulties with attention, impulse control, and overactivity, and another composite reflecting disturbance of conduct and aggression (i.e., behaviors generally reflecting problems with socialization). Theoretically suggested and practically significant moderating and mediating influences were found. The relation between family density and child externalizing behaviors was moderated by parenting practices. Family density was associated with child behavior only when parenting (e.g., monitoring of child’s whereabouts, consistency of discipline) was rated below median levels for the sample. Current demographic advantage (two parents, maternal education beyond high school) and current maternal mental health mediated the association between family density and child behavior, above and beyond the influences of other parent characteristics. Together these findings suggest that inherited vulnerability to alcoholism is visible in children’s behavior before the onset of alcohol consumption, that parental resources in the form of emotional stability and socioeconomic standing are part of the risk constellation, and that the impact of family alcoholism on child behavior is potentially modifiable at a young age.
Similar to many other studies showing strong associations between antisocial behaviors and alcoholism within individuals and within families (e.g. Zucker, 2006), we found the expected association between familial alcohol problem density and conduct problems (CP). Although the magnitude of association was small (8% of variance in the less effectively parented subgroup), this finding provides further evidence of a deviance-proneness pathway for the transmission of alcoholism in families (Sher, 1991) by extending the model to include density of alcohol problems in the family. Thus, greater familial loading may be tapping into the Type II or Type B variant of alcoholism that includes antisocial tendencies and that is more severe and chronic. The association between density and the latent factor of behavioral disinhibition, although lower in magnitude than the association between density and conduct problems, suggests that as a group these temperament traits may also play a role in alcohol vulnerability transmitted within families. These traits are visible and measureable at an early age, are highly heritable (Krueger et al., 2002; Price et al., 2001; Slutske et al., 1997), and have previously been postulated as important in the development of alcoholism (e.g. Sher et al., 1999). Our finding of a small effect was in line with the results of longitudinal studies of child behavior from non-referred samples (e.g. Caspi et al., 1995) and similar to predictions of child behavior by parental alcoholism (Martel et al., 2009). Our reliance on maternal report of alcohol problems for both sides of the family may have decreased precision of measurement. Also, our cross-sectional data did not permit us to untangle the temporal order of BD and CP, but recent prospective longitudinal studies have found support for developmental progression models in which traits akin to those in our “BD” construct (e.g., “reactive control” in Martel et al., 2009 or “hyperactivity” in Tarter et al., 2007) lead to later alcohol or substance use outcomes via the subsequent development of additional externalizing behavior problems.
Assuming replication of the current study results, the findings have potentially important implications for the early identification of alcoholism risk. Currently, the most visible evidence-based and widely discussed marker of risk for alcoholism is consumption of alcohol at a young age (DeWit et al., 2000; Grant and Dawson, 1997). This widely published finding directs interventionists’ attention to early adolescent alcohol consumption patterns. The findings of the current study, however, also suggest the potential importance of targeting child behavior at a younger age. Although the current study focused on children 8 and 10 years of age, behavior problems such as hyperactivity, impulsivity, and other indices of behavioral undercontrol may be measured at appreciably younger ages and show prediction for adolescent (Martel et al., 2009) and adulthood alcohol outcomes (Caspi et al., 1995). This pathway to alcohol problems, at least in adolescence, reliably includes proneness to deviance. Later waves of data collected in this study will allow explicit tests of the developmental progression to adolescent drinking as the children move into the peak period of risk for alcohol and drug use.
We found stronger effects of family density of alcohol problems for boys than for girls, which is consistent with reports of a possible pathway into early drinking that is more common among males and that includes “disinhibitory psychopathology” (McGue et al., 2001) and “Type II or Type B alcoholism” (Babor et al., 1992; Zucker et al., 1995). Our findings, however, do not preclude the possibility that later-developing behavior problems in girls will contribute to alcoholism risk. For example, Heath and colleagues (Heath et al., 1997) found that childhood CD was a potentially important mediator of genetic risk for alcoholism among adult female twins. Moreover, our finding of gender-specificity in this model may have been affected by our inclusion of attention regulation and outward behavioral regulation (e.g., impulse control, activity level) in the same latent construct. These variables are less linked among females. Girls are more likely to have attention regulation difficulties in the absence of other behavior problems (Milich et al., 2001). Other mediators not examined here, such as negative affect regulation, may be more relevant for girls.
Parenting practices moderated the relation between family density of alcohol problems and child behavior, such that density effects on BD and CP were reduced to non-significance when at least two of the three parenting dimensions (parental warmth, discipline consistency, and parental monitoring) were above median levels. In contrast to prior studies finding lesser quality parenting in the presence of parental alcoholism (Chassin et al., 1996) or elevated parental alcohol use (Latendresse et al., 2008), we did not find an association between density of alcoholism and parenting practices. The unique construction of our parenting variable, created to reflect the composite of parenting behaviors known to be important for child adjustment, may partly explain the different finding. We view this measurement strategy as a strength of the study that indicates the importance of multiple parenting behaviors collectively. The analytic strategy may also have decreased the possibility of measuring reactive punishment tendencies (i.e., harsh discipline in response to child misbehavior) because children had to rate their parents above median on at least two parenting practices to be included in the more effective parenting group. An equally plausible explanation for the lack of association between density of alcoholism and parenting is that a positive score on our density of alcoholism variable did not require the presence of an alcoholic parent in the home. This may explain why better child management skills were able to co-exist within some alcohol-dense families and presumably counteract the negative effects of a positive family history of alcohol problems.
These results have potentially important implications for prevention models targeting early drinking among youth. Interventions are available to improve these parenting practices (e.g., Lochman and Wells, 2004). Parents could potentially decrease risk for alcoholism among their vulnerable offspring by improving their parenting skills and subsequently reducing their child’s externalizing behavior. This is an exciting and testable proposition. However, it remains an empirical question whether reducing behavior problems in at-risk children would improve their behavioral risk for later alcohol problems. For example, nine months of intensive behavior therapy, that included behavior management training for parents of 7–9 year old children with ADHD, predicted a decreased likelihood of substance use experimentation in early adolescence (Molina et al., 2007). However, these effects were not sustained by high school age (Molina et al., 2008). In contrast, the Fast Track study showed long-lasting effects of a 10-year intervention for the most at-risk children. An intensive multi-component intervention followed by regular and periodic sessions decreased ninth grade antisocial behavior and lowered ADHD symptom scores (Conduct Problems Prevention Research Group, 2007). These results suggest the possibility that long-term interventions may be needed to sustain behavioral improvements into late adolescence when risk for heavy drinking escalates.
Our mediation model findings indicate the potentially important role of mother’s current mental health for the behavioral adjustment of the children in alcohol-dense families. Poorer maternal mental health (e.g., more symptoms of depression, anxiety, etc.), above and beyond other parental characteristics including marital status and education, significantly mediated the association of family density with both BD and with CP. As might be expected due to socialization influences occurring within families, greater maternal deviance (e.g., theft, writing bad checks) also partially explained the association between family density and child CP. Such co-occurring social disadvantage, distress, or psychopathology among parents is known to be prevalent in families with a heavy-drinking parent (but has not been documented per se among high-density families). Assortative mating may partly explain these findings (Merikangas and Brunetto, 1996). It is also possible that common genetic influences may be operating. Maternal distress and decreased “social capital” (Elgar et al., 2004) may be associated with child behavior for reasons that are environmental as well as genetic, and unidirectional or bidirectional (Rutter, 1990). For example, there is a well-established association between maternal depression and child emotional and behavioral adjustment that is believed to reflect genetic and other biological and social factors (Elgar et al., 2004). Finally, the finding that mediation of density effects was explained by mother and not by father mental health is probably a function of the higher density of alcoholism within the single mother-headed families. Had absentee (and potentially alcoholic) fathers been interviewed in these families, we might have found more mediation through current father functioning. Mediation through mother mental health may partly reflect the difficulty of raising, perhaps single-handedly, children with challenging behavioral profiles. Another explanation for the absence of mediation through father mental health might be participation by non-biological (and potentially healthier) step-fathers. However, only 10% of participating fathers/partners were not biologically related to the child in the study.
The results of the current study should be interpreted in light of the following limitations. Our measure of density relied on maternal report and is therefore subject to bias in reporting. Direct interview of biological relatives was not feasible in the current study. The reports of family history did not extend beyond the use of alcohol so it is possible that other mental health problems in the family are partly responsible for the density effects. Although our active phone recruitment methods should have decreased volunteer bias, the generalizability of our results beyond a community volunteer sample is unknown. Ultimately, however, these new findings suggest that a greater proportion of biological relatives with alcohol problems increases the chances of behavior problems in children, that the association is not large, but that it may be mitigated by effective parenting practices. These findings should be replicated, and they should be re-examined when the children are of drinking age to verify that alcohol use and related problems indeed result from the proposed pathways.
Acknowledgments
This research was supported by Grant AA-12342 from the National Institute on Alcohol Abuse and Alcoholism.
Appreciation is extended to Dr. Shirley Hill for her guidance at the early stages of analysis for this manuscript.
Footnotes
Dr. Molina, Ms. Belendiuk, and Dr. Donovan report no competing interests.
Portions of these findings were presented at the Biennial Meeting of the Society for Research on Child Development, Atlanta, GA, in April, 2005.
Contributor Information
Brooke S. G. Molina, Departments of Psychiatry & Psychology, University of Pittsburgh
John E. Donovan, Department of Psychiatry, University of Pittsburgh
Katherine A. Belendiuk, Department of Psychology, University of Pittsburgh
References
- Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 profile. University of Vermont Department of Psychiatry; Burlington, VT: 1991a. [Google Scholar]
- Achenbach TM. Manual for the Teacher’s Report Form and 1991 profile. University of Vermont Department of Psychiatry; Burlington, VT: 1991b. [Google Scholar]
- Aston CE, Hill SY. Segregation analysis of alcoholism in families ascertained through a pair of male alcoholics. Am J Hum Genet. 1990;46:879–887. [PMC free article] [PubMed] [Google Scholar]
- Babor TF. Classification of alcoholics: Typology theories from the 19th century to the present. Alcohol Health Res World. 1996;20:6–14. [PMC free article] [PubMed] [Google Scholar]
- Babor TF, Hofmann M, DelBoca FK, Hesselbrock V, Meyer RE, Dolinsky ZS, Rounsaville B. Types of alcoholics, I. Evidence for an empirically derived typology based on indicators of vulnerability and severity. Arch Gen Psychiatry. 1992;49:599–608. doi: 10.1001/archpsyc.1992.01820080007002. [DOI] [PubMed] [Google Scholar]
- Baer JS, Sampson PD, Barr HM, Connor PD, Streissguth AP. A 21-year longitudinal analysis of the effects of prenatal alcohol exposure on young adult drinking. Arch Gen Psychiatry. 2003;60:377–385. doi: 10.1001/archpsyc.60.4.377. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Fischer M, Smallish L, Fletcher K. The persistence of attention-deficit/hyperactivity disorder into young adulthood as a function of reporting source and definition of disorder. J Abnorm Psychol. 2002;111:279–289. [PubMed] [Google Scholar]
- Capone C, Wood MD. Density of familial alcoholism and its effect on alcohol use and problems in college students. Alcoholism Clinical and Experimental Research. 2008;32:1451–1458. doi: 10.1111/j.1530-0277.2008.00716.x. [DOI] [PubMed] [Google Scholar]
- Carbonneau R, Tremblay RE, Citaro F, dobkin PL, Saucier J-F, Pihl RO. Paternal alcoholism, paternal absence and the development of problem behaviors in boys from age six to twelve years. J Stud Alcohol. 1998;59:387–398. doi: 10.15288/jsa.1998.59.387. [DOI] [PubMed] [Google Scholar]
- Caspi A, Henry B, McGee RO, Moffitt TE, Silva PA. Temperamental origins of child and adolescent behavior problems: From age three to age fifteen. Child Dev. 1995;66:55–68. doi: 10.1111/j.1467-8624.1995.tb00855.x. [DOI] [PubMed] [Google Scholar]
- Caspi A, Moffitt TE, Newman DL, Silva PA. Behavioral observations at age 3 years predict adult psychiatric disorders. Arch Gen Psychiatry. 1996;53:1033–1039. doi: 10.1001/archpsyc.1996.01830110071009. [DOI] [PubMed] [Google Scholar]
- Chassin L, Pitts SC, Prost J. Binge drinking trajectories from adolescence to emerging adulthood in a high-risk sample: Predictors and substance abuse outcomes. J Consult Clin Psychol. 2002;70:67–78. [PubMed] [Google Scholar]
- Chassin L, Rogosch F, Barrera M. Substance use and symptomatology among adolescent children of alcoholics. J Abnorm Psychol. 1991;100:449–463. doi: 10.1037//0021-843x.100.4.449. [DOI] [PubMed] [Google Scholar]
- Cloninger CR. Neurogenetic adaptive mechanisms in alcoholism. Science. 1987;236:410–416. doi: 10.1126/science.2882604. [DOI] [PubMed] [Google Scholar]
- Conduct Problems Prevention Research Group. Fast track randomized controlled trial to prevent externalizing psychiatric disorders: findings from grades 3 to 9. J Am Acad Child Adolesc Psychiatry. 2007;46:1250–1262. doi: 10.1097/chi.0b013e31813e5d39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR, Melisaratos N. The Brief Symptom Inventory: An introductory report. Psychol Med. 1983;13:595–605. [PubMed] [Google Scholar]
- Derogatis LR, Savitz KL. The SCL-90-R and Brief Symptom Inventory (BSI) in primary care. In: Maruish ME, editor. Handbook of psychological assessment in primary care settings. Lawrene Erlbaum Associates; Mahwah, NJ: 2000. pp. 297–334. [Google Scholar]
- Derringer J, Krueger RF, McGue M, Iacono WG. Genetic and environmental contributions to the diversity of substances used in adolescent twins: A longitudinal study of age and sex effects. Addiction. 2008:1744–1751. doi: 10.1111/j.1360-0443.2008.02305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dick DM, Aliev F, Wang JC, Grucza RA, Schuckit M, Kuperman S, Kramer J, Hinrichs A, Bertelsen S, Budde JP, Hesselbrock V, Porjesz B, Edenberg HJ, Bierut LJ, Goate A. Using dimensional models of externalizing psychopathology to aid in gene identification. Arch Gen Psychiatry. 2008;65:310–318. doi: 10.1001/archpsyc.65.3.310. [DOI] [PubMed] [Google Scholar]
- Dick DM, Bierut LJ, Hinrichs A, Fox L, Bucholz KK, Kramer J, Kuperman S, Hesselbrock V, Schuckit M, Almasy L, Tischfield J, Porjesz B, Begleiter H, Nurnberger J, Xuei X, Edenberg HJ, Foroud T. The role of GABRA2 in risk for conduct disorder and alcohol and drug dependence across developmental stages. Behav Genet. 2006;36:577–590. doi: 10.1007/s10519-005-9041-8. [DOI] [PubMed] [Google Scholar]
- Dick DM, Viken RJ, Purcell S, Kaprio J, Pulkkinen L, Rose RJ. Parental monitoring moderates the imporance of genetic and environmental influences on adolescent smoking. J Abnorm Psychol. 2007;116:213–218. doi: 10.1037/0021-843X.116.1.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dishion TJ, Patterson GR. The development and ecology of antisocial behavior in children and adolescents. In: Cigghetti D, Cohen DJ, editors. Developmental psychopathology. Vol. 3. John Wiley & Sons; Hoboken, NJ: 2006. [Google Scholar]
- Dishion TJ, Patterson GR, Reid JR. Parent and peer factors associated with drug sampling in early adolescence: Implications for treatment. In: Rahdert ER, Grabowski J, editors. Adolescent drug abuse: Analyses of treatment research, No. 77, DHHS Publication No. ADM 88–1523 ed. Rockville, MD: 1988. pp. 69–93. [PubMed] [Google Scholar]
- Donovan JE. Young adult drinking-driving: Behavioral and psychosocial correlates. J Stud Alcohol. 1993;54:600–613. doi: 10.15288/jsa.1993.54.600. [DOI] [PubMed] [Google Scholar]
- Donovan JE, Molina BSG. Children’s introduction to alcohol use: Sips and tastes. Alcoholism Clinical and Experimental Research. 2008;32:108–119. doi: 10.1111/j.1530-0277.2007.00565.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sheikh M, Flanagan E. Parental problem drinking and children’s adjustment: Family conflict and parental depression as mediators and moderators of risk. J Abnorm Child Psychol. 2001;29:417–432. doi: 10.1023/a:1010447503252. [DOI] [PubMed] [Google Scholar]
- Elgar FJ, McGrath PJ, Waschbusch DA, Stewart SH, Curtis LJ. Mutual influences on maternal depression and child adjustment problems. Clin Psychol Rev. 2004;24:441–459. doi: 10.1016/j.cpr.2004.02.002. [DOI] [PubMed] [Google Scholar]
- Emery RE, O’Leary KD. Children’s perceptions of marital discord and behavior problems of boys and girls. J Abnorm Child Psychol. 1982;10:11–24. doi: 10.1007/BF00915948. [DOI] [PubMed] [Google Scholar]
- Eysenck SBG, Easting G, Pearson PR. Age norms for impulsiveness, venturesomeness, and empathy in children. Personality and Individual Differences. 1984;5:315–321. [Google Scholar]
- Fergusson DM, Horwood LJ, Lynskey MD. The prevalence and risk factors associated with abusive or hazardous alcohol consumption in 16-year olds. Addiction. 1995;90:935–946. doi: 10.1046/j.1360-0443.1995.9079356.x. [DOI] [PubMed] [Google Scholar]
- Fuller BE, Chermack ST, Cruise KA, Kirsch E, Fitzgerald HE, Zucker RA. Predictors of aggression across three generations among sons of alcoholics: Relationships involving grandparental and parental alcoholism, child aggression, marital aggression and parenting practices. Q J Stud Alcohol. 2003;64:472–483. doi: 10.15288/jsa.2003.64.472. [DOI] [PubMed] [Google Scholar]
- Han C, McGue M, Iacono WG. Life-time tobacco, alcohol and other substance use in adolescent Minnesota twins: Univariate and multivariate behavioral genetic analyses. Addiction. 1999;94:981–983. doi: 10.1046/j.1360-0443.1999.9479814.x. [DOI] [PubMed] [Google Scholar]
- Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: Implications for substance abuse prevention. Psychol Bull. 1992;112:64–105. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- Heath AC, Bucholz KK, Madden PAF, Dinwiddie SH, Slutske WS, Bierut LJ, Statham DJ, Dunne MP, Whitfield JB, Martin NG. Genetic and environmental contributions to alcohol dependence risk in a national twin sample: Consistency of findings in women and men. Psychol Med. 1997;27:1381–1396. doi: 10.1017/s0033291797005643. [DOI] [PubMed] [Google Scholar]
- Hill SY, Shen S, Lowers L, Locke J. Factors predicting the onset of adolescent drinking in families at high risk for developing alcoholism. Biol Psychiatry. 2000;48:265–275. doi: 10.1016/s0006-3223(00)00841-6. [DOI] [PubMed] [Google Scholar]
- Hill SY, Yuan H. Familial density of alcoholism and onset of adolescent drinking. J Stud Alcohol. 1999;60:7–17. doi: 10.15288/jsa.1999.60.7. [DOI] [PubMed] [Google Scholar]
- Hoza B, Pelham WE, Dobbs J, Owens JS, Pillow DR. Do boys with attention-deficit/hyperactivity disorder have positive illusory self-concepts? J Abnorm Psychol. 2002;111:268–278. doi: 10.1037//0021-843x.111.2.268. [DOI] [PubMed] [Google Scholar]
- Iacono WG, Carlson SR, Taylor J, Elkins IJ, McGue M. Behavioral disinhibition and the development of substance use disorders: Findings from the Minnesota Twin Family Study. Dev Psychopathol. 1999;11:869–900. doi: 10.1017/s0954579499002369. [DOI] [PubMed] [Google Scholar]
- Jessor R, Donovan JE, Costa FM. Beyond adolescence: Problem behavior and young adult development. Cambridge University Press; Cambridge, England: 1991. [Google Scholar]
- Jester JM, Nigg JT, Adams K, Fitzgerald H, Puttler LI, Wong MM, Zucker RA. Inattention/hyperactivity and aggression from early childhood to adolescence: heterogeneity of trajectories and differential influence of family environment characteristics. Dev Psychopathol. 2005;17:99–125. doi: 10.1017/50954579405050066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Etiological connections among substance dependence, antisocial behavior, and personality: Modeling the externalizing spectrum. J Abnorm Psychol. 2002;111:411–424. [PubMed] [Google Scholar]
- Lamborn SD, Mounts NS, Steinberg L, Dornbusch SM. Patterns of competence and adjustment among adolescents from authoritative, authoritarian, indulgent, and neglectful families. Child Dev. 1991;62:1049–1065. doi: 10.1111/j.1467-8624.1991.tb01588.x. [DOI] [PubMed] [Google Scholar]
- Latendresse SJ, Rose RJ, Viken RJ, Pulkkinen L, Kaprio J, Dick DM. Parenting mechanisms in links between parents’ and adolescents’ alcohol use behaviors. Alcoholism: Clinical and Experimental Research. 2008;33:322–330. doi: 10.1111/j.1530-0277.2007.00583.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard KE, Blane HT. Psychological theories of drinking and alcoholism. 2. Guildford Press; New York, NY: 1999. [Google Scholar]
- Lochman JE, Wells KC. The Coping Power Program for preadolescent aggressive boys and their parents: Outcome effects at the 1-year follow-up. J Consult Clin Psychol. 2004;72:571–578. doi: 10.1037/0022-006X.72.4.571. [DOI] [PubMed] [Google Scholar]
- Loeber R, Farrington DP, Stouthamer-Loeber M, Van Kammen WB. Antisocial behavior and mental health problems. Lawrence Erlbaum Associates, Inc; Mahwah, NJ: 1998. [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39:99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann RE, Sobell LC, Sobell MB, Pavan D. Reliability of a Family Tree questionnaire for assessing family history of alcohol problems. Drug Alcohol Depend. 1985;15:61–67. doi: 10.1016/0376-8716(85)90030-4. [DOI] [PubMed] [Google Scholar]
- Martel MM, Pierce L, Nigg JT, Jester JM, Adams K, Puttler LI, Buu A, Fitzgerald H, Zucker RA. Temperament pathways to childhood disruptive behavior and adolescent substance abuse: Testing a cascade model. J Abnorm Child Psychol. 2009;37:363–373. doi: 10.1007/s10802-008-9269-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masse LC, Tremblay RE. Behavior of boys in kindergarten and the onset of substance use during adolescence. Arch Gen Psychiatry. 1997;54:62–68. doi: 10.1001/archpsyc.1997.01830130068014. [DOI] [PubMed] [Google Scholar]
- McGue M, Iacono WG, Legrand LN, Elkins I. Origins and consequences of age at first drink. II. Familial risk and heritability. Alcoholism Clinical and Experimental Research. 2001;25:1166–1173. [PubMed] [Google Scholar]
- Merikangas KR, Brunetto W. Assortative mating and psychiatric disorders. In: Papadimitriou G, Mendlewicz J, editors. Bailliere’s Clinical Psychiatry: International Practice and Research. Bailliere Tindall; London, England: 1996. pp. 175–185. [Google Scholar]
- Milich R, Balentine AC, Lynam DR. ADHD Combined Type and ADHD Predominately Inattentive Type are Distinct and Unrelated Disorders. Clinical Psychology: Science and Practice. 2001;8:463–488. [Google Scholar]
- Milne BJ, Caspi A, Harrington H, Poulton R, Rutter M, Moffitt TE. Predictive value of family history on severity of illness: The case for depression, anxiety, alcohol dependence, and drug dependence. Arch Gen Psychiatry. 2009;66:738–747. doi: 10.1001/archgenpsychiatry.2009.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina BSG. Substance use, abuse, and dependence as a function of prior treatment and ADHD symptom trajectory in the MTA. In: Volkow ND, Swanson J Chairs, editors. Effects of stimulant treatment of ADHD in childhood and adolescence and subsequent drug abuse in adulthood ADHD; Symposium at the Annual Meeting of the American Academy of Child and Adolescent Psychiatry; Chicago, IL. 2008. [Google Scholar]
- Molina BSG, Flory K, Hinshaw SP, Greiner AR, Arnold LE, Swanson J, Hechtman J, Jensen PS, Vitiello B, Hoza B, Pelham WE, Elliott GR, Wells KC, Abikoff HB, Gibbons RD, Marcus S, Epstein J, Conners CK, Greenhill LL, March J, Newcorn JH, Severe JB, Wigal T. Delinquent behavior and emerging substance use in the MTA at 36-months: Prevalence, course, and treatment effects. J J Am Acad Child Adolesc Psychiatry. 2007;46:1027–1039. doi: 10.1097/chi.0b013e3180686d96. [DOI] [PubMed] [Google Scholar]
- Molina BSG, Hinshaw SP, Swanson JM, Arnold LE, Vitiello B, Jensen PS, Epstein JN, Hoza B, Hechtman L, Abikoff HB, Elliott GR, Greenhill LL, Newcorn JH, Wells KC, Wigal T, Gibbons RD, Hur K, Houck PR, MTA Cooperative Group The MTA at 8 years: prospective follow-up of children treated for combined-type ADHD in a multisite study. J Am Acad Child Adolesc Psychiatry. 2009;48:484–500. doi: 10.1097/CHI.0b013e31819c23d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mounts NS, Steinberg L. An ecological analysis of peer influence on adolescent grade point average and drug use. Dev Psychol. 1995;31:915–922. [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 5. Muthen & Muthen; Los Angeles, C.A: 1998–2007. [Google Scholar]
- Nigg JT, Wong MM, Martel MM, Jester JM, Puttler LI, Glass JM, Adams KM, Fitzgerald HE, Zucker RA. Poor response inhibition as a predictor of problem drinking and illicit drug use in adolescents at risk for alcoholism and other substance use disorders. J Am Acad Child Adolesc Psychiatry. 2006;45:468–475. doi: 10.1097/01.chi.0000199028.76452.a9. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Gnagy EM, Greenslade KE, Milich R. Teacher ratings of DSM-III-R symptoms for the disruptive behavior disorders. J Am Acad Child Adolesc Psychiatry. 1992;31:210–218. doi: 10.1097/00004583-199203000-00006. [DOI] [PubMed] [Google Scholar]
- Pfiffner LJ, McBurnett K, Rathouz PJ. Father absence and familial antisocial characteristics. J Abnorm Child Psychol. 2001;29:357–367. doi: 10.1023/a:1010421301435. [DOI] [PubMed] [Google Scholar]
- Price TS, Simonoff E, Waldman I, Asherson P, Plomin R. Hyperactivity in preschool children is highly heritable. J Am Acad Child Adolesc Psychiatry. 2001;40:1362–1364. doi: 10.1097/00004583-200112000-00002. [DOI] [PubMed] [Google Scholar]
- Rhee SH, Hewitt JK, SEY, Corley RP, Crowley TJ, Stallings MC. Genetic and environmental influences on substance initiation, use, and problem use in adolesents. Arch Gen Psychiatry. 2003;60:1256–1264. doi: 10.1001/archpsyc.60.12.1256. [DOI] [PubMed] [Google Scholar]
- Rose RJ, Kaprio J, Pulkkinen L, Koskenvuo M, Viken RJ, Bates JE. FinnTwin12 and FinnTwin16: Longitudinal twin-family studies in Finland. Behav Genet. 1997:27. [Google Scholar]
- Rothbart MK, Ahadi SA, Hersey KL, Fisher P. Investigations of temperament at three to seven years: The Children’s Behavior Questionnaire. Child Dev. 2001;72:1394–1408. doi: 10.1111/1467-8624.00355. [DOI] [PubMed] [Google Scholar]
- Rutter M. Commentary: Some focus and process considerations regarding effects of parental depression on children. Dev Psychol. 1990;26:60–67. [Google Scholar]
- Schuckit M. An overview of genetic influences in alcoholism. J Subst Abuse Treat. 2009;36:S5–14. [PubMed] [Google Scholar]
- Sher KJ. Children of alcoholics. A critical appraisal of theory and research. The University of Chicago Press; Chicago: 1991. [Google Scholar]
- Sher KJ, Trull TJ, Bartholow BD, Vieth A. Personality and alcoholism: Issues, methods, and etiological processes. In: Leonard KE, Blane HT, editors. Psychological theories of drinking and alcoholism. 2. Guilford Press; New York, NY: 1999. [Google Scholar]
- Slutske WS, Heath AC, Dinwiddie SH, Madden PAF, Bucholz KK, Dunne MP, Statham DJ, Martin NG. Modeling genetic and environmental influences in the etiology of conduct disorder: A study of 2,682 adult twin pairs. J Abnorm Psychol. 1997;106:266–279. doi: 10.1037//0021-843x.106.2.266. [DOI] [PubMed] [Google Scholar]
- Sobel ME. Asymptotic intervals for indirect effects in structural equation models. In: Leinhart S, editor. Sociological methodology 1982. Jossey-Bass; San Francisco, CA: 1982. pp. 290–312. [Google Scholar]
- Steinberg L, Lamborn S, Dornbusch S, Darling N. Impact of parenting practices on adolescent achievement: Authoritative parenting, school involvement, encouragement to succeed. Child Dev. 1992;63:1266–1281. doi: 10.1111/j.1467-8624.1992.tb01694.x. [DOI] [PubMed] [Google Scholar]
- Tarter RE, Kirisci L, Feske U, Vanyukov M. Modeling the pathways linking childhood hyperactivity and substance use disorder in young adulthood. Psychology of Addictive Behaviors. 2007;21:266–271. doi: 10.1037/0893-164X.21.2.266. [DOI] [PubMed] [Google Scholar]
- Tarter RE, Vanyukov M. Alcoholism: A developmental disorder. J Consult Clin Psychol. 1994;62:1096–1107. doi: 10.1037//0022-006x.62.6.1096. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. Allegheny County QuickFacts from the US Census Bureau. Vol. 2007 2007. [Google Scholar]
- Waschbusch DA. A meta-analytic examination of comorbid hyperactive-impulsive-attention problems and conduct problems. Psychological Bulletim. 2002;128:118–150. doi: 10.1037/0033-2909.128.1.118. [DOI] [PubMed] [Google Scholar]
- Windle M. Temperament and personality attributes of children of alcoholics. In: Windle M, editor. Children of alcoholics. Critical Perspectives. The Guilford Press; New York, NY: 1990. pp. 129–167. [Google Scholar]
- Windle M, Davies PT. Developmental theory and research. In: Leonard KE, Blane HT, editors. Psychological theories of drinking and alcoholism. 2. Guilford Press; New York: 1999. pp. 164–202. [Google Scholar]
- Wolraich ML, Hannah JN, Pinnock TY, Maumgaertel A, Brown J. Comparison of diagnostic criteria for Attention-Deficit/Hyperactivity Disorder in a county-wide sample. J Am Acad Child Adolesc Psychiatry. 1996;35:319–324. doi: 10.1097/00004583-199603000-00013. [DOI] [PubMed] [Google Scholar]
- Yuan H, Marazita M, Hill SY. Segregation analysis of alcoholism in high density families: A replication. Am J Med Genet. 1996;67:71–76. doi: 10.1002/(SICI)1096-8628(19960216)67:1<71::AID-AJMG12>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- Zucker RA. The four alcoholisms: A developmental account of the etiological process. In: Rivers PC, editor. Nebraska Symposium on Motivation: Vol. 34, Alcohol and addictive behavior. University of Nebraska Press; Lincoln: 1987. pp. 27–83. [PubMed] [Google Scholar]
- Zucker RA. Alcohol use and the alcohol use disorders: A developmental-biopsychosocial systems formulation covering the life course. In: Cicchette D, Cohen DJ, editors. Developmental Psychopathology, Second Edition, Volume Three: Risk, Disorder, and Adaptation. Vol. 3. John Wiley & Sons, Inc; Hoboken, NJ: 2006. pp. 620–656. [Google Scholar]
- Zucker RA, Fitzgerald HE, Moses HD. Emergence of alcohol problems and the several alcoholisms: A developmental perspective on etiologic theory and life course trajectory. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology: Vol. 2. Risk, disorder, and adaptation. Wiley; New York: 1995. pp. 677–711. [Google Scholar]
- Zucker RA, Gomberg ESL. Etiology of alcoholism reconsidered. Am Psychol. 1986;41:783–793. doi: 10.1037//0003-066x.41.7.783. [DOI] [PubMed] [Google Scholar]