LIVER transplantation has been offered at the University of Pittsburgh since early 1981. The principal criterion for case selection when an organ becomes available is recipient medical urgency. In 1987, a point system was developed by us for the equitable distribution of extrarenal organs, and this was adopted by the United Network for Organ Sharing (UNOS).1,2 In addition to medical urgency, time waiting and proximity to the transplant center of both the donor and recipient contribute to the points accrued by a candidate. No credits or demerits are given for race, color, creed, national origin, or socioeconomic class.
In this study, we examined the percentage of transplants performed by race as well as the outcomes in the ethnic subgroups. The broad categories of black and nonblack were used. The nonblack group was further subdivided into Caucasian, Hispanics, and Asians. We were particularly interested to see if the patterns of organ distribution were significantly different before and after the implementation of the point system in 1987.
PATIENTS AND METHODS
One thousand four hundred twenty-nine (1429) patients underwent 1829 liver transplantations at the University of Pittsburgh between March 1981 and December 1988. Liver-kidney, liver-heart, liver-pancreas, and multivisceral transplantations were not included.
The donor and recipient had the same ABO blood type unless the urgency was so great that the patient could not wait. The incidence of ABO compatible but not identical donors or ABO incompatible donors3 was less than 10%. Postoperative immunosuppression was with cyclosporine and prednisone, to which azathioprine and OKT3 were added variably as adjuncts. Actuarial patient and graft survivals were calculated. Statistical analysis was performed using BMDP software. Significance was assessed by the Mantle-Cox or the Breslow test.
RESULTS
Ethnic Representation
Over the 8-year period, there were 1309 nonblack patients and 120 (8.4%) who were black (Table 1). Other minorities, which included Hispanic, Asians, and American Indians, accounted for 94 recipients (6.6%). Thus, the total representation of minorities was 15% (Table 1).
Table 1.
Ethnic Distribution in 1429 Liver Transplant Recipients, 1981-1988
| White | 1215 | (85%) |
| Black | 120 | (8.4%) |
| Other minoritiesa | 94 | (6.6%) |
Hispanic, Asian, and American Indians.
The number of minority cases was not changed by the institution of the point system in early 1987. If anything, the percentage of black recipients dropped off in 1987 and 1988 compared to the highwater year of 1986 (Fig 1).
Fig 1.
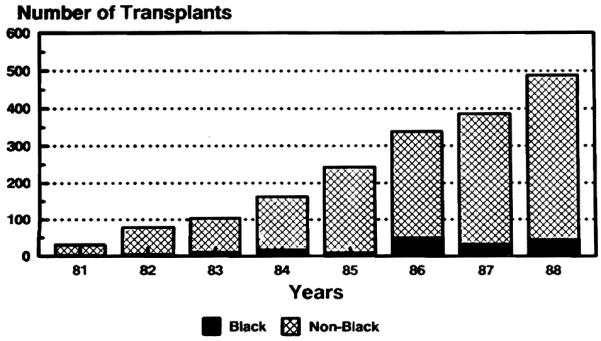
Black and nonblack recipients by year from 1981 through 1988. The point system was first used in 1987.
Ethnicity and Survival
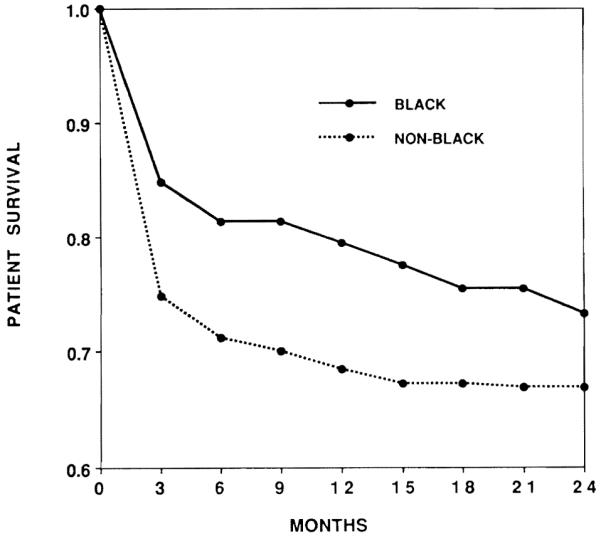
Two-year survival curves are shown in Fig 2. Hispanic recipients did best, Asians fared worst, and black and white patients were in between. The results in black recipients were not significantly different at 2 years from those in the combined other groups (Fig 3).
Fig 2.
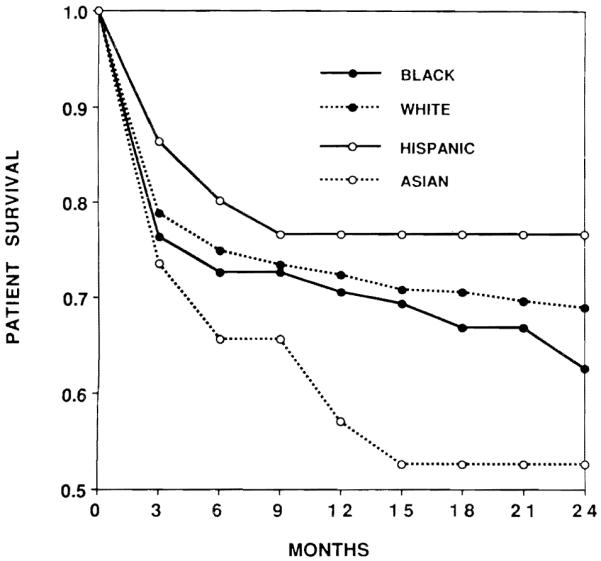
Two-year patient survival of liver transplants by race, 1981 through 1988.
Fig 3.
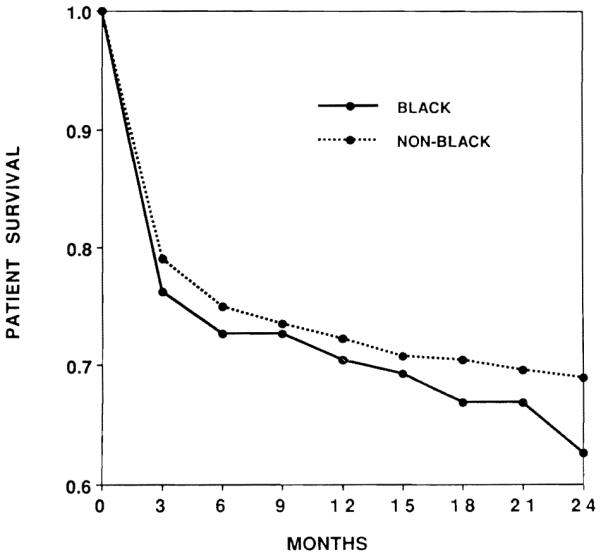
Two-year survival for black vs nonblack liver recipients, 1981 through 1988.
An Artifact of Age
The mean age of the 120 black patients was 19.3 ± 16.4 (SD) years, compared to 31.9 ± 20.4 (SD) for the 1309 nonblack patients. This meant that there was a substantially higher proportion of black pediatric recipients, relative to the total black patient pool, in comparison to the white recipients. Therefore, it became necessary to analyze the pediatric and adult patient populations separately.
The Average Adult Black Recipient
The liver diseases for which treatment was undertaken were very similar among adult blacks and nonblacks (Table 2). However, black adults were underrepresented relative to the rest of the adult patients, both before and after the implementation of the point system in early 1987. Throughout the 8 years (1981-1988), blacks accounted for only 6.0% of the adults receiving transplants. Furthermore, the average age of the black patients was 33.95 ± 10.20 (SD) years vs 43.36 ± 12.44 (SD) years for the nonblack group.
Table 2.
Liver Diseases of Adult Recipients, 1981-1988
| Disease | Black | Nonblack | Total |
|---|---|---|---|
| Cirrhosis (postnecrotic and cryptogenic) |
18 | 269 | 287 |
| HBsAg positive | 3 | 61 | 64 |
| Alcoholic | 5 | 103 | 108 |
| Primary biliary cirrhosis | 4 | 203 | 207 |
| Primary sclerosing cholangitis | 10 | 91 | 101 |
| Liver-based inborn metabolic er- rors (α1-antitrypsin deficiency, Wilson’s disease) |
1 | 50 | 51 |
| Primary hepatic malignancy | 4 | 50 | 54 |
| Fulminant hepatic failure | 11 | 37 | 48 |
| Secondary biliary cirrhosis | — | 13 | 13 |
| Budd-Chiari syndrome | 1 | 18 | 19 |
| Bile duct cancer | — | 10 | 10 |
| Secondary hepatic malignancy | — | 8 | 8 |
| Others | 3 | 24 | 27 |
| Total | 60 | 937 | 997 |
Black women appeared to have a different incidence of disease requiring transplant. Thirty-eight of the 60 black adults were females. The diagnosis of primary biliary cirrhosis, a predominantly woman’s disease was the reason for transplantation 207 times. Only 4 of these recipients were black.
Survival for the small number of blacks who managed to get into the candidacy stream leading to eventual transplantation was inferior to that of nonblacks (Fig 4). By the end of 2 years, less than half of the black recipients were alive compared to 70% of nonblacks (p < 0.015).
Fig 4.
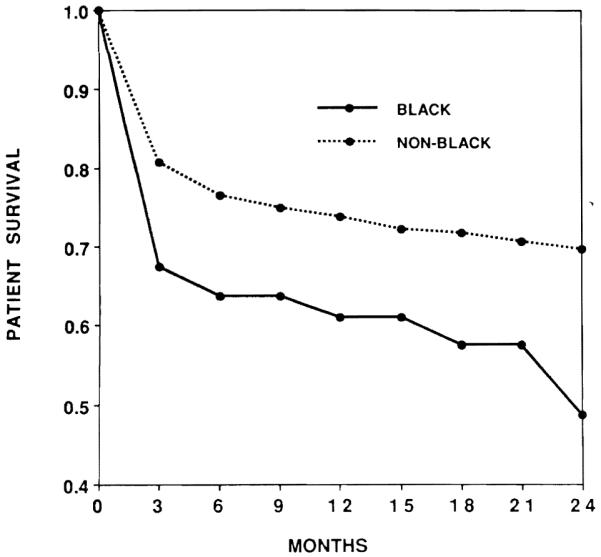
Two-year survival of black vs nonblack adults, 1981 through 1988.
The Average Pediatric Black Recipient
Black infants and children had most of the same diseases as their nonblack counterparts (Table 3). They represented 13.9% of the pediatric caseload, which was defined by an age ceiling of 18 years. The mean age of the black patients was 5.21 ± 4.70 (SD) years vs 5.44 ± 4.62 (SD) for nonblacks.
Table 3.
Liver Diseases of Pediatric Recipients, 1981-1988
| Disease | Black | Nonblack | Total |
|---|---|---|---|
| Biliary atresia | 46 | 188 | 234 |
| Liver-based inborn metabolic er- rors (α1-antitrypsin deficiency, Wilson’s disease) |
1 | 73 | 74 |
| Cirrhosis (postnecrotic and cryptogenic) |
5 | 39 | 44 |
| Familial cholestatic syndrome | — | 15 | 15 |
| Fulminant hepatic failure | 3 | 20 | 23 |
| Secondary biliary cirrhosis | — | 9 | 9 |
| Congenital hepatic fibrosis | — | 6 | 6 |
| Primary hepatic malignancy | 2 | 6 | 8 |
| Budd-Chiari syndrome | — | 2 | 2 |
| Neonatal hepatitis | 1 | 4 | 5 |
| Others | 2 | 10 | 12 |
| Total | 60 | 372 | 432 |
In contrast to the adults, the black pediatric recipients survived at a higher rate at all postoperative times than their nonblack companions (Fig 5). At 2 years, three-quarters of the blacks were alive vs two thirds of the nonblacks. These differences were not significant (p = 0.184).
Fig 5.
Two-year pediatric liver transplant survival, black vs nonblack, 1981 through 1988.
DISCUSSION
This is the first report of the influence of race on liver candidacy and on posttransplantation survival. Overall, the black recipients did not do worse than the nonblack patients, an observation similar to that reported from our center with renal transplantation.4 However, a closer look at the black transplant constituency revealed a disquieting trend that suggested the difficulty of older blacks in gaining entry to the waiting list.
This was a difficulty not encountered to the same degree by black pediatric recipients, who represented 13.9% of the pediatric cases. Most of these patients were treated after 1983. Late in that year, a decision was made by Federal Medicare and announced by the Secretary of the Department of Health, Education and Welfare (HEW) that liver transplantation was a service as opposed to an experimental operation but only for those who were 18 years old or younger. This meant that black infants and children could qualify for coverage under the Social Security system. More important, it strengthened their claim to other federal insurance programs, such as CHAMPUS, and on conventional civilian health insurance carriers.
Unfortunately, the Medicare ruling retained the terminology of “experimental” if a liver transplantation candidate was older than 18 years. This administrative stigma has never been formally removed. The natural consequence has been that socially and economically underprivileged adults have been selectively denied life-saving health care. Black adults have been disproportionately affected.
The extent of the injustice can be further illustrated by examining reports from the National Center For Health Statistics about chronic liver disease and cirrhosis.5 Liver disease was the ninth leading cause of death for all races in the United States in 1986. Black males had a death rate from liver disease of 17.3/100,000, whereas in white males, the figure was 14.1/100,000. Since the black population of the United States is 12.2% of the total, it would seem obvious that the percentage of adult liver recipients should be at least as high as nonblack recipients and probably even slightly greater.
The point system is color blind. However, it ensures equity only after entry to the candidacy list. The naked prejudice implicit in our data is fiscal in nature.6 There is no medical justification for such a prejudice, since the overall results are equivalent in blacks and whites. The degraded results in adult blacks were most obvious perioperatively and may have reflected the more advanced disease that seemed common in this population. The poor results also could represent economic and vocational hardships even after a successful transplantation. That there is no inherent biologic explanation is evident from the superior results in black infants and children.
Acknowledgments
Supported by Research Grants from the Veterans Administration and Project Grant No. DK 29961 from the National Institutes of Health.
REFERENCES
- 1.Starzl TE, Gordon RD, Tzakis A, et al. Transplant Proc. 1988;20:131. [PMC free article] [PubMed] [Google Scholar]
- 2.Starzl TE, Shapiro R, Teperman L. Transplant Proc. 1989;21:3422. [PMC free article] [PubMed] [Google Scholar]
- 3.Gordon R, Iwatsuki S, Esquivel C, et al. Transplant Proc. 1987;19:4575. [PMC free article] [PubMed] [Google Scholar]
- 4.Shapiro R, Tzakis A, Hakala T. Transplant Proc. this issue. [PMC free article] [PubMed] [Google Scholar]
- 5.National Center for Health Statistics Monthly Vital Statistics Report. 1988 September 30;37(6) [Google Scholar]
- 6.Bryant DD. J Natl Med Assoc. 1985;77:113. [PMC free article] [PubMed] [Google Scholar]


