In a recent publication,1 attention was directed to an increased incidence of intra-abdominal emergencies in recipients of renal homo-grafts who were being treated with immunosuppression. The most common disorders were complications of peptic ulcer disease, intestinal obstruction, and appendicitis. Only one example was cited of a surgically significant colon lesion.
Since then, several fatal colonic complications have been seen. Because of the lethal nature of this kind of problem, these cases, as well as several earlier unpublished ones, have been compiled for the present report. There were ten patients (Table 1) who developed difficulties with the large bowel in the series of 243 renal and 31 hepatic homotransplantations.
Colonic Problems
| No. | Age | Sex | Nature of Colonic Problem | Time After Transplant | Treatment | Outcome |
|---|---|---|---|---|---|---|
| 1 | 46 yr | M | Perforated sigmoid diverticulitis | Approx 24 days | Defunctioning colostomy, antibiotics | Died |
| 2 | 46 yr | F | Perforated sigmoid diverticulitis | 200 days | Defunctioning colostomy, repair of perforation, antibiotics |
Died |
| 3 | 20 yr | F | Perforation of transverse colon; leak at colonic anastomotic site |
89 days; 104 days | Resection of affected colon; transverse colostomy |
Died |
| 4 | 19 yr | M | Pseudomembranous enterocolitis | Unknown | Fluid and blood replacement, antibiotics | Died of septicemia secondary to enterocolitis |
| 5 | 40 yr | F | Ulceration o f the colon (? granulomatous colitis) |
Approx 56 days | Fluid and blood replacement, antibiotics | Died |
| 6 | 12 yr | F | Ulceration of the colon | Approx 578 days | Fluid and blood replacement | Died |
| 7 | 10 yr | M | Massive fecal impaction at the hepatic flexure |
8 days | Multiple enemas, laparotomy and breaking up of fecal mass, further enemas |
Alive |
| 8 | 17 yr | F | Massive fecal impaction at the hepatic flexure |
8 days | Multiple enemas, Cantor tube and administration of stool softeners and purgatives |
Alive |
| 9 | 39 yr | M | Injury of sigmoid colon | At time of transplant | Repair | Alive |
| 10 | 27 yr | M | Injury of splenic flexure; subphrenic abscess |
103 days; 110 days |
Drainage of abscess, defunctioning transverse colostomy |
Died |
| 11 | 1 yr 4 mo | F | Injury to transverse colon | At time of transplant | Repair | Alive |
Report of Cases
CASE 1
More than four years after transplantation from an unrelated donor, a renal homograft failed; it had been placed in the right iliac fossa. A kidney from a cadaver donor was then transplanted retroperitoneally on the opposite side without removing the first homograft. From the time of the second operation the patient had a low-grade fever, which was initially attributed to therapy with antilymphocyte globulin (ALG). One week following operation he complained of pain in the wound, and during the ensuing days the fever became more marked and was associated with chills. However, the wound appeared to be normal.
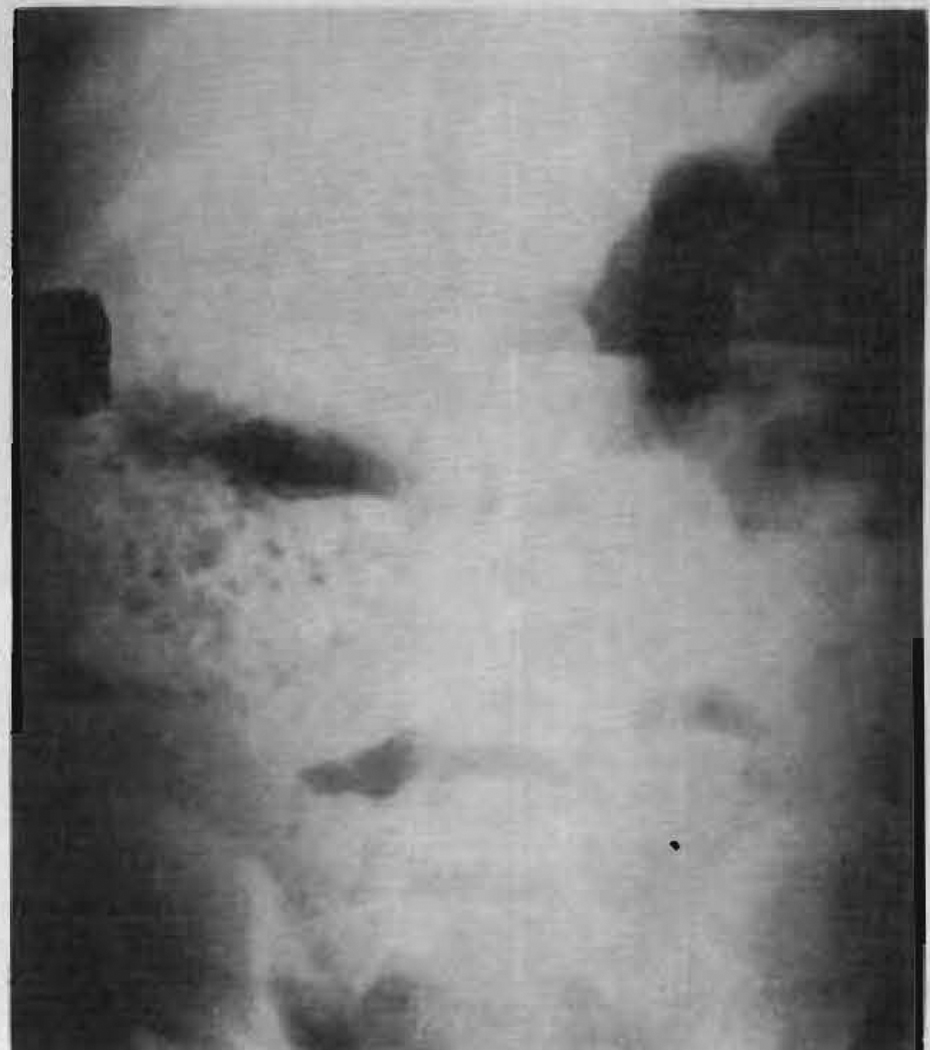
Twenty-six days later a high fever associated with hypotension developed in the patient. The next day a fluctuant mass appeared in the wound. This was opened and a large amount of pus containing Escherichia coli, Pseudomonas aeruginosa and Proteus vulgaris was evacuated from the area surrounding the transplanted kidney. The appropriate antibiotics were administered and the wound was thoroughly irrigated daily, Until that time the patient had received from 50 to 100 mgm of prednisone per day, but dosage was now reduced. Six days later feces was found draining from the wound. Radiographic studies (Fig 1 and 2) demonstrated diverticula in the sigmoid and descending colon, with a colocutaneous fistula. A transverse colostomy was performed. However, his condition progressively deteriorated and he died 60 days posttransplantation. Autopsy examination confirmed the diagnosis of perforated diverticulitis, with a large abscess surrounding the transplanted kidney. In addition, a purulent peritonitis was present.
Fig. 1.
Injection of 50% diatrizoate (Hypaque) sodium through catheter introduced into perinephric abscess cavity. Results in visualization of sigmoid colon and demonstrates diverticula (case 1).
Fig. 2.
Barium enema examination of medial displacement of colon by transplanted kidney, and extravasation of contrast medium into dressings covering abscess cavity (case 1).
CASE 2
Two hundred days after her operation the patient was being treated for an episode of threatened rejection of the transplanted kidney, associated with hypertension and poor kidney function, when lower abdominal pain and signs of peritonitis suddenly developed in the patient.
Operation revealed thick, creamy, yellow-white pus in the peritoneal cavity. Diverticula were present in the sigmoid colon, and one of these had perforated. The perforation was closed, the proximal sigmoid colon was exteriorized as a colostomy, and the abdomen was drained. Despite fluids administered intravenously, antibiotic therapy, nasogastric suction, and reduction of steroid therapy, the patient failed to recover from the peritonitis and died ten days following laparotomy.
CASE 3
Eighty-nine days after renal transplantation, while on a dose of 40 mgm of prednisone per day, severe abdominal pain and signs of generalized peritonitis suddenly developed in the patient. Abdominal exploration revealed a 2-mm perforation in the left portion of the transverse colon. No diverticula could be found. The lesion was treated by resection of a 7.5-cm segment of colon, containing the perforated area, and end-to-end anastomosis was performed. Histologic examination of the lesion showed acute inflammation, necrosis, and granulation tissue along the path of the fistula.
Postoperatively, the peritonitis settled down satisfactorily with antibiotic therapy and reduction of steroid dosage but renal function deteriorated. Large doses of steroids were given, but severe rejection of the kidney continued and hemodialysis became necessary.
Fifteen days after the colonic operation abdominal pain and generalized peritonitis again suddenly developed in the patient. Operation showed a small leak at the site of the previous anastomosis. The perforated segment of colon was exteriorized as a left transverse colostomy.
The patient was making a satisfactory recovery from this operation when a massive nosebleed developed on the fourth postoperative day and she died.
CASE 4
Following renal transplantation, the patient had fever accompanied by anorexia and episodes of abdominal pain. His stools were persistently positive for occult blood. These symptoms occurred while receiving 60 mgm of prednisone per day.
Thirty-four days after transplantation massive upper-gastrointestinal tract bleeding necessitated emergency vagotomy and pyloroplasty for its control. This, however, was only temporarily successful. A gram-negative septicemia occurred with thrombocytopenia, gross hematuria, and resumption of gastrointestinal bleeding; the patient died six days after gastric surgery. Homograft function remained adequate throughout the course.
At autopsy a severe pseudomembranous enterocolitis was found. Pseudomonas aeruginosa was cultured from the colon, peritoneal fluid, blood, urinary bladder, kidney, and lungs. The patient had received intermittent antibiotic therapy (methicillin sodium, streptomycin sulfate, and chloramphenicol succinate) at various stages of his postoperative course.
CASE 5
Multiple postoperative complications marred the patient’s postoperative course. Severe weight loss and generalized wasting were attributed to the high dosage of steroid therapy. Recurrent episodes of upper-gastrointestinal tract bleeding occurred, but the patient refused surgical treatment. Fifty-six days after renal transplantation, fever and a urinary fistula developed. This necessitated revision of the previous ureteroureterostomy, which healed satisfactorily. Several days later a further massive gastrointestinal bleed required emergency vagotomy and pyloroplasty for its control.
From the time of ureteral repair the patient was febrile, and numerous investigations were performed to find the cause. Cystitis was diagnosed and the patient was treated vigorously with antibiotics but fever persisted. Her course was progressively downhill. She had severe diarrhea during the last four weeks of her life. Terminally, severe pneumonia developed and she died 108 days after transplantation. Besides pneumonia, autopsy examination revealed multiple severe ulcerations of the colon. Histologic examination of the lesions was suggestive of actinomycosis, but no fungi could be obtained on culturing material from the ulcers.
CASE 6
The patient had been in good health with good urinary function for 578 days after renal transplantation. Then markedly impaired renal function, hypertension, and severe hypermagnesemia suddenly developed in the patient. She was treated with increased doses of steroids, antihypertensive drugs, and two hemodialyses. Eleven days after readmission to the hospital she began to pass guiac-positive stools, but without diarrhea. One of the stools contained tissue, which was diagnosed histologically as a pseudomembranous slough of the bowel mucosa. Sixteen days after admission she developed a herpes zoster eruption on the right chest wall. She died the next day after suddenly developing bleeding from the mouth, multiple ecchymoses, a small hematemesis, and very frequent melena stools. Coagulation studies showed a prothrombin time of less than 10%, and severe fibrinolysis. There was no evidence of a consumption coagulopathy. There was also a marked elevation of the serum glutamic oxaloacetic transaminase and lactic dehydrogenase levels.
At autopsy there was severe ulceration of the colon, with very little mucosa present from the ileocecal valve to the anus. Histologic examination showed lesions in the colon, liver, and other organs which contained inclusion bodies suggestive of varicella virus. Postmortem blood cultures contained Staphylococcus aurells.
CASE 7
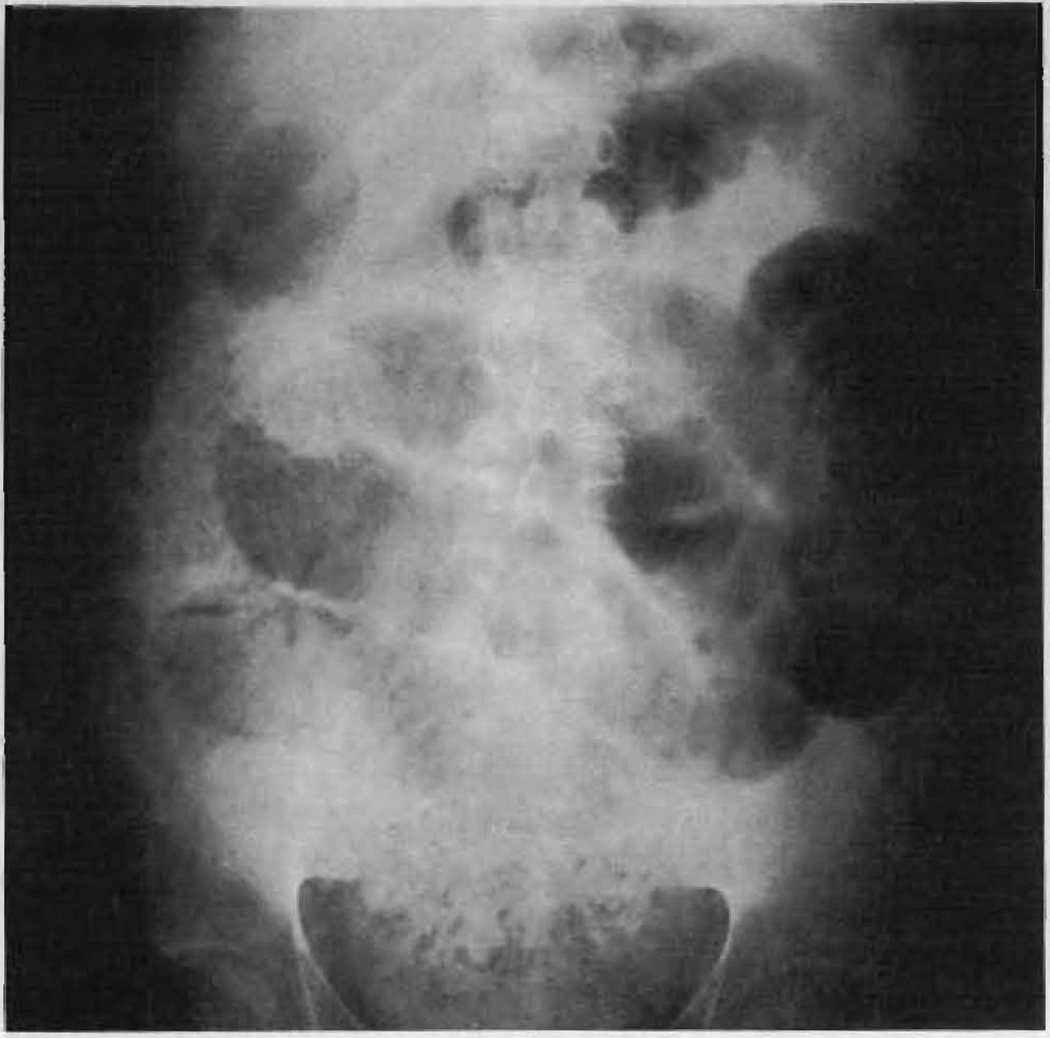
A 10-year-old boy suffered from cystinosis, which resulted in renal failure. Prior to his transplant operation, there was a long history of recurrent bouts of constipation which had been treated with stool softeners and a mixture of biphosphate and sodium phosphate (Phospho-Soda). The kidney was obtained from a 10-year-old cadaver donor and was placed extraperitoneally in the right lower quadrant. In addition, bilateral nephrectomy and splenectomy were performed. Eight days after his operation he complained of abdominal pain, his abdomen became moderately distended, and there was a suggestion of a mass on the right side above the transplanted kidney. Radiographic studies (Fig 3) showed small-bowel obstruction. Despite treatment with enemas, nasogastric suction, and fluids administered intravenously, he became more distended and the pain became more severe. The next day a radiograph revealed progression of the obstruction, and operation was performed. A large, hard, mass of feces was firmly impacted at the hepatic flexure. The small bowel proximally was grossly dilated, while the colon distally was completely collapsed. The mass was manually broken up and milked along the colon. In addition, a small enterotomy was used to decompress the small bowel. Postoperatively, frequent enemas and purgatives were necessary to prevent a recurrence of the fecal impaction. A pelvic abscess caused by Escherichia coli required drainage after the relief of the obstruction. This closed in and healed eventually.
Fig. 3.
Radiograph in upright position. Large fecal mass in right colon with dilated loops of small bowel proximally (case 7).
CASE 8
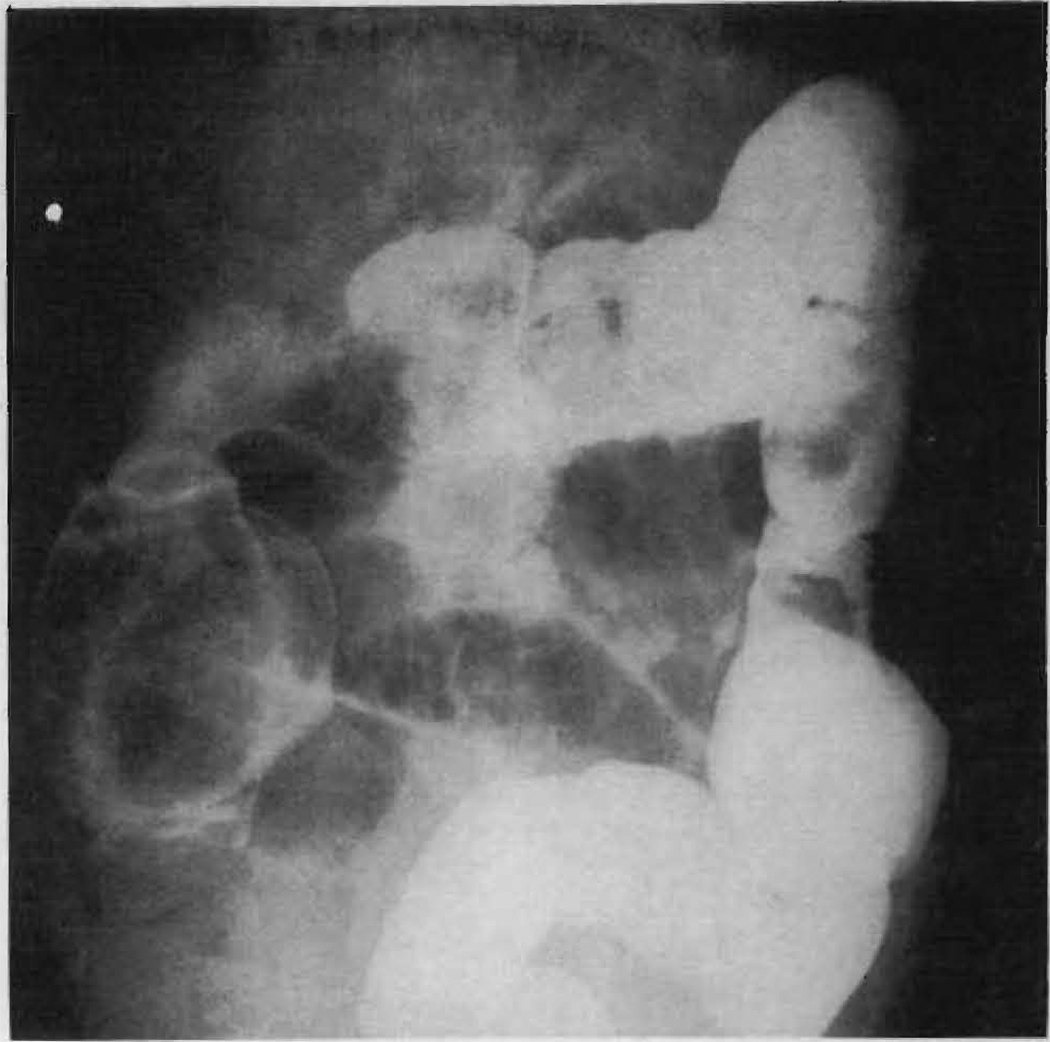
Eight days after orthotopic liver transplantation the patient complained of constipation but was initially able to pass flatus. Despite several enemas, her abdomen became very distended and she vomited. Radiographs of the abdomen (Fig 4 to 6) showed small-bowel obstruction proximal to a large fecal impaction in the cecum and ascending colon, a finding confirmed by barium enema examination. Treatment with nasogastric suction, fluids administered intravenously, and repeated enemas failed to relieve her condition. A Cantor tube was passed along the small bowel, which was then thoroughly decompressed. A series of enemas containing either dioctyl sodium sulfosuccinate (Colace), olive oil, trypsin, or soap suds was administered, and later these were supplemented by the administration through the Cantor tube of acetylcysteine, castor oil, milk of magnesia, and magnesium sulfate. This attack on the fecal mass from above and below broke up the impaction, and within 48 hours the patient passed large quantities of liquid feces containing hard fecal masses. Her symptoms subsided completely. Subsequently, she was treated with stool softeners and mild laxatives to avoid a recurrence of the colonic problem.
Fig. 4.
Radiograph in supine position. Large fecal mass in the right colon with dilated loops of small bowel proximately (case 8).
Fig. 6.
Radiograph of Cantor tube in decompressed small bowel. Residual barium is present in colon and fecal mass is well outlined (case 8).
CASE 9
At the renal transplant operation, a small opening was inadvertently made in the sigmoid colon. This was immediately repaired in two layers. The patient was treated with potassium penicillin and chloramphenicol for the first six postoperative days. On the 13th day a superficial wound infection caused by Staphylococcus aureus developed. The patient responded satisfactorily to thorough drainage, daily dressings, and the administration of methicillin.
CASE 10
One hundred and three days after kidney transplantation the abdomen was reexplored because of recurrent bouts of abdominal pain, weight loss, and persistently elevated serum amylase levels. Severe inflammation and pseudocyst formation, involving the tail of the pancreas, necessitated a distal pancreatectomy. The operation was very difficult because of dense adhesions. The splenic flexure of the colon, which formed part of the wall of the pseudocyst, was traumatized but not perforated. A week later it was necessary to drain a left subphrenic abscess, which had resulted from leakage from the site of colonic injury. A defunctioning transverse colostomy was also performed. Despite vigorous antibiotic therapy the patient’s condition progressively deteriorated, and he died 127 days after transplantation. Renal function remained satisfactory throughout his course.
CASE 11
During the performance of the recipient hepatectomy in the course of an orthotopic liver transplantation for congenital biliary atresia, very dense adhesions between the liver and bowel were encountered. In freeing these, two rents were produced in the transverse colon. These were immediately repaired in two layers. Postoperatively, the patient was treated with antibiotics, in addition to the immunosuppressive agents azathioprine (Imuran), prednisone, and antilymphocyte globulin (ALG). No complications attributable to the colonic injury occurred in the 105 days of postoperative life.
Comment
Disturbances of bowel activity are common in renal homograft recipients. Before the transplant operation the patient may have a hypomotility syndrome, or even frank ileus, because of uremia.2 At the time of transplantation, the patient usually has a laparotomy for removal of both kidneys and spleen, and is thus a candidate for postoperative ileus. After transplantation there may be a period of poor renal function, which may perpetuate a preexisting hypomotility state. When a large organ is placed in a relatively small abdomen, as in renal transplantation from an adult donor to a child, a period of postoperative ileus is common, especially if rejection of the organ occurs. As soon as the patient can take liquids by mouth he is given large doses of antacids to prevent gastric complications, which may result from steroid therapy. At times, the nonabsorbable antacid gels may cause constipation or fecal impaction.3 Similar problems may also be encountered in liver homograft recipients. It is well known that fecal impaction can cause complete bowel obstruction,4 or may even cause death.5
In order to avoid these problems in organ recipients, the colon is kept empty by preoperative and postoperative enemas. In spite of such precautions, high-grade intestinal obstruction from fecal impaction in the right colon developed in two patients in the present series. In one case, laparotomy became necessary (case 7), while in the other (case 8) conservative measures were successful. The child who required operation suffered from cystinosis, a disease in which constipation often occurs.6
Since transplant recipients must be treated with agents that reduce their immunologic reactivity, a very great risk would be anticipated from colon complications that cause fecal contamination. This expectation was realized in three patients of the present series who developed perforation. The mortality in this group was 100%, despite the fact that the drug doses, particularly with the steroids, were promptly and drastically reduced. The perforations were controlled either by proximal colostomy or, in one case, by excision of the diseased bowel and primary reanastomosis. Nevertheless, death followed within a few days or weeks.
The question as to whether a colonic perforation in immunosuppressed patients should be treated by performing a colostomy in preference to primary resection does not yet appear to be settled. It is clear that an acute traumatic injury to the colon can be closed primarily with the expectation of prompt healing (cases 9 and 11), but healing was not accomplished (cases 1 to 3) in the presence of preexisting fecal peritonitis. On the other hand, our experience with proximal colostomy has also been uniformly unsuccessful. The only renal transplant recipient known to have survived for a prolonged period with a colostomy is that of DeLorimer et al.7 Their patient developed a colonic perforation ten days after transplantation and resection of a bilateral Wilms’ tumor. The difficult mobilization of the left kidney had apparently caused devascularization of the bowel. The condition was treated by resection of the perforated area of bowel and a double-barreled colostomy. This was successfully closed five months later.
Although there have only been occasional reports in the literature,1,7 there is reason to believe that colon perforation will not be rare in organ homograft recipients. In addition to our experience, we have learned by personal communication that Monaco has had two patients die from this kind of complication and that DeBakey has had to treat perforated diverticulitis in three of his first ten recipients of orthotopic cardiac homografts.
In our series, fatalities from colonic disorders have also been seen in three patients who did not have gross fecal contamination of the peritonemn (cases 4 to 6). An unexplained clinical state developed, for which the cause was discovered only at autopsy. In all three of the recipients, the etiology was colitis, which was either nonspecific or which had many of the features of pseudomembranous enterocolitis.
As already discussed, the disease for which organ transplantation is undertaken could predispose to colon complications, which in turn would have a peculiarly dangerous connotation because of the bacterial flora in feces. Moreover, the immunosuppressive agents (azathioprine, prednisone, and in some cases ALG) all undermine host defenses to invading bacteria from any focus, including the intestinal tract.
An additional dimension is that the drugs used to prevent rejection may contribute to colonic perforation. This has been especially well documented with steroids,8–10 although not with azathioprine and ALG, under conditions not involving transplantation. Use of the agents together could conceivably increase the risk, since the cumulative result of treating organ recipients with combination drug therapy is lymphoid depletion. It is conceivable that atrophic changes in intestinal lymphoid collections could weaken resistance to bacterial invasion at a local tissue level or could even cause thinning of the bowel wall.
Summary
Colonic complications have been seen in eleven immunosuppressed recipients of kidney and liver homografts. The lesions included perforation, colitis, fecal impaction, and iatrogenic laceration. The colons, which were repaired immediately after their injury, healed uneventfully. In all cases in which perforation or serious colitis developed, the patients died. There were two examples of severe fecal impaction of the ascending colon; one was successfully treated conservatively, but the other required operation.
Fig. 5.
Barium enema examination of large fecal mass in right colon (case 8).
Acknowledgments
This investigation was supported by Public Health Service grants AM-06344, AM-07772, FR-00051, AI-04152, FR-00069, AM-12148, and AT-AT-08898.
Footnotes
Nonproprietary and Trade Names of Drug
Acetylcysteine—Mucomyst, NAC.
References
- 1.Penn I, et al. Surgically Corredable Intra-Abdominal Complications Before and After Renal Homotransplantation. Ann Surg. 1968 Nov;168:865–870. doi: 10.1097/00000658-196811000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Starzl TE. Experience in Renal Transplantation. Philadelphia: W. B. Saunders Co.; 1964. chap 12. [Google Scholar]
- 3.Brettschneider L, Monafo W, Osborne DP. Intestinal Obstruction Due to Antacid Gels: Complication of Medical Therapy for Gastrointestinal Bleeding. Gastroenterology. 1965 Sept;49:291–294. [PubMed] [Google Scholar]
- 4.Davis JH. In: Complications in Surgery and Their Management. ed 2. Artz CP, Hardy JD, editors. Philadelphia: W. B. Saunders Co.; 1967. p. p 213. [Google Scholar]
- 5.Wangensteen OH. Intestinal Obstructions: Physiological, Pathological and Clinical Considerations With Emphasis on Therapy, Including Description of Operative Procedures. ed 3. Springfield, Ill: Charles C Thomas, Publisher; 1955. p. p 526. [Google Scholar]
- 6.Ellis RWB. Disease in Infancy and Childhood. ed 4. Edinburgh: E. & S. Livingstone, Ltd.; 1963. p. p 469. [Google Scholar]
- 7.DeLorimer AA, et al. Simultaneous Bilateral Nephrectomy and Renal Allotransplantation for Bilateral Wilms’ Tumor. Surgery. 1968 Oct;64:850–855. [PubMed] [Google Scholar]
- 8.Fein BT. Perforation and Inflammation of Diverticula of the Colon Secondary to Long-Term Adrenocorticosteroid Therapy for Bronchial Asthma and Pulmonary Emphysema. Southern Med J. 1961 April;54:355–359. doi: 10.1097/00007611-196104000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Sauer WG, Dearing WH, Wollaeger EE. Serious Untoward Gastrointestinal Manifestations Possibly Related to Administration of Cortisone and Corticotrophin. Mayo Clin Proc. 1953 Nov;28:641–649. [PubMed] [Google Scholar]
- 10.Sautter RD, Ziffren SE. Adrenocortical Steroid Therapy Resulting in Unusual Gastrointestinal Complications. Arch Surg. 1959 Aug;79:346–356. doi: 10.1001/archsurg.1959.04320080182021. [DOI] [PubMed] [Google Scholar]