Twenty-six years after the first human liver transplantation was performed in Denver,1 the procedure has evolved into the preferred therapy for end-stage liver disease of various etiologies. A number of significant events have enabled this transformation of an experimental to a service procedure. These include the following four critical steps:
The first use of cyclosporine in clinical trials in 19792 and its systemic combination with steroids3,4 were essential. The use of cyclosporine in combination with other immunosuppressive agents, that is, prednisone, azathioprine, and antilymphocyte globulin, resulted in markedly improved results in cadaveric renal and extra-renal organ transplantation.3–5
The introduction and routine use of the veno-venous bypass in 19836–8 made the procedure safer for the patient and technically easier for the surgeon. It has allowed for the training of a new generation of liver transplant surgeons.
The National Consensus Meeting at the National Institutes of Health in 1983 determined that liver transplantation was no longer an experimental, but rather a therapeutic procedure for a variety of chronic irreversible liver diseases.9 This administrative blessing allowed the broad application of liver transplantation.
A new preservation solution developed at the University of Wisconsin by Dr F. O. Belzer and associates became available in the fall of 1987.10 Safe preservation of the liver for greater than 24 hours became possible.11 Although the impact and revolutionary effects of this advance are immediately evident, their full extent has surely not as yet been appreciated.
LIVER TRANSPLANTATION FOR PRIMARY BILIARY CIRRHOSIS
One of the most favorable indications for liver transplantation has traditionally been cholestatic liver disease.12 Primary biliary cirrhosis (PBC), one of the cholestatic syndromes, is the second most common indication for liver transplantation in the adult,13,14 accounting for 16.5% of all liver transplants performed.
There are two reasons why liver transplantation is favored treatment for PBC. First, survival is substantially better than that to be expected with conservative management.12,13 Second, good health is restored with the operation. About 90% of the recipients transplanted for PBC have returned to their occupation at least part time. In contrast, the group of patients who stoically endure their disease are on a march to a miserable death.
THE ISSUE OF RECURRENCE OF THE DISEASE AFTER TRANSPLANTATION
The initial report of recurrence of PBC in three patients by Neuberger et al15 was not confirmed in the Pittsburgh experience.16 Recurrence of the disease, using the criteria described by Neuberger et al,15 was not found by Demetris et al17 in a recent pathologic review of graft specimens obtained from 106 patients with PBC. The antimitochondrial antibodies (AMA) usually returned or never went away (see Berg and Klein in this issue of Seminars), but this was not reflected in the homografts. PBC-like changes were observed by the Cambridge group18 in transplant patients who did not have the disease originally. An increased incidence of chronic rejection in the patients transplanted for PBC was noted by the Pittsburgh group,17 but the significance of this is purely speculative.
It is possible that the histopathologic changes of PBC or the natural course of the disease could be altered by treatment with cyclosporine. However, the study has never been done adequately.
THE SUCCESS RATE
For 194 patients with PBC transplanted between 1973 and 1988 at the University of Colorado and the University of Pittsburgh (see later), 1-year actuarial survival was 75.62%; the 5-year actuarial survival is 70.71% (Fig. 1). These cases included four from the precyclosporine era.
FIG. 1.
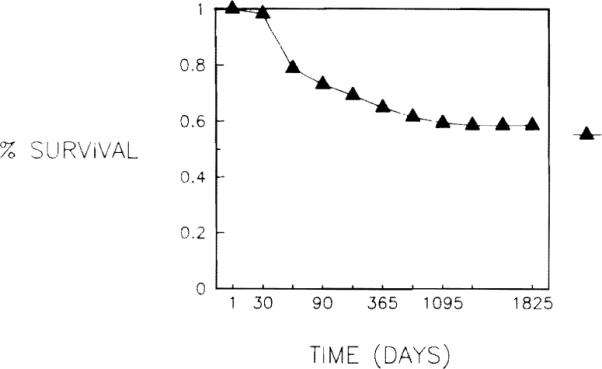
Five-year survival of patients with PBC treated with transplantation at the University of Pittsburgh.
INFLUENCE OF TRANSPLANTATION ON SURVIVAL
There is strong evidence that transplantation improves the survival of patients with PBC. Results of transplantation for PBC in Cambridge and Pittsburgh have been compared with predicted survival calculated from a statistical model (see Grambsch et al in this issue of Seminars). In both centers the results suggest a significant benefit from transplantation.
The Cambridge Series
The predicted survial of the first 29 patients (using the Cambridge model), who underwent liver transplantation for PBC at Cambridge, King's College hospital, was compared with their actual survival after transplantation.19 The comparison favored transplantation, even though the 1-year survival in this group of transplant patients was only 25%
The Pittsburgh Series, Judged with the Mayo Model
The Mayo model is a recently developed statistical model that predicts survival in PBC patients who have not undergone transplantation. It uses five variables: age, total serum bilirubin and albumin, prothrombin time, and edema (see Grambsch et al in this issue of Seminars.)
One hundred sixty-one patients with a median follow-up of 25 months after transplantation were studied. Their actual survival, when compared with the predicted survival of a simulated control group using the Mayo model, was 76% versus 45% at 1 year, and 74% versus 31% at 2 years.20
The transplant patients were further divided into three risk groups, and their survival was compared with the actuarial survival of simulated controls. The advantage of transplantation was observed in all three groups.20
PROGNOSTIC VALUE OF THE PREOPERATIVE CLINICAL VARIABLES
The Pittsburgh experience with 194 patients who underwent 230 liver transplantations for PBC between April, 1973, and June, 1988, was reviewed. Their ages ranged from 23.5 to 76.6 years (mean, 48.1 ± 9.5 SD). Eleven of the patients (5.7%) were males and 183 (94.3%) were females. Survival was calculated at 1 year after transplantation.
The clinical variables studied were: age, gender, time elapsed between diagnosis of the disease and transplantation, previous surgery, pathologic staging, ascites, total bilirubin, prothrombin time, creatinine, liver weight, and encephalopathy. Groups were defined within the variables in order to allow analysis of the survival data. Survival curves and statistical analysis were calculated on an IBM-AT computer using BMOP software (Los Angeles, CA).
The results are summarized in Table 1. A number of variables were found to have no prognostic significance. Thus, survival in patients with encephalopathy was 69.6% versus 78.4% in those without. Gender also failed to influence survival: Of 11 male patients, 9 (81.8%) are alive as are 136 (74.3%) of the 183 females. Survival according to the time elapsed between diagnosis of PBC and transplantation is shown in Table 2. The known duration of the disease had no effect on survival after transplantation. Notable also is that patients older than 50 years fared at least as well as t h e younger group.21
TABLE 1.
The Relationship of Clinical Variables to Survival
| Variable and Group | No. | Survival | Significance |
|---|---|---|---|
| Age (yr) | |||
| >60 | 26 | 81.3% | |
| 50–60 | 46 | 75.4% | |
| <50 | 100 | 72.5% | 0.5787 |
| Previous surgery | |||
| None | 71 | 80.7% | |
| (R) Upper abdomen | 36 | 67.9% | |
| Other | 35 | 67.3 | 0.1220 |
| Pathologic staging* | |||
| Stage 3 | 21 | 77.8% | |
| Stage 4 | 117 | 73.6% | 0.8239–0.6453* |
| Ascites | |||
| Controlled | 63 | 64.9% | |
| Uncontrolled | 8 | 88.9% | |
| None | 70 | 82.4% | 0.0165 |
| Total bilirubin (mg/dl) | |||
| >20 | 32 | 66.7% | |
| 10–20 | 65 | 75.6% | |
| 2–10 | 37 | 78.7% | |
| <2 | 8 | 88.9% | 0.3857 |
| Prothrombin time (sec) | |||
| >15 | 10 | 55.6% | |
| <15 | 129 | 77.2% | 0.0826–0.0431† |
| Creatinine (mg/dl): | |||
| >1.3 | 10 | 58.8% | |
| <1.3 | 128 | 76.6% | 0.1859–0.1059† |
| Liver weight (native hepatectomy specimen) (% of body weight) |
|||
| >3.5 | 56 | 77.8% | |
| 2.5–3.5 | 54 | 77.1% | |
| <2.5 | 31 | 66.0% | 0.2900 |
No patients at stage 2 or 3 were transplanted at our center.
Before the Yates correction.
TABLE 2.
Survival According to the Time Elapsed Between the Diagnosis of PBC and Transplantation
| Years Elapsed | No. | Alive | Dead | Percent |
|---|---|---|---|---|
| 1 | 18 | 16 | 2 | 88.8 |
| 2 | 14 | 8 | 6 | 57.1 |
| 3 | 19 | 15 | 4 | 78.9 |
| 4 | 26 | 20 | 6 | 76.9 |
| 5 | 19 | 10 | 9 | 52.6 |
| 6 | 14 | 9 | 5 | 64.2 |
| 7 | 11 | 9 | 2 | 81.8 |
| 8 | 17 | 15 | 2 | 88.2 |
| 9 or more | 48 | 38 | 10 | 79.1 |
Comments
Although none of these variables has a statistically significant predictive value, some groups appear to be associated with a poor survival, for example, patients with a total bilirubin greater than 20 mg/dl, prothrombin time greater than 15 seconds, serum creatinine above 1.3 mg/dl, and a liver weight less than 2.5% of body weight. These patients usually had advanced disease, indicating the need for earlier treatment.
REHABILITATION AFTER TRANSPLANTATION
Of our 194 patients, 145 (74.7%) are currently alive. Of these, we have accurate follow-up data on rehabilitation in 129: One hundred twelve patients (86.8%) enjoy full activity. Eleven patients (8.5%) have a somewhat restricted activity. The cause of the partial disability is bone disease in nine, manifested either as frequent bone fractures or as severe back pain, and in two hypertention and renal disease. Five patients (3.9%) are homebound. In two this is due to renal failure, probably a complication of cyclosporine; two are still recovering from transplantation; and one is recovering from a recent colon resection.
One patient (0.8%) is currently hospitalized, awaiting retransplantation.
TECHNICAL PROBLEMS PARTICULAR TO LIVER TRANSPLANTATION FOR PRIMARY BILIARY CIRRHOSIS
PBC is generally a disease regarded with special favor by liver transplant surgeons because transplantation is technically easy, particularly in the absence of previous upper abdominal surgery.
Special care is required for the arterialization of the new Ii ver, because a high incidence of intimal dissection ofthe common hepatic artery has been observed.22 If this occurs, alternate sites such as the celiac axis or aorta should be used.23
ROLE OF RETRANSPLANTATION
Liver transplantation is occasionally followed by potentially fatal complications. The salvage role of retransplantation in this setting cannot be overemphasized.24
In our series of 194 patients studied, 39 (20.1%) required retransplantation and six required a third transplant (3%). Of the retransplantations, 31 (79%) were perfornled during the first month after the original implantation. The causes for retransplantation are shown in the Table 3. Overall survival after retransplantation was 38.4%. Survival after the third transplantation was 16.7% (one of six). Complete recovery was possible in 14 (87.5%) of the 16 survivors. Two patients are homebound; one patient has marginal renal function, and the second patient is temporarily disabled due to a recent colon resection.
TABLE 3.
Cause of Retransplantation in Patients with PBC
| Cause of Retransplantation | No. | % |
|---|---|---|
| Primary liver nonfunction | 10 | 22.3 |
| Hepatic artery thrombosis | 16 | 35.6 |
| Chronic rejection | 9 | 20 |
| Acute rejection | 6 | 13.3 |
| Portal vein thrombosis | 3 | 6.6 |
| Suprahepatic caval stricture | 1 | 2.2 |
EFFECT OF SUCCESSFUL LIVER TRANSPLANTATION ON THE COMPLICATIONS OF PRIMARY BILIARY CIRRHOSIS
Encephalopathy
This is usually reversed within hours after termination of anesthesia; occasionally, a longer period is required, depending on its degree and the early function of the graft. In fact, the mental condition of the patient immediately postoperatively is one of the best available indicators of graft function.
Pruritus
Pruritus disappears promptly after liver transplantation.
Jaundice
Fast reversal of jaundice is a reliable sign of good early graft function. It fades away completely, usually within 1 to 2 weeks, depending on its preoperative depth.
Deep skin pigmentation is also reversible but requiring a longer period, as long as a few months.
Skin Xanthomas
Skin xanthomas usually regress completely within a few weeks after transplantation.
Varices and Variceal Bleeding
A healthy liver is a perfect portocaval shunt and dramatically stops variceal bleeding. On a few occasions, we have encountered postoperative variceal bleeding from very large gastric or intestinal varices that have required ligation.
Ascites
Ascites is cured at a rate depending on its preoperative volume and the renal function.
Splenomegaly
Splenomegaly usually regresses within months.25 Immediately postoperatively, the enlarged spleen can be a source of infection, especially if the splenic artery has been ligated during the transplant procedure.
Weight Loss
Weight loss is usually replaced by the problem of weight control, which often occurs with return to good health. Prednisone is a significant contributing factor, although not as notable in the cyclosporine era since less of it is used.
Muscle Wasting
Restoration of the muscle mass can be complete but requires systematic physical therapy. The importance of the patient's motivation cannot be overemphasized in this part of rehabilitation because the effort is usually hampered by the often coexisting osteopathic pains. This bone pathologic condition must be considered during the rehabilitation.
Osteoporosis and Osteomalacia
Back and bone pains frequently regress immediately after transplantation, but improve as recovery proceeds. Severe osteopathy requires a very lengthy rehabilitation, is resistant to treatment, but has been shown to be reversible.26 Calcium and vitamin D supplements are given empirically and the patients are alerted about the risk of fracture. If indicated, braces can be used. Despite all efforts, the pretransplant osteopathy can be a source of long-term disability after transplantation.
TRANSPLANTATION OF MORE THAN ONE ORGAN IN PATIENTS WITH PRIMARY BILIARY CIRRHOSIS
More than one vital organ can be transplanted if necessary. In our series, three patients who underwent liver transplantation for PBC also received a renal allograft: two of them simultaneously and the third patient at 5 years after liver transplantation. The indications for the renal transplantation were nephrotic syndrome, interstitial nephritis, and possible cyclosporine toxicity, respectively. All patients are alive, well, and with normally functioning grafts 2, 3, and 6 years after liver transplantation.
The Cambridge Group have recently reported successful heart, lung, and liver transplantation in a patient with primary pulmonary hypertension and PBC.27 It can be expected that the transplantation of various vital organs in combination will be used increasingly for the treatment of patients with PBC who would not recover with liver transplantation alone.
SUMMARY
Liver transplantation is an effective treatment for PBC. The Pittsburgh experience is reported, with 1- and 5-year survival of 75.62% and 70.71%, respectively. Recurrence of PBC, when it occurs, has not been of clinical significance.
Transplantation markedly improves chances for survival, an advantage that is demonstrable in all of the risk groups. Rehabilitation is achieved after transplantation in approximately 90% of the patients.
Some clinical variables are associated with a poorer outcome and indicate the need for earlier treatment.
Acknowledgments
Supported by Research Grants from the Veterans Administration and Project Grant No. DK29961 from the National Institutes of Health, Bethesda, Maryland.
REFERENCES
- 1.Starzl TE, Marchiro TL, Von Kaulla KN, et al. Homotransplantation of the liver in humans. Surg Gynecol Obstet. 1963;117:659–676. [PMC free article] [PubMed] [Google Scholar]
- 2.Calne RY, Rolles K, White DJG, et al. Cyclosporin A initially as the only immunosuppressant in 34 recipients of cadaveric organs: 32 kidneys, 2 pancreases, and 2 livers. Lancet. 1979;2:1033–1036. doi: 10.1016/s0140-6736(79)92440-1. [DOI] [PubMed] [Google Scholar]
- 3.Starzl TE, Klintmalm GBG, Porter KA, et al. Liver transplantation with use of cyclosporin A and prednisone. N Engl J Med. 1981;305:266–269. doi: 10.1056/NEJM198107303050507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Starzl TE, Weil R, III, Iwatsuki S, et al. The use of cyclosporin A and prednisone in cadaver kidney transplantation. Surg Gynecol Obstet. 1980;151:17–26. [PMC free article] [PubMed] [Google Scholar]
- 5.Starzl TE, Iwatsuki S, Klintmalm G, et al. Liver transplantation, 1980, with particular reference to cyclosporin-A. Transplant Proc. 1981;13:281–285. [PMC free article] [PubMed] [Google Scholar]
- 6.Denmark SW, Shaw BW, Jr, Starzl TE, Griffith BP. Veno-venous bypass without systemic anticoagulation in canine and human liver transplantation. Surg Forum. 1983;34:380–382. [PMC free article] [PubMed] [Google Scholar]
- 7.Griffith BP, Shaw BW, Jr, Hardesty RL, et al. Veno-venous bypass without systemic anticoagulation for transplantation of the human liver. Surg Gynecol Obstet. 1985;160:270–272. [PMC free article] [PubMed] [Google Scholar]
- 8.Shaw BW, Jr, Martin DJ, Marquez JM, et al. The advantage of venous bypass during orthotopic transplantation of the liver. Semin Liver Dis. 1985;5:344–348. doi: 10.1055/s-2008-1040631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Institutes of Health Consensus Development Conference Statement: Liver Transplantation—June 20–23, 1983. Hepatology. 1983;4:107S–110S. [PubMed] [Google Scholar]
- 10.Jamieson NV, Sundberg R, Lindell S, et al. Successful 24 to 30 hour preservation of the canine liver: A preliminary report. Transplant Proc. 1988;20:945–947. [Google Scholar]
- 11.Todo S, Nery J, Yanaga K, et al. Extended preservation of human liver grafts with the UW solution. JAMA. 1989;261:711–714. [PMC free article] [PubMed] [Google Scholar]
- 12.Adler M, Gavaler JS, Duquesnoy R, et al. Relationship between the diagnosis, preoperative evaluation and prognosis after orthotopic liver transplantation. Ann Surg. 1988;208:196–202. doi: 10.1097/00000658-198808000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gordon RD, Shaw BW, Jr, Iwatsuki S, et al. Indications for liver transplantation in the cyclosporine era. Surg Clin North Am. 1985;65:541–556. doi: 10.1016/s0039-6109(16)43939-3. [DOI] [PubMed] [Google Scholar]
- 14.Iwatsuki S, Starzl TE, Todo S, et al. Experience in 1,000 liver transplants under cyclosporine-steroid therapy: A survival report. Transplant Proc. 1988;20:498–504. [PMC free article] [PubMed] [Google Scholar]
- 15.Neuberger J, Portmann D, MacDougall BRD, et al. Recurrence of primary biliary cirrhosis after liver transplantation. N Engl J Med. 1982;306:1–4. doi: 10.1056/NEJM198201073060101. [DOI] [PubMed] [Google Scholar]
- 16.Starzl TE, Iwatsuki S, Van Thiel DH, et al. Evolution of liver transplantation. Hepatology. 1982;2:614–636. doi: 10.1002/hep.1840020516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Demetris AJ, Markus BH, Esquivel C, et al. Pathologic analysis of liver transplantation for primary biliary cirrhosis. Hepatology. 1988;8:939–947. doi: 10.1002/hep.1840080439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Portman B, Wight DGD. Pathology of liver transplantation. In: Calne R, editor. Liver transplantation. 2nd ed. Grune & Stratton; Orlando, FL: 1987. pp. 437–470. excluding rejection. [Google Scholar]
- 19.Nueberger J, Altman DG, Christensen E, et al. Use of a prognostic index in evaluation of liver transplantation for primary biliary cirrhosis. Transplantation. 1986;41:713–716. doi: 10.1097/00007890-198606000-00009. [DOI] [PubMed] [Google Scholar]
- 20.Markus BH, Dickson ER, Grambsch PM, et al. Transplantation improves survival in patients with primary biliary cirrhosis: Comparison of estimated survival based on Mayo model and actual survival in the Pittsburgh transplant population. In preparation. [Google Scholar]
- 21.Starzl TE, Todo S, Gordon R, et al. Liver transplantation in older patients. N Engl J Med. 1987;316:484–485. doi: 10.1056/NEJM198702193160814. Letter. [DOI] [PubMed] [Google Scholar]
- 22.Esquivel CO, Van Thiel DH, Demetris AJ, et al. Transplantation for primary biliary cirrhosis. Gastroenterology. 1988;94:1207–1216. doi: 10.1016/0016-5085(88)90014-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shaw BW, Jr, Iwatsuki S, Starzl TE. Alternative methods of arterialization of the hepatic graft. Surg Gynecol Obstet. 1984;159:490–493. [PMC free article] [PubMed] [Google Scholar]
- 24.Shaw BW, Jr, Gordon RD, Iwatsuki S, Starzl TE. Hepatic retransplantation. Transplant Proc. 1985;17:264–271. [PMC free article] [PubMed] [Google Scholar]
- 25.Yanaga K, Tzakis A, Shimada M, et al. Reversal of hypersplenism after liver transplantation. Ann Surg. doi: 10.1097/00000658-198908000-00007. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weaver GZ, Franck WA, Streck WF, Starzl TE. Hepatic ostedystrophy after liver transplantation in patients with primary biliary cirrhosis. Am J Gastroenterology. 1983;78:102–106. [PubMed] [Google Scholar]
- 27.Wallwork J, Williams R, Calne RY. Transplantation of liver, heart, and lungs for primary biliary cirrhosis and primary pulmonary hypertension. Lancet. 1987:182–184. doi: 10.1016/s0140-6736(87)90765-3. [DOI] [PubMed] [Google Scholar]


