Abstract
INTRODUCTION AND AIMS
To explore the association between primary care professionals’ (PCPs) attitudes towards unhealthy alcohol and other drug (AOD) use (from risky use through dependence) and readiness to implement AOD-related preventive care.
DESIGN AND METHODS
PCPs from 5 health centers in Sao Paulo were invited to complete a questionnaire about preventive care and attitudes about people with unhealthy AOD use. Logistic regression models tested the association between professional satisfaction and readiness. Multiple Correspondence Analysis (MCA) assessed associations between stigmatizing attitudes and readiness.
RESULTS
Of 160 PCPs surveyed, 96 (60%) completed the questionnaire. Only 25% reported implementing unhealthy AOD use clinical prevention practices; and 53% did not feel ready to implement such practices. Greater satisfaction when working with people with AOD problems was significantly associated with readiness to implement AOD-related preventive care. In MCA two groups emerged: 1. PCPs ready to work with people with unhealthy AOD use, who attributed to such patients lower levels of dangerousness, blame for their condition and need for segregation from the community (suggesting less stigmatizing attitudes); 2. PCPs not ready to work with people with unhealthy AOD use, who attributed to them higher levels of dangerousness, blame, perceived level of patient control over their condition, and segregation (suggesting more stigmatizing attitudes).
DISCUSSION AND CONCLUSIONS
More stigmatizing attitudes towards people with unhealthy AOD use are associated with less readiness to implement unhealthy AOD-related preventive care. Understanding these issues is likely essential to facilitating implementation of preventive care, such as screening and brief intervention, for unhealthy AOD use.
Keywords: Alcohol, Drugs, Primary Health Care, Attitudes, Stigma
Introduction
The use of alcohol and other drugs (AOD) can be perceived as positive or negative depending on many factors. In many situations alcohol use is associated with prestigious activities and social status. On the other hand, the use of illegal drugs and the way some substances are used seems to attract stigma, marginalization, and negative emotional reactions (1–3).
AOD-related attitudes may develop from and impact people’s personal and professional experiences and behaviors. Attitude is a hypothetical construct that represents the person’s perspective (positive or negative) toward a specified target (person, place, thing or event). Attitudes are generally defined as being composed of three components: cognitive (beliefs), affective (emotions) and behavioral (verbal or typical behavioral tendency). The three components are interlinked and negative beliefs, for example, seem to be associated with stigmatizing attitudes (4). Link and Phelan (5), defined stigma as the co-occurrence of labeling, stereotyping, separation, status loss and discrimination. Wainer and colleagues (6) apply the attribution theory to understand the perceived cause of stigma. According to this theory, attributions of responsibility will determine affective reactions towards the stigmatized person (e.g. anger or pity), future expectations regarding the individual (e.g. likelihood of recovery), and a variety of behavioral responses, including altruistic actions (7).
Health professionals’ negative attitudes, particularly about AOD use, have been cited as important barriers to the implementation of clinical prevention practices (8–10). Some health professionals consider AOD-related problems difficult issues to discuss, and many report a lack of skills, confidence, satisfaction and competence to identify and manage these problems (11–13). Ronzani et al (14) pointed out that unhealthy AOD use (the spectrum from risky use through dependence) was the most negatively judged behavior by health professionals when compared to other health conditions such as Hansen’s disease, obesity, HIV and others.
In order to reach a broad range of people for early intervention, decrease stigma and improve attitudes and care, many have advocated addressing unhealthy AOD use in primary health care (PHC) settings (12, 15 16), where the focus is on prevention, health promotion and longitudinal comprehensive care. This laudable goal has the potential to make addressing unhealthy AOD use a mainstream health issue and risk behavior, managed like others addressed routinely in these settings. However, few studies about health professionals’ attitudes related to unhealthy AOD use have examined the association between them and the professional’s clinical prevention practices. The present study aimed to explore the association between primary care professionals’ (PCP) attitudes about people with unhealthy AOD use (including stigma) and PCPs’ readiness to implement AOD clinical prevention practices. We anticipated that negative attitudes about people with unhealthy AOD use would influence PCPs’ readiness to implement AOD-related preventive care; and that PCPs’ satisfaction when working with people with unhealthy AOD use would be associated with readiness to implement AOD-related preventive care.
Methods
Study Sample
Physicians, nurses, nursing assistants and community health workers1 from 5 PHC centers in Sao Paulo, Brazil, were invited to participate in the study. These centers were randomly selected from 222 centers in total, one center from each of the city’s regions - North, South, Southeast, Center-west and East. All the health professionals from each center were invited to participate (n=160) and 96 completed the survey, giving a response rate of 60%. The participants were physicians or nurses (31%), nursing assistants (19%) and community health workers (50%).
As regards socio-demographic characteristics, 87% were women, 60% single, mean age 40.6 (SD 9.7); 49% were Catholic, 25% Protestant, 24% had other religions or did not have a religion.
Data Collection
The first step was to present the study to the primary care unit managers. They were responsible for inviting all the health professionals in the unit to participate. Before agreeing to participate, professionals were told about the aims of the project and informed about the confidentiality of the data (it was an anonymous survey), were asked to sign informed consent and instructed about how to complete the questionnaire. All participants received the questionnaire in an envelope. The researcher waited outside of the room to receive the envelope containing the completed survey, or in some cases, returned to the health center to pick it up on another day.
Instrument
The instrument was composed of three parts. The first part was a questionnaire developed by the authors, with multiple response options: socio-demographic data, clinical prevention practices, beliefs about unhealthy AOD use, satisfaction when working with people with AOD problems and readiness to implement preventive interventions with people with risky AOD use (2 items, one for alcohol, one for drugs) (“On a scale of one to five, where 1 means not even a little ready, and 5 totally ready, how ready do you feel to carry out preventive interventions for risky alcohol/drug use?”). For the questions about beliefs, satisfaction and readiness Likert scales ranging from 1–5 were used. AOD-related preventive care was defined as any type of screening or intervention done in the primary care setting studied. The second questionnaire was an adaptation made by the authors of the Attribution Questionnaire Short Form (3, 17), a stigma measure. The Adapted version of the Attribution Questionnaire (AAQ) addressed health professionals’ attributions for different health conditions represented by hypothetical vignettes about people with: 1. Risky alcohol use; 2. Alcohol abuse; 3. Alcohol dependence; 4. Drug dependence; 5. Hypertension; 6. Depression; 7. Schizophrenia; 8. HIV-AIDS. Participants were instructed to read the eight vignettes and score nine different items: pity for the patient, dangerousness of the patient, fear of the patient, blame (patient is responsible for his condition), segregation (would be better for the community for the patient to be removed from it for treatment), anger (about or towards the patient), likelihood that the professional would help the patient, avoidance (of taking care of the patient) and control (how much the patients have control over for the solutions of their problems), on a 9-point agreement scale ranging from none/a little (1) to a lot (9). The “help” item was reverse-coded. Internal consistency (Cronbach’s alpha) for each factor was tested: pity: 0.89; dangerousness: 0.77; fear: 0.72; blame: 0.65; segregation: 0.82; anger: 0.77; help: 0.83; avoidance: 0.71; and control: 0.72. We added a final question across the 8 vignettes to assess PCPs’ opinions about each health condition: “If you were this person, how would you define your health condition? From 1 (very bad health) to 10 (very good health).” Each vignette was developed considering PCPs’ daily practice, including health conditions typically associated with stigma and others which were not expected to be associated with stigma.
The last part of the instrument was the ASSIST (Alcohol, Smoking and Substance Involvement Screening Test) (18 – 20) aiming to evaluate the PCPs’ AOD use. The ASSIST score categorizes respondents as low risk/no use (should receive information), moderate risk (should receive a brief intervention) and high risk (should receive more intensive care).
Statistical Analysis
The Pearson X2 test was applied to assess the association between categorical independent variables and readiness to implement AOD clinical prevention practices. In logistic regression models, we tested the association between satisfaction when working with people with unhealthy AOD use and readiness to implement AOD-related preventive care. Satisfaction was categorized as “none” (1+2), “some” (3) and “a great deal” (4+5) and readiness was coded as a binary variable (not ready (1–3) vs. ready (4+5)). P<0.05 was considered statistically significant.
Non-parametric analyses using median regression, with bootstrap estimation were used to compare the participants’ opinion about each health condition of the vignettes. Multiple Correspondence Analysis (MCA) was used to assess patterns of associations among the items in the AAQ (medians) and readiness to implement AOD clinical prevention practices (binary). MCA is an exploratory technique (not inferential) that is a generalization of a principal component analysis for categorical variables. This approach allows testing each difference among groups. Its interpretation can be based upon proximities between points in a low dimensional map, where the axes are the coordinates, the geometric figures represent the different variables in the model, and the proximities reflect the strength of associations (21).
Ethics
All the study procedures were approved by the Ethics Committee of the Universidade Federal de São Paulo, project number CEP1581/07.
Results
Over half (56%) of the 96 respondents reported always or almost always implementing general health clinical prevention practices, but only 25% reported implementing clinical prevention practices targeting unhealthy AOD use; 53% felt only a little or not at all ready to implement clinical prevention practices for unhealthy AOD use. In spite of that, the majority expressed positive beliefs about working with people with unhealthy AOD use, even though around 60% reported not having adequate training to do so. Sixty eight percent of the respondents believed that their amount of work would increase if they start to identify unhealthy AOD use in their clinical routine.
Based on the ASSIST questionnaire, 6.2% of the PCPs used alcohol and 14.6% used tobacco at moderate risk levels for which receipt of a brief counseling intervention would be appropriate. One used alcohol at a high risk level. None used drugs. Alcohol and tobacco risk levels were not significantly associated with readiness to implement AOD preventive care for patients with risky use. The proportion ready to implement alcohol preventive care was 24% of those at lower tobacco risk, 43% for moderate risk, and 25% of never smokers; 28% of those at lower alcohol risk, 17% for moderate risk, and 25% of never drinkers. The proportion ready to implement drug preventive care was 22% of those at lower tobacco risk, 36% for moderate risk, and 25% of never smokers; 25% of those are lower alcohol risk, 17% for moderate risk, and 25% of never drinkers.
Greater professional satisfaction when working with people with AOD problems was significantly associated with readiness to implement AOD-related preventive care (Tables 1 and 2). For example, compared with none, having a great deal of professional satisfaction when working with people with alcohol problems increased the odds of readiness to carry out preventive interventions for risky use 6.2 times and the odds of readiness to carry out drug preventive interventions 10.6 times.
Table 1.
Association between: satisfaction and readiness to carry out interventions for risky alcohol use
| OR (95% CI) | ||
|---|---|---|
| Satisfaction when working with people with unhealthy alcohol use | None | 1.0 |
| Some | 4.8 (0.9–26.2) | |
| A great deal | 6.2 (1.6–23.4) | |
| Satisfaction when working with people with unhealthy drug use | None | - |
| Some | 5.0 (1.0–24.1) | |
| A great deal | 12.0 (3.1–46.6) |
CI = Confidence interval OR = odds ratio
Table 2.
Association between: satisfaction and readiness to carry out interventions for drug use
| OR (95% CI) | ||
|---|---|---|
| Satisfaction when working with people with unhealthy alcohol use | None | 1.0 |
| Some | 1.4 (0.1–16.6) | |
| A great deal | 10.6 (2.2–49.6) | |
| Satisfaction when working with people with unhealthy drug use | None | 1.0 |
| Some | 4.0 (0.6–26.3) | |
| A great deal | 18.5 (3.8–89.2) |
CI = Confidence interval OR = odds ratio
We did not find statistically significant differences between professional categories and readiness to implement AOD-related preventive care. For physicians/nurses, nursing assistants and community health workers 37%, 22%, and 23%, respectively, were ready to implement alcohol preventive care; similarly, 30%, 22%, and 21%, respectively, were ready to implement drug preventive care.
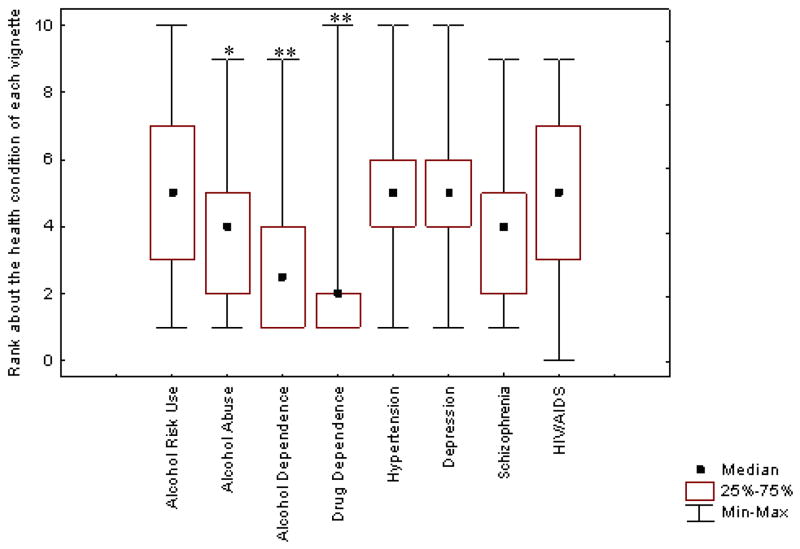
PCPs rated drug-dependence, alcohol-dependence, and alcohol abuse as conditions representing worse health than HIV-AIDS, depression, hypertension and schizophrenia (overall p<0.01 except for schizophrenia)(Figure 1).
Figure 1.
PCPs rating of the health condition presented in each vignette (from very bad (0) to very good (10) health) (overall p<0.01)
* Alcohol abuse rating differs significantly from all other ratings (p<0.01) except Schizophrenia
** Alcohol and drug dependence ratings differ significantly (p<0.05) from all others
The Multiple Correspondence Analysis (MCA) suggested two distinct groups - PCP’s that feel ready to carry out preventive interventions for risky AOD use and PCPs that do not (Figure 2). Two patterns of associations between AAQ attitudes and readiness emerged: 1. Professionals ready to carry out preventive interventions for risky AOD use, who attributed lower levels of dangerousness, blame (patient is responsible for his condition) and segregation (would be better for the community for the patient to be removed from it for treatment) to such patients (suggesting less stigmatizing attitudes). 2. Professionals not ready to carry out preventive interventions for risky AOD use, who attributed higher levels of dangerousness, blame, control (how much the patient has for the solutions of his problems) and segregation to such patients (suggesting more stigmatizing attitudes). Also, within the group of PCPs that do not feel ready, there appear to be two subgroups: those who attribute higher levels of dangerousness and segregation, and those who attribute higher levels of blame and control.
Figure 2.
Multiple correspondence analysis (MCA) map of the associations between the items in the Adapted Attribution Questionnaire (AAQ) and primary care professionals’ readiness to implement alcohol and other drug (AOD) clinical prevention practices.
Footnote:
Different color geometric figures represent the different variables in the model that are significantly associated with readiness, and the proximities reflect the strength of associations. Vignette conditions: AR = risky alcohol use; AA = alcohol abuse; AD = alcohol dependence; DD = drug dependence. Not ready/Ready = to carry out preventive interventions for risky alcohol/drug use. Control, danger(ousness), segreg(ation), and blame are items from the AAQ addressing stigmatizing attitudes.
Discussion
The aim of this study was to explore the association between PCPs’ attitudes about unhealthy AOD use and their readiness to implement AOD-related preventive care. Our key findings suggest that health professionals’ attitudes appear to influence clinical practices, at least self-reported practices, with more stigmatizing attitudes associated with lower readiness to implement unhealthy AOD-related preventive care. Moreover, PCPs who endorsed more negative attitudes were also the ones that attributed more blame (responsibility for causing the problem) and control (for the solutions of the problem) to patients with unhealthy AOD use. These findings are consistent with Weiner and colleagues attributional theoretical framework (6) and confirm other findings in the literature (3, 13).
Health professionals’ satisfaction when working with people with unhealthy AOD use was associated with their readiness to implement AOD-related preventive care. In the same direction, Saitz and colleagues (11) showed that health professionals’ greater satisfaction caring for patients with substance problems was associated with positive attitudes toward addiction treatment.
Previous research has found that health professionals tend to be positive about working with people with unhealthy AOD use (12, 15), however this seems to be more associated with a sense of professional responsibility, rather than personal interest, since at the same time, they tend to report low levels of professional satisfaction when working with this population. This discrepancy between perceived role responsibility and other attitudes and satisfaction seems to be even more evident for professionals’ views regarding people with unhealthy drug use in particular, as this study also showed. The illegal status of these substances can reinforce stereotypes of dangerousness, creating safety concerns among health professionals (22–24), leading to discrimination against the patient, and poor quality of care (25).
The present study has some limitations. Causality cannot be determined from a cross-sectional survey. We assessed readiness to implement AOD-related preventive care, not actual implementation of practices, and similarly, instead of observing actual practice with patients, we used vignettes of hypothetical cases that may or may not reflect how health professionals would feel or respond in real situations. Social desirability may also have biased PCPs’ responses towards more positive attitudes. On the other hand, the fact that PCPs did report substantial lack of readiness and negative attitudes suggests otherwise. In addition, the fact that the survey was anonymous likely minimized these biases. Results may be affected by the non-response (40%) rate; however, this response rate is similar to that seen often in surveys with health professionals (23). The generalizability of this study may be limited as this is a relatively small sample, from one city in Brazil. However, at a minimum the results likely apply to the many health centers in São Paulo, and other urban centers in Brazil. Also, since the findings seem consistent with studies done in other countries (9, 12, 15), there is little reason to suspect that the findings would differ if the study were repeated elsewhere.
Despite the study limitations, the findings have important practical implications. We found an association between attitudes, including stigmatizing attitudes, and clinicians’ readiness to implement AOD-related preventive care. This association suggests that the way unhealthy AOD use is perceived by PCPs has implications for the relationship between the patient and clinician, and for the quality of care they receive. The development of positive attitudes and practices among health professionals in regard to AOD-related work must involve interventions that go beyond the individual (26, 27). Training and education are good strategies that are necessary, but are not sufficient to change health professionals’ attitudes and practices. Yet knowing that attitudes are important in determining practices suggests avenues for change and improvement of care. Multifaceted approaches including education, training, practice guidelines, systems approaches, policy changes and even attention to societal norms may improve PCP’s attitudes and have substantial impact on patient care. Efforts in these areas should be pursued and studied to improve the care of primary care patients with unhealthy alcohol and other drug use.
Acknowledgments
We thank to Fernando Colugnati for the statistical analysis and manuscript review.
Michaela Bitarello do Amaral-Sabadini (MB Amaral-Sabadini) had financial support from: FAPESP - Fundação de Amparo a Pesquisa do Estado de São Paulo - Brazil (Doctoral Scholarship - Process number: #2007/07368-2) and from CAPES - Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brazil (Scholarship - Process number: # 0389099).
Footnotes
Place where the work was undertaken: Department of Psychobiology, Universidade Federal de São Paulo (Federal University of São Paulo - UNIFESP), Brazil.
This study was presented in abstract (poster) form at the INEBRIA Meeting (International Network on Brief Interventions for Alcohol Problems), 8th and 9th October 2009, Newcastle Gateshead (England).
Community Health Workers are people from the community where the health center is located, trained and hired to work on community health activities, such as screening and education about health issues.
Contributor Information
Michaela Bitarello do Amaral-Sabadini, Department of Psychobiology, Federal University of Sao Paulo, Brazil
Richard Saitz, Clinical Addiction Research and Education (CARE) Unit, Section of General Internal Medicine, Department of Medicine, Boston Medical Center and Boston University School of Medicine; Department of Epidemiology, Boston University School of Public Health, Boston, USA.
Maria Lucia O. Souza-Formigoni, Department of Psychobiology, Federal University of São Paulo, Brazil
References
- 1.Heatherton TF, Kleck RE, Hebl MR, Hull JG. The social psychology of stigma. New York: The Guilford Press; 2003. [Google Scholar]
- 2.Room R. Stigma, social inequality and alcohol and drug use. Drug Alcohol Rev. 2005;24:143–155. doi: 10.1080/09595230500102434. [DOI] [PubMed] [Google Scholar]
- 3.Corrigan PW, Lurie BD, Goldman HH, Slopen N, Medasani K, Phelan S. How adolescents perceive the stigma of mental illness and alcohol abuse. Psychiatric Services. 2005;56(5):544–550. doi: 10.1176/appi.ps.56.5.544. [DOI] [PubMed] [Google Scholar]
- 4.Gilbert DT, Fiske ST, Lindzey G. The handbook of social psychology. 4. New York: Oxford University Press; 1998. [Google Scholar]
- 5.Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol. 2001;27:363–85. [Google Scholar]
- 6.Weiner B. Social motivation, justice, and the moral emotions - An attributional approach. Mahwah, New Jersey: Lawrence Erlbaum Associates; 2006. [Google Scholar]
- 7.Corrigan PW, Markowitz FE, Watson AC, Rowan D, Kubiak MA. An attribution model of public discrimination towards persons with mental illness. J Health Soc Behav. 2003;44(2):162–79. [PubMed] [Google Scholar]
- 8.Palm J. The nature of and responsibility for alcohol and drugs problems: views among treatment staff. Addict Res Theory. 2004;12 (5):413–431. [Google Scholar]
- 9.McCormick KA, Cochran NE, Back AL, Merrill JO, Williams EC, Bradley KA. How primary care providers talk to patients about alcohol - A qualitative study. J Gen Intern Med. 2006;21:966–972. doi: 10.1111/j.1525-1497.2006.00490.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Amaral MB, Ronzani TM, Souza-Formigoni MLO. Process evaluation of the implementation of a screening and brief intervention program for alcohol risk in primary health care: An experience in Brazil. Drug Alcohol Rev. doi: 10.1111/j.1465-3362.2009.00120.x. in press. [DOI] [PubMed] [Google Scholar]
- 11.Saitz R, Friedman PD, Sullivan LM, et al. Professional satisfaction experienced when caring for substance-abusing patients - Faculty and resident physicians perspectives. J Gen Intern Med. 2002;17:373–376. doi: 10.1046/j.1525-1497.2002.10520.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anderson P, Kaner E, Wutzke S, Wensing M, Grol R, Heather N. Attitudes and management of alcohol problems in general practice: Descriptive analysis based on findings of a World Health Organization international collaborative survey. Alcohol Alcsm. 2003;38(6):597–601. doi: 10.1093/alcalc/agg119. [DOI] [PubMed] [Google Scholar]
- 13.Ronzani TM, Amaral MB, Souza-Formigoni MLO, Babor TF. Evaluation of a training program to implement alcohol screening, brief intervention and referral to treatment in primary health care in Minas Gerais, Brazil. Nordic Studies on Alcohol and Drugs. 2008;25:529–538. [Google Scholar]
- 14.Ronzani TM, Higgins-Biddle J, Furtado EF. Stigmatization of alcohol and other drug users by primary care providers in Southeast Brazil. Social Science & Medicine. 2009:1–5. doi: 10.1016/j.socscimed.2009.07.026. [DOI] [PubMed] [Google Scholar]
- 15.Aira M, Kauhanen J, Larivaara P, Rautio P. Factors influencing inquiry about patient’s alcohol consumption by primary health care physicians: qualitative semi-structured interview study. Family Practice. 2003;20(3):270–275. doi: 10.1093/fampra/cmg307. [DOI] [PubMed] [Google Scholar]
- 16.WHO (World Health Organization) & Wonca (World Organization of Family Doctors) Report. Integrating mental health into primary care - A global perspective. 2008. [Google Scholar]
- 17.Brown SA. Factors and Measurement of Mental Illness Stigma: A Psychometric examination of the attribution questionnaire. Psychiatric Rehabilitation Journal. 2008;32(2):89–94. doi: 10.2975/32.2.2008.89.94. [DOI] [PubMed] [Google Scholar]
- 18.WHO - World Health Organization. [Accessed in 03/05/2008];The ASSIST project - Alcohol, Smoking and Substance Involvement Screening Test. http://www.who.int/substance_abuse/activities/assist_portuguese.pdf.
- 19.WHO ASSIST Working Group. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility. Addiction. 2002;97(9):1183–1194. doi: 10.1046/j.1360-0443.2002.00185.x. [DOI] [PubMed] [Google Scholar]
- 20.Humeniuk R, Ali R, Babor TF, Farrell M, Formigoni ML, Jittiwutikarn J, de Lacerda RB, Ling W, Marsden J, Monteiro M, Nhiwatiwa S, Pal H, Poznyak V, Simon S. Validation of the Alcohol, Smoking And Substance Involvement Screening Test (ASSIST) Addiction. 2008;103(6):1039–47. doi: 10.1111/j.1360-0443.2007.02114.x. [DOI] [PubMed] [Google Scholar]
- 21.Panagiotakos DB, Pitsavos C. Interpretation of epidemiological data using multiple correspondence analysis and log-linear models. Journal of Data Science. 2004;2:75–86. [Google Scholar]
- 22.McKeown A, Matheson C, Bond C. A qualitative study of GPs’ attitudes to drug misusers and drug misuse services in primary care. Family Practice. 2003;20(2):120–125. doi: 10.1093/fampra/20.2.120. [DOI] [PubMed] [Google Scholar]
- 23.Ding L, Landen B, Wilson I, Wong M, Shapiro M, Cleary P. Predictors and consequences of negative physician attitudes toward HIV infected injection drug users. Arch Intern Med. 2005;165:618–623. doi: 10.1001/archinte.165.6.618. [DOI] [PubMed] [Google Scholar]
- 24.Fortney J, Mukherjee S, Curran G, Fortney S, Han X, Booth B. Factors Associated With Perceived Stigma for Alcohol Use and Treatment Among At-Risk Drinkers. The Journal of Behavioral Health Services & Research. 2004;31:418–429. doi: 10.1007/BF02287693. [DOI] [PubMed] [Google Scholar]
- 25.Yokaichiya CM, Figueredo WS, Schraiber LB. Injecting drug users and antiretroviral therapy: perceptions of pharmacy teams. Rev Saude Publica. 2007;41(2):14–21. doi: 10.1590/s0034-89102007000900005. [DOI] [PubMed] [Google Scholar]
- 26.Skinner N, Roche AM, Freeman T, Mckinnon A. Health professionals’ attitudes towards AOD-related work: Moving the traditional focus from education and training to organizational culture. Drugs: Education, Prevention and Ppolicy. 2009;16(3):232–249. [Google Scholar]
- 27.Pavin T, Duarte P, Souza-Formigoni ML. Predictors of the implementation of SBI by health professionals trained by SUPERA course twenty months before. [Accessed in: 20/11/2009]; www.inebria.net/Du14/html/en/dir1338/doc17833.htm.