Abstract
Subject matter experts systematically reviewed evidence on the effectiveness of housing interventions that affect safety and injury outcomes, such as falls, fire-related injuries, burns and drowning, carbon monoxide poisoning, heat-related deaths, and noise-related harm, associated with structural housing deficiencies. Structural deficiencies were defined as those deficiencies for which a builder, landlord, or homeowner would take responsibility (ie, design, construction, installation, repair, monitoring). Three of the 17 interventions reviewed had sufficient evidence for implementation: installed, working smoke alarms; 4-sided isolation pool fencing; and preset safe hot water temperature. Five interventions needed more field evaluation, 8 needed formative research, and 1 was found to be ineffective. This evidence review shows that housing improvements are likely to help reduce burns and scalds, drowning in pools, and fire-related deaths and injuries.
Keywords: burns, drowning, falls, fires, housing, injury, prevention, scalds
Residential injuries result in thousands of deaths and millions of emergency department visits each year. In 2003, one-third of all injury-related deaths resulted from home injuries.1 The rates of unintentional home injury death are highest in the youngest and oldest age groups.2,3 For infants, children, and young adults aged 0 to 19 years, at least 55% of unintentional deaths (excluding motor vehicle crashes) occur in the home.4–6 Overall, preventable, unintentional residential injuries in US children younger than 19 years result in more than 4 million visits to US emergency departments and 74 000 hospitalizations each year.5,6 For adults 65 years and older, home injuries result in more than 7000 deaths and 1.7 million emergency department visits each year in the United States.7 Structural and other deficiencies in housing are important causes of fatal and nonfatal injuries and involve factors related to construction, design, installation, and lack of monitoring or maintenance.
Falls
Falls account for 45% of all injuries in the home that require medical attention.3 Among persons 65 years and older, 60% of falls resulting in emergency department visits occurred at home.8 Structural residential hazards, such as stairs in disrepair, lack of adequate handrails, lack of grab bars, and nonslip surfaces in the bathroom, tripping or slipping hazards, such as slippery flooring, and inadequate lighting may lead to falls in older adults, depending on their physical abilities and risk-taking behaviors.9,10
Falls also are a major cause of nonfatal injury in children 18 years and younger and result in an estimated 2.7 million emergency department visits each year.11 Fall hazards include a lack of stairway safety gates and window guards, uncarpeted or concrete floors, missing or damaged window locks or catches, structural defects (eg, inadequate spacing and height of steps and railings), and insufficient lighting over stairs and in other areas.12–14
Fire-Related Injuries
In 2006, US Fire Departments responded to 412 500 residential fires that resulted in 2580 deaths, 12 925 injuries, and nearly $7 billion in property damage.15 Most fire-related fatalities are due to smoke inhalation or toxic gases.16 Groups at increased risk of fire-related injury and death include persons younger than 45 years and older than 74 years, African Americans, Native Americans, low-income Americans, rural residents, and occupants of manufactured (ie, mobile) homes and substandard housing.1,17–19 Fire-related injury hazards include the lack of functional smoke alarms near or inside bedrooms and on every floor of a house, lack of adequate escape routes (eg, egress windows), and sources of fire ignition such as faulty wiring, defective appliances, misuse and poor maintenance of electrical appliances, lack of arc fault circuit interrupters (AFCIs),* and overloaded circuits and extension cords.18,20–26
Scald-Related Injuries
In 1997, an estimated 12 400 children received scald burns, nearly a quarter of which were caused by hot tap water, most commonly in the bathtub or shower and also in the kitchen of bathroom sink.27 Most scald-related deaths occur in children younger than 4 years.28,29 Other high-risk groups include older persons and persons with physical or mental disabilities.20 Scalds are associated with the lack of antiscald devices for showerheads and faucets, and water heater thermostats that are set above 120°F.20
Drowning
An average of 823 unintentional drowning deaths occur in or on home premises each year.19 Drowning has been defined as “the process of experiencing respiratory impairment from submersion/immersion in liquid.”30 In 2001–2002, nonfatal and fatal drowning rates were highest for children 4 years or younger.31 In 2006, for every child younger than 15 years who died from drowning, 5 children received emergency department care for nonfatal submersion injuries, which can result in brain damage and long-term disability.32 Among children younger than 5 years, 50% of fatal drownings and more than 80% of nonfatal drownings occur in swimming pools31 and are associated with lack of barriers (eg, having an unfenced or uncovered swimming pool)33,34 and door or pool alarms.35
Carbon Monoxide Poisoning
Carbon monoxide (CO) exposure causes approximately 450 deaths and more than 15 000 emergency department visits annually; 64% of these occur in the home.36 High levels of CO can cause unconsciousness, long-term neurological disabilities, coma, cardiorespiratory failure, and death.37 Long-term low-level exposure can cause viral-like symptoms, such as fatigue, dizziness, headache, and disorientation.38,39
Heat-Related Mortality
Residents unable to keep cool during very hot weather can experience serious illness and death. During 1999–2003, a total of 3 442 deaths from heat exposure were reported (annual mean = 688) in the United States.40 During heat waves, mortality is most prevalent among older persons, the socially isolated, and those people living in homes without air-conditioning.41
Noise
Excessive noise levels may result in sleep disturbances, cardiovascular and psychophysiological problems, performance reduction, increased annoyance responses, adverse social behavior, and, at very high levels, hearing loss.42 Noise exposure disproportionately affects low-income communities and families,43–46 which more commonly reside near airports, railroad yards, highways, and other sources of high-noise levels. Living in crowded neighborhoods and substandard or poorly designed homes has also been associated with increased noise in homes.47
Interventions Reviewed
The literature search and review methods are described in more detail in the companion article of Jacobs et al48 in this series. Briefly, content experts were invited to serve on a panel to review scientific evidence on housing deficiencies that can result in injuries. Relevant literature was identified and provided to the panel by a team from the Centers for Disease Control and Prevention and the National Center for Healthy Housing, which determined the topics to be reviewed after preliminary searches. The interventions identified from the literature were to some extent dependent upon the search terms used. The panel (C.D. [Chair], K.J.P., A.M., and D.O.), with D.E.J., comprising experts representing academic and nongovernmental organizations, reviewed the evidence (see www.nchh.org for details of how each study was rated), provided and reviewed additional relevant literature, and prepared a preliminary report on which this article is based (www.nchh.org/LinkClick.aspx?fileticket=2lvaEDNBIdU%3d&tabid=229).
This review includes structural deficiencies, monitoring to identify structural deficiencies (eg, CO detectors), and those behavior changes specifically intended to correct structural deficiencies or increase monitoring. Structural deficiencies are defined as those deficiencies for which a builder, landlord, or homeowner would take responsibility (ie, design, construction, installation, repair, monitoring). Although home injuries often involve the complex interplay of structural hazards with human biology, psychology, and behavior, this review focuses primarily on modifications to the built environment that require limited if any behavioral change on the part of occupants. The review thus excludes many behaviors that household residents might implement to improve home safety, such as safely storing poisons, matches, or firearms; affixing loose rugs; and purchasing nonslip bath-mats. The review of evidence did not involve human subjects.
For each intervention identified, the panel of subject matter experts considered evidence regarding the efficacy of the intervention itself (ie, whether it, when correctly implemented, was efficacious in reducing injury). The panel also considered the effectiveness of methods to increase implementation, such as legislation, regulation (eg, building codes), device distribution and installation programs, and home- and community-based education. The panel recognizes that “home- or community-based education” in this context encompasses a wide range of interventions, varying in mode of delivery, content, and target audience. However, the emphasis in this review is on passive interventions rather than educational programs to enhance behavior change. The interested reader is therefore referred to the specific research publications cited to learn more about the precise educational interventions evaluated and their relative effectiveness in yielding behavioral change.
The panel placed the greatest weight on evidence from well-conducted, comprehensive systematic reviews of the literature but also included evidence from well-conducted controlled trials and observational studies. For each study examined, the panel evaluated the extent to which the magnitude and significance of the outcomes may have been influenced by various effect modifiers and confounding variables. Where particularly salient, variations in effect have been described. However, it is beyond the scope of this article to delineate this information for every study reviewed.
Formative and process evaluation studies, both in the published and unpublished literature, are important in determining knowledge, attitudes, and behaviors underpinning injury control efforts, as well as demonstrating programmatic reach. However, this research was not mined deeply because it rarely yields evidence of program effectiveness.
The following 17 interventions were identified and examined:
smoke alarms, including installation of working smoke alarms and community smoke alarm give-away programs without steps to install them;
safe ignition sources (eg, electrical and heating systems) and ignition source controls;
home modification to improve fire escape (eg, egress windows and doors, exit signage, protected stairways);
automatic fire sprinkler systems;
-
4-sided isolation pool fencing
-
◯
four-sided isolation fencing;
-
◯
three-sided perimeter fencing;
-
◯
pool covers and pool alarms;
safe hot water heater temperatures (preset and reset);
temperature-controlled mixer (water) faucets;
home modifications to prevent falls (eg, installation of stair gates, window guards, handrails, grab bars, improved stair lighting, and safe stair and balcony design);
bathtub design;
stove and stove control design;
carbon monoxide exposure prevention through design, engineering, legislation, and education;
improved enforcement of building and housing codes;
air-conditioning/cooling during heat waves;
noise control measures; and
design of residential construction materials.
Results
Of these 17 interventions, 3 were shown to be effective and are ready for implementation, 5 need more field testing but are promising, 8 need formative research, and 1 is ineffective. In addition, a number of the interventions that have been proven effective or appear promising would also benefit from further formative research to improve design and implementation.
Sufficient evidence
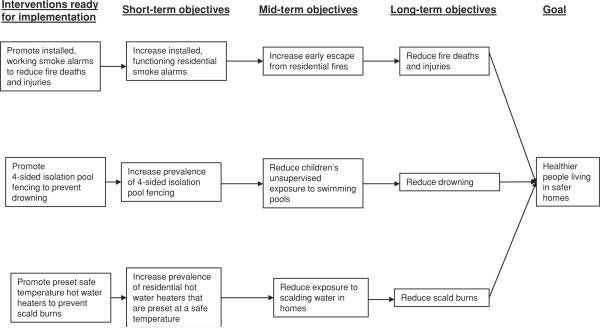
The panel found that 3 of the interventions reviewed—installed, working smoke alarms; 4-sided isolation pool fencing; and preset safe temperature hot water heaters—were supported by sufficient evidence to warrant implementation. The Figure depicts the relationship between these interventions and health outcomes.
FIGURE 1.
Housing Interventions to Control Injury-Related Structural Deficiencies: Interventions Ready for Implementation
Installed, working smoke alarms
Five studies show that working smoke alarms installed in the home reduce death and injuries from residential fires.25,26,49–51 Homes with working smoke alarms have a 40% to 50% lower fire death rate than homes without working smoke alarms.51 Furthermore, 70% of all home fire deaths occurred in homes without working smoke alarms.51
Further investigation is needed to determine the most effective method(s) of increasing the presence of working smoke alarms in the home. Two implementation methods that appear promising but require field testing are (1) community-based installation of smoke alarms, with education, in high-risk homes and (2) building codes or legislation, or both, that requires smoke alarms. Furthermore, an estimated 20% of US homes have smoke alarms present but not working, most commonly due to dead or missing batteries; many of these were disabled because of nuisance alarms.21 Hence, formative research is needed to improve the design of smoke alarms to reduce nuisance alarms and ease maintenance.
The evidence that community-based installation of smoke alarms, combined with education, reduces fire-related injuries in high-risk homes comes from a systematic review that describes 2 relevant trials.52 This review concluded that community-based programs that install free smoke alarms are significantly more effective at increasing the prevalence of installed, working smoke alarms in high-risk homes than community-based programs that give away free smoke alarms without installing them. In addition, one trial found that the incidence of fire-related injuries had been significantly reduced in intervention areas, but not in control areas, after installation of free alarms. However, because of methodological limitations in this trial, the panel recommended further field testing of community-based programs that install free smoke alarms.
The rationale for using building codes and legislation to increase the prevalence of working smoke alarms comes from McLoughlin et al.53 This controlled before-after study53 demonstrated a higher proportion of homes with working smoke alarms and greater reductions in fatal fires and fire deaths in one county after it passed legislation requiring smoke alarms in all homes than a similar county without such legislation. In both counties, homes built after the implementation of building codes requiring smoke alarm installation had more working smoke alarms than homes built before the code was implemented. Confirmation of these findings in other settings, with attention to potential confounding by population differences, is needed.
Four-sided isolation pool fencing
The evidence that 4-sided pool fencing is effective in preventing drowning comes from 3 studies and 1 systematic review.54–57 Fencing that completely encircles the pool and isolates it from the house (4-sided isolation pool fencing) is much more effective than methods in which children can still gain access to the pool through the house (3-sided perimeter fencing). One study reported an odds ratio (OR) of the risk of drowning in a fenced pool of 0.29, ie, the risk of drowning in a fenced pool was about 3 times lower than drowning in an unfenced pool.54 A second study showed that 4-sided isolation fencing is about 5 times more effective than 3-sided perimeter fencing (OR = 0.17).55 The third study56 reported similar ORs to those reported by Thompson and Rivara57 in their systematic review. Overall, the evidence shows that 4-sided isolation pool fencing significantly reduces childhood drowning and performs significantly better than 3-sided perimeter fencing.
A 2001–2003 national telephone survey found that although nearly 15% of households reported access to a swimming pool at their residence, only 74% were reported to have isolation pool fencing by which the pool was separated from the residence and yard areas with a self-closing and self-latching gate.58 A number of different methods for implementing 4-sided isolation fencing have been considered, such as ordinances, legislation, building codes, and home- or community-based education.57,59,60 Available evidence does not establish the best method(s) for implementation. Hence, field testing is needed to establish the optimal implementation method(s) to increase the prevalence of 4-sided isolation fencing.
Preset safe temperature hot water heaters
The evidence that preset safe temperature hot water heaters reduce scald burns comes primarily from Feldman et al61 and Erdmann et al.62 Feldman et al61 determined through testing that 80% of children hospitalized for scald burns lived in homes with unsafe bathtub water temperatures of 130°F or higher. Erdmann et al62 found that 5 years after a 1983 Washington State law required new water heaters to be preset at 120°F at the factory, 77% of homes tested had safe tap water temperatures and the frequency, morbidity, and mortality of tap water burn injuries in children were reduced.62 The effect of requesting manufacturers to voluntarily comply with the presetting of water heater temperatures to a safe level, in the absence of legislation, has not been evaluated. However, such voluntary compliance, with appropriate monitoring, is likely to be a promising approach that deserves field testing.63
Field testing is needed to determine effective methods for making safe the hot water heaters that are currently set at unsafe temperatures in homes. One such method is educating parents to lower the temperature setting of their hot water heaters. Studies evaluating home education have been comprehensively reviewed by Kendrick et al,60 who identified 11 studies that evaluated home education to promote safe hot tap water temperatures. A meta-analysis of the results of these studies demonstrated that families receiving home safety education were likelier to have a safe hot tap water temperature than did control families.60 A subsequently published study also found a greater prevalence of safe water temperature in households that had been provided a safety kit with a water temperature card than a control group that did not receive this information (OR = 2.21).64 However, evidence from these studies did not show any effect of home education on scald burns. Hence, further field testing is needed to determine the effect of home education to promote safe hot water heater temperature on water temperature and scald burns. In addition, formative research is needed to examine the effects of community-based education for safe hot water temperature and coordinated, multistrategy initiatives for burn prevention in young children.65
Promising interventions that need more field evaluation
The panel found that 5 of the interventions reviewed are promising but need more field testing.
Fall prevention by home modifications, such as handrails, grab bars, and improved lighting
Lyons et al66 conducted a systematic review of studies of home structural modifications, such as installation of handrails, grab bars, and improved stair lighting, for reducing risk of falls among older adults. The authors concluded that there is a need for more appropriately designed and sized studies to test the effectiveness of home environmental interventions. However, several studies included in the review suggest the potential for benefit from home modification.67–70
Three studies67–70 included in the review by Lyons et al evaluated the independent effect of physically modifying the home to reduce fall hazards. All 3 of these studies included home modifications implemented by professionals (occupational therapists or skilled trades-persons). In Cumming et al,67 home modifications, including installation of stair rails, nonslip mats, and night-lights, significantly reduced home hazards relative to no modifications in the homes. This study reported a significant reduction in falls among those persons with a history of falls (relative risk 0.64; 95% confidence interval [CI] = 0.5–0.83); however, among those persons without a history of falling, the intervention was not effective (relative risk = 1.03; 95% CI = 0.75–1.41).67 Day et al68 conducted a multifactorial study that evaluated exercise, vision correction, and home modification as single interventions and in combination.68 Day et al68 reported significantly reduced home hazards and a small, nonsignificant relative risk of 0.92 (95% CI = 0.75–1.08) for falls with home modification alone, suggesting that structural interventions may be modestly effective in reducing the risk of falls among the elderly. A strong, significant reduction in falls was observed when exercise and vision correction were combined with home hazard management (rate ratio = 0.67; 95% CI = 0.51–0.88). Neither Cumming et al67 nor Day et al68 evaluated effects on fall injuries. A third trial involving modifications such as installation of grab bars and improved lighting also reported significantly fewer home hazards in intervention homes relative to control homes.69,70 Stevens et al70 found no beneficial effect on the incidence of falls from a home visit to assess hazards combined with provision of free devices and education (adjusted rate ratio = 1.11), although the rate of injurious falls among the intervention group was nonsignificantly reduced (adjusted rate ratio = 0.92; 95% CI = 0.73–1.14). Additional, larger field evaluations are needed to evaluate and identify specific types of modifications likely to be consistently successful in reducing falls and fall injuries for those with and without a history of falling and to determine whether this approach is effective among specific populations (eg, frail adults or older adults with mobility impairment).
Field testing is also needed to determine the best method for implementing home modification for fall prevention among older adults, which can be costly and labor intensive. Two implementation methods appear promising: (1) multifactorial interventions that encompass home modification along with other fall prevention strategies such as exercise, medication review, nutritional supplements, or mobility aids; and (2) community-based, coordinated, multistrategy initiatives that include home hazard reduction.
Among the trials of multifactorial programs for fall prevention reviewed in Lyons et al,66 the majority of the studies showed reductions in falls. However, only 1 showed reduced injuries after intervention and 2 studies showed increased falls with implementation of the multifactorial program.66 The programs varied substantially in the types of cointerventions that were included, and some combinations of fall prevention strategies (eg, exercise, home hazard management, vision correction) are likely to be more effective than others, although the optimal combination has not been established. Evidence for community-based, coordinated, multistrategy initiatives to prevent older adult falls was reviewed by McClure et al.71 The review identified and described 5 studies that reported changes in medically treated, fall-related injuries among older people following the implementation of a controlled, population-based intervention that included home modifications to prevent falls. Despite methodological limitations of the studies reviewed, the reported reductions in fall-related injuries were consistent across all 5 programs. These systematic reviews suggest that both these types of implementation methods for preventing fall-related injury in older adults are promising, but further studies are needed to establish their effectiveness.
The evidence that window guards reduce childhood morbidity and mortality from falls comes primarily from dramatic results following a community-wide program to provide window guards in high-risk apartments. Falls declined 50% in these homes in the 2 years after the program's inception.72 A cohort study by Kendrick et al73 demonstrated a reduced risk of injury in homes with fitted stair gates and other safety devices but suggested that this finding may reflect generally a safe home rather than a specific benefit from stair gates or similar interventions.
Several methods for implementing these interventions have been evaluated. Kendrick et al reviewed 37 studies and reported that home education produced a statistically significant increase in the odds that a home would have a fitted stair gate (OR 1.26; 95% CI = 1.05–1.51) and a modest, nonsignificant increase in the prevalence of installed window locks and other window guards (OR = 1.16; 95% CI = 0.84–1.59). At the same time, the study did not show any change in child injury rates.60 Community-based, coordinated, multi-strategy initiatives that include home hazard reduction for fall prevention, targeting children, have been examined, but additional formative research is required.74,75
Building codes that require window guards, safe stair and balcony design, and other modifications are likely to be effective for fall prevention because they remove the need for home dwellers to modify their home for safety or encourage their landlords to install such interventions. However, evidence evaluating this intervention is lacking. Hence, these interventions are promising but need more field investigation to demonstrate an effect on injury rates and to determine optimal methods for implementation and for obtaining compliance with consistent stair gate and window guard use.
Temperature-controlled mixer faucets
Temperature-controlled mixer faucets reduce the temperature of hot water from faucets in manufacturer's tests and in institutional settings.63,76 Because of the risk of scald burns from high tap water temperatures and the evidence for a benefit from hot water heaters that are preset to a safe temperature (described earlier), mixer faucets would seem to be a valuable approach to scald burn prevention. However, one study showed that the majority of families that were given a thermostatic mixing valve removed the device within 9 months after installation.77 In addition, in a recent community-based trial to promote installation of temperature mixing valves, there was no evidence of a significant reduction in hot water temperature or scald injury rates.78 Therefore, although the technology is promising, field testing is required to determine how to implement this technology successfully. In addition, formative research is needed to improve the design (ie, long-term function and acceptability) of temperature-controlled mixer faucets.
Safe ignition sources and ignition source controls to prevent fires and burns
Evidence that electrical and heating systems are important sources for the ignition of residential fires in the United States has been reported by Hall.79 Fires involving heating equipment (eg, furnace, chimney) account for 22.1% of deaths in residential fires, whereas fires involving electrical distribution and lighting equipment (eg, electrical wiring, plugs, lighting) account for 11.2%. Given the evidence that legislation requiring smoke detector installation, and regulations mandating hot water heaters preset to safe temperatures, is effective in reducing fire and burn risk,53,62 legislation and enhanced building codes are considered promising methods to reduce fire risk related to electrical and heating systems. One example might be a requirement that all residential wiring, panel boards, circuit breakers, and outlets be updated to meet current building codes whenever homes are rented to new occupants or sold. However, field research is required to evaluate the effect of implementing new legislation and revising building codes relevant to this domain. Formative research is also needed to investigate whether home-and community-based education and distribution programs are effective in promoting safe ignition sources (eg, updated wiring, clean chimneys, and safe space heaters). Ignition source controls (eg, AFCI installation, which is currently required by the US National Electrical Code only in bedrooms of new residential construction) are one potential approach to improve safety of ignition sources, but methods to promote AFCI installation in existing buildings, such as building codes, legislation, or community education, require formative research.
Home modification to escape fires
Although working smoke alarms reduce the risk of fire injury, their efficacy depends on safe egress from the home in the event of a fire (eg, via access windows or protected stairways). The potential benefits of building codes and legislation requiring safe exits from fire are supported by the evidence of beneficial effects from building codes and legislation on other aspects of home structural safety.53,62 However, field testing of this intervention in the residential setting has not been conducted. In addition, formative research examining escape behaviors during fires is needed to inform safe egress design.
Working air-conditioning during heat waves
The strongest protective factor in preventing heat-related mortality during the 1999 heat wave in Chicago was a working air-conditioning system (OR = 0.2).41 However, no evaluations have measured the effectiveness of legislating, mandating, or promoting the installation of air-conditioning, to prevent heat-related mortality; therefore, field testing is needed. In addition, field testing is needed to understand the impact of legislating hot weather rules, which prohibit utility companies from disconnecting power for homes in which occupants are unable to pay their bill during extreme heat waves.80 Given the energy demands and cost of air-conditioning, formative research on the potential effect on heat-related mortality of other measures to maintain cool temperature in the home, such as home and landscape design that minimizes the need for air conditioning, is needed.
Interventions in need of formative research
In addition to the formative research needs identified earlier for a number of the effective and promising interventions, the panel identified 8 more interventions for which formative research is needed. Seven of these involve formative research in efficacy and design:
automatic fire sprinkler systems for housing,
pool covers and alarms,
bathtub design to reduce falls,
stove control design to prevent burns,
carbon monoxide poisoning prevention through design, engineering, legislation, and education,
noise reduction, and
design of residential construction materials (eg, laboratory-based testing of coatings on electrical wires to prevent arcing).
The eighth intervention for which the panel recommended formative research is the enforcement and/or use of incentives to improve the implementation of the following:
safety-related building and housing codes and legislation
The panel noted that interactions among a range of structural hazards (eg, falls and CO exposure) may occur and should be evaluated.
No evidence/ineffective interventions
The panel found that 1 intervention reviewed, 3-sided pool fencing, was ineffective.
Three-sided pool fences
Use of 3-sided pool fencing instead of complete 4-sided pool fencing is not effective and may actually increase risk because caregivers may believe that the incomplete fencing is adequate.55,57
Conclusions
Several interventions to improve home safety are likely to significantly reduce residential morbidity and mortality if effectively implemented. These interventions include installed, working smoke alarms; 4-sided isolation pool fencing; and hot water heaters that are preset by the manufacturer at a safe temperature. Although the effectiveness of safety interventions are strongly influenced by population demographics and other contextual factors, these 3 interventions have been shown to be effective when implemented in broad populations or in multiple different populations and contexts. Addressing structural deficiencies to reduce the enormous burden of unintentional injuries that occur in unsafe homes is likely to require concerted efforts from a broad range of agencies, organizations, and industries. It is not the purpose of this scientific review to specify which policies should be implemented to prevent injuries due to structural deficiencies. However, the review does aim to inform decisions about which policies are likely to result in the best and most efficient use of resources to address structural deficiencies and to illuminate where further research is needed to allow informed policy decisions to be made.
Acknowledgments
This work was supported by a cooperative grant from the Centers for Disease Control and Prevention, Office of Healthy Homes and Lead Poisoning Prevention, and the National Center for Healthy Housing.
Footnotes
Arc fault circuit interrupters protect against fire by continuously monitoring electrical current in a circuit and shutting off the current when unintended arching occurs.
Publisher's Disclaimer: Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of, nor have they been officially endorsed by the Centers for Disease Control and Prevention.
REFERENCES
- 1.National Safety Council . Injury Facts. 2003 Edition National Safety Council; Itasca, IL: 2003. [Google Scholar]
- 2.Agran PF, Anderson C, Winn D, Trent R, Walton-Haynes L, Thayer S. Rates of pediatric injuries by 3-month intervals for children 0 to 3 years of age. Pediatrics. 2003;111(6, pt 1):e683–e692. doi: 10.1542/peds.111.6.e683. [DOI] [PubMed] [Google Scholar]
- 3.Runyan CW, Perkis D, Marshall SW, et al. Unintentional injuries in the home in the United States, part II: morbidity. Am J Prev Med. 2005;28(1):80–87. doi: 10.1016/j.amepre.2004.09.017. [DOI] [PubMed] [Google Scholar]
- 4.Breysse P, Farr N, Galke W, Lanphear B, Morley R, Bergofsky L. The relationship between housing and health: children at risk. Environ Health Perspect. 2004;112(15):1583–1588. doi: 10.1289/ehp.7157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nagaraja J, Menkedick J, Phelan KJ, Ashley P, Zhang X, Lanphear BP. Deaths from residential injuries in US children and adolescents, 1985–1997. Pediatrics. 2005;116(2):454–461. doi: 10.1542/peds.2004-1415. [DOI] [PubMed] [Google Scholar]
- 6.Phelan KJ, Khoury J, Kalkwarf H, Lanphear B. Residential injuries in US children and adolescents. Public Health Rep. 2005;120(1):63–70. doi: 10.1177/003335490512000111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Home Safety Council . Older Adults and Home Injuries. Home Safety Council; Wilkesboro, NC: 2004. [Accessed September 8, 2009]. http://www.homesafetycouncil.org/AboutUs/Research/re_sohs_w010.asp. [Google Scholar]
- 8.Mathers L, Weiss H. Incidence and characteristics of fall-related emergency department visits. Acad Emerg Med. 1998;5(11):1064–1070. doi: 10.1111/j.1553-2712.1998.tb02663.x. [DOI] [PubMed] [Google Scholar]
- 9.Carter SE, Campbell EM, Sanson-Fisher RW, Redman S, Gillespie WJ. Environmental hazards in the homes of older people. Age Ageing. 1997;26(3):195–202. doi: 10.1093/ageing/26.3.195. [DOI] [PubMed] [Google Scholar]
- 10.Lord SR, Menz HB, Sherrington C. Home environment risk factors for falls in older people and the efficacy of home modifications. Age Ageing. 2006;35(suppl 2):ii55–ii59. doi: 10.1093/ageing/afl088. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention . Web-based Injury Statistics Query and Reporting System (WISQARS) US Department of Health and Human Services; Atlanta, GA: 2006. [Accessed November 30, 2009]. online. http://www.cdc.gov/injury/wisqars/. [Google Scholar]
- 12.Khambalia A, Joshi P, Brussoni M, Raina P, Morrongiello B, Macarthur C. Risk factors for unintentional injuries due to falls in children aged 0–6 years: a systematic review. Inj Prev. 2006;12:378–381. doi: 10.1136/ip.2006.012161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cayless SM. Slip, trip and fall accidents: relationship to building features and use of coroners' reports in ascribing cause. Appl Ergon. 2001;32(2):155–162. doi: 10.1016/s0003-6870(00)00052-1. [DOI] [PubMed] [Google Scholar]
- 14.Staunton CE, Frumkin H, Dannenberg AL. Changing the built environment to prevent injury. In: Doll LS, Bonzo SE, Sleet DA, Mercy JA, Haas EN, editors. Handbook of Injury and Violence Prevention. Springer; New York, NY: 2007. pp. 257–276. [Google Scholar]
- 15.Karter MJ. Fire Loss in the United States During 2006. National Fire Protection Association, Fire Analysis and Research Division; Quincy, MA: 2007. [Google Scholar]
- 16.Hall JR., Jr. Burns, Toxic Gases, and Other Hazards Associated With Fires: Deaths and Injuries in Fire and Non-Fire Situations. National Fire Protection Association, Fire Analysis and Research Division; Quincy, MA: 2001. [Google Scholar]
- 17.Istre GR, McCoy MA, Osborn L, Barnard JJ, Bolton A. Deaths and injuries from house fires. N Engl J Med. 2001;344(25):1911–1916. doi: 10.1056/NEJM200106213442506. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention . Fire Deaths and Injuries. US Department of Health and Human Services; Atlanta, GA: 2003. [Accessed March 25, 2008]. http://www.cdc.gov/ncipc/factsheets/fire.htm. [Google Scholar]
- 19.Home Safety Council . The State of Home Safety in America: Facts About Unintentional Injuries in the Home. 2nd ed. Home Safety Council; Wilkesboro, NC: 2004. [Google Scholar]
- 20.US Department of Housing and Urban Development . Healthy Homes Issues: Injury Hazards. Version 3. US Department of Housing and Urban Development; Washington, DC: 2006. [Accessed November 30, 2009]. http://www.hud.gov/offices/lead/library/hhi/HHIInjury_final_6_06.pdf. [Google Scholar]
- 21.US Fire Administration . Home Fire Prevention. US Fire Administration; Emmitsburg, MD: 2009. [Accessed April 14, 2009]. http://www.usfa.dhs.gov/citizens/all_citizens/home)_fire_prev/index.shtm. [Google Scholar]
- 22.US Fire Administration . Home Fire Safety: On the Safety Circuit: A Factsheet on Home Electrical Fire Prevention. US Department of Homeland Security; Washington, DC: 2006. [Accessed March 25, 2008]. http://www.usfa.dhs.gov/downloads/pdf/fswy5.pdf. [Google Scholar]
- 23.Mallonee S, Istre G, Rosenberg M, et al. Surveillance and prevention of residential-fire injuries. N Engl J Med. 1996;335(1):27–31. doi: 10.1056/NEJM199607043350106. [DOI] [PubMed] [Google Scholar]
- 24.Diekman ST, Ballesteros MF, Berger LR, Caraballo RS, Kegler SR. Ecological level analysis of the relationship between smoking and residential-fire mortality. Inj Prev. 2008;14(4):228–231. doi: 10.1136/ip.2007.017004. [DOI] [PubMed] [Google Scholar]
- 25.Runyan CW, Bangdiwala SI, Linzer MA, Sacks JJ, Butts J. Risk factors for fatal residential fires. N Engl J Med. 1992;327(12):859–863. doi: 10.1056/NEJM199209173271207. [DOI] [PubMed] [Google Scholar]
- 26.Marshall S, Runyan C, Bangdiwala S, Linzer MA, Sacks JJ, Butts JD. Fatal residential fires: who dies and who survives? JAMA. 1998;279(20):1633–1637. doi: 10.1001/jama.279.20.1633. [DOI] [PubMed] [Google Scholar]
- 27.Schieber RA, Gilchrist J, Sleet DA. Legislative and regulatory strategies to reduce childhood unintentional injuries. Future Child. 2000;10(1):111–136. [PubMed] [Google Scholar]
- 28.Simon PA, Baron RC. Age as a risk factor for burn injury requiring hospitalization during early childhood. Arch Pediatr Adolesc Med. 1994;148(4):394–397. doi: 10.1001/archpedi.1994.02170040060010. [DOI] [PubMed] [Google Scholar]
- 29.Morrow SE, Smith DL, Cairns BA, Howell PD, Nakayama DK, Peterson HD. Etiology and outcome of pediatric burns. J Pediatr Surg. 1996;31(3):329–333. doi: 10.1016/s0022-3468(96)90732-0. [DOI] [PubMed] [Google Scholar]
- 30.van Beeck EF, Branche CM, Szpilman D, Modell JH, Bierens JJLM. A new definition of drowning: towards documentation and prevention of a global public health problem. [Accessed December 21, 2009];Bull World Health Org. 2005 83:853–856. http://www.who.int/bulletin/volumes/83/11/vanbeeck1105abstract/en/index.html. [PMC free article] [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention Nonfatal and fatal drownings in recreational water settings—United States, 2001–2002. MMWR Morb Mortal Wkly Rep. 2004;53(21):447–452. [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention. National Center for Injury Prevention and Control [Accessed January 10, 2010];Web-based Injury Statistics Query and Reporting System (WISQARS) www.cdc.gov/ncipc/wisqars.
- 33.US Consumer Product Safety Commission [Accessed April 14, 2009];Swimming pool safety alert. http://www.cpsc.gov/cpscpub/pubs/5101.pdf.
- 34.US Consumer Product Safety Commission [Accessed April 14, 2009];How to plan for the unexpected: preventing child drownings. http://www.cpsc.gov/cpscpub/pubs/359.pdf.
- 35.US Consumer Product Safety Commission . An Evaluation of Swimming Pool Alarms. US Consumer Product Safety Commission; Washington, DC: 2000. [Accessed December 21, 2009]. http://www.cpsc.gov/library/alarm.pdf. [Google Scholar]
- 36.Centers for Disease Control and Prevention Unintentional non-fire-related carbon monoxide exposures—United States, 2001–2003. MMWR Morb Mortal Wkly Rep. 2005;54(2):36–39. [PubMed] [Google Scholar]
- 37.Ernst A, Zibrak J. Carbon monoxide poisoning. N Engl J Med. 1998;339(22):1603–1608. doi: 10.1056/NEJM199811263392206. [DOI] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention Unintentional non-fire-related carbon monoxide exposures—United States, 2004–2006. MMWR Morb Mortal Wkly Rep. 2008;57(33):896–899. [PubMed] [Google Scholar]
- 39.Raub J, Mathieu-Nolf M, Hampson N. Carbon monoxide poisoning—a public health perspective. Toxicology. 2000;145:1–14. doi: 10.1016/s0300-483x(99)00217-6. [DOI] [PubMed] [Google Scholar]
- 40.Centers for Disease Control and Prevention Heat-related deaths-United States, 1999–2003. MMWR Morb Mortal Wkly Rep. 2006;55(29):796–798. [PubMed] [Google Scholar]
- 41.Naughton MP, Henderson A, Mirabelli MC, et al. Heat-related mortality during a 1999 heat wave in Chicago. Am J Prev Med. 2002;22(4):221–227. doi: 10.1016/s0749-3797(02)00421-x. [DOI] [PubMed] [Google Scholar]
- 42.Centers for Disease Control and Prevention . Healthy Housing Reference Manual. US Department of Health and Human Services; Atlanta, GA: 2006. [Accessed November 30, 2009]. US Department of Housing and Urban Development. http://www.cdc.gov/nceh/publications/books/housing/housing.htm. [Google Scholar]
- 43.Pennington G, Topham N, Ward R. Aircraft noise and residential property values adjacent to Manchester International Airport. J Transp Econ Policy. 1990;24(1):49–59. [Google Scholar]
- 44.Bullard RD. Urban infrastructure: social, environmental, and health risks to African Americans. In: Livingston IL, editor. Handbook of Black American Health: The Mosaic of Conditions, Issues, Policies and Prospects. Greenwood Publishing; Westport, CT: 1994. pp. 315–330. [Google Scholar]
- 45.Evans GW, Saegert S. Residential crowding in the context of inner city poverty. In: Wapner S, Demick J, Yamamoto T, et al., editors. Theoretical Perspectives in Environment-Behavior Research. Kluwer Academic/Plenum Publishers; New York, NY: 2000. pp. 247–267. [Google Scholar]
- 46.Ellaway A, Macintyre S. Does housing tenure predict health in the UK because it exposes people to different levels of housing related hazards in the home or its surroundings? Health Place. 1998;4(2):141–150. doi: 10.1016/s1353-8292(98)00006-9. [DOI] [PubMed] [Google Scholar]
- 47.Evans G, Marcynyszyn L. Environmental justice, cumulative environmental risk, and health among low- and middle-income children in upstate New York. Am J Public Health. 2004;94(11):1942–1944. doi: 10.2105/ajph.94.11.1942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jacobs DE, Brown MJ, Baeder A, et al. A systematic review of housing interventions and health: introduction and methods. J Public Health Manag Pract. 2010;x(x) doi: 10.1097/PHH.0b013e3181e31d09. [DOI] [PubMed] [Google Scholar]
- 49.DiGuiseppi C, Roberts I, Li L. Smoke alarm ownership and house fire death rates in children. J Epidemiol Community Health. 1998;52(11):760–761. doi: 10.1136/jech.52.11.760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Watson L, Gamble J. Fire Statistics: United Kingdom 1998. Government Statistical Service; London, UK: 1999. [Google Scholar]
- 51.Ahrens M. US Experience With Smoke Alarms and Other Fire Alarms. National Fire Protection Association; Quincy, MA: 2004. [Google Scholar]
- 52.DiGuiseppi C, Goss CW, Higgins JPT. Interventions for promoting smoke alarm ownership and function. [Accessed November 30, 2009];Cochrane Database Syst Rev. 2008 (4):CD002246. doi: 10.1002/14651858.CD002246. http://www.cochrane.org/reviews/en/ab002246.html. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.McLoughlin E, Marchone M, Hanger SL, German PS, Baker SP. Smoke detector legislation: its effect on owner-occupied homes. Am J Public Health. 1985;75(8):858–862. doi: 10.2105/ajph.75.8.858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fergusson DM, Horwood LJ. Risks of drowning in fenced and unfenced domestic swimming pools. N Z Med J. 1984;97(767):777–779. [PubMed] [Google Scholar]
- 55.Intergov WA. Pre-school Drowning in Private Swimming Pools. Health Department of Western Australia; Perth, Western Australia, Australia: 1988. Intergovernmental Working Party on Swimming Pool Safety. [Google Scholar]
- 56.Pitt WR, Balanda KP. Childhood drowning and near-drowning in Brisbane: the contribution of domestic pools. Med J Aust. 1991;154(10):661–665. doi: 10.5694/j.1326-5377.1991.tb121253.x. [DOI] [PubMed] [Google Scholar]
- 57.Thompson DC, Rivara FP. Pool fencing for preventing drowning in children. Cochrane Database Syst Rev. 1998;(2):CD001047. doi: 10.1002/14651858.CD001047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gilchrist J, Mack K. Prevalence of pools and adequate pool fencing in the United States, 2001–2003. Int J Aquat Res Educ. 2008;1:16–26. [Google Scholar]
- 59.Morgenstern H, Bingham T, Reza A. Effects of pool-fencing ordinances and other factors on childhood drowning in Los Angeles County, 1990–1995. Am J Public Health. 2000;90(4):595–601. doi: 10.2105/ajph.90.4.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kendrick D, Coupland C, Mulvaney C, et al. Home safety education and provision of safety equipment for injury prevention. Cochrane Database Syst Rev. 2007;(1):CD005014. doi: 10.1002/14651858.CD005014.pub2. [DOI] [PubMed] [Google Scholar]
- 61.Feldman K, Schaller R, Feldman J, McMillon M. Tap water scald burns in children. Pediatrics. 1978;62:1–7. [PubMed] [Google Scholar]
- 62.Erdmann TC, Feldman KW, Rivara FP, Heimbach DM, Wall HA. Tap water burn prevention: the effect of legislation. Pediatrics. 1991;88(3):572–577. [PubMed] [Google Scholar]
- 63.Katcher M. Tap water scald prevention: it's time for a worldwide effort. Inj Prev. 1998;4:167–169. doi: 10.1136/ip.4.3.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Babul S, Olsen L, Janssen P, McIntee P, Raina P. A randomized trial to assess the effectiveness of an infant home safety programme. Int J Inj Contr Saf Promot. 2007;14(2):109–117. doi: 10.1080/17457300701272474. [DOI] [PubMed] [Google Scholar]
- 65.Turner C, Spinks A, McClure R, Nixon J. Community-based interventions for the prevention of burns and scalds in children. Cochrane Database Syst Rev. 2004;(3):CD004335. doi: 10.1002/14651858.CD004335.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lyons RA, John A, Brophy S, et al. Modification of the home environment for the reduction of injuries. Cochrane Database Syst Rev. 2006;(4):CD003600. doi: 10.1002/14651858.CD003600.pub2. [DOI] [PubMed] [Google Scholar]
- 67.Cumming RG, Thomas M, Szonyi G, et al. Home visits by an occupational therapist for assessment and modification of environmental hazards: a randomized trial of falls prevention. J Am Geriatr Soc. 1999;47(12):1397–1402. doi: 10.1111/j.1532-5415.1999.tb01556.x. [DOI] [PubMed] [Google Scholar]
- 68.Day L, Fildes B, Gordon I, Fitzharris M, Flamer H, Lord S. Randomised factorial trial of falls prevention among older people living in their own homes. BMJ. 2002;325(7356):128–131. doi: 10.1136/bmj.325.7356.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Stevens M, Holman CDJ, Bennett N. Preventing falls in older people: impact of an intervention to reduce environmental hazards in the home. J Am Geriatr Soc. 2001;49(11):1442–1447. doi: 10.1046/j.1532-5415.2001.4911235.x. [DOI] [PubMed] [Google Scholar]
- 70.Stevens M, Holman CDJ, Bennett N, de Klerk N. Preventing falls in older people: outcome evaluation of a randomized controlled trial. J Am Geriatr Soc. 2001;49(11):1448–1455. doi: 10.1046/j.1532-5415.2001.4911236.x. [DOI] [PubMed] [Google Scholar]
- 71.McClure R, Turner C, Peel N, Spinks A, Eakin E, Hughes K. Population-based interventions for the prevention of fall-related injuries in older people. Cochrane Database Syst Rev. 2005;(1):CD004441. doi: 10.1002/14651858.CD004441.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Spiegel C, Lindaman F. Children can't fly: a program to prevention childhood morbidity and mortality from window falls. Am J Public Health. 1977;67:1143–1147. doi: 10.2105/ajph.67.12.1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kendrick D, Watson M, Mulvaney C, Burton P. How useful are home safety behaviours for predicting childhood injury? A cohort study. Health Educ Res. 2005;20(6):709–718. doi: 10.1093/her/cyh021. [DOI] [PubMed] [Google Scholar]
- 74.McClure R, Nixon J, Spinks A, Turner C. Community-based programmes to prevent falls in children: a systematic review. J Paediatr Child Health. 2005;41(9–10):465–470. doi: 10.1111/j.1440-1754.2005.00685.x. [DOI] [PubMed] [Google Scholar]
- 75.Guyer B, Gallagher SS, Chang BH. Prevention of childhood injuries: evaluation of the Statewide Childhood Injury Prevention Program (SCIPP) Am J Public Health. 1989;79(11):1521–1527. doi: 10.2105/ajph.79.11.1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Stephen FR, Murray JP. Prevention of hot tap water burns: a comparative-study of 3 types of automatic mixing valve. Burns. 1993;19(1):56–62. doi: 10.1016/0305-4179(93)90102-e. [DOI] [PubMed] [Google Scholar]
- 77.Fallat ME, Rengers SJ, Bachulis BL, Pruitt BA. The effect of education and safety devices on scald burn prevention. J Trauma. 1993;34(4):560–564. doi: 10.1097/00005373-199304000-00013. [DOI] [PubMed] [Google Scholar]
- 78.Spallek M, Nixon J, Bain C, et al. Scald prevention campaigns: do they work? J Burn Care Res. 2007;28(2):328–333. doi: 10.1097/BCR.0B013E318031A12D. [DOI] [PubMed] [Google Scholar]
- 79.Hall JR., Jr. Home Structure Fires Involving Kitchen Equipment Other Than Cooking Equipment. National Fire Protection Association; Quincy, MA: 2008. [Google Scholar]
- 80.Koster C. Missouri's Hot Weather Rule—Consumer Blog. Missouri Attorney General's Office; Jefferson City, MO: 2008. [Accessed November 13, 2009]. http://ago.mo.gov/ConsumerCorner/blog/10430/Missouris_hot_weather_rule/. [Google Scholar]