Abstract
Background:
The etiology of esophageal squamous cell cancer (ESCC) in high prevalence regions of China remains unclear.
Methods:
Endoscopic biopsies were conducted among 7381 inhabitants aged from 25 to 65 of Anyang, China.
Results:
In this study, 2.57, 0.20 and 0.16% of the participants had mild, moderate and severe squamous dysplasia, respectively; 0.19 and 0.08% showed squamous carcinoma in situ and invasive ESCC. Using deep well (depth >100 meters) as water source (odds ratio=0.72, 95% confidence interval: 0.54–0.96) was negatively associated with ESCC and its precursors, whereas tobacco and alcohol use were not significantly associated with ESCC.
Conclusions:
Water source and other factors in this region need further evaluation by longitudinal studies.
Keywords: prevalence, risk factor, esophageal cancer, precursor lesion, China
Esophageal cancer is the sixth most common cancer among men and ninth most common among women (WHO & IARC, 2008). Tobacco and alcohol use are well recognized as the main risk factors for esophageal cancer in western countries (Castellsague et al, 2000; Adami et al, 2002).
In Anyang, a region in north central China, mortality from esophageal squamous cell cancer (ESCC) is among the highest in the world (Ke, 2002; WHO & IARC, 2008) being 10-fold greater than the nationwide rate for China and 100-fold greater than the rate among Caucasian Americans (Blot and Li, 1985). Beginning in the 1980s, a series of epidemiology studies to identify the risk factors in this area were carried out in Linzhou (formerly Linxian or Lin County), Anyang. These indicated that cigarette smoking, tooth loss and lack of certain nutrients and minerals (e.g. selenium) were associated with higher risk of ESCC (Mark et al, 2000; Abnet et al, 2001; Tran et al, 2005; Wei et al, 2005; Qiao et al, 2009). However, the discrimination model for ESCC that was constructed on the basis of these determinants performed suboptimally, with sensitivity and specificity values of 57 and 54%, respectively (Wei et al, 2005), strongly suggesting that other pathogenic factors had not been effectively evaluated.
In 2007, we initiated a population-based esophageal cancer cohort study in Anyang, China using endoscopic biopsy and a questionnaire investigation to determine its age specific prevalence and that of its precursor lesions in this region, and investigate the possible risk factors for ESCC. The results would also serve as baseline data for our subsequent longitudinal investigation.
Materials and methods
Anyang, an agricultural region in the northern part of Henan Province, PR China, consisting of five counties, Linzhou, Hua County, Anyang County, Tangyin County and Neihuang County, with a population of 5.37 million; its gross domestic product (GDP) per capita is about US $1760. In 2007–09, we conducted an endoscopic survey for esophageal cancer and precursor lesions in nine villages of rural Anyang, which were selected on the basis of the population size and location. Five were in Hua County, two in Linzhou, one in Anyang County and one in Tangyin County. Criteria for participant eligibility were as follows: (1) permanent residency in one of these villages; (2) age 25 to 65; (3) no previous cardiocerebral vascular diagnoses or psychological disorders; (4) voluntary participation in this study and agreement to complete all phases of the examination, including endoscopy.
Endoscopy was performed with Lugol’s iodine staining. The entire esophagus and stomach were visually examined, and biopsies were taken from all focal lesions identified. A standard site in the mid-esophagus (25 cm distal to the incisors in the 6 o’clock position) was sampled if no abnormalities were found. Biopsies were fixed in 10% formaldehyde, embedded in paraffin, sectioned at 5 mm, and stained with hematoxylin and eosin. Biopsy slides were read independently by two pathologists at Anyang Cancer Hospital, without knowledge of the subjects’ history or endoscopic findings. Diagnoses included normal, esophagitis, basal cell hyperplasia (BCH), squamous dysplasia (mild, moderate and severe), squamous carcinoma in situ (CIS), invasive squamous cell carcinoma and adenocarcinoma based on commonly accepted criteria (Dawsey et al, 1994; Wei et al, 2005).
A questionnaire was completed covering socio-demographic characteristics, pesticide exposure, living environment, alcohol and tobacco use and dietary habits. Interviews were carried out one-on-one in a room situated so as to ensure privacy.
Statistical analysis
Crude detection rates of all histological diagnoses were standardized by the age structure of the World Health Organization world standard population of 1985 (Ahmad et al, 2000). Differences in detection rate among groups were evaluated using the χ2-test and Fisher’s exact test. Univariate and multivariate unconditional logistic regression was employed to identify risk factors for ESCC and its precursor lesions. All subjects were categorized either as ‘case group’ (all grades of dysplasia, CIS and ESCC) or ‘control group’ (normal epithelium, esophagitis and BCH) for logistic regression analysis. Two cases of adenocarcinoma were excluded from this analysis. All statistical analyses were conducted using SPSS for Windows version 11.5. All P-values were two-sided and P-values less than 0.05 were considered statistically significant.
Ethical review
An individual informed consent was signed by all participants. This study was approved by the Institutional Review Board of the School of Oncology, Peking University, China.
Results
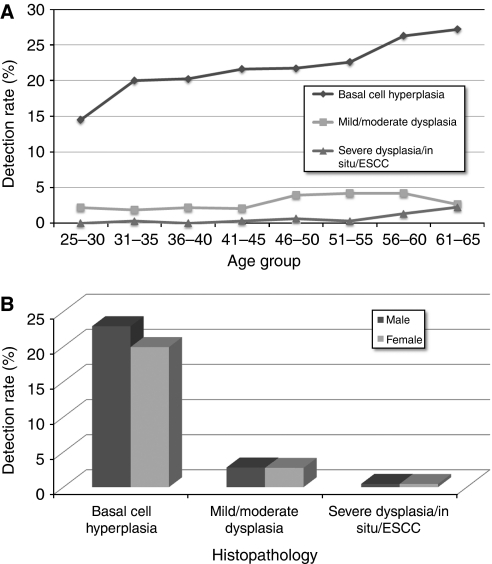
A total of 10439 residents were eligible and 7643 (73.22%) completed all required blood testing, endoscopy and biopsy and the questionnaire. Of these individuals, 7381 (96.57%) had at least one biopsy technically adequate for pathology diagnosis. As a recent study in this region demonstrated that esophagitis was not associated with risk of esophageal cancer (Wang et al, 2005), ‘normal’ and ‘esophagitis’ diagnoses were combined into one category. For all 7381 subjects, 5568 (75.44%) were diagnosed as normal or esophagitis; 1574 (21.33%) had BCH; 190 (2.57%) showed mild squamous dysplasia; 15 (0.20%) had moderate squamous dysplasia; 12 (0.16%) had severe squamous dysplasia; 14 (0.19%) had CIS; 6 (0.08%) had squamous cell carcinoma; and 2 (0.03%) had adenocarcinoma (Table 1). Figure 1a shows the age specific detection rates of lesions ranging from BCH to ESCC. Detection rates of BCH increased monotonically with age in all age groups. Detection rates of mild/moderate dysplasia were higher than that of severe dysplasia/CIS/ESCC in all age groups. However, mild/moderate dysplasia began to decrease in the 51–55 year group, whereas detection rates of severe dysplasia/CIS/ESCC showed a concomitant significantly increasing trend and these two curves almost intersected in the 61–65 year group. More BCH was found in males (22.92%) than in females (19.94%, P=0.002) and there were no other significant gender differences in detection rates of esophageal cancer or its precursor lesions (Table 1, Figure 1b).
Table 1. Detection rates of esophageal cancer and precursor lesions by gender.
|
Total (N=7381)
|
Male (N=3425)
|
Female (N=3956)
|
||||||
|---|---|---|---|---|---|---|---|---|
| Histopathology | n | % | % (Adjusted)a | n | % | n | % | P b |
| Normal or esophagitis | 5568 | 75.44 | 76.19 | 2528 | 73.81 | 3040 | 76.85 | 0.003 |
| Basal cell hyperplasia | 1574 | 21.33 | 20.67 | 785 | 22.92 | 789 | 19.94 | 0.002 |
| Squamous dysplasia | ||||||||
| Mild | 190 | 2.57 | 2.53 | 89 | 2.60 | 101 | 2.55 | 0.902 |
| Moderate | 15 | 0.20 | 0.17 | 7 | 0.20 | 8 | 0.20 | 0.984 |
| Severe | 12 | 0.16 | 0.15 | 3 | 0.09 | 9 | 0.23 | 0.137 |
| Squamous carcinoma in situ | 14 | 0.19 | 0.19 | 7 | 0.20 | 7 | 0.18 | 0.787 |
| Squamous cell carcinoma | 6 | 0.08 | 0.08 | 5 | 0.15 | 1 | 0.03 | 0.160 |
| Squamous cell carcinoma and precursor lesions | 237 | 3.21 | 3.12 | 111 | 3.24 | 126 | 3.19 | 0.892 |
| Adenocarcinoma | 2 | 0.03 | 0.02 | 1 | 0.03 | 1 | 0.03 | 1.000 |
Detection rates were adjusted by standard age structure of the world population (WHO, 1985).
P-values were derived by χ2-test or Fisher's exact test.
Figure 1.
(A) Detection rates of esophageal cancer and precursor lesions by age. (B) Detection rates of esophageal cancer and precursor lesions by gender.
Potential ESCC risk factors, including tobacco and alcohol use were evaluated using unconditional logistic regression analysis (Table 2). Univariate logistic regression showed that tooth loss (Ptrend=0.017) was associated with increased risk of ESCC and its precursors, whereas use of water pumped from a deep well (over 100 m depth) (odds ratio=0.72, 95% confidence interval=0.54–0.95, P=0.022) showed a negative association with ESCC and its precursor lesions. After adjusting for age and sex, use of deep well water remained as having a negative association with ESCC and precursor lesions (odds ratio=0.72, 95% confidence interval=0.54–0.96; P=0.023). Cigarette smoking, alcohol intake, pesticide exposure and hot food intake were not found to correlate with ESCC and precursor lesions.
Table 2. Univariate and multivariate unconditional logistic analysis of risk factors associated with esophageal squamous cell carcinoma and precursor lesions.
| Subjects with ESCC and | Subjects without ESCC and | Unadjusted |
95%CI
|
Adjusted |
95%CI
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | precursor lesions n (%) | precursor lesions n (%) | odds ratio | Lower | Upper | P | P-trenda | odds ratiob | Lower | Upper | P | P-trenda |
| Smoking history | ||||||||||||
| Never | 161 (70.61) | 4934 (71.18) | 1.00 | — | — | Ref. | 1.00 | — | — | Ref. | ||
| Current | 60 (26.32) | 1713 (24.71) | 1.07 | 0.79 | 1.45 | 0.645 | 1.00 | 0.67 | 1.50 | 0.998 | ||
| Former | 7 (3.07) | 285 (4.11) | 0.75 | 0.35 | 1.62 | 0.467 | 0.62 | 0.27 | 1.40 | 0.246 | ||
| Drinking history | ||||||||||||
| Never | 204 (89.47) | 5995 (86.52) | 1.00 | — | — | Ref. | 1.00 | — | — | Ref. | ||
| Current | 23 (10.09) | 902 (13.02) | 0.75 | 0.48 | 1.16 | 0.195 | 0.71 | 0.45 | 1.14 | 0.158 | ||
| Former | 1 (0.44) | 32 (0.46) | 0.92 | 0.12 | 6.75 | 0.933 | 0.83 | 0.11 | 6.16 | 0.854 | ||
| Tooth loss | ||||||||||||
| ⩽4 | 23 (48.94) | 1677 (70.43) | 1.00 | — | — | Ref. | 0.018 | 1.00 | — | — | Ref. | 0.809 |
| 5–9 | 14 (29.79) | 391 (16.42) | 2.61 | 1.33 | 5.12 | 0.005 | 1.86 | 0.90 | 3.87 | 0.095 | ||
| 10–14 | 5 (10.64) | 129 (5.42) | 2.83 | 1.06 | 7.56 | 0.038 | 1.59 | 0.54 | 4.68 | 0.397 | ||
| ⩾15 | 5 (10.64) | 184 (7.73) | 1.98 | 0.74 | 5.27 | 0.171 | 0.97 | 0.32 | 2.93 | 0.963 | ||
| Pesticide exposure | ||||||||||||
| No | 38 (16.67) | 1187 (17.12) | 1.00 | — | — | Ref. | 1.00 | — | — | Ref. | ||
| Yes | 190 (83.33) | 5745 (82.88) | 1.03 | 0.73 | 1.47 | 0.857 | 1.00 | 0.70 | 1.44 | 0.991 | ||
| Preferred food temperature | ||||||||||||
| Cold | 24 (10.53) | 843 (12.17) | 1.00 | — | — | Ref. | 0.102 | 1.00 | — | — | Ref. | 0.135 |
| Moderate | 115 (50.44) | 3758 (54.24) | 1.07 | 0.69 | 1.68 | 0.751 | 0.98 | 0.62 | 1.54 | 0.929 | ||
| Hot | 89 (39.04) | 2328 (33.60) | 1.34 | 0.85 | 2.12 | 0.207 | 1.27 | 0.80 | 2.01 | 0.314 | ||
| Water source | ||||||||||||
| Shallow well | 151 (66.81) | 4067 (59.17) | 1.00 | — | — | Ref. | 1.00 | — | — | Ref. | ||
| Deep motor-pumped well | 75 (33.19) | 2806 (40.83) | 0.72 | 0.54 | 0.95 | 0.022 | 0.72 | 0.54 | 0.96 | 0.023 | ||
Abbreviation: CI=confidence interval.
To evaluate trends in odds, ordinal variables were modeled as single, continuous, independent variables.
Odds ratios were adjusted for age (5-year groups) and sex.
Discussion
The Anyang region of China is a high-risk region for ESCC, and a series of studies on ESCC have been carried out there. To obtain the greatest number of patients with ESCC or precursor lesions as possible, participants chosen for almost all these studies were of generally greater age (Li et al, 1989; Dawsey et al, 1994; Tran et al, 2005; Wang et al, 2005; Wei et al, 2005). These studies, therefore, typically reported much higher rates of cancer and precursor lesions. For example, rates of mild, moderate and severe esophageal dysplasia of 8.6, 7.8 and 2.6%, respectively, were recently reported in Cixian, an adjacent high-risk region (Lu et al, 2004). In our population-based screening study we evaluated data over a broader age range (25–65 years), and included individuals from entirety rural area around Anyang. This age difference is important given the positive association with age of ESCC and precancerous lesions. We consider the prevalence of ESCC and its precursors in younger age groups is important for etiologic studies in this high-risk region, as the cumulative effects of pathogenic factors (e.g. water source) may be evaluated more efficiently through analysis with full consideration and adjustment for age.
Water source is not a common risk factor for ESCC, especially in developed countries. Until about 20 years ago, the main sources of drinking water in rural area of Anyang were rivers or shallow wells. However, since the 1980s, the local government has committed significant resources to an extensive water improvement project, and now-a-days deep groundwater has become the main water source for most of the inhabitants of rural Anyang. A previous ecologic study reported that the incidence and mortality from esophageal cancer in Linzhou showed a decreasing trend in villages included in this water improvement project as compared with those without water improvement (Han et al, 2007). The conclusions of ecological studies cannot be directly linked to the etiology of disease, but in the current population-based study, we found that use of deep well water had an independent negative association with ESCC and precancerous lesions. This is the first population-based study to suggest an association between water source and ESCC. Although further confirmation and studies of the mechanism will be necessary, these findings could be taken as evidence for the promotion of etiologic research and ESCC control in economically underdeveloped regions where surface or shallow ground water are still used as a main water source.
Although tobacco and alcohol are well-established risk factors for ESCC in western countries (Adami et al, 2002; IARC, 2004; Freedman et al, 2007; Pandeya et al, 2008) this is neither the case in Asian high-risk regions including Anyang (Cook-Mozaffari et al, 1979; Yu et al, 1993; Guo et al, 1994) nor in our study. Tooth loss has been reported to be associated with an increased risk of esophageal cancer (Wang et al, 1992; Abnet et al, 2001, 2005) Changes in chewing may expose the esophagus to more frequent injury and may also result in increased risk of oral bacterial infection and production of carcinogens, such as nitrosamines (Abnet et al, 2001; Guha et al, 2007). In our analysis, tooth loss was positively associated with ESCC in the univariate analysis, but not in the multivariate analysis. Subsequent multivariate analysis stratified by age showed a clear association with tooth loss in the group less than 50 years old, but not in older subjects (data not shown). We believe that both tooth loss itself and lack of retrospective information about tooth loss history are likely to have contributed to these age differences, and to have biased the relationship toward the null hypothesis in the older age groups. We consider that tooth loss in early life is likely to be associated with ESCC in Anyang.
In summary, 7381 individuals of rural Anyang participated in this cross-sectional endoscopic survey. Detection rates of mild, moderate and severe squamous dysplasia, CIS and ESCC were 2.57, 0.20, 0.16, 0.19 and 0.08%. Use of water pumped from deep wells was negatively associated with ESCC and precursor lesions, whereas tobacco and alcohol use had no significant relationship with ESCC. Longitudinal studies are needed of other risk factors that may contribute to ESCC in this high-risk region.
Acknowledgments
This work was supported by Natural Science Foundation of China 30430710 and 30930102, ‘863’ Key Projects of National Ministry of Science and Technology Grant 2006AA2Z467 and 2006AA02A403, Research Special Fund Public Welfare Industry of Health 200902002-8, Natural Science Foundation of Beijing 7100001 and Beijing Project on Science and Technology Commission Z09050703080902 to Yang Ke. We would also like to thank Dr Michael A. McNutt for editing and correction of this paper.
References
- Abnet CC, Qiao YL, Dawsey SM, Dong ZW, Taylor PR, Mark SD (2005) Tooth loss is associated with increased risk of total death and death from upper gastrointestinal cancer, heart disease, and stroke in a Chinese population-based cohort. Int J Epidemiol 34: 467–474 [DOI] [PubMed] [Google Scholar]
- Abnet CC, Qiao YL, Mark SD, Dong ZW, Taylor PR, Dawsey SM (2001) Prospective study of tooth loss and incident esophageal and gastric cancers in China. Cancer Causes Control 12: 847–854 [DOI] [PubMed] [Google Scholar]
- Adami H, Hunter D, Trichopoulos D (2002) Textbook of Cancer Epidemiology. Oxford University Press: Oxford [Google Scholar]
- Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJ, Lozano R, Inoue M (2000) Age standardization of rates: a new WHO standard In GPE Discussion Paper Series: No31 World Health Orgnization
- Blot WJ, Li JY (1985) Some considerations in the design of a nutrition intervention trial in Linxian, People’s Republic of China. Natl Cancer Inst Monogr 69: 29–34 [PubMed] [Google Scholar]
- Castellsague X, Munoz N, De Stefani E, Victora CG, Castelletto R, Rolon PA (2000) Influence of mate drinking, hot beverages and diet on esophageal cancer risk in South America. Int J Cancer 88: 658–664 [DOI] [PubMed] [Google Scholar]
- Cook-Mozaffari PJ, Azordegan F, Day NE, Ressicaud A, Sabai C, Aramesh B (1979) Oesophageal cancer studies in the Caspian Littoral of Iran: results of a case-control study. Br J Cancer 39: 293–309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawsey SM, Lewin KJ, Liu FS, Wang GQ, Shen Q (1994) Esophageal morphology from Linxian, China. Squamous histologic findings in 754 patients. Cancer 73: 2027–2037 [DOI] [PubMed] [Google Scholar]
- Freedman ND, Abnet CC, Leitzmann MF, Mouw T, Subar AF, Hollenbeck AR, Schatzkin A (2007) A prospective study of tobacco, alcohol, and the risk of esophageal and gastric cancer subtypes. Am J Epidemiol 165: 1424–1433 [DOI] [PubMed] [Google Scholar]
- Guha N, Boffetta P, Wunsch Filho V, Eluf Neto J, Shangina O, Zaridze D, Curado MP, Koifman S, Matos E, Menezes A, Szeszenia-Dabrowska N, Fernandez L, Mates D, Daudt AW, Lissowska J, Dikshit R, Brennan P (2007) Oral health and risk of squamous cell carcinoma of the head and neck and esophagus: results of two multicentric case-control studies. Am J Epidemiol 166: 1159–1173 [DOI] [PubMed] [Google Scholar]
- Guo W, Blot WJ, Li JY, Taylor PR, Liu BQ, Wang W, Wu YP, Zheng W, Dawsey SM, Li B, Fraumeni JF (1994) A nested case-control study of oesophageal and stomach cancers in the Linxian nutrition intervention trial. Int J Epidemiol 23: 444–450 [DOI] [PubMed] [Google Scholar]
- Han JY, Xu ZX, Xing HP, Tan JJ, Wang MX, Zhang SH, Kong FJ, Si JH, Li XM, Tang LN, Tian PQ (2007) A historical cohort study on the effect of drinking water improvement to the mortality of esophageal carcinoma among Linzhou residents. Chinese Journal of Epidemiology 28: 515–516 [PubMed] [Google Scholar]
- IARC (2004) IARC Monographs on the Evaluation of the Carcinogenic Risk of Chemicals to Human. In Tobacco Smoke and Involuntary Smoking. IARC: Lyon [PMC free article] [PubMed] [Google Scholar]
- Ke L (2002) Mortality and incidence trends from esophagus cancer in selected geographic areas of China circa 1970–90. Int J Cancer 102: 271–274 [DOI] [PubMed] [Google Scholar]
- Li JY, Ershow AG, Chen ZJ, Wacholder S, Li GY, Guo W, Li B, Blot WJ (1989) A case-control study of cancer of the esophagus and gastric cardia in Linxian. Int J Cancer 43: 755–761 [DOI] [PubMed] [Google Scholar]
- Lu XJ, Chen ZF, Guo CL, Li SS, Bai WL, Jin GL, Wang YX, Meng FS, Gao F, Hou J (2004) Endoscopic survey of esophageal cancer in a high-risk area of China. World J Gastroenterol 10: 2931–2935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mark SD, Qiao YL, Dawsey SM, Wu YP, Katki H, Gunter EW, Fraumeni Jr JF, Blot WJ, Dong ZW, Taylor PR (2000) Prospective study of serum selenium levels and incident esophageal and gastric cancers. J Natl Cancer Inst 92: 1753–1763 [DOI] [PubMed] [Google Scholar]
- Pandeya N, Williams GM, Sadhegi S, Green AC, Webb PM, Whiteman DC (2008) Associations of duration, intensity, and quantity of smoking with adenocarcinoma and squamous cell carcinoma of the esophagus. Am J Epidemiol 168: 105–114 [DOI] [PubMed] [Google Scholar]
- Qiao YL, Dawsey SM, Kamangar F, Fan JH, Abnet CC, Sun XD, Johnson LL, Gail MH, Dong ZW, Yu B, Mark SD, Taylor PR (2009) Total and cancer mortality after supplementation with vitamins and minerals: follow-up of the Linxian General Population Nutrition Intervention Trial. J Natl Cancer Inst 101: 507–518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran GD, Sun XD, Abnet CC, Fan JH, Dawsey SM, Dong ZW, Mark SD, Qiao YL, Taylor PR (2005) Prospective study of risk factors for esophageal and gastric cancers in the Linxian general population trial cohort in China. Int J Cancer 113: 456–463 [DOI] [PubMed] [Google Scholar]
- Wang GQ, Abnet CC, Shen Q, Lewin KJ, Sun XD, Roth MJ, Qiao YL, Mark SD, Dong ZW, Taylor PR, Dawsey SM (2005) Histological precursors of oesophageal squamous cell carcinoma: results from a 13 year prospective follow up study in a high risk population. Gut 54: 187–192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang YP, Han XY, Su W, Wang YL, Zhu YW, Sasaba T, Nakachi K, Hoshiyama Y, Tagashira Y (1992) Esophageal cancer in Shanxi Province, People’s Republic of China: a case-control study in high and moderate risk areas. Cancer Causes Control 3: 107–113 [DOI] [PubMed] [Google Scholar]
- Wei WQ, Abnet CC, Lu N, Roth MJ, Wang GQ, Dye BA, Dong ZW, Taylor PR, Albert P, Qiao YL, Dawsey SM (2005) Risk factors for oesophageal squamous dysplasia in adult inhabitants of a high risk region of China. Gut 54: 759–763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO & IARC (2008) World Cancer Report 2008. WHO, IARC: Lyon [Google Scholar]
- Yu Y, Taylor PR, Li JY, Dawsey SM, Wang GQ, Guo WD, Wang W, Liu BQ, Blot WJ, Shen Q, Li B (1993) Retrospective cohort study of risk-factors for esophageal cancer in Linxian, People’s Republic of China. Cancer Causes Control 4: 195–202 [DOI] [PubMed] [Google Scholar]