Abstract
INTRODUCTION
Following the merger of two major units to form a regional centre for plastic surgery in the West Midlands, acute hand surgery referrals reached overwhelming proportions. This study describes audits performed at three time points. The first highlighted the extent of in-patient delay and was instrumental in the subsequent development of a dedicated hand trauma day-case unit.
PATIENTS AND METHODS
Data were collected on 77 patients in June 2002, 109 patients in November 2003 and 90 patients in November 2004. The day-case unit opened on 1 November 2003.
RESULTS
The number of bed-days per patient fell from 2.63 to 1.34 (P < 0.001) over the study period. In November 2004, 51% of patients received a day-case procedure. Importantly, if admission was required at initial presentation, the delay to theatre reduced from 1.5 bed-days per patient in June 2002 to 0.6 in November 2004. Overall, the in-patient delay was significantly reduced (P < 0.001) but time from presentation to theatre was not significantly affected (P = 0.119).
CONCLUSIONS
This series of audits confirmed that a significant number of acute hand injuries are suitable for day-case procedures and that simple audit can lead to a significant change in service provision. Improvements were demonstrated in reduced in-patient delay and total stay. We hope that other units find our experience useful given that it may be possible to apply this approach to other forms of ambulatory trauma.
Keywords: Day-case, Hand, Trauma, Audit
Hand trauma is a frequent occurrence and there is evidence to show that the incidence is rising.1 In the West Midlands, two major hand units (Wordsley Hospital and Selly Oak Hospital) merged as part of the formation of a regional centre for plastic surgery. As expected, acute hand referrals at the centre were high, but ultimately became overwhelming despite increasing the number of dedicated operating lists during working hours. It was perceived that patients were waiting an inordinate amount of time in hospital before undergoing surgery and, as a result, elective cases were being cancelled due to high bed occupancy by these patients. There was also a perception that complaints by patients with hand injuries to the trust were high.
This article details the results of three audits that were performed at the University Hospital Birmingham NHS Trust (Selly Oak Hospital) following the above merger. An initial audit was conducted to quantify the magnitude of the problem. The results of this audit were presented to the management team and were instrumental in the development of a hand-surgery day-case unit. Two further audits were then conducted to close the audit loop. These were performed 1 month and 12 months after the unit opened. The ultimate aim was to assess the impact of the unit on the acute hand-surgery service over time.
Patients and Methods
The first audit was conducted in June 2002, the second during the opening month of the unit in November 2003 and the third in November 2004. Each audit was performed for a complete calendar month. Patients with acute hand injuries requiring surgery were identified from theatre record books and cross-referenced with copies of theatre lists to maximise data collection. All patients were 16 years and over as no paediatric patients are treated at this hospital.
Once the patients had been identified, case notes were analysed. Basic demographic data were collected, as were delays to admission and surgery, operative time, type of operation and length of stay. Date and time of presentation was recorded from the emergency department admission card. The length of anaesthesia was recorded to give an indication of the duration of surgery. Where possible, theatre records were used to assess the duration of local anaesthetic procedures.
Following the inception of the day-surgery unit, additional data were collected including ASA grade, complication and re-admission rates. It was also ascertained if each patient was admitted on first presentation or sent home as part of their care pathway to be re-admitted as a planned day-case. As before, all theatre lists were studied, including those of the new day-surgery unit.
The concept of bed-days was used during the analysis. One bed-day was defined as one overnight stay. Therefore, admission and discharge on the same day of admission was regarded as zero bed-days. Statistical analysis was performed using SPSS v.15.0 for Windows and Microsoft Excel 2002. Fisher's exact test was used to compare the distribution of categorical variables in the three audit periods. Kendall's tau-b statistic was used to analyse ASA grade. The Kruskal–Wallis test was used to compare ages and bed-days in the three audit periods. Where the Kruskal–Wallis test was significant, Dunn's test was used to identify significant pair-wise comparisons.
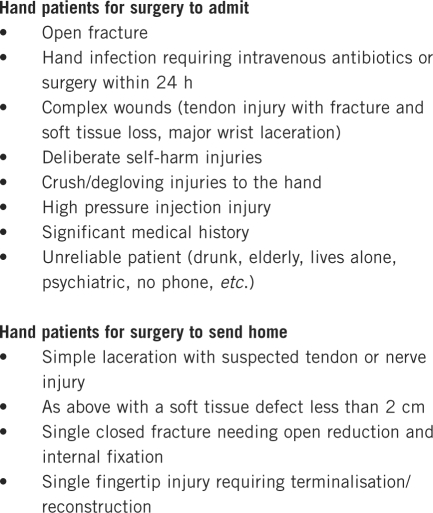
The protocol for suitability for admission and day-case used at the unit is shown in Figure 1. Pivotal to the running of this service is a hand co-ordinator, who is a senior nurse.
Figure 1.
The Birmingham Protocol
Results
The results of the three audits with respect to patient age, ASA grade and bed occupancy are shown in Table 1. To aid comparison between the audits performed, individual operations were crudely categorised according to the procedures performed. Category of operation performed during each month audited is shown in Table 2, which demonstrates no significant difference across audit periods using Fisher's exact test (P = 0.42). The median delay during each stage of the patient's journey is presented in Table 3.
Table 1.
Patient age, ASA grade and overall bed occupancy across the three audits
| June 2002 (n = 77) | Nov. 2003 (n = 109) | Nov. 2004 (n = 90) | |
|---|---|---|---|
| Median age in years (range) | 34 (17–80) | 39 (17–89) | 36 (19–83) |
| ASA grade | |||
| Recorded | n/a | 92 | 89 |
| I | n/a | 65 | 73 |
| II | n/a | 18 | 14 |
| III | n/a | 7 | 2 |
| IV | n/a | 2 | 0 |
| V | n/a | 0 | 0 |
| Bed-days | |||
| In-patient delay | 114 | 106 | 55 |
| Total stay | 203 | 227 | 121 |
| Days per patient | 2.64 | 2.08 | 1.34 |
n/a, not applicable.
Table 2.
Category of operations performed during each audit period
| Operations | June 2002 (n = 77) | Nov. 2003 (n = 109) | Nov. 2004 (n = 90) |
|---|---|---|---|
| Terminalisation | 2 | 4 | 5 |
| Extensor tendon repair | 7 | 12 | 11 |
| Debride/suture | 21 | 29 | 25 |
| Nail bed repair | 4 | 1 | 4 |
| Semi-elective | 2 | 2 | 2 |
| Digital nerve repair | 7 | 2 | 4 |
| Fracture fixation | 10 | 27 | 17 |
| Flexor tendon repair | 5 | 4 | 5 |
| Tendon and digital nerve | 4 | 3 | 1 |
| Complex/multiple | 15 | 17 | 12 |
| Tissue transfer | 0 | 3 | 4 |
| Miscellaneous | 0 | 5 | 0 |
Table 3.
The median delay during each stage of the patients'journey
| June 2002 | November 2003 | November 2004 | P-value | |
|---|---|---|---|---|
| Day-case rate (All patients with zero bed days) | 10 | 37 | 46 | |
| Admitted directly | 65 | 70 | 42 | |
| Sent home for planned day-case | 12 | 39 | 48 | < 0.001 |
| Patients admitted directly | Days (IQR) | Days (IQR) | Days (IQR) | |
| Delay to theatre | 1 (1–2) | 1 (1–2) | 1 (0–2) | 0.409 |
| Postoperative days | 1 (0–1) | 1 (0–2) | 1 (0–2) | 0.224 |
| Patients sent home | ||||
| Delay to admission | 2 (1–3.75) | 2 (2–3) | 3 (2–4) | 0.045 |
| Time from admission to theatre | 0.5 (0–2) | 0 (0–0) | 0 (0–0) | < 0.001 |
| Time from presentation to theatre | 4 (1.5–4) | 2 (2–3) | 3 (2–4) | 0.086 |
| Postoperative days | 0.5 (0–1) | 0 (0–0) | 0 (0–0) | < 0.001 |
| Overall | ||||
| Delay to admission | 0 (0–0) | 0 (0–2) | 1 (0–3) | <0.001 |
| Time from admission to theatre | 1 (0.5–2) | 1 (0–1) | 0 (0–1) | <0.001 |
| Time from presentation to theatre | 2 (1–3) | 2 (1–2) | 2 (1–3) | 0.119 |
| Postoperative days | 1 (0–1) | 0 (0–1) | 0 (0–1) | 0.017 |
IQR, interquartile range.
June 2002
For the first audit performed in June 2002, there were 85 patients with hand/forearm injuries identified from operating lists. Case notes were not located for eight patients. Data were, therefore, collected on the remaining 77 patients. Operations performed were of short duration with 38% of procedures less than 1 h and 74% less than 2 h. Of cases, 10% were performed using local anaesthetic with unspecified operation duration.
A total of 114 bed-days (56% of the total number of bed-days) were incurred while waiting for surgery. In-patient delays to theatre were common. Only 19 patients (25%) received surgery on the day of admission. Although not formally quantified, patients with long in-patient delays were frequently starved on consecutive days in anticipation of going to theatre only to be cancelled later in the day due to a lack of theatre availability.
Following surgery, 29 patients (38%) were discharged the same day. These patients occupied 42 pre-operative bed-days. Only 16% of patients required a postoperative stay of greater than 1 day. Ten patients (13%) were managed as day-cases, i.e. being admitted, treated and discharged the same day.
November 2003
Following the inception of the hand-surgery day unit on 1 November 2003, a further study was performed analysing patients treated in the first month. During this period, 112 patients were identified. Two patients were excluded because of concomitant serious multiple injuries and one due to an in-patient stay of 44 days for medical reasons. Data were, therefore, collected on the remaining 109 patients.
During this second study period, 39 patients were sent home with the intention of planned day-case surgery. Five of these patients had their operations deferred and were admitted for logistical reasons or to allow medical optimisation. Of these five patients, four also incurred postoperative bed-days. Of the 70 patients admitted at presentation, eight received their operation the same day and four of these as day-cases.
Complications occurred in eight patients. Two of these occurred in patients treated as day-cases. One patient had an infected Kirschner wire requiring removal and antibiotics and the other had continued infection in an abscess cavity requiring further debridement. Three patients required additional fracture fixation following manipulation. Three patients developed wound infections that settled with antibiotics.
November 2004
The final study performed in this series occurred 12 months following the opening of the day-case unit. During November 2004 there were 90 patients identified.
Forty-eight (53%) patients were intended for day-case surgery during this time. One patient had the operation cancelled on admission due to previously undiagnosed hypertension and subsequently occupied 2 bed-days. Another patient was admitted from the day-case unit after surgery. This corresponds to an overstay rate of 2.1%. Eleven patients were discharged the day of their surgery but occupied pre-operative bed-days. Fifty-eight patients (64%) had no in-patient delay to theatre and, therefore, occupied no bed-days in waiting for their operation. Five patients required further intervention within 1 month, which included two patients treated as day-cases. An additional four patients were lost to follow-up.
Discussion
Hand injuries are common and the incidence is increasing.1 Strategies for managing patients with these injuries need to ensure a good standard of care and minimise the effects on elective surgery beds and operating lists. Day-case surgery is an effective modality for treating elective surgical patients2,3 and has also been described for patients with acute orthopaedic injuries.4 The number of patients presenting as an emergency is unpredictable and varies from month to month, as our study demonstrates. There is also the potential for the extent of injuries to be underestimated. We do believe, however, that patients with hand injuries lend themselves to day-case treatment for a number of reasons. As demonstrated in this study, hand trauma procedures are of relatively short duration and are most commonly performed on young, fit, ambulant patients (Table 1). These patients, therefore, have few co-morbidities to complicate the peri-operative period.
As required by The Royal College of Surgeons of England guidelines on day-case surgery,2 postoperative analgesia is achieved with simple oral analgesics. Day-case surgery does, of course, preclude regular postoperative intravenous antibiotics; however, in our experience, this is frequently unnecessary. This is borne out by a low postoperative infection rate of 3.7% (4 of 109). It is our practice to administer oral antibiotics pre- and postoperatively.
It is commonly felt that in-patient elevation of the injured limb pre- and postoperatively is beneficial to patients with hand injuries. Although data specific to hand injuries are lacking, one clinical trial of high arm elevation versus simple arm sling for patients who had undergone day-case carpal tunnel decompression failed to show any difference in volumetric analysis of swelling of the hand.5 This does, however, warrant further consideration in the trauma setting. One important, unanswered question is whether elevation to minimise oedema and commencement of hand therapy as an in-patient yields better functional results than day-case surgery. Also, it would be of interest to assess whether pain relief is significantly improved with overnight elevation in hospital.
We believe that this study is significant for a number of reasons. First, it demonstrates the value of auditing acute services to provide necessary information for the hospital management team to change service delivery, particularly when an existing service has an impact on elective surgical beds. It also demonstrates the importance of closing audit loops to ensure optimal efficiency. In this case, the first re-audit demonstrated that the day-case unit had a relatively low impact on the service. We believe that the act of presenting this audit within the department raised awareness of the service and led to increased uptake. Promotion of the service was extremely important. We believe that the day-case rate increased as confidence in the system grew and initial scepticism regarding patients waiting at home for surgery and being forgotten was unfounded. Our study also showed that complication rates are acceptable and conversion to in-patient care is an infrequent occurrence when appropriate care pathways are in place. A year after inception of the service, the overstay rate was 2%. This rate is comparable to the recommended target of less than 2% suggested by the Royal College of Anaesthetists6 and further supports the practice of day surgery for patients with acute hand injuries. The overstay rate for hand surgery is comparable to other specialities.3,7,8
The appointment of a dedicated senior nurse hand co-ordinator has been vital in the running of the hand day-unit. The role allows a point of contact for both patients and members of staff to ensure care pathways are appropriately utilised. Patients are given a mobile telephone number to contact both in the planning of their admission and during the postoperative period. A point of communication of this nature has been shown to increase patient satisfaction in the peri-operative period.9 The role also includes prioritisation of theatre time, production of theatre lists and maximising uptake of suitable patients for day-case surgery by working closely with junior doctors. There are now three hand co-ordinators in the department enabling the provision of weekend cover.
The initial audit demonstrated that a mean delay of 2 bed-days occurred prior to theatre and 38% of patients were ultimately discharged the same day of surgery, with a further 47% of patients being discharged the following day. This led to the hypothesis that a large proportion of these patients would be amenable to day-case care if appropriate care-pathways were introduced. This hypothesis was proved to be correct with the day-case rate achieving 51% in November 2004. This figure taken 12 months after the introduction of the service was a significant improvement when compared with 34% in November 2003 (first month after opening) and 13% in June 2002. As expected, this service reduced overnight bed occupancy by patients with hand injuries.
The introduction of the hand unit brought two new dedicated theatres. Previously, acute hand injuries were placed on a rolling list to be performed in a general emergency theatre. Shared theatre space led to the majority of hand injuries gaining low priority and a high risk of postponement. There are now planned all-day lists dedicated to hand surgery from Monday to Friday and a Saturday hand list. Elective hand surgery patients are also treated in this facility.
The Birmingham protocol (Fig. 1) incorporates The Royal College of Surgeons of England guidelines on day-case surgery.2 Those patients with poor social support, physical (ASA > 2) or mental health are deemed unsuitable. Complex injuries likely to require an operation of greater than 1 h or those patients requiring intravenous antibiotics are admitted.
At first glance it may be criticised that the patients who receive out-patient surgery have to wait longer than those admitted. On the other hand, it could be viewed that by sending patients with minor injuries home for planned day surgery, patients who require in-patient care with worse injuries receive their operations sooner and occupy fewer bed-days in waiting as overall the pre-operative in-patient delay has reduced (P < 0.001). Overall, the median time from presentation to operation has not significantly increased (P = 0.119; Table 3). This means that patients who need in-patient care and expedient surgery receive it and those with more minor injuries are managed as an out-patient with slightly longer delays but without the daily anxiety of waiting for surgery and prolonged starvation. Previously, patients were waiting in a hospital bed for surgery and were often starved all day on consecutive days in anticipation of going to theatre. Understandably, complaints occurred on a daily basis. The original audit in 2002 demonstrated that patients waited on a rolling list for up to 5 days before their operation. With patients waiting at home, they are not put at risk of hospital-acquired infections and do not occupy a hospital bed, which may prevent the admission of elective surgery patients.
The total bed-days per patient in November 2004 has halved when compared with the results from June 2002, thus halving the cost of in-patient stay in terms of bed-days. In-patient waiting times, in terms of bed-days have clearly reduced with the introduction of the day-case service.
The percentage of patients waiting one day or less for their operation was similar for all three audits (47% for 2002, 48% for 2003 and 37% for 2004). However, the range of time waited for surgery did increase in the latter two audits with higher percentage of patients undergoing day surgery, although delay was not significant (P = 0.119; Table 3). There is still room for improvement in this regard, although increasing capacity in an efficient manner is difficult in an unpredictable service.
No problems occurred with respect to recovery from anaesthesia. Admissions overnight were due to severity of injury and need for hospitalisation for elevation and intravenous antibiotics. During the study, the majority of these cases were performed under general anaesthesia, although we have recently introduced a regional block service to minimise risk and increase efficiency. Further audit of this is planned in the future.
The question remains as to whether the day-case trauma surgery rate of 51% achieved in the most recent study can be improved upon. Ultimately, there will always be a subset of patients who are not suitable for day-case surgery based upon the nature of their injury, concomitant illness, social circumstances and psychological factors. Our results compare favourably with a report from an established unit with day-case facilities quoting a 63% day-case trauma surgery rate that had remained unchanged over a 10-year period.1 This may, therefore, represent the gold standard that one can achieve for this population. Further audits will be conducted in the future to assess whether time is required for further uptake or whether increases in capacity are the only way of increasing day-case rates.
We are currently planning a study of patient satisfaction with the service, in particular, assessing patients' pain whilst waiting for surgery at home. It would also be important to assess functional recovery from specific injuries treated in this way, in light of the delays to theatre and lack of in-patient elevation. This would be particularly important for tendon injuries. We do not believe having treated many of these patients that rehabilitation is in any way hindered by this service. Day-case surgery in our unit does not preclude early hand therapy as there are therapy out-patient appointments every day (Monday to Friday).
Conclusions
Comparison of the three audits presented demonstrates that there is a period of evolution for a trauma day-case unit to reach maximum efficiency. It is important to perform audits at various time points to re-assess and potentially alter service provision and care pathways. Education and awareness of a service need to be high to ensure maximum efficiency and it is our view that the very act of performing and presenting audit results improves the use of such a service. We would recommend that other units in similar predicaments consider their policies of managing hand trauma patients and start by assessing in-patient bed occupancy. Although management of acute patients is outwith Government targets and often given low priority by management colleagues, demonstration of an impact on elective service provision is a powerful tool. We would also recommend that any new service has a dedicated nurse who acts as co-ordinator and who can offer advice to patients who are waiting at home. We hope that other units find our experiences useful given that it may be possible to apply this sort of service to other forms of ambulatory trauma.
Acknowledgments
The authors thank Mary McCarthy and Kim McCalister for their help throughout this series of audits and their continued contribution to the unit.
References
- 1.Burke FD, Dias JJ, Heras Palou C, Bradley MJ, Wildin C. Providing care for hand disorders a re-appraisal of need. J Hand Surg Br. 2004;29:575–9. doi: 10.1016/j.jhsb.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 2.The Royal College of Surgeons of England. Guidelines for day case surgery. London: RCSE; 1992. [Google Scholar]
- 3.Mandal A, Imran D, McKinnell T, Rao GS. Unplanned admissions following ambulatory plastic surgery – a retrospective study. Ann R Coll Surg Engl. 2005;87:466–8. doi: 10.1308/003588405X60560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Charalambous CP, Zipitis CS, Yarwood S, Hirst P. The development of a protocol in using day surgery for minor orthopaedic trauma patients. Ann R Coll Surg Engl. 2003;85:28–31. doi: 10.1308/003588403321001390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fagan DJ, Evans A, Ghandour A, Prabhkaran P, Clay NR. A controlled clinical trial of postoperative hand elevation at home following day-case surgery. J Hand Surg Br. 2004;29:458–60. doi: 10.1016/j.jhsb.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 6.Royal College of Anaesthetists. Unplanned hospital admission after day surgery. Raising the standard; day surgery services. 2nd edn. London: RCA; 2006. [Google Scholar]
- 7.Tewfik MA, Frenkiel S, Gasparrini R, Zeitouni A, Daniel SJ, et al. Factors affecting unanticipated hospital admission following otolaryngologic day surgery. J Otolaryngol. 2006;35:235–41. doi: 10.2310/7070.2006.0018. [DOI] [PubMed] [Google Scholar]
- 8.Tham C, Koh KF. Unanticipated admission after day surgery. Singapore Med J. 2002;43:522–6. [PubMed] [Google Scholar]
- 9.Rhodes L, Miles G, Pearson A. Patient subjective experience and satisfaction during the perioperative period in the day surgery setting: a systematic review. Int J Nurs Pract. 2006;12:178–92. doi: 10.1111/j.1440-172X.2006.00575.x. [DOI] [PubMed] [Google Scholar]