Abstract
INTRODUCTION
The objective of this study was to determine the safety and acceptability of the implementation of a day-case laparoscopic cholecystectomy (LC) service in a large UK teaching hospital, and analyse factors influencing contact with primary care providers. Wide-spread introduction of day-case LC in the UK is a major target of healthcare providers. However, few centres have reported their experience. In the US, out-patient surgery for LC has been reported, though many groups have utilised 24-h observation units to facilitate discharge. Concerns remain amongst surgeons regarding the feasibility and acceptability of the introduction of day-case LC in the UK.
PATIENTS AND METHODS
Comprehensive care and operative data were prospectively collected on the first 106 consecutive day-case procedures in our hospital. Postoperative recovery was monitored by telephone questionnaire on days 2, 5 and 14, including complications, satisfaction and general practitioner consultation.
RESULTS
A total of 106 patients were admitted for day-case LC, of whom 84% were discharged on the day of surgery. Patient satisfaction rate was 94% in both the successful day-case and the admitted patients. Mean operation time was 62 min, with an average total stay on the day-care unit of 426 min. Training-grade surgeons performed 31% of operations. Both the re-admission rate after surgery and rate of conversion to open surgery were 2%. Advice from primary healthcare providers was sought by 33% of patients within the first 14 postoperative days.
CONCLUSIONS
Introduction of day-case LC in the UK is feasible and acceptable to patients. The potential burden to primary care providers needs further study.
Keywords: Cholecystectomy, Laparoscopic, Day-case
Laparoscopic cholecystectomy (LC) is now widely accepted as the treatment of choice for symptomatic gallbladder disease.1 Improvements in operative and anaesthetic techniques, together with increased familiarity with the procedure have lead to progressively shorter hospital stay.1 The Department of Health has identified increased rates of day-case surgery as one of its key targets in the National Health Service plan for the UK.2 In order to achieve the target of 75% of operations being performed as day-cases, procedures such as LC will need to be introduced into most day-surgery units. However, little is known about the acceptability to patients and feasibility of the introduction of LC with same-day discharge in the UK.
Some recent publications have reported safe same-day discharge after LC, with complication and re-admission rates similar to those procedures performed on patients with overnight observation.3–8 However, there is little data on the difficulties of introducing this service to current day-case units in the UK, many of which will only have dealt with patients undergoing minor surgery. In addition, no studies have examined the potential burden to primary care providers in the early postoperative period.
Up to May 2004, our day-case unit had never performed a laparoscopic procedure. General surgical cases were confined to procedures such as herniorrhaphy or excision of lipomata. Prior to commencement of our day-case LC service, theatre and recovery day-case personnel spent several sessions training alongside experienced staff from our main theatre team. In June 2004, we started performing in-patient LC in the day-case unit twice a month on our normal day-case operating list. Staff from our main theatres initially worked alongside day-unit personnel to facilitate their training in the key skills of laparoscopic surgery. After an 11 month introductory period, the first true day-case was performed in May 2005. Subsequently, a prospective audit of all patients undergoing day-case LC was conducted. Comprehensive data have been collected on the surgical procedures, recovery period, postoperative pain and other problems. Factors influencing same-day discharge and contact with primary care providers have also been analysed.
Patients and methods
All patients listed for LC were considered for day surgery. This included patients seen in the out-patient clinic with symptoms consistent with biliary colic and an ultrasound scan confirming gallstones. In addition, patients admitted with acute biliary pain and/or cholecystitis which settled after conservative treatment were also considered for day-case surgery.
Patients with a body mass index (BMI) >?38 kg/m2, American Society of Anesthesiologists (ASA) score of 3 or more, complicated biliary disease (evidence of common bile duct stones or previous endoscopic retrograde cholangiogram, severe pancreatitis, recurrent admissions with cholecystitis), previous extensive abdominal surgery, or a history of severe postoperative nausea and vomiting were considered unsuitable for day-case surgery and excluded. However, patients with abnormal liver function tests, but a normal pre-operative magnetic resonance cholangiopancreatogram (MRCP) were eligible for day-case LC.
All patients were required to have a responsible adult available to accompany them home and stay with them for 48 h. A prospective database of all included patients was established and used to capture demographic, operative and peri-operative details throughout the day-case centre episode.
Operative technique
All patients were admitted on the day of surgery at 7:30 am having been nil-by-mouth from midnight. LC was commenced before 13:00 h with up to two cases performed on the morning operating list. Two consultant surgeons supervised all procedures, though the operating list was treated as a standard session, with no limits on the grade of primary operating surgeon. A standard four-port technique was used for LC, with open canulation using a 10-mm port through a sub-umbilical incision and three further ports – epigastric (10-mm) and two right upper quadrant (5-mm) – under laparoscopic vision. Intra-abdominal pressure was maintained below 12 mmHg and a careful 1-l saline lavage and suction was performed at the end of each procedure. On closure, 0.5% bupivicaine was administered to all the port sites according to safe weight-calculated doses. Antibiotic prophylaxis was not administered routinely, although was administered peri-operatively if there was a specific indication.
Anaesthetic/postoperative management
All patients received pre-operative paracetamol (1 g), diclofenac sodium (75 mg), ondansetron (4 mg) and clexane 20 mg an hour before surgery, unless contra-indicated. A standardised anaesthetic was utilised which included intravenous propofol and fentanyl (100 mcg) for induction and maintenance. All patients received intra-operative analgesia with morphine (10 mg). Intravenous fluids were given to maintain hydration. Combination intravenous anti-emetic therapy was given intra-operatively with cyclizine (50 mg) and dexamethazone (8 mg) to limit postoperative nausea and vomiting. On transfer to the post-anaesthetic care unit, intravenous fluids were discontinued if observations were satisfactory. In the recovery area, patients were encouraged to mobilise as soon as possible and offered diet and fluids as tolerated.
On discharge patients were provided with a supply of anti-emetic (domperidone 10–20 mg QDS) and an analgesic combination of paracetamol 1 g QDS, diclofenac sodium 50 mg TDS and codeine phosphate 30–60 mg 4-hourly. In those patients in whom non-steroidal anti-inflammatory drugs were contra-indicated, voltarol was substituted with tramadol 50–100 mg 4-hourly. Wound care advice and literature was given along with contact numbers for the day-care unit. Patients were also given details of how to contact the on-call surgical registrar in the event of experiencing severe symptoms as listed in their information booklet.
Telephone follow-up
In the first 2 weeks after surgery, all patients were telephoned on days 2, 5 and 14 by the day-case nursing staff and interviewed using a standardised questionnaire. Contact with healthcare professionals, patient satisfaction, pain and nausea control and any complications were recorded.
Statistical analysis
The probabilities of discharge and of contacting a healthcare practitioner in the first 2 weeks after surgery were modelled using chi-squared test, Mann–Whitney test and binary logistic regression. All explanatory variables, operative data and telephone phone-back answers were used in the statistical software package SPSS v.16.0 (LEAD technologies).
Results
Between May 2005 and May 2008, 106 patients underwent intended day-case LC in our hospital. All patients agreed to be managed as day-cases after receiving written pre-operative information. Demographic data are detailed in Table 1. The mean age at operation was 42 years (range, 19–76 years) and 87% of patients were female. The mean body mass index was 28 kg/m2 (range, 18–38 kg/m2) and mean weight 77 kg (range, 53–110 kg). Demographic factors were well matched between successfully discharged and admitted patients and did not influence successful day surgery. Despite our exclusion protocol, a number of patients attended who did not fulfil the criteria for day-case LC. Two patients had a history of postoperative nausea and vomiting, one patient had a history of chronic pain, one of sickle cell trait and one of previously abnormal liver function with no pre-operative MRCP. These patients all went ahead with their operation as planned, but affected our results as detailed below.
Table 1.
Demographic factors according to successful day surgery
| All patients (n = 106) | Successful day-case (n = 89) | Admitted (n = 17) | P-value | |
|---|---|---|---|---|
| Sex ratio M/F | 14/92 | 13/76 | 1/16 | 0.330a |
| Age (years) | 42 [19–76] | 41 [21–76] | 42 [19–64] | 0.653b |
| ASA-score 1 and 2 | 43/63 | 37/52 | 6/11 | 0.730a |
| Body mass index (kg/m2) | 28 [18–38] | 28 [18–38] | 28 [21–37] | 0.418b |
ASA, American Society of Anesthesiologists.
Chi-squared test
Mann–Whitney test.
Mean operating time for all patients was 6 2 min (range, 15–120 min). One-third of operations (31%) were carried out by training-grade surgeons. The policy in our unit is to perform pre-operative MRCP in patients with a history suggesting possible common bile duct stones. Therefore, we do not perform routine intra-operative cholangiograms (IOCs). However, IOCs were performed in two patients due to uncertain anatomy in one and abnormal LFTs with no pre-operative MRCP in the other; both were normal. There were two conversions to open operation. The first was due to difficult anatomy – IOC was not possible due to stones in the apparent cystic duct preventing canulation. The case was converted in order to assess anatomy fully. The other case was converted due to significant peri-cholecystic adhesions and bleeding from a cystic artery branch. Three patients had drains inserted: two were taken out 6 h after surgery and both patients were successfully discharged that day; the other patient was admitted overnight due to pain in the right upper quadrant and allowed home the following morning, once the drain was removed. Overall, 89 patients (84%) were successfully discharged on the day of surgery. Average duration of stay for successful day-case patients from start of operation to discharge was 426 min (range, 23 5–660 min). The reasons for admission of the other 17 patients are shown in Table 2.
Table 2.
Reason for overnight admission
| Reason for admission | Patients (n) |
|---|---|
| Oxygen saturation < 93% on air | 5 |
| Pain requiring parenteral opioid analgesia | 4 |
| Conversion to open operation | 2 |
| Drain inserted | 1 |
| Nausea and vomiting | 2 |
| Acute retention of urine (female) | 1 |
| Sinus tachycardia | 1 |
| History of sickle cell trait | 1 |
Admitted patients
In the group of five patients admitted with low oxygen saturations the median BMI was 32 kg/m2 (range, 29–37 kg/m2; P = not significant). Four of the other admissions could potentially have been avoided as they did not meet our entry criteria as described previously. One had suffered with chronic pain after a back injury and was taking regular opioid-based analgesics. On the morning of surgery, both the consultant surgeon and anaesthetist counselled the patient that she was unlikely to be discharged that day. The operation proceeded after consultation with the hospital bed manager. As predicted, her postoperative pain was difficult to manage and required intravenous opioid analgesia, eventually necessitating admission. The second avoidable admission was a patient with sickle cell trait which had been missed at the pre-assessment clinic. Our postoperative care protocol for such patients requires overnight admission for oxygen and fluid therapy. Otherwise, the patient was ambulatory 4 h after surgery and keen to go home. He met all other discharge criteria. The other two patients had a strong history of postoperative nausea and vomiting which was also missed at pre-assessment; both were admitted with emetic symptoms.
Of all the factors analysed, only the addition of a non-steroidal anti-inflammatory agent in the pre-medication was a significant factor in predicting successful day-case discharge. Other significant factors on univariate analysis included previously deranged liver function, postoperative hypotension requiring fluid bolus and low oxygen saturations, although none of these were significant on multivariate testing (Table 3).
Table 3.
Analysis of demographic and peri-operative factors and relation to the need for overnight admission
| All patients (n = 106) | Successful day-case (n = 89) | Admitted (n = 17) | P-value | ||
|---|---|---|---|---|---|
| UVA | MVA | ||||
| Age ≥ 60 years | 12 | 9 | 3 | 0.369 | NS |
| BMI ≥ 35 kg/m2 | 7 | 6 | 1 | 0.896 | NS |
| NSAID in pre-medication | 78 | 69 | 9 | 0.035 | 0.032 [OR = 9.178] |
| Operation by training grade surgeon | 33 | 26 | 7 | 0.329 | NS |
| Cholecystitis at operation/previous pancreatitis | 19 | 16 | 3 | 0.604 | NS |
| Previous deranged liver function | 5 | 3 | 2 | 0.017 | NS |
| Mean operation time min [range] | 62 [15–120] | 62 [15–120] | 66 [35–90] | 0.369b | NS |
| Operative complication/difficulty | 15 | 12 | 3 | 0.652 | NS |
| Operation commenced after 10 am | 30 | 26 | 4 | 0.634 | NS |
| Intravenous opiate in recovery | 43 | 34 | 9 | 0.257 | NS |
| Intravenous antiemetic in recovery | 10 | 10 | 0 | 0.146 | NS |
| Hypotension requiring fluid bolus | 6 | 3 | 3 | 0.020 | NS |
| O2 saturation < 95% in recovery | 20 | 13 | 7 | 0.010 | NS |
| Anti-emetic on the ward | 18 | 14 | 4 | 0.433 | NS |
NS, not significant; OR, odds ratio; UVA, univariate analysis; MVA, multivariate analysis. (P = chi-squared test in univariate and multiple logistic regression in multivariate analysis.)
Mann–Whitney test.
Re-admission
Two patients were re-admitted after successful day-case LC. One patient was re-admitted with abdominal pain on the second day after discharge. Investigations were unremarkable and her pain settled after 2 days on the ward. The other patient was re-admitted 5 days after surgery with pain in the right upper quadrant associated with pyrexia. Subsequent ultrasound scan revealed a collection which was inaccessible to percutaneous drainage. The patient was taken back to theatre and underwent laparotomy and washout of bile-stained fluid. No source could be found and a drain was left in situ. On-going biliary drainage necessitated endoscopic intervention with biliary stenting; subsequently, the patient made a full recovery.
Telephone follow-up
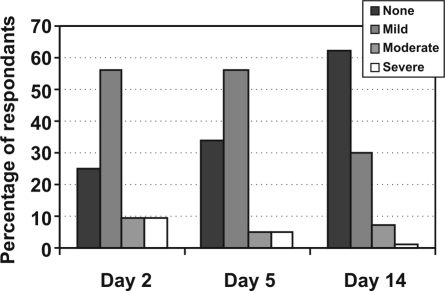
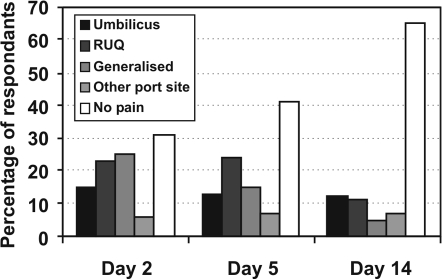
Figure 1 demonstrates postoperative pain responses. Overall, 86% of patients were contacted on all three phone-backs. Ninety patients had returned to normal activity by day 14 and the mean time taken to return to driving in those that were able was 10 days (range, 4–16). On day 2, pain and nausea were reported as none to mild by 85% and 99% of respondents, respectively.
Figure 1.
Percentage of patients experiencing pain on days 2, 5 and 14 according to (A) severity and (B) location.
There were 40 consultations by 35 patients with medical professionals in the first 14 days after operation (Table 4). Concerns regarding wound healing were the commonest reason for contact, although the majority of patients (11) were simply re-assured. In both the successful day-case patients, and those that were admitted, 94% were highly satisfied with the service they received. The remaining 6% commented that they would have felt‘safer’or‘more comfortable’in hospital overnight. Of these patients, three contacted their GP with wound concerns and all were re-assured without further treatment.
Table 4.
Reasons for patient contact with primary care providers or early out-patient appointment
| Day | Problem | Patients (n) | Healthcare provider | Action taken | ||
|---|---|---|---|---|---|---|
| GP | Walk-in centre | Out-patient clinic | ||||
| 2 | Sick note | 1 | 1 | – | – | Provided |
| Wound check | 1 | – | – | 1 | Re–assured | |
| 5 | Umbilical wound infection | 3 | 3 | – | – | Antibiotics |
| Minor skin dehiscence | 3 | 1 | 1 | 1 | None | |
| Constipation | 3 | 3 | – | – | Laxatives | |
| Wound check | 5 | 3 | 1 | 1 | None | |
| Analgesic review | 4 | 3 | 1 | – | Changed analgesics | |
| 14 | Umbilical wound infection | 7 | 6 | 1 | – | Antibiotics |
| Wound check | 3 | 3 | – | – | None | |
| Further sick note | 4 | 4 | – | – | Provided | |
| Removal of sutures | 4 | 3 | 1 | – | Removed | |
| Continued pre-operative symptoms | 2 | 2 | – | – | PPI | |
Discussion
The introduction of day-case LC in the UK presents healthcare providers with considerable challenges. Despite the available evidence relating to the safety of day-case LC, little is known as to the feasibility of its introduction in the UK population.8
Our day-case unit had never performed a laparoscopic procedure prior to the commissioning of this service. The provision of adequate staff education and training prior to full LC introduction is essential to the success of the service.9,10 Our day-case unit staff observed and participated during in-patient LC for a year prior to the first true day-case. Seminars were arranged in the use of laparoscopic equipment and in the differences of nursing care both in the operating theatre and recovery areas. All staff were invited to attend a service delivery meeting prior to commencement of the study, during which key personnel including surgical, anaesthetic and nursing lead practitioners gave presentations on the aims of the service and the study. We would recommend this strategy as we felt it gave all staff a feeling of involvement in the success of the service.
We recruited and successfully undertook day-case LC in 106 patients during the 3-year study period. There are several reasons behind the relatively low number of cases given the size of our unit. Only two consultants were willing to submit their patients to day-case operations and, initially, a dedicated day-case operating list was only available on a fortnightly basis. In addition, these day-case lists serve all day-case procedures for the two participating consultants, including herniorrhaphy and minor operations. Also, a small number of patients suitable for day-case LC turned the procedure down, preferring instead to have an overnight stay. These limitations, as well as the loss of patients to NHS initiative lists due to waiting time pressures, meant that we were unable to recruit as many patients as we would have anticipated in this time period.
We successfully discharged 84% of our patients on the day of surgery, in keeping with experience outside the UK.11–13 This figure could be improved to 89% by the exclusion of patients not meeting our day-case LC criteria. However, our analysis on an intention-to-treat basis represents a realistic appraisal of the true problems in setting up this service. Several authors have examined peri-operative factors in attempts to identify variables which might predict admission in order to allow selection of patients for day-case LC. Increasing age, ASA grade > 2, length of operation and previous cholecystitis or pancreatitis are among the indices identified by investigators as predictive of admission.11,14–16 However, several of these studies have failed to perform multivariate analyses, and other investigators in day-case LC have failed to show any correlation between peri-operative or demographic factors and admission in their patients.17 In our group, the only factor which independently predicted admission was the omission of diclofenac sodium from the pre-medication regimen (Table 5). Other variables such as previously deranged liver function, hypotension or hypoxaemia in the recovery area, although significant in univariate analysis, were not independently predictive of admission. Patient demographics, such as age, BMI and ASA score, were well matched between admitted and discharged patients and were unrelated to successful discharge.
Table 5.
Analysis of response to telephone feedback questions and relation to contact with a primary healthcare provider
| All patients (n = 106) | Contacted GP | No GP contact | P-value | ||
|---|---|---|---|---|---|
| UVA | MVA | ||||
| Admitted postoperatively | 17 | 5 | 12 | 0.730 | NS |
| Felt they had been discharged too soon | 6 | 5 | 1 | 0.007 | NS |
| Day 2 | |||||
| Any pain | 71 | 28 | 43 | 0.045 | NS |
| Moderate/severe pain | 15 | 9 | 6 | 0.016 | 0.006 [OR = 0.014] |
| Severe pain | 8 | 4 | 4 | 0.288 | NS |
| Any nausea | 14 | 7 | 7 | 0.147 | NS |
| Unable to tolerate diet | 22 | 5 | 17 | 0.249 | NS |
| Day 5 | |||||
| Any pain | 59 | 23 | 36 | 0.143 | NS |
| Moderate/severe pain | 9 | 3 | 6 | 0.983 | NS |
| Using regular analgesia | 40 | 12 | 28 | 0.607 | NS |
| Nausea | 17 | 7 | 10 | 0.435 | NS |
| Wound problems | 10 | 9 | 1 | < 0.001 | NS |
| Unable to tolerate diet | 21 | 6 | 15 | 0.628 | NS |
| Day 14 | |||||
| Any pain | 35 | 18 | 17 | 0.005 | NS |
| Moderate/severe pain | 7 | 3 | 4 | 0.567 | NS |
| Severe pain | 1 | 0 | 1 | 0.481 | NS |
| Nausea | 4 | 2 | 2 | 0.462 | NS |
| Wound problems | 25 | 21 | 4 | < 0.001 | < 0.001 [OR = 0.011] |
| Unable to tolerate diet | 17 | 2 | 15 | 0.042 | NS |
| Not returned to normal activity | 21 | 6 | 15 | 0.628 | NS |
NS, not significant; OR, odds ratio; UVA, univariate analysis; MVA, multivariate analysis. (P = chi-squared test in univariate and multiple logistic regression in multivariate analysis.)
The acceptability of same-day discharge has been reported in populations outside the UK, with satisfaction rates varying from 71–95%.4,17–21 In this study, 94% of patients were highly satisfied with the service we provided, both in the discharged and admitted groups. Sixteen significant intra-operative difficulties in 15 patients were encountered (Table 6). However, neither operative complications or difficulties, nor evidence of cholecystitis at operation affected successful discharge. Despite these cases, our conversion rate to open operation of 2% compares well with the literature.11,12,14
Table 6.
Intra-operative difficulties and outcomes
| Intra-operative difficulty/complication | Patients (n) | Outcome | |
|---|---|---|---|
| Anaesthetic/medical | |||
| Tachycardia/bradycardia | 2 | Resolved | |
| Hypertension | 1 | Labetolol infusion | |
| Surgical | |||
| Bleeding | 1 | Converted to open | |
| Anatomical difficulty | 1 | Converted to open | |
| Empyema/mucocele | 4 | Completed laparoscopically | |
| Port site bleed | 2 | Sutured (1), diathermy (1) | |
| Adhesions | 4 | Completed laparoscopically | |
| Wide cystic duct | 1 | Endo-loop applied | |
In ophthalmic surgery, the utilisation of day-case lists has increased surgical throughput and. consequently. the numbers of cases available for training.22 There appears to be no reason why this cannot also be the case for LC. A third of the operations presented here were performed by junior surgeons. Contrary to other reports, we found no correlation between grade of operating surgeon and admission on univariate or multivariate analysis.13,17 This should encourage service providers to maintain or increase training opportunities for surgeons, despite the introduction of day-case LC.
Along with high satisfaction rates, it is clear from our postoperative telephone survey that the patients recovered well after surgery, with 85% of patients returning to normal activity by day 14, comparable to the results of Hollington and colleagues6 in their day case series. When the published evidence examining recovery after LC was reviewed, the length of convalescence appeared very variable and influenced by multiple factors.23,24 Return to full activity in our study is certainly equivalent to many of these series, and comparison with in-patient LC in a large, randomised, controlled trial may reveal a benefit. Pain and nausea also appeared well controlled in our patients in comparison to published series.4,11 To date, no authors have examined the burden on primary care providers after day-case LC. Our results indicate that 33% of patients contacted a healthcare professional within 14 days of surgery for an unplanned consultation. No data exist on consultation rates amongst in-patient LC groups, but we feel this rate seems excessive. Accordingly, we have initiated a telephone survey of patients receiving in-patient LC as a comparison group.
On multivariate analysis of independently predictive factors for contact with healthcare providers, the presence of moderate or severe pain on day 2 or wound problems by day 14 were significant. Patients in these two groups would be of concern to the surgical team. However, the majority of requests for consultation were regarding perceived wound problems (n = 21), and half of these patients were merely re-assured. This highlighted a need for better pre-operative counselling and information. We have subsequently introduced further written and oral information into the patient pathway with regard to the nor mal progress of wound healing.
Conclusions
Our experience demonstrates that the introduction of day-case LC in the UK is both feasible and acceptable to patients. The difficulties in predicting admission based on demographic or peri-operative factors will present significant challenges to service providers. Further evaluation of patient satisfaction at 6 weeks post surgery and their suggestions for service development may identify other important factors influencing same-day discharge. In addition to the variables analysed, we felt the single most important factor influencing discharge and satisfaction rates was education of both the staff and patients.
Acknowledgments
The authors would like to thank all the staff at the Royal Hallamshire Hospital day-case unit.
References
- 1.Keus F, de Jong JA, Gooszen HG, van Laarhoven CJ. Laparoscopic versus open cholecystectomy for patients with symptomatic cholecystolithiasis. Cochrane Database Syst Rev. 2006;(4) doi: 10.1002/14651858.CD004788.pub2. CD006231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Department of Health. The NHS Plan: a plan for investment, a plan for reform. London: London, DH; 2000. [Google Scholar]
- 3.Johansson M, Thune A, Nelvin L, Lundell L. Randomized clinical trial of day-care versus overnight-stay laparoscopic cholecystectomy. Br J Surg. 2006;93:40–5. doi: 10.1002/bjs.5241. [DOI] [PubMed] [Google Scholar]
- 4.Keulemans Y, Eshuis J, de Haes H, de Wit LT, Gouma DJ. Laparoscopic cholecystectomy: day-care versus clinical observation. Ann Surg. 1998;228:734–40. doi: 10.1097/00000658-199812000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dirksen CD, Schmitz RF, Hans KM, Nieman FH, Hoogenboom LJ, Go PM. [Ambulatory laparoscopic cholecystectomy is as effective as hospitalization and from a social perspective less expensive: a randomized study] Ned Tijdschr Geneeskd. 2001;145:2434–9. [PubMed] [Google Scholar]
- 6.Hollington P, Toogood GJ, Padbury RT. A prospective randomized trial of day-stay only versus overnight-stay laparoscopic cholecystectomy. Aust NZ J Surg. 1999;69:841–3. doi: 10.1046/j.1440-1622.1999.01713.x. [DOI] [PubMed] [Google Scholar]
- 7.Young J, O'Connell B. Recovery following laparoscopic cholecystectomy in either a 23 hour or an 8 hour facility. J Qual Clin Pract. 2001;21:2–7. doi: 10.1046/j.1440-1762.2001.00399.x. discussion 8. [DOI] [PubMed] [Google Scholar]
- 8.Gurusamy K, Junnarkar S, Farouk M, Davidson BR. Meta-analysis of randomized controlled trials on the safety and effectiveness of day-case laparoscopic cholecystectomy. Br J Surg. 2008;95:161–8. doi: 10.1002/bjs.6105. [DOI] [PubMed] [Google Scholar]
- 9.Gilmartin J, Wright K. The nurse's role in day surgery: a literature review. Int Nurs Rev. 2007;54:183–90. doi: 10.1111/j.1466-7657.2007.00528.x. [DOI] [PubMed] [Google Scholar]
- 10.Mitchell M. Nursing intervention for day-case laparoscopic cholecystectomy. Nurs Stand. 2007;22:35–41. doi: 10.7748/ns2007.10.22.6.35.c4641. [DOI] [PubMed] [Google Scholar]
- 11.Psaila J, Agrawal S, Fountain U, Whitfield T, Murgatroyd B, et al. Day-surgery laparoscopic cholecystectomy: factors influencing same-day discharge. World J Surg. 2008;32:76–81. doi: 10.1007/s00268-007-9225-x. [DOI] [PubMed] [Google Scholar]
- 12.Sherigar JM, Irwin GW, Rathore MA, Khan A, Pillow K, Brown MG. Ambulatory laparoscopic cholecystectomy outcomes. JSLS. 2006;10:473–8. [PMC free article] [PubMed] [Google Scholar]
- 13.Proske JM, Dagher I, Revitea C, Carloni A, Beauthier V, et al. Day-case laparoscopic cholecystectomy: results of 211 consecutive patients. Gastroenterol Clin Biol. 2007;31:421–4. doi: 10.1016/s0399-8320(07)89403-6. [DOI] [PubMed] [Google Scholar]
- 14.Rathore MA, Andrabi SI, Mansha M, Brown MG. Day case laparoscopic cholecystectomy is safe and feasible: a case controlled study. Int J Surg. 2007;5:255–9. doi: 10.1016/j.ijsu.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 15.Lau H, Brooks DC. Predictive factors for unanticipated admissions after ambulatory laparoscopic cholecystectomy. Arch Surg. 2001;136:1150–3. doi: 10.1001/archsurg.136.10.1150. [DOI] [PubMed] [Google Scholar]
- 16.Simpson JP, Savarise MT, Moore J. Outpatient laparoscopic cholecystectomy: what predicts the need for admission? Am Surg. 1999;65:525–8. discussion 529. [PubMed] [Google Scholar]
- 17.Bona S, Monzani R, Fumagalli Romario U, Zago M, Mariani D, Rosati R. Outpatient laparoscopic cholecystectomy: a prospective study of 250 patients. Gastroenterol Clin Biol. 2007;31:1010–5. doi: 10.1016/s0399-8320(07)78322-7. [DOI] [PubMed] [Google Scholar]
- 18.Willsher PC, Urbach G, Cole D, Schumacher S, Litwin DE. Outpatient laparoscopic surgery. Aust NZ J Surg. 1998;68:769–73. doi: 10.1111/j.1445-2197.1998.tb04673.x. [DOI] [PubMed] [Google Scholar]
- 19.Lillemoe KD, Lin JW, Talamini MA, Yeo CJ, Snyder DS, Parker SD. Laparoscopic cholecystectomy as a ‘true’ outpatient procedure: initial experience in 130 consecutive patients. J Gastrointest Surg. 1999;3:44–9. doi: 10.1016/s1091-255x(99)80007-9. [DOI] [PubMed] [Google Scholar]
- 20.Calland JF, Tanaka K, Foley E, Bovbjerg VE, Markey DW, et al. Outpatient laparoscopic cholecystectomy: patient outcomes after implementation of a clinical pathway. Ann Surg. 2001;233:704–15. doi: 10.1097/00000658-200105000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fleisher LA, Yee K, Lillemoe KD, Talamini MA, Yeo CJ, et al. Is outpatient laparoscopic cholecystectomy safe and cost-effective? A model to study transition of care. Anesthesiology. 1999;90:1746–55. doi: 10.1097/00000542-199906000-00033. [DOI] [PubMed] [Google Scholar]
- 22.Tey A, Grant B, Harbison D, Sutherland S, Kearns P, Sanders R. Redesign and modernisation of an NHS cataract service (Fife 1997–2004): multifaceted approach. BMJ. 2007;334:148–52. doi: 10.1136/bmj.39050.520069.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bisgaard T, Kehlet H, Rosenberg J. Pain and convalescence after laparoscopic cholecystectomy. Eur J Surg. 2001;167:84–96. doi: 10.1080/110241501750070510. [DOI] [PubMed] [Google Scholar]
- 24.Majeed AW, Troy G, Nicholl JP, Smythe A, Reed MW, et al. Randomised, prospective, single-blind comparison of laparoscopic versus small-incision cholecystectomy. Lancet. 1996;347:989–94. doi: 10.1016/s0140-6736(96)90143-9. [DOI] [PubMed] [Google Scholar]