Abstract
INTRODUCTION
The advent of the image intensifier has revolutionised trauma surgery since its development in 1955. The manufacturers have given names to various movements of the machine in the operating manual but it has not been popular among orthopaedic surgeons or radiographers. Lack of knowledge of names of various movements and ambiguity in command often leads to confusion between the surgeon and the radiographer regarding which way to move the image intensifier. A questionnaire-based study was conducted to assess the efficacy of communication between orthopaedic surgeons and radiographers while using the image intensifier intra-operatively.
SUBJECTS AND METHODS
Diagrams depicting the movements of the image intensifier were used in the questionnaire. Fifty questionnaires were given to orthopaedic surgeons and 50 to radiographers to name the various movements.
RESULTS
Ninety questionnaires were returned, 45 from surgeons and 45 from radiographers. Five questionnaires from surgeons and five from radiographers were returned blank. Of those responding, 97% could name the vertical movement, 68% the horizontal movement, 12% the swivel and 29% the angulation movement. None could name the orbital movement.
CONCLUSIONS
Even though orthopaedic surgeons do not operate the image intensifier themselves, knowledge of the movements of the image intensifier and their names can improve the efficacy of communication between surgeons and radiographers. A common language and precision in command can avoid confusion and has the potential to improve theatre time utilisation. The nomenclature of various movements of the image intensifier has been described and possible precise commands for various movements have been postulated.
Keywords: Image intensifier, C-arm, Language for communication, Nomenclature, Movements of image intensifier
Since its advent in 1955, the image intensifier has become an essential component of theatre equipment especially for trauma surgery. Manufacturers have given names to the various movements of the image intensifier in operating manuals but these have not been popular among orthopaedic surgeons or radiographers.1
True anteroposterior or lateral views are not always easy to obtain because of the topography or patient position and, on many occasions, may not be the most desired views. Most orthopaedic surgeons help their radiographers by asking them to move the image intensifier in specific directions and to perform specific movements to get the desired view of the part being operated on. This is most often done by informal, but imprecise, commands like ‘please move this way’, ‘move like this please’, ‘up/down’, ‘left/right’ or ‘higher/lower’. Whilst this works sometimes, such imprecision can create confusion and frustration for both the surgeon and the radiographer. On odd occasions, other theatre staff and the anaesthetist also get involved in helping the radiographer to interpret what the surgeon wants correctly. This results in loss of valuable theatre time for the want of a better language of communication between the surgeon and the radiographer.
Trehan and Tennent2 demonstrated the lack of consensus among orthopaedic surgeons and between surgeons and radiographers with regards to what commands should be used to perform a specific movement of image intensifier. Uniformity in command for specific movements of the image intensifier across the specialty is highly desirable. We believe the problem is compounded by the lack of knowledge of the names of various movements and their use in the command.
The aims of this study were to define the lack of knowledge of nomenclature of various movements of ‘the image intensifier’ among orthopaedic surgeons and radiographers and to develop an unambiguous language in the operating theatre appertaining to the use of image intensifier.
Subjects and Methods
A questionnaire consisting of diagrams of five movements of the image intensifier (Fig. 1) was designed. Fifty questionnaires each were given to orthopaedic surgeons and radiographers. Amongst 50 surgeons, 20 were consultants, 15 were middle-grade surgeons and 15 were senior house officers familiar with the use of an image intensifier. They were asked to name the movements of the image intensifier illustrated in the diagrams. The questionnaire was supplied to them during a coffee break in their departmental audit meeting and was collected at the end of the meeting. This did not allow referral to any study material.
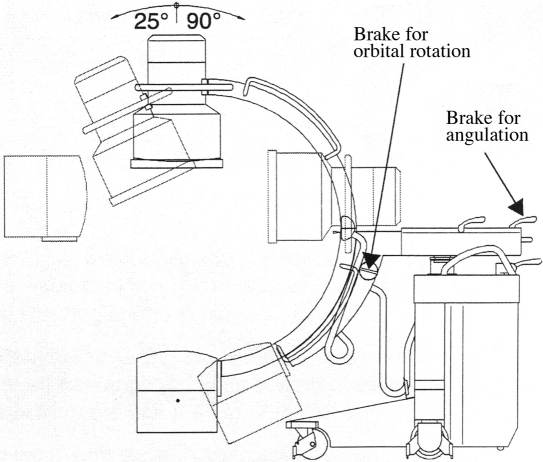
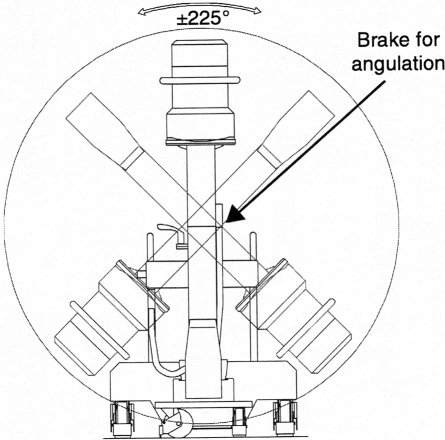
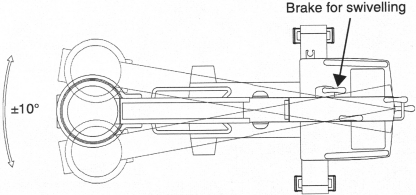
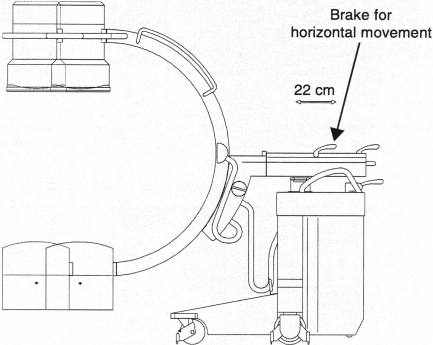
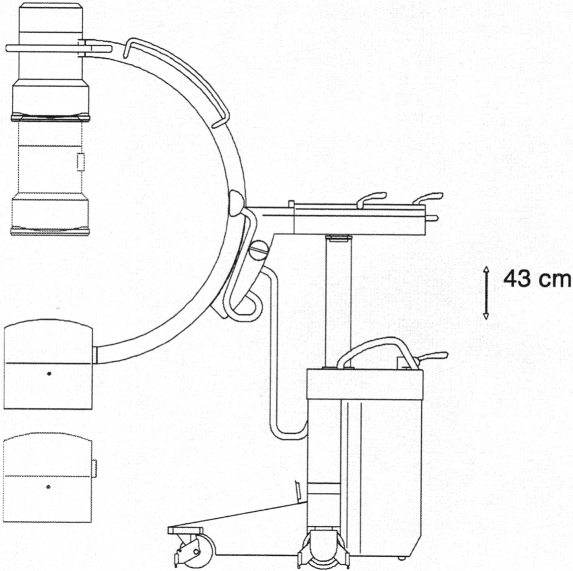
Figure 1.
Diagrams showing (A) orbital, (B) angulation, (C) swivel, (D) horizontal and (E) vertical movement of the image intensifier (reprinted from Ziehm Vista User Manual 26355-4.20.EN.01, Figs 9–13, 2003; 34–7, with permission of the publisher Instrumentarium Imaging Ziehm GmbH).
Responses were analysed using Microsoft Excel software.
Results
Ninety questionnaires were returned, 45 from surgeons and 45 from radiographers (Table 1). Surgeons consisted of 18 consultants, 12 middle-grade surgeons and 15 senior house officers making a total of 45. The horizontal and vertical movements were correctly named by most of the surgeons (38 and 43, respectively) and radiographers (23 and 44, respectively). None of the surgeons or the radiographers could name the orbital movement. Radiographers were much better than the surgeons in naming angulation movement (3 and 23, surgeons versus radiographers). Overall, radiographers were better than surgeons in recognising and naming the movements of the image intensifier. Interestingly, only two consultants were able to recognise swivel movement of which one consultant answered it as Wig-Wag movement, the classic name for swivel movement.
Table 1.
Number of correct responses
| Surgeons (out of 45) | Radiographers (out of 45) | Total (out of 90) | |
|---|---|---|---|
| Orbital | 0 | 0 | 0 |
| Angulation | 3 (6.6%) | 23 (51%) | 26 (28.9%) |
| Swivel (Wig-Wag) | 5 (11%) | 6 (13%) | 11 (12.2%) |
| Horizontal | 38 (84%) | 23 (51%) | 61 (67.8%) |
| Vertical | 43 (95%) | 44 (97%) | 87 (96.6%) |
Discussion
The results of this study show that an average of 97% of the surgeons and the radiographers were familiar with the name of vertical movement and 68% were familiar with that of horizontal movement. Radiographers were better than surgeons in recognising and naming angulation movement but, surprisingly, were equally unfamiliar with the names of swivel and orbital movements. It is important to clarify here that horizontal movement is referred to here as only the movements performed by protracting or retracting the arm with the wheels locked. Movements in any direction on the wheels are also horizontal but must be clearly specified as ‘on the wheels’. Swivel movements are also, in fact, horizontal but are along an arc rather than a straight line.
It is important to use the names of the various movements of the image intensifier to communicate effectively with the radiographers in operating theatre. Much time and effort could be saved if trainees learn this art early in their training. This responsibility should rest with the consultant surgeon and senior radiographers as the team leaders. The problem requires greater debate from both radiographers and the surgeons.
Commands to move the image intensifier should be precise. ‘Horizontal movement towards patient's head or foot’ (when the image intensifier is approaching from head or foot end of the patient) and ‘horizontal movement towards patient's left or right’ (when the image intensifier is on one side of the patient) should be used rather than ‘upwards and downwards’ or ‘to the left or to the right’. ‘Vertical movement towards the ceiling or the floor’ is an unambiguous expression and should be used rather than saying ‘up and down’ or ‘higher and lower’. In orbital and angular movements, the direction should include either the source or the receptor of the X-rays to avoid confusion (e.g. ‘orbital movement with the source of the X-rays towards the patient's left’ or ‘angulation movement with the source of X-rays towards the patient's foot’; (Table 2). We suggest that the commands for the image intensifier movements should be referred to the source of the X-rays and body of the patient. Imperative without accusative leads to ambiguity and must be avoided. The surgeon should quickly find out which of the request words has the minimum ‘no response’ rate from the radiographers. ‘Screen please’ has been noted to be popular and effective among the radiographers. Shoot, picture, image, etc. are less effective alternatives.
Table 2.
Examples of possible precise commands for various movements
| Name of movement | Direction of movement | |||
|---|---|---|---|---|
| ‘On the wheels’ | Towards patient's head | Towards patient's foot | Towards patient's right | Towards patient's left |
| Vertical | Towards ceiling | Towards floor | ||
| Image intensifier on the head or the foot end | Image intensifier on one side | |||
| Horizontal | Towards patient's head | Towards patient's foot | Towards patient's right | Towards patient's left |
| Swivel | Towards patient's right | Towards patient's left | Towards patient's head | Towards patient's foot |
| Orbital with X-ray source | Towards patient's head | Towards patient's foot | Towards patient's right | Towards patient's left |
| Angulation with X-ray source | Towards patient's right | Towards patient's left | Towards patient's head | Towards patient's foot |
The surgeon should also familiarise himself or herself with the image intensifier enough to know which handle allows which movement and how much movement is possible in which direction (Fig. 1).
Trehan and Tennent2 presented their work in a specialist meeting showing the lack of consensus with regards to commands for specific movements but their work included only vertical and horizontal movements. The present study is more comprehensive, includes other three commonly used movements and highlights the fact that the level of ignorance is much higher than one might imagine.
The adoption of a common language between surgeons and radiographers has the potential to save valuable theatre time and, hence, improve theatre throughput (utilisation). It can also reduce unnecessary radiation exposure to patients and make the working environment in theatre less confusing and frustrating.
References
- 1. Instrumentarium Imaging Ziehm GmbH. Ziehm Vista User Manual 26355-4.20.EN.01, Figs 9–13, 2003; 34–7 < www.ziehm.com/>.
- 2.Trehan R, Tennent TD. Which way is up? The control of image intensifier movement in the operating theatre. J Bone Joint Surg Br. 2006;88(Suppl II):277. [Google Scholar]
- 3.Kreienfeld H, Klimpel H, Bottcher V. Use of X-rays in operating suite. In: Aschemann D, Krettek C, editors. Positioning Techniques in Surgical Applications. vol. 4.2. Berlin: Springer; 2006. pp. 37–9. [Google Scholar]