Abstract
Intussusception in adults is a rare cause of abdominal pain. Unlike its paediatric counterpart, intussusception in adults is associated with obvious pathology. We describe a case of ileocolic intussusception extending to the splenic flexure. We were able to reduce the intussusception partially and pedicle was stapled carefully. The specimen was delivered through a small incision and right hemicolectomy was performed adhering to oncological principles. We recommend laparoscopic-assisted surgery is considered for adult intussusceptions.
Keywords: Laparoscopy, Hemicolectomy, Ileocolic intussusception, Caecal neoplasm
Case history
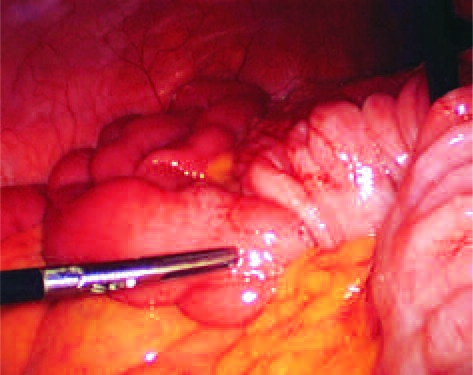
A 69-year-old woman was admitted with abdominal pain. There was no history of change in bowel habit or weight loss. Clinical examination revealed a lump in the left upper quadrant. Haematological investigations and plain abdominal X-rays were unremarkable. An abdominal computed tomography (CT) scan was suggestive of ileocolic intussusception extending to the splenic flexure (Fig. 1). These findings were confirmed at laparoscopy, with the intussuscipiens lying in the transverse colon (Fig. 2). Gentle traction on the terminal ileum and then appendix partially reduced the intussusception. The ileocolic pedicle was isolated and divided after a conventional medial to lateral dissection. The right colon was mobilised easily and a laparoscopic assisted right hemicolectomy was performed (stapled extracorporeal anastomoses). On opening the specimen, a cauliflower like caecal polyp was found. The patient was discharged on the third postoperative day. Histology revealed a T3N0 mucinous adenocarcinoma with clear resection margins.
Figure 1.
Abdominal CT scan showing ileocolic intussusception extending to the splenic flexure.
Figure 2.
Ileocolic intussusception being reduced at laparoscopy.>.
Discussion
Intussusception in adults is a rare cause of abdominal pain. In a large series over 20 years, of 292 patients diagnosed with intussusception, only 8.2% patients were adults.1 Common sites of intussusception are the junctions of mobile and immobile bowel segments, i.e. ileocolic, rectosigmoid junction.
Clinical diagnosis is difficult and is often made on radiological investigation. Unlike its paediatric counterpart, intussusception in adults is associated with obvious pathology such as submucosal lipoma, polyp, Meckel's diverticulum or band in more than 85% of cases.2 In one series of 27 adult patients operated for intussusception, there were 22 small bowel and 5 colonic lesions. A pathological cause was identified in 85% of patients with 8 of 22 (36%) small bowel and 4 of 5 (80%) of large bowel lesions being malignant.2
Laparoscopic surgery is well established for routine colorectal procedures while laparoscopic management for emergency colorectal procedures such as acute complicated diverticulitis is gaining popularity.3,4 Given that laparoscopic management of paediatric intussusception has been available for some time5 and the long-term safety of laparoscopic resection for colorectal cancer is well established, laparoscopic-assisted surgery was an obvious option in this case.
In paediatric intussusception, laparoscopic reduction and pexy is performed with a conversion rate of about 30% due to the inability to reduce the intussusception.5 In adults, a laparoscopic-assisted procedure entails mobilisation and delivering the specimen with an extracorporeal anastomosis in most patients. If it is difficult to reduce the intussusceptions in situ, the specimen can be mobilised after taking the pedicle. This requires utmost care and an experienced laparoscopic surgeon as the normal vascular anatomy may be distorted due to the intussusception. In our case, we were able to reduce the intussusception partially and pedicle was stapled carefully. The specimen was delivered through a small incision and right hemicolectomy was performed adhering to oncological principles.
Conclusion
We recommend laparoscopic-assisted surgery is considered for adult intussusceptions.
References
- 1.Wang LT, Wu Yu JC, Hsiao CW, Hsu CC, Jao SW. Clinical entity and treatment strategies for adult intussusceptions: 20 years' experience. Dis Colon Rectum. 2007;50:1941–9. doi: 10.1007/s10350-007-9048-8. [DOI] [PubMed] [Google Scholar]
- 2.Eisen LK, Cunningham JD, Aufses AH., Jr Intussusception in adults: institutional review. J Am Coll Surg. 1999;188:390–5. doi: 10.1016/s1072-7515(98)00331-7. [DOI] [PubMed] [Google Scholar]
- 3.Kuhry E, Schwenk W, Gaupset R, Romild U, Bonjer J. Long-term outcome of laparoscopic surgery for colorectal cancer: a Cochrane systematic review of randomised controlled trials. Cancer Treat Rev. 2008;34:498–504. doi: 10.1016/j.ctrv.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 4.Myers E, Hurley M, O'Sullivan GC, Kavanagh D, Wilson I, Winter DC. Laparoscopic peritoneal lavage for generalized peritonitis due to perforated diverticulitis. Br J Surg. 2008;95:97–101. doi: 10.1002/bjs.6024. [DOI] [PubMed] [Google Scholar]
- 5.Bonnard A, Demarche M, Dimitriu C, Podevin G, Varlet F, François M, et al. GECI (Groupe d'Etude de Coelioscopie Pédiatrique). Indications for laparoscopy in the management of intussusception: a multicenter retrospective study conducted by the French Study Group for Paediatric Laparoscopy (GECI) J Pediatr Surg. 2008;43:1249–53. doi: 10.1016/j.jpedsurg.2007.11.022. [DOI] [PubMed] [Google Scholar]