Abstract
INTRODUCTION
Acute appendicitis remains a common surgical condition and the importance of specific elements in the clinical diagnosis remain controversial. A variety of neoplastic and inflammatory conditions mimic acute appendicitis. The purpose of this study was to determine the presenting pattern of acute appendicitis and to review the pathological diagnosis.
PATIENTS AND METHODS
This is a retrospective analysis of 324 patients who had appendicectomy for acute appendicitis at Prince Mshiyeni Memorial Hospital (Natal, South Africa) during the period January 2002 to December 2004. Patient demographics, clinical features, white cell count, operative findings, outcome and histology results were recorded on a special patient proforma.
RESULTS
A total of 371 patients underwent appendicectomy during this period and 324 (M:F, 3.6:1) were available for analysis. The majority of our patients were in the second decade (43.1%) with only 29.3% presenting within 24 h of onset of symptoms. The most common symptoms were abdominal pain (100%), vomiting (57.4%) and anorexia (49.0%). Generalised and localised abdominal tenderness were present in 62.0% and 19.4% of patients, respectively. Pyrexia was noted in 41.0%. Localised and generalised peritonitis were present in 26.4% and 14.0%, respectively. The most common incisions were lower midline laparotomy (47.2%) and gridiron (37.3%). The negative appendicectomy rate was 17.0%. Acute appendiceal inflammation and gangrenous appendicitis was present in 36.1% and 9.6%, respectively. The perforation rate was 34.0% and there was a direct correlation with delayed presentation. There were no patients with carcinoid tumour or adenocarcinoma. Parasites and other associated conditions were seen in 8.6% of cases. Postoperative complications included: wound sepsis (25.3%), prolonged ileus (6.2%), peritonitis (4.6%) and chest infection (3.4%). Four patients died (1.2%) all from the perforated group.
CONCLUSIONS
Our patients present late with advanced disease and complications. All surgeons should bear in mind the possibility of parasitic infestations mimicking acute appendicitis and the presence of significant unusual histological findings in our setting justifies routine histopathological examination of appendices.
Keywords: Appendicitis, Histology, Audit
Suspected acute appendicitis remains the most frequent cause for emergency operations in gastrointestinal surgery. The pathological spectrum of the acutely inflamed appendix encompasses a wide spectrum of infectious and non-infectious conditions and the variations in the pathophysiological development of the disease explain why barely half of patients have a classical history on presentation. A number of non-appendiceal pathologies in the right iliac fossa can mimic appendicitis and, as such, a significant number of appendicectomies are being performed for non-appendiceal pathologies. This retrospective review was performed to determine the clinical patterns of acute appendicitis and to document the type of pathology found in appendicectomy specimens at our institution.
Patients and Methods
Patients
The clinical and pathological reports of 324 patients undergoing surgery for suspected acute appendicitis between January 2002 and December 2004 were retrospectively reviewed. Incidental appendicectomies and appendicular inflammatory masses that resolved on conservative management were excluded from this study. Information entered included patient demographics, clinical symptoms and signs, duration of symptoms, white cell count (WCC) level, type of incisions and operative findings, histological findings, postoperative complications and outcome. Appendicectomy was indicated when there was a high suspicion of acute appendicitis, based on symptoms and signs. WCC was used as a complementary finding and ultrasound scan was performed only when the clinical findings were equivocal. All specimens were routinely examined morphologically, and the final diagnosis was based on histology.
Definitions and histology
The histopathology reports were studied for details of the gross and microscopic characteristics of the specimens with special staining for selected specimens. Acute appendicitis is defined as the presence of transmural inflammation or pus in the lumen of the appendix.1 Negative appendicectomy is defined as one which is performed for a clinical diagnosis of acute appendicitis but where the appendix is found to be normal on histopathological examination. This includes a histologically normal appendix with or without the presence of faecolith or parasites in the lumen.
Incidental appendicectomy is defined as the removal of a normal appendix along with treatment of another pathology to avoid confusion of diagnosis of appendicitis later or to prevent metachronous metastasis in malignancy.1 A diagnosis of peritonitis is made if the exudate extends into the fibrofatty tissues of the meso-appendix. Non-perforated appendicitis was defined as an inflamed appendix without evidence of macroscopic perforation.
Results
Demographics
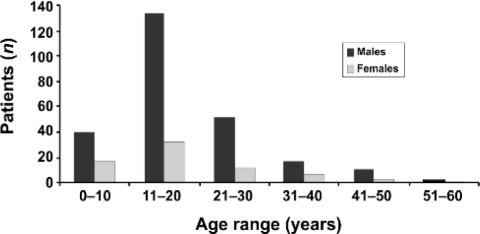
A total of 371 patients underwent appendicectomy during the study period and 324 (M:F, 3.6:1) were available for clinical and pathological analysis. The majority of patients were in the second decade (43.1%; Fig. 1). A total of 173 males and 49 females were below the age of 20 years.
Figure 1.
Age and gender distribution of patients with acute appendi
Clinical features
SYMPTOMS
The most common complains were abdominal pain (100%), vomiting (57.4%) and anorexia (49.0%; Table 1). Diarrhoea was present in 18.2% and 11.1% of patients had appendix abscesses. Three patients (0.9%) presented with a history of vomiting or passing worms in stools. Only 29.3% of patients presented within 24 h of onset of symptoms and the mean delay in presentation was 4 ± 3.5 days.
Table 1.
Frequency and distribution of symptoms and signs of acute appendicitis
| Number (%) | |
|---|---|
| Symptoms | |
| Abdominal pain | 324 (100) |
| Vomiting | 186 (57.4) |
| Anorexia | 159 (49.0) |
| Nausea | 68 (21.0) |
| Diarrhoea | 59 (18.2) |
| Constipation | 21 (6.5) |
| Dysuria | 12 (3.7) |
| Haematuria | 7 (2.2) |
| Worms (vomiting or stools) | 3 (0.9) |
| Mass in abdomen | 2 (0.6) |
| Signs | |
| Generalised abdominal tenderness | 201 (62.0) |
| Fever (> 37°C) | 133 (41.0) |
| Peritonitis | 131 (40.4) |
| •localised | 87 (26.8) |
| •generalised | 44 (13.6 |
| Localised abdominal tenderness | 63 (19.4) |
| Right iliac fossa mass | 56 (17.2) |
SIGNS
Generalised and localised abdominal tenderness were present in 62.0% and 19.4% of patients, respectively. Peritonitis was present in 40.4% of patients and was localised in 26.4% and generalised in 14.0%. Right iliac fossa mass was present in 17.2% and digital rectal examination was recorded in 23.0% of patients. Fever and raised WCC (> 10 × 109 per litre) level was noted in 41.0% and 33.9% of patients, respectively.
Operative findings
At surgery, 40.7% of the patients were found to have complicated appendicitis (Table 2). Acute appendicitis and normal appendices were present in 53.0% and 4.9%, respectively. Of the grossly normal appendices, another underlying pathology was found in 3.1% cases, commonly pelvic inflammatory disease in females. Both male and female groups had one case each of perforated peptic ulcer mimicking acute appendicitis. Perforation was present in 30.5% of patients – males (19.5%) and females (11.0%). The most common incisions were lower midline laparotomy (47.2%) and gridiron incision (37.3%). Combined lower midline and gridiron incisions were done in 5.6% of patients and the rest had either long midline, Lanz incision or laparoscopy (5.5%). Laparostomy at the initial or subsequent surgery was done in 13 patients (4.0%).
Table 2.
Operative findings in 324 patients
| Findings | Number (%) |
|---|---|
| Inflamed | 171 (53.0) |
| Perforated | 99 (30.5) |
| Gangrenous | 33 (10.2) |
| Grossly normal | 16 (4.9) |
| •with other pathology | 10 (3.1) |
| •without other pathology | 6 (1.9) |
| Faecolith | 5 (1.5) |
Histology findings
Acute appendicitis was seen in 36.1% of patients and the negative appendicectomy rate was 17.0% – 10.2% in females and 6.8% in men (Table 3). Of the normal specimens, incidental findings such as schistosomiasis, Trichuris trichuria, amoebiasis, ascaris, Enterobius vermicularis and endometriosis was found in 8.6% of patients. Eleven patients (3.4%) had pelvic peritonitis, three (0.9%) mesenteric adenitis and in the rest no obvious pathology was found. There were no patients with carcinoid tumour or adenocarcinoma. The perforation rate was higher in males (25.3%) than females (8.7%). One female had endometriosis of the appendix with no other pathology.
Table 3.
Histological findings following 324 appendicecto
| Number (%) | |
|---|---|
| Findings | |
| Acute inflammation | 117 (36.1) |
| Perforated | 110 (34.0) |
| Gangrenous | 31 (9.6) |
| Normal | 55 (17.0) |
| Faecoliths | 11 (3.4) |
| Associated conditions | 28 (8.6%) |
| Schistosomiasis | 12 (3.7) |
| Trichuris trichuria | 5 (1.5) |
| Ascaris lumbricoides | 3 (0.9) |
| Enterobius vermicularis | 3 (0.9) |
| Amoebiasis | 2 (0.6) |
| Tuberculous appendicitis | 2 (0.6) |
| Endometriosis | 1 (0.3) |
Morbidity and mortality
The overall complication rate was 42.8% – 27.8% for complicated appendicitis and 15.0% for acute appendicitis (Table 4). Wound sepsis (25.3%) and prolonged ileus (6.2%) were the most common complications. Of the 15 patients (4.6%) who were complicated by peritonitis, nine (2.8%) had intraperitoneal abscesses and six (1.9%) developed abdominal compartment syndrome. The mean hospital stay was 6.5 ± 4.45 days and 6.1% of patients needed intensive care management. Four patients (1.2%), two children and two adults, died, all from the perforated group. Two developed septic shock and the other two had multi-organ failure following retroperitoneal necrotising fasciitis.
Table 4.
Morbidity and mortality within one month of sur
| Complication | Number (%) |
|---|---|
| Wound sepsis | 82 (25.3) |
| Postoperative ileus (prolonged) | 20 (6.2) |
| Peritonitis | 15 (4.6) |
| •intraperitoneal abscess | 9 (2.8) |
| •compartment syndrome | 6 (1.9) |
| Chest infection | 11 (3.4) |
| Iatrogenic small bowel injury | 4 (1.2) |
| Wound dehiscence | 3 (0.9) |
| Retroperitoneal necrotising fasciitis | 2 (0.6) |
| Faecal fistula | 2 (0.6) |
| Death | 4 (1.2) |
Discussion
Acute appendicitis remains one of the most common surgical conditions leading to emergency operation. According to a South African study conducted in 1982,2 10.5% of white South Africans had an appendicectomy and the figures among urban and rural blacks was 0.7% and 0.6%, respectively. The importance of early recognition and treatment of perforated appendicitis has been emphasised, so in equivocal cases surgeons felt obliged to operate without delay. We evaluated the clinical presentation, diagnostic clues, outcome and histopathological findings of acute appendicitis in our setting.
In this series, acute appendicitis occurred most commonly during the second decade of life, accounting for 43.1% of patients. There was a much higher male predominance (3.6:1) compared to previous African reports.3,4 Some Western studies5 have reported the opposite of our findings. Only 29.3% of our patients presented within 24 h of onset of symptoms and this trend is common in other African countries.6 The most common symptoms in our patients were abdominal pain (100%), vomiting (57.4%) and anorexia (49.0%). Diarrhoea was present in 18.2% of patients and 11.1% of these patients had a pelvic abscess. Right iliac fossa mass and generalised peritonitis was present in 17.2% and 13.6% of patients, respectively. In a previous study from Durban, South Africa, Madiba et al.7 found an incidence of right iliac fossa masses of 3.0%.
The most common surgical incision was lower midline laparotomy (47.2%), which probably reflects the high rate of delayed presentation with complicated appendicitis. The high rate of midline incisions contrast sharply with a study from the UK,8 in which 10.0% of their patients had a laparotomy. Possible explanations for a high wound sepsis rate (25.3%) in our setting include late presentation with complicated disease, liberal use of abdominal drains and the common practice of intra-operative peritoneal lavage (IOPL). The aim of IOPL is to reduce peritoneal contamination but the practice is controversial and there is risk of conversion of a localised area of contamination to a generalised one. A recent systemic review and meta-analysis9 concluded that neither simple nor the gangrenous or perforated appendicitis benefit from the routine use of prophylactic drains (recommendation A) and their use has been found to be associated with increased risk of wound sepsis and faecal fistula.
The negative appendicectomy rate of 17.0% falls within the 10–25% rate considered acceptable10 and was significantly higher in female patients (10.2%). We commonly use ultrasound scan in females with equivocal signs and symptoms of acute appendicitis and most of those in the reproductive age group are assessed by gynaecologists before surgical intervention. Borgstein et al.11 concluded that the negative appendicectomy rate was reduced from 38.0% to 5.0% in fertile female patients by the use of laparoscopy and from 8.0% to 4.0% in postmenopausal women and in men. In this study, only 18 patients (5.5%) had laparoscopic appendicectomy. This low rate is because it is not our current general policy to do laparoscopic appendicectomy due to lack of suitable facilities and expertise.
Our series revealed a high number of unusual histologies (8.6%) in the appendicectomy specimens. Parasitic infestation is a public health problem in South Africa and its presentation as appendiceal colic is difficult to differentiate from the pain of acute appendicitis. A high index of suspicion should be maintained for those patients presenting with signs of an acute abdomen, normal WCC and increased eosinophil count. The definitive diagnosis of amoebic colitis is made by demonstration of heamatophagous trophozoites of E. histolytica. T. trichiura occurs commonly in children and presentation include bloody stools, rectal prolapse and growth retardation. In a normal looking appendix, the surgeon must bear in mind the possibility of resident worms as the surgical technique in this group of patients requires some technical considerations.12 Furthermore, patients should receive antihelminthic treatment afterwards. Tubercular appendicitis is difficult to diagnose because the clinical picture is of acute appendicitis and diagnosis is usually made on histological examination of the specimen. Treatment includes a full course of anti-tubercular therapy.
The perforation rate on histology was 34.0% and this is higher than the 5–26% reported in the literature.13 Colson et al.13 proposed that a delay in presentation of more than 12 h after onset of symptoms increased the perforation rate and that an in-hospital delay did not affect the perforation rate. In our study, there was a direct correlation between perforation and delayed presentation. Of our patients, 32% were females and the majority (46.5%) were in the 11–20 year age group. The diagnostic accuracy rate in males and females was 96.4% and 74.6%, respectively, and pelvic sepsis was the most common diagnosis in normal female appendices. In the 33 female patients with normal appendices, 14 had associated conditions (Table 3) and 11 were found to have a gynaecological cause. One 31-year-old female had an ectopic pregnancy and another had a perforated peptic ulcer mimicking acute appendicitis. Twenty-two males had normal appendices, 14 with associated conditions and in 5, no pathology was identified.
We evaluated postoperative complications in the first month of operation and we had no data on long-term follow-up. The overall complication rate was 42.8% and was higher in perforated appendices. Wound sepsis (25.3%) was the most common complication noted which is higher than the 30.0% reported in the literature.14 Six patients (1.9%) developed abdominal compartment syndrome post-surgery. Four patients (1.2%) died in our series, all from the perforated group and this falls within the reported range of 0–2%.15
Conclusions
The majority of our patients present late with advanced disease requiring laparotomies and consequently a high rate of wound complications. To address the morbidity of this group of patients, we recommend the following: pre-operative high care optimisation, systemic peri-operative antibiotics, and control of source of infection, damage control laparotomy for unstable patients, planned re-look laparotomies, postoperative irrigation of the open wound and no routine use of abdominal drains. All surgeons, including those practising in developed nations should be aware of the possibility of parasitic infestations mimicking acute appendicitis which are now seen more frequently because of immigration and increased world travel.
References
- 1.Marudanayagam R, Williams GT, Rees BI. Review of the pathological results of 2660 appendicectomy specimens. J Gastroenterol. 2006;41:745–9. doi: 10.1007/s00535-006-1855-5. [DOI] [PubMed] [Google Scholar]
- 2.Walker ARP, Walker BF, Duvehage A, Jones J, Ncongwane J, Segal I. Appendicectomy prevalences in South African Blacks. Digestion. 1982;23:274–8. doi: 10.1159/000198762. [DOI] [PubMed] [Google Scholar]
- 3.Fulton J, Lazarus C. Acute appendicitis among black South Africans. S Afr J Surg. 1995;33:165–6. [PubMed] [Google Scholar]
- 4.Levy RD, Degiannis E, Kantarovsky A, Maberti PM, Wells M, Hatzitheofilou C. Audit of acute appendicitis in a black South African population. S Afr J Surg. 1997;35:198–202. [PubMed] [Google Scholar]
- 5.John H, Neff U, Kelemen M. Appendicitis diagnosis today: clinical and ultrasound deductions. World J Surg. 1993;17:243–9. doi: 10.1007/BF01658936. [DOI] [PubMed] [Google Scholar]
- 6.Willmore WS, Hill AG. Acute appendicitis in a Kenyan Rural Hospital. East Afr Med J. 2001;78:355–7. doi: 10.4314/eamj.v78i7.9007. [DOI] [PubMed] [Google Scholar]
- 7.Madiba TE, Haffeejee AA, Mbete DL, Chaithram H, John J. Appendicitis among African patients at King Edward VIII Hospital, Durban, South Africa. East Afr Med J. 1998;75:81–4. [PubMed] [Google Scholar]
- 8.Lansdown MRJ, Gray AJG, Treasure T, Layer GT. Appendicectomy: who performs it, when and how? Ann R Coll Surg Engl. 2006;88:530–4. doi: 10.1308/003588406X114875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Petrowsky H, Demartines N, Rousson V, Clavien PA. Evidence-based value of prophylactic drainage in gastrointestinal surgery. Ann Surg. 2004;240:1074–84. doi: 10.1097/01.sla.0000146149.17411.c5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mason JH, Byrne MP, Gaw FC. Surgery of the vermiform appendix. Surg Clin North Am. 1977;57:1303–15. doi: 10.1016/s0039-6109(16)41389-7. [DOI] [PubMed] [Google Scholar]
- 11.Borgstein PJ, Gordijn RV, Eijsbouts QA, Cuesta MA. Acute appendicitis – a clear-cut case in men, a guessing game in young women. A prospective study on the role of laparoscopy. Surg Endosc. 1997;11:923–7. doi: 10.1007/s004649900488. [DOI] [PubMed] [Google Scholar]
- 12.Saxena AK, Springer A, Tsokas J, Willital GH. Laparoscopic appendectomy in children with Enterobius vermicularis. Surg Laparosc Endosc Percutan Tech. 2001;11:284–6. doi: 10.1097/00129689-200108000-00012. [DOI] [PubMed] [Google Scholar]
- 13.Colson M, Skinner KA, Punnington G. High negative appendicectomy rates are no longer acceptable. Am J Surg. 1997;174:723–6. doi: 10.1016/s0002-9610(97)00183-9. [DOI] [PubMed] [Google Scholar]
- 14.Epstein MD. Complications of acute appendicitis. Ohio Med. 1990;8:602–7. [PubMed] [Google Scholar]
- 15.Ricci MA, Trevisani MF, Beck WC. Acute appendicitis – a 5-year review. Am Surg. 1991;57:301–5. [PubMed] [Google Scholar]