Abstract
Electronic personal health records (ePHRs) can potentially maximize access and coordination of health information and improve patient/clinician collaboration, patient self-management, and health outcomes. Most ePHRs are designed by vendors, physicians, and other proprietary partners and have neglected the patient perspective. This study sought to incorporate patient feedback into an existing ePHR system. Patients participated in a semistructured interview after one to two weeks of using an ePHR. Interviews addressed strengths and weaknesses of the PHR. Two iterations of interviews, referred to as Wave 1 and Wave 2, occurred sequentially. An iterative process of theme identification was used, and three theme categories (User, System Acceptance, and Technology) were identified in the two waves. Seven technology themes with 40 specific questions were identified and were rank ordered by importance and feasibility, and 20 suggestions were subsequently implemented into the ePHR. Thus, incorporating patient feedback on specific utilities and functionality into an existing ePHR is possible.
Introduction
The principles of patient-centered care emphasize patient access to information about their healthcare. Delivery of personal healthcare information to patients and families via technological systems such as electronic personal health records (ePHRs) provides an opportunity to motivate patients to improve their health and potentially increase the safety and quality of care. The American Health Information Management Association (AHIMA) defines a personal health record (PHR) as a “universally available, lifelong resource of health information needed by individuals to make health decisions. Individuals own and manage the information in the PHR, which comes from healthcare providers and the individual. The PHR is maintained in a secure and private environment, with the individual determining rights of access. The PHR is separate from and does not replace the legal record of any provider.”1 Electronic PHRs can be obtained from a wide range of providers including hospitals and physicians, insurers, private marketers, and large technology developers such as Google. Electronic PHRs either are free standing, with individual consumers loading their personal health data into the record, or are connected to the electronic medical record (EMR) of the patient's healthcare provider, whereby “official” health information can be sent to the ePHR. Some PHRs provided by insurance carriers can also be automatically populated with data, such as claims information.
Historically, research regarding health information technology has emphasized delivery of care in hospital or inpatient settings. Today, with shortened hospital stays, more controlled symptoms, and changes in reimbursement approaches, the majority of patient care occurs in ambulatory settings. Ambulatory care systems provide a unique perspective—one in which the patient's role is more important because most of the “care” occurs outside of the healthcare setting and is mainly under the patient's control. Contemporary emphasis on patient-centered care supports the notion that empowering patients to manage their health leads to improved outcomes. “Early experience confirms that when patients are given the chance to bridge the information gap between themselves, their health data, and their health care providers, many people enthusiastically take a more active role.”2 Recent technological advances provide an opportunity to use technology to empower patients by providing access to their healthcare information and providers.
Patient- and family-centered care (PFCC) has been defined as an “approach to the planning, delivery, and evaluation of health care that is grounded in mutually beneficial partnerships among health care providers, patients, and families.”3 Davis et al. have characterized patient-centered care as having seven dimensions, one of which is giving patients an “option to be informed and engaged partners in their care.”4 Patients experiencing PFCC have a better sense of control in managing their illness. Greater levels of “patient enablement” correlate with the doctor's interest in health promotion, the impact of health issues on a patient's life, and the patient's positive view of self-management.5 Preliminary studies have found that when patients have access to their health information, they feel more empowered.6 Empowered patients experience improved outcomes. Brink et al. describe the shift to an empowerment paradigm in the care of juvenile diabetes, where outcomes are improved when a combination of a team approach and patient-centered adjustments of food and insulin is put into play.7
There is growing recognition that the “brief visit model of care,” which evolved from the fee-for-service reimbursement system, fails to meet patient needs.8 Results of a national survey show 97 percent of primary care physicians support patient-centered practices, but only 14 to 33 percent adopt these practices.9 Many have acknowledged that ambulatory care systems must be redesigned to accomplish patient-centered care.10, 11 A critical component of this redesigned system is free-flowing information between the patient and provider in a “two-way interaction.”12 Electronic PHRs have the potential to incorporate many aspects of patient-centered care.
A prime component of PFCC, the involvement of patients, has been limited in the development and improvement of ePHRs. Most ePHRs have been developed from the perspective of physicians and/or information technology (IT) developers.13 As technology evolves, it is imperative to consider the utility of ePHRs from the patient's perspective. “Developers should solicit patient input regarding the education and support that patients require to make decisions and participate in their own care.”14
The purpose of this study is to examine patient perspectives on ePHR use and functionality as part of the development process of an existing ePHR, to assess whether or not these ideas are technologically feasible, and to compare the patient views to the expectations of a collaborative team of providers, IT professionals, PFCC experts, and investigators. This work is part of a larger study designed to test the effectiveness of an ePHR to increase blood pressure (BP) control by patients with hypertension. These initial waves of patient-centered input into the product design were intended to improve an existing ePHR by incorporating the patient perspective and to identify expectations of potential ePHR users.
This qualitative work asked the following questions:
What do patients with little or no previous experience with ePHRs notice after brief periods of ePHR use?
Are patient suggestions realistic technologically?
What do patients with little or no previous ePHR experience expect from ePHR use?
Can we, as experts, grasp the patient perspective or do our perceptions differ?
Is this mixed collaboration possible?
Methods
Two iterations of patient feedback, referred to as Wave 1 and Wave 2, were obtained sequentially.
Procedures
In each wave, a convenience sample of ambulatory patients with hypertension attending a family medicine clinic based in an academic medical center was recruited based on physician recommendations. Hypertension criteria were based on Joint National Committee (JNC) 7 guidelines and included patients with prehypertension (systolic BP 120–139 mm Hg or diastolic BP 80–89 mm Hg), stage 1 hypertension (systolic BP 140–159 mm Hg or diastolic BP 90–99 mm Hg), or stage 2 hypertension (systolic BP 160 mm Hg or above or diastolic BP 100 mm Hg or above).
Patients were consented, granted access, and trained on the ePHR by an investigator. The ePHR training consisted of a brief demonstration of key features of the ePHR, and patients were given a unique user name and password. Participants were then asked to use the ePHR for one to two weeks and later return to the clinic to complete a semistructured interview. The semistructured interview process allows for flexibility in the patient/interviewer interaction, yet maintains an overall consistency by utilizing a predetermined set of questions.15 This allowed the interviewer more freedom and fewer limitations in the approach but maintained uniformity across the interviews. All interviews were recorded and later transcribed. All methods were reviewed and approved by the Institutional Review Board at the academic center.
Participants
In the first wave, 9 of 15 recruited patients returned for the interviews (5 females, 4 males). In the second wave, 7 of 16 recruited patients returned for the interviews (4 females, 3 males). Interviews lasted from 10 to 30 minutes. Patients were given a $20 gift card for their participation.
Interview Questions
The interview questions were based on recommendations from the American College of Medical Informatics 2005 symposium, as described by Tang et al., which expressed the need for PHR research to address PHR functionality, data issues, health tracking, decision support, issues concerning the patient/provider relationship, and the patient's role in their own healthcare.16 Interview questions for both Wave 1 and Wave 2 (see Appendix A) addressed ease of use, technological understanding, blood pressure tracking capability, and personal goal setting.
Description of the ePHR
The ePHR evaluated in this study is the Cerner Corporation's proprietary PHR system known as IQHealth that was deployed at MCGHealth under the brand name My HealthLink. My HealthLink provides a secure, comprehensive electronic record that enables consumers to store personal health information.
The core functions of the ePHR include:
Secure messaging;
Access to educational materials;
Medication interaction checking;
Recording and monitoring health measures, for example, blood pressure; and
Goal setting and health diaries.
Analyses
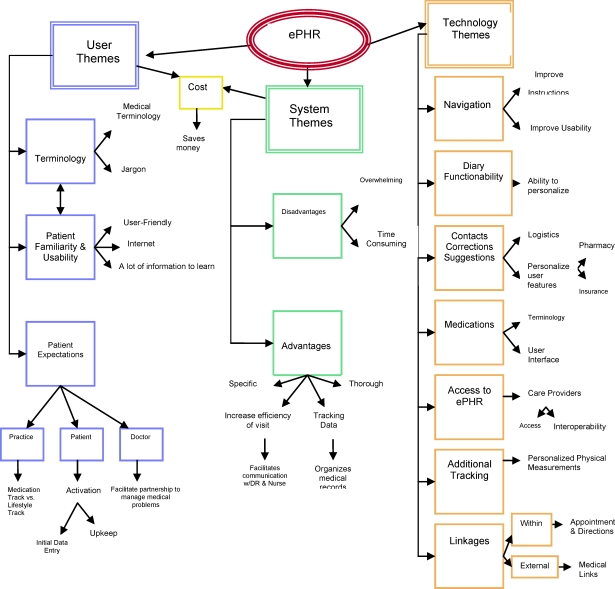
Interview transcripts were reviewed by three researchers (two research associates and one investigator, P.W.) using an iterative process of theme development utilizing the five steps of qualitative data interpretation (describing, connecting, corroborating, organizing, and representing the account) as described by Crabtree and Miller.17 Initial themes were identified in the first coded interviews, subsequent interviews were coded according to existing themes, and new themes were added as they arose. A conceptual model of all Wave 1 themes can be seen in Figure 1.
Figure 1.
Wave 1 Conceptual Map
Technology theme suggestions were reviewed by the research advisory group, which consisted of patients (two), health IT representatives (up to five), PFCC consultants (two), and project faculty and staff (five). In order to decide which patient suggestions to implement in a timely fashion, each patient suggestion was rated by the group via consensus on a scale of importance (essential, important, relevant, or not relevant) and on a scale of technical feasibility (essential, reasonable, possible, or impossible). Implementation tasks and priorities were assigned based on these rankings. When possible, changes were made prior to Wave 2. Analysis of the Wave 2 interviews was conducted using the same iterative process of theme development.
Results
Wave 1
Fifty-eight unique suggestions were identified from participants in Wave 1. These suggestions were classified into 13 themes, which were then divided into three categories: User Themes, System Acceptance Themes, and Technology Themes.
User Themes
Patients identified three distinct User Themes in the area of personal user issues. The first User Theme was the ePHR Terminology. Patients thought the terminology was sometimes difficult to understand and would require help from the healthcare team.
“[You] have to really read it closely and if you don't know much about terminology … it could be real confusing.”
The second User Theme, Usability and Patient Familiarity, suggests patients are aware of potential generational issues that impact the degree of patient comfort with technology.
“… the only problem that I could see would be a problem is that the generation is getting older”
The third User Theme showed the Patient Expectations concerning outcomes if the ePHR was implemented, such as how the practice and doctor would interact with the patient and what would be expected of the patient.
“… they don't necessarily give it to us in your visit, e.g. vitals, blood pressure reading which it is necessary to upkeep the ePHR.”
“ … if you haven't seen your physician in six months, it should be that he will be able to determine there are things there—such as a trend down or a trend up.”
“It wasn't something on my radar every day or a few times a day … I found you had to go directly there for that purpose.”
System Acceptance Themes
Two System Acceptance Themes were observed, reflecting the Advantages and Disadvantages of an ePHR. A minor theme related to the Cost impact of an ePHR was also identified by one patient.
Twenty-one Advantages of an ePHR were noted, including the ability to capture information, identify inconsistencies, track data, increase understanding, decrease time with physician, and facilitate communication.
“I have diabetes mellitus, and I also have hypertension … trying to track what shows up here and what you have at home to make sure that there are no inconsistencies.”
Some Disadvantages noted included that the ePHR was sometimes overwhelming and time consuming.
Technology Themes
Seven Technology Themes were observed, with the most common being the Navigation theme. This theme reflected health and technology literacy, patient usability, ease of access, need for additional instructions, and the potential of customizable menus.
“But I found myself finding it hard to find where to put readings and that is what I mean—just walk you through it, even.”
Themes of Diary Functionality, Medications, Linkages, Additional Tracking, and miscellaneous specific Suggestions also emerged. One of the most valued applications, the diary for tracking health issues, was of great interest for eight of the nine patient participants.
The Medication theme concerned the ability to track and record one's medications in the current system, which was found to be difficult by some patients but relatively easy by others.
Both the Internal and External Linkages themes identified the need for more linkages, such as directions to the office and external links to additional medical information. The final theme, Access, identified that a more direct path to the ePHR was needed from the health system home page and that patients desired to choose which providers have access to their ePHR.
Only the Technology Theme recommendations were ranked by the group on importance and feasibility to determine strategies for implementation. Twenty (50 percent) of the technology recommendations were implemented into the ePHR, 80 percent via technology changes and 20 percent via education materials or planned training elements. Items were given a rank of importance and a rank of feasibility. Importance-by-feasibility ratings were calculated by giving three points to items rated as essential on either importance or feasibility, two points to items rated as important or reasonable, one point to items rated as relevant or possible, and zero points to items rated as not relevant or impossible. The points were then multiplied, giving a maximum of nine points for each item. Table 1 reflects the number of items implemented for each importance-by-feasibility rating. Items that received higher ratings were more likely to be implemented.
Table 1.
Items Implemented into the PHR According to Importance-by-Feasibility Rating
| Importance-by-Feasibility Rating Score | Implemented | Not Implemented | Total |
|---|---|---|---|
| 0 | 3 | 19 | 22 |
| 2 | 2 | 0 | 2 |
| 3 | 2 | 0 | 2 |
| 4 | 1 | 0 | 1 |
| 6 | 5 | 1 | 6 |
| 9 | 7 | 0 | 7 |
| Total | 20 | 20 | 40 |
Wave 2
No new themes or theme categories were identified in Wave 2. Themes were again organized into three theme categories: User Themes, System Acceptance Themes, and Technology Themes. The Diary Functionality theme, the specific Suggestions theme, and the Cost theme did not emerge in Wave 2. Thirty-three specific suggestions were identified, but only three were unique to Wave 2. Two of these unique suggestions emerged in the Advantages theme. The appointment scheduling feature, implemented after Wave 1, was seen as an advantage. The possibility of future integration of the ePHR with the electronic medical records of the patients’ physicians also emerged in Wave 2. The third unique suggestion concerned the newly implemented message center, which was described as confusing by some patients.
Discussion
PHRs have the power to increase patients’ self-management of their health by providing access to their health information. To accomplish this effectively, ePHRs need to be perceived as functional and valuable to patients. Typically, ePHRs have been designed by vendors, physicians, or other proprietary partners and have neglected the patient perspective.18 The present study examined whether patient feedback about the functionality of an ePHR could be incorporated into future versions and whether patient perspectives differ from those of the collaborative team of developers. Results indicate that a mixed collaboration is possible and may emphasize different system elements. Seventy-six percent of suggestions regarding specific utilities and functionality were regarded as relevant by the collaborative team, and 50 percent of the suggestions in the Technology Theme were viewed as technologically feasible and subsequently implemented into the ePHR.
The Technology Theme suggestions were most important to us as we hoped to improve the ePHR itself. Responses from our patients suggested that they can recognize the importance of navigation, and their responses add another perspective when examining usability. Suggestions from the Navigation theme, such as improving instructions and the user interface, were implemented after Wave 1 into the ePHR to improve understanding and ease of use. Patient feedback from Wave 2 identified fewer issues in this area, which may suggest an improvement in the ePHR format. Additionally, a medical terminology glossary was implemented, and Wave 2 respondents made no comments regarding medical terminology, also suggesting improvement in the ePHR format. Patients from both waves described the ePHR as fairly user-friendly and adjusting to using the ePHR as a relatively quick process. Although the small sample size, the use of a single clinic, and the selection of patients at the recommendation of physicians may limit the generalizability of the results, the suggestions were considered viable, appropriate, and feasible for the development of this ePHR.
Many themes reflected elements of a patient-centered approach. Borrowing from the work of Little et al. on patient perspectives about patient-centered care, which found three domains: partnership, communication, and health promotion,19 we summarize our results as indicating that the ePHR has the potential to support the patient-centered approach to care by improving these three domains.
Patients anticipate that the ePHR will facilitate partnership with their doctor to manage their medical problems. The questions patients had about how the ePHR would be utilized by their physician and how using the ePHR would change the patients’ responsibility for their health highlighted the importance of the partnership and the need for clarification about what this new partnership will mean. According to a 2004 Markle Foundation report, “physicians currently using some form of PHR report many benefits to both their practice and their interactions with their patients.”20
Patients not only expressed that the ePHR could help them self-manage their medical problems but conveyed expectations that their doctor will use information from their ePHR as a source for assessment and communication about their health. Points raised by patients also implied that they do not understand that the ePHR is not part of their official medical record. This suggests that significant education and clarification will be necessary to insure that the communication desired by the patient and physician is possible.
The third element of patient-centered care is health promotion. The ability to personalize and track one's health information emerged as an important function of the ePHR. The electronic diary, medication tracking, and blood pressure tracking were all viewed as positive features of the ePHR. Such tracking can increase the patient's role in managing illness and improve health outcomes. The focus of self-management support, arising from the Chronic Care Model, has stimulated significant developments in chronic illness management.21 A meta-analysis by Cappuccio et al. found that patients with hypertension who monitor their blood pressure at home have “better blood pressure control and greater achievement of blood pressure targets.”22 In a separate meta-analysis focusing on the effects of self-management for older adults, similar results were reported: “we found … clinically important benefits for measures of blood glucose and blood pressure reduction for chronic disease self-management programs aimed at patients with diabetes and hypertension.”23 Another health promotion element from our patient interviews was the importance of internal and external links to medical information. Research utilizing focus groups has found that patients desire more information regarding their illness and treatment options than what their doctors currently provide.24
A critical variant of ePHRs is whether or not the ePHR is linked to information in any official EMR, such as one maintained by a hospital system. A limitation of this study was that at the time the interviews were conducted, the ePHR was not tethered to the hospital EMR; therefore, information did not feed from the official hospital record to the ePHR. Participants in the American College of Medical Informatics symposium on PHRs have concluded that “PHRs integrated with EHRs, either through tethering or interconnectivity, provide much greater benefits than stand-alone PHRs.”25 Recent evidence suggests that when patients are allowed to have direct input into the health maintenance portion of their record, accuracy increases in terms of identifying who is due for screenings.26 Cancer patients report that an electronic self-monitoring system that sends notices to healthcare clinicians based on patient self-reporting was extremely useful and highly used by patients.27 Cimino et al. found that patients who have access to their EHR reported improved understanding of their health issues and increased communication with their physicians.28 When patients have been allowed to view their medical records, they have found it extremely useful,29 and an online survey found that 91 percent of patients see reviewing their medical records as important, 82 percent would like to review test results online, and 84 percent want to look for possible mistakes in their medical record.30 The importance of interoperability was also seen in this study, as reflected by patient responses.
“If you have access between the two … as far as being able to eliminate any misconceptions or any misunderstandings”
In conclusion, we found that the incorporation of patient feedback for specific utilities and functionality is possible and technologically feasible, highlighting the strengths of a design collaboration between experts and patients. Additionally, patients with little or no experience with ePHRs highlighted potential benefits of an ePHR such as motivation, partnership with physicians, improved communication, and ease of access, which are all key elements emphasized by the PFCC approach.31 To express these benefits differently and with patient-oriented nuances, incorporation of patient suggestions may increase patient utilization and acceptance of this technological tool that holds great promise to encourage patient motivation and improve consequent health outcomes.
Appendix A
Interview Questions
Are you familiar with the ePHR?
What did you find most useful about the ePHR?
What did you find least useful about the ePHR?
Do you think the ePHR helps you control your blood pressure?
Do you think the ePHR helps you prepare for office visits?
Do you think the ePHR helps you better follow your doctor's treatment recommendations?
Do you think the ePHR helps you feel more responsible for your health?
Did the ePHR slow down your healthcare, or increase the time your doctor spent with you?
Do you think the ePHR intruded on your relationship with your doctor?
Do you think the ePHR confused you?
Footnotes
This project was supported by a grant from the Agency for Healthcare Research and Quality (grant number R18HS017234). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Contributor Information
Peggy J Wagner, the Medical College of Georgia in Augusta, GA and a Clinical Professor in the Department of Family Medicine at the University of South Carolina in Columbia, SC.
Shalon M Howard, the Medical College of Georgia in Augusta, GA.
Douglas R Bentley, the Veterans Administration-Ann Arbor Healthcare System in Ann Arbor, MI.
Yoon-Ho Seol, the Medical College of Georgia in Augusta, GA.
Patricia Sodomka, the Medical College of Georgia in Augusta, GA during the time of this study. Ms. Sodomka sadly lost her fight with cancer prior to this publication.
Notes
- 1.AHIMA e-HIM Personal Health Record Work Group “The Role of the Personal Health Record in the EHR.”. Journal of AHIMA. 2005;76(no. 7) [PubMed] [Google Scholar]
- 2.Tang P. C, Lansky D. “The Missing Link: Bridging the Patient-Provider Health Information Gap.”. Health Affairs (Millwood) 2005;24(no. 5):1290–95. doi: 10.1377/hlthaff.24.5.1290. [DOI] [PubMed] [Google Scholar]
- 3.Institute for Patient- and Family-Centered Care. Institute for Patient- and Family-Centered Care.http://www.ipfcc.org/faq.html
- 4.Davis K, Schoenbaum S. C, Audet A.-M. “Adoption of Patient-Centered Care Practices by Physicians: Results from a National Survey.”. Archives of Internal Medicine. 2006;166(no. 7):754–59. doi: 10.1001/archinte.166.7.754. [DOI] [PubMed] [Google Scholar]
- 5.Little P, et al. “Preferences of Patients for Patient Centred Approach to Consultation in Primary Care: Observational Study.”. BMJ. 2001;322(no. 7284):468–72. doi: 10.1136/bmj.322.7284.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Markle Foundation—Connecting for Health. Working Group on Policies for Electronic Information Sharing Between Doctors and Patients. Connecting Americans to their Healthcare: Final Report. 2004.
- 7.Brink S. J, Miller M, Moltz K. C. “Education and Multidisciplinary Team Care Concepts for Pediatric and Adolescent Diabetes Mellitus.”. Journal of Pediatric Endocrinology. 2002;15(no. 8):1113–30. doi: 10.1515/jpem.2002.15.8.1113. [DOI] [PubMed] [Google Scholar]
- 8.Scherger J. E. “The Biopsychosocial Model Is Shrink Wrapped, on the Shelf, Ready to Be Used, But Waiting for a New Process of Care.”. Families, Systems & Health. 2005;23(no. 4):444–47. [Google Scholar]
- 9.Davis, K., S. C. Schoenbaum, and A.-M. Audet. “Adoption of Patient-Centered Care Practices by Physicians: Results from a National Survey.” [DOI] [PubMed]
- 10.Scherger, J. E. “The Biopsychosocial Model Is Shrink Wrapped, on the Shelf, Ready to Be Used, But Waiting for a New Process of Care.”
- 11.Bergeson S. C, Dean J. D. “A Systems Approach to Patient-Centered Care.”. JAMA. 2006;296(no. 23):2848–51. doi: 10.1001/jama.296.23.2848. [DOI] [PubMed] [Google Scholar]
- 12.Markle Foundation—Connecting for Health. Working Group on Policies for Electronic Information Sharing Between Doctors and Patients. Connecting Americans to their Healthcare: Final Report.
- 13.Rodriguez M. M, Casper G, Brennan P. F. “Patient-Centered Design: The Potential of User-Centered Design in Personal Health Records.”. Journal of AHIMA. 2007;78(no. 4):44–46. [PubMed] [Google Scholar]
- 14.Demiris G, et al. “Patient-Centered Applications: Use of Information Technology to Promote Disease Management and Wellness: A White Paper by the AMIA Knowledge in Motion Working Group.”. Journal of the American Medical Informatics Association. 2008;15:8–13. doi: 10.1197/jamia.M2492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kvale Steiner. Interviews: An Introduction to Qualitative Research Interviewing. Thousand Oaks, CA: Sage Publications; 1996. [Google Scholar]
- 16.Tang P, et al. “Personal Health Records: Definitions, Benefits, and Strategies for Overcoming Barriers to Adoption.”. Journal of the American Medical Informatics Association. 2006;13(no. 2):121–26. doi: 10.1197/jamia.M2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Crabtree Benjamin F, Miller William L. Doing Qualitative Research. 2nd ed. Thousand Oaks, CA: Sage Publications; 1999. [Google Scholar]
- 18.Bergeson, S. C., and J. D. Dean. “A Systems Approach to Patient-Centered Care.” [DOI] [PubMed]
- 19.Little, P., et al. “Preferences of Patients for Patient Centred Approach to Consultation in Primary Care: Observational Study.” [DOI] [PMC free article] [PubMed]
- 20.Markle Foundation—Connecting for Health. Working Group on Policies for Electronic Information Sharing Between Doctors and Patients. Connecting Americans to their Healthcare: Final Report.
- 21.Glasgow R. E, et al. “Self-Management Aspects of the Improving Chronic Illness Care Breakthrough Series: Implementation with Diabetes and Heart Failure Teams.”. Annals of Behavioral Medicine. 2002;24(no. 2):80–87. doi: 10.1207/S15324796ABM2402_04. [DOI] [PubMed] [Google Scholar]
- 22.Cappuccio F, Kerry S, Forbes L, Donald A. “Blood Pressure Control by Home Monitoring: Meta-analysis of Randomised Trials.”. BMJ. 2004;329(no. 7458):145. doi: 10.1136/bmj.38121.684410.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chodosh J, et al. “Meta-analysis: Chronic Disease Self-Management Programs for Older Adults.”. Annals of Internal Medicine. 2005;143(no. 6):427–46. doi: 10.7326/0003-4819-143-6-200509200-00007. [DOI] [PubMed] [Google Scholar]
- 24.Tang P, Newcomb C. “Informing Patients: A Guide for Providing Patient Health Information.”. Journal of the American Medical Informatics Association. 1998;5(no. 6):563–70. doi: 10.1136/jamia.1998.0050563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tang, P., et al. “Personal Health Records: Definitions, Benefits, and Strategies for Overcoming Barriers to Adoption.” [DOI] [PMC free article] [PubMed]
- 26.Staroselsky M, et al. “Improving Electronic Health Record (EHR) Accuracy and Increasing Compliance with Health Maintenance Clinical Guidelines Through Patient Access and Input.”. International Journal of Medical Information. 2006;75:693–700. doi: 10.1016/j.ijmedinf.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 27.Van den Brink J. L, et al. “Involving the Patient: A Prospective Study on Use, Appreciation and Effectiveness of an Information System in Head and Neck Cancer Care.”. International Journal of Medical Informatics. 2005;74(no. 10):839–49. doi: 10.1016/j.ijmedinf.2005.03.021. [DOI] [PubMed] [Google Scholar]
- 28.Cimino J, Patel V, Kushniruk A. “The Patient Clinical Information System (PatCIS): Technical Solutions for and Experience with Giving Patients Access to Their Electronic Medical Records.”. International Journal of Medical Informatics. 2002;68:113–27. doi: 10.1016/s1386-5056(02)00070-9. [DOI] [PubMed] [Google Scholar]
- 29.Pyper C, et al. “Patients' Experiences When Accessing Their On-line Electronic Patient Records in Primary Care.”. British Journal of General Practice. 2004;54(no. 498):38–43. [PMC free article] [PubMed] [Google Scholar]
- 30.Markle Foundation—Connecting for Health. Americans See Access to Their Medical Information as a Way to Improve Quality, Reduce Health Care Cost. Press release, July 13, 2006.
- 31.Tang, P. C., and D. Lansky. “The Missing Link: Bridging the Patient-Provider Health Information Gap.” [DOI] [PubMed]