Abstract
In this study we measure the concurrent validity of administering FIM™ instrument (“FIM”) by interview. Data from twenty-eight community-dwelling, cognitively intact, elderly patients with hip fracture were collected in five post-acute rehabilitation facilities. Within 72 hours of admission to (and at discharge from) the post-acute facilities, both a FIM-certified interviewer and a multidisciplinary team administered the FIM instrument to each participant concurrently. At admission, the mean FIM ratings assigned by the interviewer and by the team were 84.3 and 80.5, respectively (p<0.001). At discharge, the mean FIM ratings were 104.4 and 103.4 (p>0.50), reflecting the participants' functional recovery during post-acute rehabilitation. The intra-class correlation between the FIM ratings assigned by the interviewer and by the team was 0.74 (95% CI = 0.58–0.91) at admission and 0.76 (95% CI = 0.60–0.92) at discharge. FIM ratings assigned by FIM-certified interviewers are valid indicators of the functional status of groups of older people recovering from hip fracture, and feasible for longitudinal study.
Keywords: FIM, Validity, Interview, Hip Fracture
BACKGROUND AND PURPOSE
Clinicians and researchers use the FIM instrument to monitor the recovery of functional ability by people undergoing rehabilitation.1–6 The FIM assessment includes 18 activities of self care, sphincter control, transferring, locomotion, communication, social interaction, and cognition. To rate the FIM assessment, members of an interdisciplinary team observe a patient performing the 18 activities and rate his or her ability to perform each activity on a seven-point ordinal scale (1 = totally unable, 7 = totally independent). The difference between the sum of the 18 ratings (range = 18–126) and the maximum possible FIM rating (126) provides a gauge of the amount of assistance required by the patient.1,2,5,6 FIM ratings are valid3, 5, 7–17 and reliable2,5, 7, 15–19 indicators of functional independence, and they reflect aggregate changes in functional status that occur over time.7, 11, 13 To assure reliable collection of FIM data, the Uniform Data System of Medical Rehabilitation (UDSMR) provides a standardized training and certification process for professionals who wish to administer the FIM instrument.
The FIM instrument can be used in rehabilitation facilities, hospitals, clinics, nursing homes, and private homes.1,2, 5, 6, 20 Because its administration requires a multidisciplinary team, however, using it outside of clinical facilities presents logistical and financial challenges. Either the members of the team must travel to private homes, or people with functional deficits must travel to clinical sites. As a result, few investigators use the FIM instrument to monitor changes in functional status over an extended period of time. Most studies of recovery from hip fracture, for example, have followed patients only until their discharge from rehabilitation facilities,6, 21–25 or they have monitored functional change with instruments that are less well-studied than the FIM instrument.
In our one-year longitudinal study on rehabilitation and functional recovery among hip fracture patients, the study design requires three post-acute rehabilitation follow-ups at patients' current residence. It would be costly and logistically not feasible to collect FIM data and employ a multidisciplinary team to evaluate the participants' at their current residence for the three follow-up evaluations. An attractive alternative would be to track patients' functional status throughout the entire course of rehabilitation using FIM data collected by a single interviewer. This pilot study is to evaluate the validity of this approach. We studied patients who were recovering from hip fracture and compared the FIM ratings assigned by their multidisciplinary teams -- at admission to and at discharge from rehabilitation facilities -- with FIM ratings assigned concurrently by an interviewer who had successfully passed the standardized FIM training and mastery test.
METHODS
Participants
For the present investigation, we studied the initial 28 enrollees in a 5-year longitudinal study of functional recovery from hip fracture, beginning on December 2001. The parent study recruited older (age 65+ years) community-dwelling participants who were admitted for rehabilitation for hip fracture (ICD-9-CM 820-820-9) at five post-acute facilities in the Baltimore metropolitan area and who met the following eligibility criteria: having had a surgical procedure (ICD9-CM 81.21, 81.40, 81.51, 81.52) for a first-time, non-pathologic fracture; having a MMSE score greater than 23; and not having metastatic cancer, Alzheimer's disease or other dementia.
Measurements
Within 72 hours of admission to a post-acute rehabilitation facility, a FIM-certified multidisciplinary team (generally consisting of a nurse, a physical therapist, an occupational therapist and a social worker) observed each patient performing the 18 activities and then assigned a “team admission FIM rating.” During this same interval, a FIM-certified researcher, blinded to the ratings of the team, interviewed the patient about his or her ability to perform the 18 tasks and assigned an “interviewer admission FIM rating.” The team and the interviewer used the same standard FIM scoring algorithms to assign their FIM ratings. Within 72 hours before discharge, the team and the interviewer repeated these procedures and assigned discharge team and interviewer FIM ratings.
Analysis
We used the paired-t test to compare mean FIM ratings and the intra-class correlation coefficient (ICC) to assess the agreement between individual FIM ratings obtained by the team and the interviewer, both at admission and at discharge.
RESULTS
The participants were mostly were white (89.3%) unmarried (64%) women (71%) who lived with others (61%). The average age (79 years), mini-mental status examination (MMSE) score (27) and number of chronic conditions (2.3) reflected the study's eligibility criteria.
At admission, the mean FIM ratings assigned by the team and by the interviewer were 80.5 and 84.5, respectively (p <0.001). The ICC between team and interviewer admission FIM ratings for individuals was 0.74 (p<0.001). At discharge, the mean FIM ratings assigned by the team and the interviewer were 103.4 and 104.4, respectively (p>0.50). The ICC between team and interviewer discharge FIM ratings for individuals was 0.76 (p<0.001). The changes in the mean FIM ratings between admission and discharge were 22.9 and 19.9 for the team and the interviewer, respectively (p=0.15). The ICC for the individual change ratings measured by the team and interviewer was 0.44 (p<0.001).
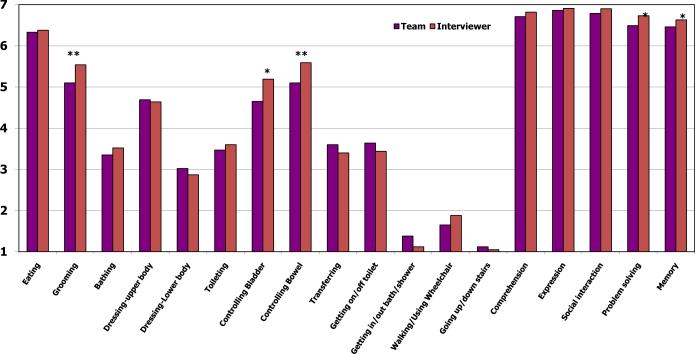
Figure 1 compares the mean ratings assigned at admission by the multidisciplinary team and the interviewer for each of the 18 FIM activities. As expected with hip fracture patients, functional independence was most impaired for activities that depend on the lower extremities (e.g., walking, climbing stairs, and using a tub or shower) and least impaired for cognitive activities (e.g., memory, comprehension and social interaction).
Figure 1.
Mean FIM ratings assigned at admission by interviewer and by multidisciplinary team.
*P<.05, **P<.01
There were no significant differences between the mean ratings assigned at admission by the team and the interviewer for 15 of the 18 FIM activities. For three activities (grooming and controlling bowel and bladder), however, the mean ratings assigned by the interviewer were significantly higher than the mean ratings assigned by the team.
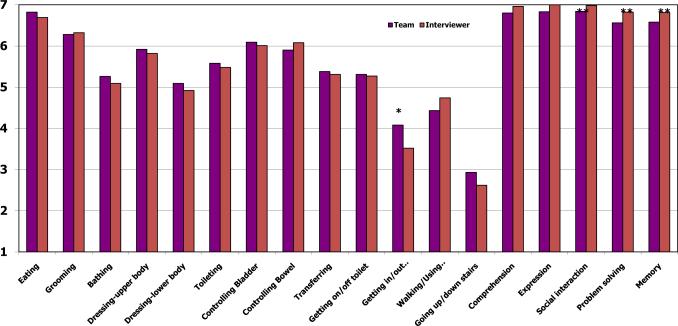
Figure 2 compares the activity-specific FIM ratings assigned at discharge by the interviewer and multidisciplinary team. As expected, considerably lower ratings in the lower extremities dependent activities is seen among recovering hip fracture patients at admission. There were no significant differences between the mean ratings assigned at discharge by the team and the interviewer for 16 of the 18 FIM activities. For two activities (dressing lower body and controlling bowel), however, the mean ratings assigned by the interviewer were significantly different from the mean ratings assigned by the team.
Figure 2.
Mean FIM ratings assigned at discharge by interviewer and by multidisciplinary team.
*P<.05, **P<.01
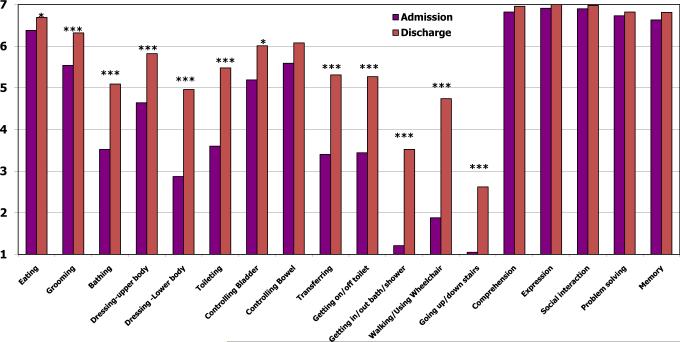
Figure 3 illustrates the changes between admission and discharge in the FIM ratings assigned by the interviewer. The largest increases in FIM ratings were for activities at which rehabilitation was directed, e.g., walking, climbing stairs, using a tub or shower, transferring, dressing the lower extremities, and bathing.
Figure 3.
Mean FIM ratings assigned by interviewer at admission and discharge.
*P<.05;***P<.001
The admission-to-discharge changes in FIM ratings detected by the team and the interviewer were similar for 15 of the 18 activities. Larger improvements were detected by the team, however, for toileting (team=2.25 vs. interviewer=1.57, p < 0.001), bladder management (team=1.8 vs. interviewer=0.4, p = 0.002) and bowel management (team=1.06 vs. interviewer=0.42, p = 0.03).
DISCUSSION AND CONCLUSION
This pilot study suggests that using aggregate FIM data collected by interview may be a valid approach to tracking the functional recovery of groups during post-acute rehabilitation. We found that the average total FIM rating of a group of patients that had completed rehabilitation was similar regardless of whether a team of health care professionals (the “gold standard”) or a single non-clinician interviewer collected the raw data. Moreover, there was no significant difference between the team's and the interviewer's average ratings for the group's improvement on the FIM assessment during inpatient rehabilitation.
Where differences did occur, the interviewer's mean total FIM ratings tended to be slightly higher than those of the team, while the interviewer-administered mean rating for global improvement during rehabilitation tended to be slightly lower. These differences in ratings appear to be attributable primarily to differences in the sub-ratings for four of the 18 activities included in the FIM instrument: bladder sphincter control, bowel sphincter control, and grooming and dressing lower body. For three of these activities, the team rated the study group as more impaired than did the interviewer. We speculate that the team's ratings, derived from performance data, were more accurate than the interviewer's ratings, which the participants' may have exaggerated because of embarrassment and the team may have noted bowel and/or bladder accidents over the previous 7 days that may have escaped the attention of the interviewer.
The appropriate interpretation of this study must include its limitations. The sample of 28 individuals is small due to budgetary and time constraints. The results do not provide strong evidence that the interviewer-administered FIM assessment is a valid measure of individuals' functional ability or recovery. While the agreement between the team's and the interviewer's ratings for individual participants' functional status (ICC = 0.74 – 0.76) was adequate, that for improvement in functional ability (ICC = 0.44) was modest. As mentioned earlier, the correlation between team and interviewer FIM ratings for incontinence and grooming and dressing the lower body was poor. In the future, investigators may wish to address this problem by training interviewers how to inquire effectively about incontinence and grooming and dressing the lower body by allowing them to seek additional information from informants or records. Finally, because we studied a fairly homogeneous sample, our results may not apply completely to other populations, such as younger people or patients with cognitive impairment or other difficulties with communication.
Our study validated interview technique for administering the FIM instrument is feasible to monitor long-term functional recovery. If confirmed by other studies, the findings reported here would facilitate the measurement of functional recovery throughout the course of rehabilitation. With the caveats mentioned above, they would allow FIM-certified clinicians and researchers to use the FIM instrument in populations with disability, which is the industry standard in rehabilitation facilities, at all sites of care, regardless of the availability of equipment and interdisciplinary assessment teams. The resulting information about the long-term outcomes of treatment and rehabilitation would enhance the value of research and programs designed to improve the quality of care.
Acknowledgements
This research was funded by the National Institute on Aging, Grant R01 AG15918-02. We are grateful to the hip fracture patients who completed the interviews. Without their cooperation and support, this study would not have been possible. We also thank for Holly Hatch-Stock for project and data management, Nancy W. Germain and Vyacheslav Paliy for assistance with data collection.
Funding Source: The National Institute on Aging, Grant R01 AG15918-02
Footnotes
Disclosures: FIM is a trademark of Uniform Data System for Medical Rehabilitation, a division of UB Foundation Activities, Inc.
REFERENCES
- 1.Guide for the Uniform Data Set for Medical Rehabilitation (including the FIM™ Instrument) Version 5.1 State University of New York at Buffalo; Buffalo, NY 14214: 1997. [Google Scholar]
- 2.Hamilton BB, Granger CV, Sherwin FS, et al. A uniform national data system for medical rehabilitation. In: Fuhrer MJ, editor. Rehabilitation outcomes: analysis and measurement. Paul H. Brookes; Baltimore, Md: 1987. pp. 137–147. [Google Scholar]
- 3.Granger CV, Hamilton BB. The Functional Independence Measure. In: MacDowell Ian, Newell Claire., editors. Measuring Health: A guide to rating scales and questionnaires. 2nd edition Oxford University Press; New York, NY: 1996. pp. 115–121. [Google Scholar]
- 4.Granger CV, Hamilton BB. The Uniform Data System for Medical Rehabilitation report of first admission for 1991. Am J Phys Med Rehabil. 1993;72:33–38. doi: 10.1097/00002060-199302000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Jensen MP, Abresch RT, Carter GT. The reliability and validity of a self-report version of the FIM instrument in persons with neuromuscular disease and chronic pain. Arch Phys Med Rehabil. 2005;86(1):116–122. doi: 10.1016/j.apmr.2004.01.040. [DOI] [PubMed] [Google Scholar]
- 6.Hershkovitz A, Kalandariov Z, Hermush V, Weiss R, Brill S. Factors affecting short-term rehabilitation outcomes of disabled elderly patients with proximal hip fracture. Arch Phys Med Rehabil. 2007;88(7):916–921. doi: 10.1016/j.apmr.2007.03.029. [DOI] [PubMed] [Google Scholar]
- 7.Granger CV, Cotter AC, Hamilton BB, et al. Functional assessment scales: a study of persons with multiple sclerosis. Arch Phys Med Rehabil. 1990 Oct;71(11):870–875. [PubMed] [Google Scholar]
- 8.Granger CV, Hamilton BB, Linacre JM, et al. Performance profiles of the functional independence measure. Am J Phys Med Rehabil. 1993 Apr;72(2):84–89. doi: 10.1097/00002060-199304000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Dodds TA, Martin DP, Stolov WC, Deyo RA. A validation of the functional independence measurement and its performance among rehabilitation inpatients. Arch Phys Med Rehabil. 1993 May;74(5):531–536. doi: 10.1016/0003-9993(93)90119-u. [DOI] [PubMed] [Google Scholar]
- 10.Keith RA, Granger CV, Hamilton BB, Sherwin FS. The functional independence measure: a new tool for rehabilitation. Adv Clin Rehabil. 1987;1:6–18. [PubMed] [Google Scholar]
- 11.Granger CV, Cotter AC, Hamilton BB, Fiedler RC. Functional assessment scales: a study of persons after stroke. Arch Phys Med Rehabil. 1993 Feb;74(2):133–138. [PubMed] [Google Scholar]
- 12.Disler PB, Roy CW, Smith BP. Predicting hours of care needed. Arch Phys Med Rehabil. 1993 Feb;74(2):139–143. [PubMed] [Google Scholar]
- 13.Rockwood K, Stolee P, Fox RA. Use of goal attainment scaling in measuring clinically important change in the frail elderly. J Clin Epidemiol. 1993 Oct;46(10):1113–1118. doi: 10.1016/0895-4356(93)90110-m. [DOI] [PubMed] [Google Scholar]
- 14.Di Scala C, Grant CC, Brooke MM, Gans BM. Functional outcome in children with traumatic brain injury. Agreement between clinical judgment and the functional independence measure. Am J Phys Med Rehabil. 1992 Jun;71(3):145–148. doi: 10.1097/00002060-199206000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Pollak N, Rheault W, Stoecker JL. Reliability and validity of the FIM for persons aged 80 years and above from a multilevel continuing care retirement community. Arch Phys Med Rehabil. 1996 Oct;77(10):1056–1061. doi: 10.1016/s0003-9993(96)90068-4. [DOI] [PubMed] [Google Scholar]
- 16.Kidd D, Stewart G, Baldry J, et al. The Functional Independence Measure: a comparative validity and reliability study. Disabil Rehabil. 1995 Jan;17(1):10–14. doi: 10.3109/09638289509166622. [DOI] [PubMed] [Google Scholar]
- 17.Masedo AI, Hanley M, Jensen MP, Ehde D, Cardenas DD. Reliability and validity of a self-report FIM (FIM-SR) in persons with amputation or spinal cord injury and chronic pain. Am J Phys Med Rehabil. 2005;84(3):167–176. doi: 10.1097/01.phm.0000154898.25609.4a. [DOI] [PubMed] [Google Scholar]
- 18.Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC. The reliability of the functional independence measure: a quantitative review. Arch Phys Med Rehabil. 1996;77(12):1226–1232. doi: 10.1016/s0003-9993(96)90184-7. [DOI] [PubMed] [Google Scholar]
- 19.Daving Y, Andrén E, Nordholm L, Grimby G. Reliability of an interview approach to the Functional Independence Measure. Clin Rehabil. 2001;15(3):301–310. doi: 10.1191/026921501669986659. [DOI] [PubMed] [Google Scholar]
- 20.Smith PM, Illig SB, Fiedler RC, Hamilton BB, Ottenbacher KJ. Intermodal agreement of follow-up telephone functional assessment using the Functional Independence Measure in patients with stroke. Arch Phys Med Rehabil. 1996;77(5):431–435. doi: 10.1016/s0003-9993(96)90029-5. [DOI] [PubMed] [Google Scholar]
- 21.Stineman MG, Shea JA, Jette A, et al. The Functional Independence Measure: tests of scaling assumptions, structure, and reliability across 20 diverse impairment categories. Arch Phys Med Rehabil. 1996 Nov;77(11):1101–1108. doi: 10.1016/s0003-9993(96)90130-6. [DOI] [PubMed] [Google Scholar]
- 22.Beloosesky Y, Grinblat J, Epelboym B, Hendel D. Dementia does not significantly affect complications and functional gain in elderly patients operated on for intracapsular hip fracture. Arch Orthop Trauma Surg. 2001 May;121(5):257–260. doi: 10.1007/s004020000220. [DOI] [PubMed] [Google Scholar]
- 23.Heruti RJ, Lusky A, Barell V, et al. Cognitive status at admission: does it affect the rehabilitation outcome of elderly patients with hip fracture? Arch Phys Med Rehabil. 1999 Apr;80(4):432–436. doi: 10.1016/s0003-9993(99)90281-2. [DOI] [PubMed] [Google Scholar]
- 24.Goldstein FC, Strasser DC, Woodard JL, Roberts VJl. Functional outcome of cognitively impaired hip fracture patients on a geriatric rehabilitation unit. J Am Geriatr Soc. 1997 Jan;45(1):35–42. doi: 10.1111/j.1532-5415.1997.tb00975.x. [DOI] [PubMed] [Google Scholar]
- 25.Mortifee PR, Busser J, Anton HA. The performance of a limited set of items from the Functional Independence Measure for use in acute trauma care and rehabilitation. Arch Phys Med Rehabil. 1996 May;77(5):436–439. doi: 10.1016/s0003-9993(96)90030-1. [DOI] [PubMed] [Google Scholar]
- 26.Weh L, Ramb JF. Functional Independence Measure as a predictor of expected rehabilitation outcome in patients with total endoprosthesis replacement and after apoplectic infarct. Z Orthop Ihre Grenzgeb. 1992 Jul–Aug;130(4):333–338. doi: 10.1055/s-2008-1039627. [DOI] [PubMed] [Google Scholar]