Abstract
In a cohort of Maryland Medicaid recipients with severe mental illness followed from 1993-2001, we compared mortality to the Maryland general population including race and gender subgroups. Persons with severe mental illness died at a mean age of 51.8 years, with a standardized mortality ratio of 3.7 (95%CI, 3.6-3.7).
Keywords: severe mental illness, mortality, Medicaid
1. Introduction
Persons with severe mental illnesses comprise a vulnerable population with high prevalence of medical comorbid conditions. Obesity, diabetes mellitus, chronic lung disease, HIV and hepatitis B and C afflict persons with severe mental illness at least two to five times as commonly as the general population.(Rosenberg, et al. 2001; Daumit et al. 2003; Carney, et al. 2006) This overwhelming medical disease burden is due in part to unhealthy behaviors including tobacco smoking, diet, physical inactivity, and substance abuse.(Regier, et al. 1990; McCreadie 2003; Daumit, et al. 2005) Second generation antipsychotics’ effects on weight and glucose confer important additional risk for obesity and diabetes.(Allison, et al. 1999; Lean and Pajonk 2003)
Persons with chronic mental illness have higher overall mortality rates than the general population, with increased risk for suicide and other accidental deaths.(Dembling, et al. 1999; Brown, et al. 2000; Laursen, et.al. 2007) Some studies have also shown higher mortality rates for natural causes of death (Laursen, et.al. 2007), although most were performed before the advent of atypical antipsychotic medications with their risk of weight gain and metabolic syndrome. (Black, et al. 1985; Black, et al. 1985; Felker, et al. 1996; Brown 1997; Osby, et al. 2000) While U.S. population mortality rates are higher for African-Americans compared to Whites, and men compared to women, less is known about whether these patterns exist in persons with chronic mental illness.(Jemal, et al. 2008)
Our objectives were to examine cause-specific mortality for a large, community-based cohort of persons with severe mental illnesses in Maryland compared to the Maryland general population, and to examine mortality in race and gender subgroups.
2. Methods
2.1 Study Design and Population
We conducted a retrospective cohort study of Maryland Medicaid recipients with severe mental illnesses. The cohort included adults, ages 21 to 62 years between July 1, 1992 and July 1,1993, who had severe mental illness using criteria based on diagnosis, disability and duration of illness.(Skinner, et al. 1999) Criteria included having any schizophrenia diagnosis or being disabled (Supplemental Security Income) with a diagnosis of bipolar disorder, major depression, or other mental disorder diagnoses and specialty mental health care use. Other diagnoses included psychoses other than schizophrenia and affective psychoses, organic psychoses, obsessive compulsive disorder and other anxiety disorders but not substance induced psychoses or dementias. Participants needed two years continuous enrollment in Maryland Medicaid between July 1, 1992 and June 30, 1994. All Maryland Medicaid recipients meeting these criteria living in the Baltimore metropolitan area or the more rural Maryland Eastern Shore comprised the cohort.(Skinner, et al. 1999) The Johns Hopkins Bloomberg School of Public Health and the Maryland Department of Health and Mental Hygiene institutional review boards approved the study.
2.2 Data Sources
Medicaid administrative claims data files provided information on age, gender, race, county, Medicaid enrollment and diagnoses. Mental health diagnoses (schizophrenia, bipolar disorder, depression, other) were established at the initiation of the cohort. Medical and alcohol/substance abuse diagnoses were obtained from administrative data through 2001. To obtain dates and causes of death, we linked data in the cohort to the National Death Index from 1994 through 2001. We obtained data on age, race and gender of the Maryland State population and deaths from 1999-2001 from the Maryland Department of Vital Statistics.
2.3 Analysis
We used direct adjustment to the United States 2000 population for each of five age groups (25-34, 35-44, 45-54, 55-64, 65+), race (White, non-White) and sex and calculated standardized death rates for both the Maryland cohort with severe mental illness and the Maryland general population. The ratio of standardized death rates in the severely mentally ill cohort to standardized death rates in the Maryland general population provided standardized mortality ratios (SMRs). We calculated 95 percent confidence intervals for SMRs. We used Stata 9.0 for analyses.
3.0 Results
3.1 Population Characteristics of Maryland Medicaid Cohort with Severe Mental Illness
At the beginning of the study period in 1994, the mean age was 41.6 years. Thirty percent were younger than 35, 54% were between 35 and 54, and 16% were 55 years and older. Fifty-four percent were women, 51% were African-American, and 98% were disabled, receiving SSI. Ninety-two percent lived in the Baltimore metropolitan area. Persons with schizophrenia diagnoses comprised 37% of the sample, with bipolar disorder and depression each 17%. Sixteen percent had alcohol or substance abuse recorded. The cohort had the following medical conditions: 30% with chronic obstructive pulmonary disease; 24% diabetes mellitus; 17% hypertension; 13% malignancy; 8% liver disease; 7% kidney disease and 7% HIV.
3.2 Mortality
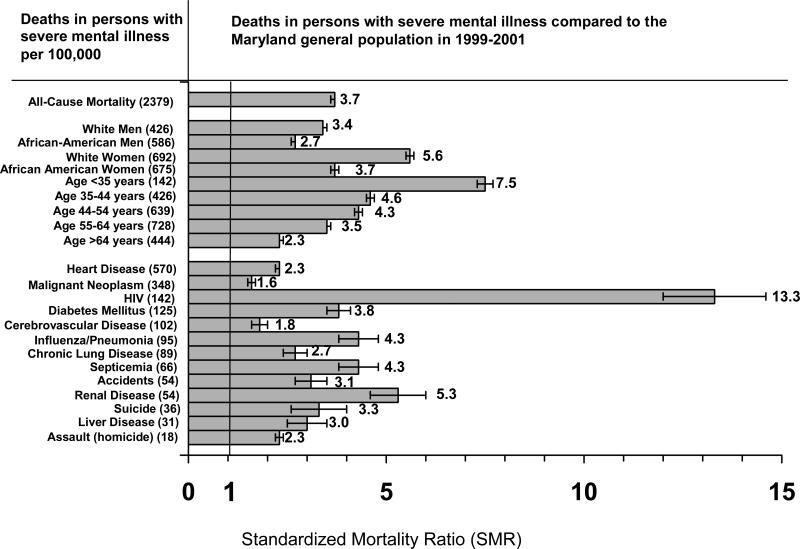
Between 1994 and 2001, 1002 persons (16.1%) in the cohort with severe mental illness died, with the mean age of death of 51.8 (SD 11.1) years. The SMR for the cohort with severe mental illness compared to the Maryland general population for 1999-2001 was 3.7, 95% CI (3.6, 3.7)) (Figure), with elevated SMRs across all diagnostic categories. With the exception of HIV, the third most common cause of death in persons with severe mental illness (6%), the most common causes of death in those with severe mental illness (heart disease (24%), malignant neoplasm (15%), diabetes mellitus (5%), cerebrovascular disease (4%) and chronic lung disease (4%)) were similar to the Maryland general population. Although SMRs were elevated for accidental death, homicide and suicide, overall these accounted for less than 5% of deaths in severe mental illness.
figure.
Deaths and causes of death per 100,000 in persons with severe mental illness in Maryland 1999-2001 and standardized mortality ratio of persons with severe mental illness compared to the Maryland general population. Numbers in parentheses depict deaths in persons with severe mental illness per 100,000. Horizontal bars with point estimates depict standardized mortality ratios. 95% CIs are depicted by error bars.
Standardized mortality rates were increased across age groups, particularly in ages younger than 35 years (SMR of 7.5, 95%CI (7.3, 7.7)). Those with severe mental illness and a substance abuse diagnosis had an SMR of 5.4, 95%CI (5.3, 5.4) compared to the Maryland general population (data not shown).
White women with severe mental illness had the highest SMR compared to White women in the Maryland general population (5.6, 95% CI (5.5, 5.7)) and African American men with severe mental illness had the lowest relative SMR, although still elevated at 2.7 (95% CI, (2.6, 2.7)) (Figure). Within the severe mental illness population, the age-adjusted ratio of deaths for African-American men compared to White men was 1.38 (586/426 deaths per 100,000, from Figure), for African-American compared to White women it was 0.98. For all women compared to all men, the ratio of deaths was 1.35, and for African Americans compared to Whites it was 1.13.
For cohort members with a diagnosis of schizophrenia, 12.4% died and the SMR was 3.0, 95% CI (2.9,3.1); for cohort members with bipolar disorder, 18.1% died and the SMR was 3.8, 95% CI (3.7,3.9). For heart disease, the SMR was 1.8 95% CI (1.7,1.9) for schizophrenia and 3.1 95% CI (3.0,3.2) for bipolar disorder. For cancer, the SMR was 1.4 95% CI (1.3,1.5) for schizophrenia and 1.3 95% CI (1.2,1.4) for bipolar disorder (data not shown).
4.0 Discussion
In this retrospective cohort study of a community-based sample of Maryland Medicaid recipients with severe mental illness, we found over 16% of the cohort died within seven years at a mean age of less than 52 years. Compared to the Maryland general population, the standardized mortality ratio was over three and a half times higher in the cohort with severe mental illness, with the main causes of death very similar. Alcohol and substance abuse diagnoses conferred increased risk of death. Mortality rates for those with severe mental illness were elevated particularly in young adults.
Our results are consistent with other studies documenting the overall high mortality rate of populations with chronic mental illness. Mortality rates for heart disease and cancer have been inconsistently elevated in persons with severe mental illness in older studies, although more recent cross-sectional work has shown that these are important causes of death in populations of clients in the public mental health system.(Brown 1997; Colton and Manderscheid 2006) A retrospective cohort study from Britain in persons with schizophrenia reported similar relative risks for mortality from heart disease and stroke as our results, but no elevation in mortality for common cancers.(Osborn, et al. 2007) A recent literature synthesis showed SMRs for heart disease and cancer in schizophrenia comparable to our estimates.(Saha, et al. 2007)
Our results underscore the importance of vascular-related disease and cancer in persons with severe mental illness. Heart disease, diabetes mellitus and cerebrovascular disease combined account for one third of all deaths from vascular-related disease and adding cancer increases the proportion to almost half of all deaths due to these causes. A myriad of factors contribute to risk for cardiovascular disease and cancer in persons with severe mental illness. Psychotropic medications contribute to obesity and diabetes, and lifestyle behaviors such as unhealthy diet and smoking increase risk for vascular-related disease and cancers.(Allison, et al. 1999; Daumit, et al. 2003; McCreadie 2003) Poorer quality health care to prevent, detect and appropriately treat these conditions in persons with severe mental illness may also contribute to higher death rates.(Druss, et al. 2000)
Although elevated at over three times the SMR of the general population, we found lower standardized mortality ratios for suicide compared to literature syntheses where SMRs for suicide were elevated at 8 to 12 times the general population. Our findings may be explained in part by many published studies using inpatient or clinic-based samples who may be at higher risk for self-harm. (Brown, 1997; Saha, et.al. 2007).
We believe this is one of the first reports to describe mortality rates in persons with severe mental illness stratified by race and gender. While all race and gender groups with severe mental illness had increased SMRs compared to the corresponding Maryland general population categories, the SMR in mental illness was higher for White men than for African-American men and for White women than for African-American women. African American adults in the U.S. population are known to have higher mortality rates than Whites by a factor of up to 1.9.(Jemal, et al. 2008); in this cohort with severe mental illness, this disparity was substantially narrowed. Possibly, lower socioeconomic status across both Whites and African Americans in this Medicaid population contributed to decreased racial disparity in death rates compared to those seen in the general population. In addition, contrary to general population estimates, within the cohort with severe mental illness, women had higher mortality rates than men. (Minino and Smith et.al., 2001)
An important strength of this study is its use of a large cohort of persons with severe mental illness enrolled in Medicaid, not a sample limited to psychiatric hospitals or clinic attendees. We also included age, race and gender in our analyses. The mean age of death in the cohort reflects the relatively young mean age of 41.6 years in the sample. One limitation is that we could not incorporate detailed patient characteristics such as tobacco smoking to assess differences in causes of death.
Another limitation is that while we had a defined cohort by age, enrollment, severe mental illness criteria and geographic region, this sample does not include all persons with severe mental illness in Maryland, and thus may not reflect the mortality experience of all with severe mental illness in the state. We estimate that this cohort represents approximately one third of Maryland Medicaid recipients with severe mental illness, and about 20% of persons with severe mental illness in Maryland. The sample was designed to include persons with severe mental illness using diagnostic and disability criteria. Virtually all in the study cohort (98%) met criteria based on diagnosis and disability. While this analysis compares a Medicaid cohort with severe mental illness to the Maryland general population, we did not have data on a Medicaid population without mental illness, which may be an informative comparison of persons with more similar socioeconomic backgrounds than the general population.
Reliability and validity of demographic variables can be a concern with administrative claims data. However, we found that race and gender were stable in the enrollment files throughout the duration of the cohort. In addition, in interview data from another study using this cohort (Daumit, et.al, 2003), gender matched Medicaid claims in 99.6% of participants, and race matched in 97.5% of participants.
In conclusion, we found high rates of premature death from preventable medical conditions in a cohort of persons with severe mental illness compared to the Maryland general population. Unlike U.S. mortality rates, in this population with severe mental illness, age-adjusted mortality rates in women were one third higher than in men, and in African Americans were only 10 percent higher than in Whites. Vascular-related diseases and cancer accounted for almost half of all deaths. Further work to understand how to decrease mortality rates in this vulnerable population with severe mental illness is needed urgently.
ACKNOWLEDGEMENTS
This work was supported by the National Alliance for Research on Schizophrenia and Depression Young Investigators Award and National Institute of Mental Health R01MH49250. We thank the Maryland Department of Health and Mental Hygiene for their collaboration.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Allison DB, Mentore JL, Heo M, Chandler LP, Cappelleri JC, Infante MC, Weiden PJ. Antipsychotic-induced weight gain: a comprehensive research synthesis. American Journal of Psychiatry. 1999;156:1686–96. doi: 10.1176/ajp.156.11.1686. [DOI] [PubMed] [Google Scholar]
- Black DW, Warrack G, Winokur G. The Iowa record-linkage study. I. Suicides and accidental deaths among psychiatric patients. Archives of General Psychiatry. 1985;42:71–5. doi: 10.1001/archpsyc.1985.01790240073007. [DOI] [PubMed] [Google Scholar]
- Black DW, Warrack G, Winokur G. The Iowa record-linkage study. III. Excess mortality among patients with 'functional' disorders. Archives of General Psychiatry. 1985;42:82–8. doi: 10.1001/archpsyc.1985.01790240084009. [DOI] [PubMed] [Google Scholar]
- Brown S. Excess mortality of schizophrenia. A meta-analysis. British Journal of Psychiatry. 1997;171:502–8. doi: 10.1192/bjp.171.6.502. [DOI] [PubMed] [Google Scholar]
- Brown S, H. Inskip H, Barraclough B. Causes of the excess mortality of schizophrenia. British Journal of Psychiatry. 2000;177:212–7. doi: 10.1192/bjp.177.3.212. [DOI] [PubMed] [Google Scholar]
- Carney CP, Jones L, Woolson RF. Medical comorbidity in women and men with schizophrenia: a population-based controlled study. Journal of General Internal Medicine. 2006;21:1133–7. doi: 10.1111/j.1525-1497.2006.00563.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colton CP, Manderscheid RW. Congruencies in Increased Mortality Rates, Years of Potential Life Lost, and Causes of Death Among Public Mental Health Clients in Eight States. Preventing Chronic Disease. 2006;3:1–14. [PMC free article] [PubMed] [Google Scholar]
- Daumit GL, Clark JM, Steinwachs DM, Graham CM, Lehman A, Ford DE. Prevalence and Correlates of Obesity in a Community Sample of Individuals with Severe and Persistent Mental Illness. Journal of Nervous and Mental Disease. 2003;191:799–805. doi: 10.1097/01.nmd.0000100923.20188.2d. [DOI] [PubMed] [Google Scholar]
- Daumit GL, Goldberg RW, Anthony C, Dickerson F, Brown CH, Kreyenbuhl J, Wohlheiter K, Dixon LB. Physical activity patterns in adults with severe mental illness. Journal of Nervous and Mental Disease. 2005;193:641–6. doi: 10.1097/01.nmd.0000180737.85895.60. [DOI] [PubMed] [Google Scholar]
- Dembling BP, Chen DT, Vachon L. Life expectancy and causes of death in a population treated for serious mental illness. Psychiatric Services. 1999;50:1036–42. doi: 10.1176/ps.50.8.1036. [DOI] [PubMed] [Google Scholar]
- Druss BG, Bradford DW, Rosenheck RA, Radford MJ, Krumholz HM. Mental disorders and use of cardiovascular procedures after myocardial infarction. Journal of the American Medical Association. 2000;283:506–11. doi: 10.1001/jama.283.4.506. [DOI] [PubMed] [Google Scholar]
- Felker B, Yazel JJ, Short D. Mortality and medical comorbidity among psychiatric patients: a review. Psychiatric Services. 1996;47:1356–63. doi: 10.1176/ps.47.12.1356. [DOI] [PubMed] [Google Scholar]
- Jemal A, Thun MJ, Ward EE, Henley SJ, Cokkinides VE, Murray TE. Mortality from leading causes by education and race in the United States, 2001. American Journal of Preventive Medicine. 2008;34:1–8. doi: 10.1016/j.amepre.2007.09.017. [DOI] [PubMed] [Google Scholar]
- Laursen TM, Munk-Olsen T, Nordentoft M, Mortensen PB. Increased mortality among patients admitted with major psychiatric disorders: a register-based study comparing mortality in unipolar depressive disorder, bipolar affective disorder, schizoaffective disorder and schizophrenia. Journal of Clinical Psychiatry. 2007;68:899–907. doi: 10.4088/jcp.v68n0612. [DOI] [PubMed] [Google Scholar]
- Lean ME, Pajonk FG. Patients on Atypical Antipsychotic Drugs: Another high-risk group for type 2 diabetes. Diabetes Care. 2003;26:1597–605. doi: 10.2337/diacare.26.5.1597. [DOI] [PubMed] [Google Scholar]
- McCreadie RG. Diet, smoking and cardiovascular risk in people with schizophrenia: descriptive study. British Journal of Psychiatry. 2003;183:534–9. doi: 10.1192/bjp.183.6.534. [DOI] [PubMed] [Google Scholar]
- Minino AM, Smith BL. Deaths: preliminary data for 2000. National Vital Statistics Report. 2001;49:1–40. [PubMed] [Google Scholar]
- Osborn DP, Levy G, Nazareth I, Petersen I, Islam A, King MB. Relative risk of cardiovascular and cancer mortality in people with severe mental illness from the United Kingdom's General Practice Rsearch Database. Archives of General Psychiatry. 2007;64:242–9. doi: 10.1001/archpsyc.64.2.242. [DOI] [PubMed] [Google Scholar]
- Osby U, Correia N, Brandt L, Ekborn A, Sparen P. Mortality and causes of death in schizophrenia in Stockholm county, Sweden. Schizophrenia Research. 2000;45:21–8. doi: 10.1016/s0920-9964(99)00191-7. [DOI] [PubMed] [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area ECA Study. Journal of the American Medical Assocation. 1990;264:2511–8. [PubMed] [Google Scholar]
- Rosenberg SD, Goodman LA, Osher FC, Swartz MS, Essock SM, Butterfield MI, Constantine NT, Wolford GL, Salyers MP. Prevalence of HIV, Hepatitis B, and Hepatitis C In People With Severe Mental Illness. American Journal of Public Health. 2001;91:31–7. doi: 10.2105/ajph.91.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Archives of General Psychiatry. 2007;64:1123–31. doi: 10.1001/archpsyc.64.10.1123. [DOI] [PubMed] [Google Scholar]
- Skinner EA, Steinwachs DM, Handley K, Lehman A, Fahey M, Lyles CA. Met and Unmet Needs for Assistance and Quality of Life for People with Severe and Persistent Mental Disorders. Mental Health Services Research. 1999;1:109–118. [Google Scholar]