Introduction
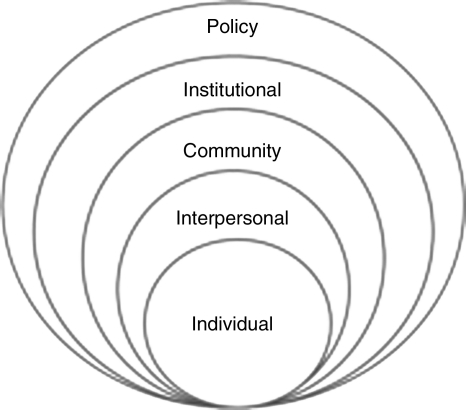
My objective in this article is to raise questions about sources of environmental toxins and possible effects on lactogenesis. Toxins are known to interrupt normal biological functioning. The effects of exposures to toxins and the underlying biological mechanisms are not well understood. Many possible negative influences on lactogenesis are not even considered for empirical research. For my purposes, toxins are defined broadly to include physical toxins (e.g., chemicals, hormones, drugs), as well as social toxins (unemployment, inadequate safety, lack of access to education) and emotional toxins (fear, uncertainty, humiliation). The social ecological model, shown in Figure 1, is a multilevel systems approach used in public health to consider multiple influences on health. The model looks at individual health behaviors (such as breastfeeding) within an expanded context of interpersonal relationships, community, institutions, and policies. The model can guide investigations and suggest sites for intervention that have significant impact.
FIG. 1.
Social ecological model.
The literature is replete with studies seeking to identify mothers' difficulties in sustaining exclusive breastfeeding. Mothers across studies, across ethnic groups, and across social classes all cite an insufficient or inadequate milk supply as an important reason for stopping exclusive breastfeeding before 6 months.1 By contrast, among health professionals, physical problems that inhibit milk production are believed to be very rare, with only about 4% of women thought to have this condition. This is a significant disconnect between what science says and what women tell us. This disconnect is relatively unexplored. Where are the follow-up studies that can pinpoint reasons for this discrepancy? Implicit in the lack of follow-up is an assumed failure of women to use the right techniques in breastfeeding, that they are lying, or that they don't really want to breastfeed. Studies to evaluate whether or not new mothers are indeed not producing milk are rare. If we assume women are at fault, the intervention is isolated at the individual level, and the optimal solution is to educate women on correct techniques and benefits of breastfeeding.
What if we took women at their word? What if we believed what they were telling us? What could cause a biological failure to produce an adequate milk supply in a new mother? If we took women seriously this would change our research questions. This would change how and where we intervene to support breastfeeding.
Environmental Toxins
University of Rochester (Rochester, NY) immunologist Paige Lawrence studies the effects of dioxin exposure on biological functions using a mouse model. Dioxins are highly toxic chemicals, ubiquitous in the environment. They are the by-product of industrial processes and the incineration of garbage. Humans are exposed primarily through food, especially dairy products, meat, and seafood. Vorderstrasse et al.2 found that when they exposed mice to dioxin in early pregnancy, their mammary glands failed to develop, and the animals were not able to produce milk; the mice pups died within a few days. In the United States, dioxin exposure is assumed to be widespread. Dioxins are just one group of chemicals among thousands whose effects on human biological functions are uncertain. Other physical exposures hypothesized to impair milk production in humans include epidurals, medroxyprogesterone (Depo-Provera®, Pfizer, New York, NY), and secondhand tobacco smoke. There are no published studies to examine this relationship, although several are underway. If toxic environmental exposures did disrupt lactogenesis, the intervention would be at the policy and institutional levels to reduce population exposure to these toxins, not at the level of the individual mothers.
Social Toxins
Low-income mothers, the group most likely to report insufficient milk, have reduced access to societal supports in raising young children. This often includes insufficient wages to support a family, inadequate housing, high crime neighborhoods, poor public transportation, lack of access to quality child care, and weak public education K–12. Return to work or school involves painful decisions about how to feed their babies. In interview studies our team has conducted with low-income mothers, they describe the stress and extreme exhaustion of managing child-rearing in such a “toxic environment.” While these situations have been documented as influencing mothers' decisions to discontinue breastfeeding and use formula, might there be a biological response to these social “toxins” that would reduce their milk supply? An intervention to mitigate this toxin would occur at the community and institutional levels, not at the level of the individual mothers.
Emotional Toxins
Low-income women may be subject to daily humiliations in trying to breastfeed their infants. Low-income mothers have reported verbal harassment when trying to breastfeed on a public bus, for example. They have been subject to derogatory comments from supervisors and coworkers for extra breaks taken to pump milk when they return to work. They worry that breastfeeding in public is seen as a sexual act rather than a maternal act. Ethnographic studies of the lives of low-income women document an extraordinary amount of violence they face on a daily basis. This violence is manifest on three different levels—interpersonal, community, and institutional. Many low-income women live in fear. Understanding the sources and effects of emotional toxins requires studies and interventions done at the policy, institutional, community, interpersonal, and individual levels. The article by Cerulli et al.3 in this issue provides a powerful statement on the emotional lives of domestic violence victims and possible effects on breastfeeding. We need more studies like theirs.
Actions
The following action steps are recommended:
Empirical studies of the influence of toxins—physical, social, and emotional—on lactogenesis
Screening prenatally for domestic violence
Creation of safe environments for new mothers in the community, household, and institutions free from chemical toxins, harassment, and violence
Sustained cultural change in interpreting breastfeeding as good mothering
Acknowledgments
This investigation was supported by U.S. Public Health Service grant RO1-HD055191, Community Partnership for Breastfeeding Promotion and Support. The author thanks the Breastfeeding Research Group at the University of Rochester School of Medicine and Dentistry (Ann Dozier, convener) for their input and feedback into this work.
Disclosure Statement
No competing financial interests exist.
References
- 1.Li R. Fein BF. Chen J, et al. Why mothers stop breastfeeding: Mothers' self-reported reasons for stopping during the first year. Pediatrics. 2008;122(Suppl 2):S69–S76. doi: 10.1542/peds.2008-1315i. [DOI] [PubMed] [Google Scholar]
- 2.Vorderstrasse BA. Fenton SE. Bohn AA, et al. A novel effect of dioxin: Exposure during pregnancy severely impairs mammary gland differentiation. Toxicol Sci. 2004;78:248–257. doi: 10.1093/toxsci/kfh062. [DOI] [PubMed] [Google Scholar]
- 3.Cerrulli C. Chin N. Talbot N. Chaudron L. Exploring the impact of intimate partner violence on breastfeeding initiation: Does it matter? Breastfeed Med. 2010;5:225–226. doi: 10.1089/bfm.2010.0054. [DOI] [PMC free article] [PubMed] [Google Scholar]