SYNOPSIS
Objective
We examined actions to control high blood pressure (HBP) and health-care provider recommendations for blood pressure control among adults by racial/ethnic group and rural/urban residence.
Methods
We examined data from 45,024 participants with HBP in the 2007 Behavioral Risk Factor Surveillance System (BRFSS) survey. We used multiple logistic regression analyses to assess the independent association between current actions to control HBP and health-care provider recommendations for blood pressure control by race/ethnicity and rural/urban status after accounting for confounders.
Results
Black people, regardless of rural or urban residence, were more likely to report reducing salt and alcohol intake, changing eating habits, and taking medications than both white urban and white rural adults. Black people,regardless of rural or urban status, were more likely to be advised to cut down on salt, reduce alcohol use, and change eating habits. Black rural adults were also more likely to report being advised to take medications than white urban adults, while white rural adults were less likely to be advised to exercise than white urban adults.
Conclusions
Race/ethnicity and rural/urban status have a differential effect on actions to control HBP and provider advice to control HBP.
High blood pressure (HBP) or hypertension is a global health-related challenge with a high prevalence worldwide. Twenty-six percent of the adult population worldwide had HBP in 2000, and this number is projected to increase to nearly 30% in 2025.1 These figures are of considerable concern because HBP is the leading cause of cardiovascular disease,2 the leading risk factor associated with mortality,3 and the third leading cause of disability-adjusted life-years.3 Recent data from the Centers for Disease Control and Prevention (CDC) National Center for Health Statistics suggest HBP prevalence of about 29% among adults aged 18 years or older in the U.S. in 2005–2006.4 The estimated direct and indirect cost of HBP in the U.S. for 2009 was $73.4 million.5 Taken together, these data highlight the significant burden of HBP on both individuals and society.
There is considerable interest in better understanding current racial/ethnic differences in the prevalence of HBP. Data from the National Health and Nutrition Examination Survey (NHANES) revealed a significantly higher prevalence of HBP among black compared with white people in the U.S.4,6 From 2005 to 2006, the age-adjusted prevalence of hypertension for the entire study population was 29%; however, the prevalence among black people was higher than among white people (41% vs. 28%).4
Higher rates of HBP among African Americans were also reported from the Multi-Ethnic Study of Atherosclerosis, a population-based study of adults without clinical cardiovascular disease designed to examine the association among ethnicity, HBP, and HBP treatment. The prevalence of HBP was significantly higher in African Americans (60%) compared with Caucasians (38%) (p<0.001), and the percentage of adults treated for HBP who remained uncontrolled adults was also higher among African Americans (35%) compared with Caucasians (24%) (p<0.0001). These findings suggest significant disparities in the prevalence of HBP among U.S. black adults—a group with one of the highest HBP prevalences in the world. More alarming, there are data to suggest that black people develop HBP earlier in life, are at 1.8 times greater risk of fatal stroke, and are at 1.5 times greater risk of end-stage kidney disease than other racial/ethnic groups.7 In addition, a study by Hertz and colleagues noted a racial disparity in blood pressure control even among those who were being treated pharmacologically that could not be explained by non-pharmacologic management, health insurance, or educational attainment.8
There are also data to suggest disparities in HBP prevalence by residential status. In multivariate models containing all available variables (e.g., age, race, gender, number of physician visits, comorbidities, and rural status), King and colleagues found that higher rates of uncontrolled HBP among males (odds ratio [OR] = 2.04, 95% confidence interval [CI] 1.17, 3.55) and individuals from a rural setting (OR=0.30, 95% CI 0.16, 0.55) were significantly associated with blood pressure control.9 In an analysis of data from NHANES III (1988–1994), which included 11,755 African American and white adults aged 20 years and older who were classified by residential status (rural or urban), Mainous and colleagues found HBP (diastolic blood pressure >90 millimeters of mercury [mmHg]) in 11% of rural white people, 13% of urban white people, 20% of urban African Americans, and 23% of rural African Americans (p<0.01). Interestingly, the prevalence of HBP was double among rural African Americans compared with rural white people even after controlling for access to care. Mainous et al. also found that rural African Americans were more likely to receive a provider recommendation for blood pressure medications than individuals from other racial/residential groups.10 However, despite receiving more recommendations for medications, a larger discrepancy (24.4%) existed between those African Americans who were recommended medications and those who were currently on medications (i.e., complied with the recommendation). In contrast, the discrepancy between rural white people who were given a recommendation to take medications and those who were currently taking medications was 17.0%.
Taken together, these findings highlight the need to better understand the interplay between racial/ethnic and rural/urban status in HBP control. We examined current actions to control blood pressure relative to provider-advised actions to control blood pressure in a national sample of adults with HBP. This study used data from the 2007 Behavioral Risk Factor Surveillance System (BRFSS)11 to determine if respondent-initiated actions to control blood pressure and health-care provider-recommended actions to control blood pressure differed by race and residential status. Additionally, we examined the independent effect of health-care provider advice on the odds of changing actions to control blood pressure. These data are critical to better understanding health disparities in HBP control at both the individual and provider levels.
RESEARCH DESIGN AND METHODS
Study setting and sample
We analyzed data from the 2007 BRFSS, a state-based, random-digit-dialing telephone survey of the U.S. adult population sponsored by CDC.11 The BRFSS uses a complex design involving stratification, clustering, and multistage sampling to yield nationally representative estimates.
Demographic and socioeconomic characteristics
The BRFSS provides information on a wide range of demographic and background characteristics. All key variables used in this study were based on self-report. For the purposes of the current study, we created four age categories: 18–34, 35–49, 50–64, and ≥65 years of age. We combined race and metropolitan status to create four racial/residential groups: urban white people, rural white people, urban black people, and rural black people. We then created four levels of education (<high school graduate, high school graduate, <college graduate, and college graduate) and four income categories (<$25,000; $25,000–$49,999; $50,000–$74,999; and ≥$75,000).
Marital, employment, and insurance status were recoded and treated as binary variables. For example, individuals who were divorced, widowed, separated, or never married were classified as “not married” relative to those who reported being married. We took the same approach for both employment and insurance status. In other words, we defined marital status as married vs. not married, employment status as employed vs. unemployed, and insurance status as insured vs. uninsured. Finally, we defined access to care as any visit to a health-care provider within 12 months of study participation, and perceived health status as excellent/very good/good vs. fair/poor.
High blood pressure
Presence of HBP was based on a participant's response (yes/no) to the following question: “Were you told on two or more different visits to a doctor or other health professional that you had HBP?”
Actions to control blood pressure
Respondent actions to control blood pressure were based on self-report. Responses were derived from the 2007 BRFSS Actions to Control Blood Pressure module. Respondents were asked, “Are you now doing any of the following to help lower or control your blood pressure?” Respondents indicated if they were (1) changing their eating habits, (2) cutting down on salt, (3) reducing alcohol use, and (4) exercising. Respondents were also asked, “Are you currently taking medications for your blood pressure?” as part of the 2007 BRFSS survey.
Advised actions to control blood pressure
Respondent provider-advised actions to control blood pressure were based on self-report. Responses were also derived from the 2007 BRFSS Actions to Control Blood Pressure module. Respondents were asked, “Has a doctor or other health-care professional ever advised you to do any of the following to help lower or control your blood pressure?” Respondents indicated if they were advised to (1) change their eating habits, (2) cut down on salt, (3) reduce their alcohol use, (4) exercise, or (5) take medications.
Statistical analyses
We used Stata® version 10.012 for all statistical analyses. We performed five types of analyses. First, we compared demographic characteristics of patients with HBP by race/residential status (urban white people, rural white people, urban black people, and rural black people) using Chi-square tests. Second, we compared actions to control blood pressure and health provider advice/recommendations to control blood pressure by race/residential status using Chi-square tests. Third, we ran separate multiple logistic regression models to assess the independent association between race/residential status and each action to control blood pressure and health provider advice/recommendation to control blood pressure. Fourth, we ran separate multiple logistic regression models to assess the independent effect of provider advice on the odds of changing behavior among those who received advice on actions to control blood pressure. Fifth, we ran separate multiple logistic regression models to assess the adjusted odds of completing actions to control blood pressure among a subpopulation of respondents who received specific health provider advice/recommendations to control blood pressure.
For each model, we used each action or advice/recommendation to control blood pressure as the dependent variable; race/residential status as the primary independent variable; and age, sex, education, income, marital status, employment, insurance status, and health status as covariates. We included all relevant demographic variables in the adjusted models because they were significantly different across race/residential groups and were conceptually related to the outcomes of interest.
RESULTS
The 2007 BRFSS sample included 430,912 adults. Of this number, 153,510 responded “yes” to the following question, “Have you ever been told by a doctor, nurse, or other health professional that you have high blood pressure?” These respondents represented 27.6% of the U.S. population based on weighted percentages. Subsequently, 56,398 of the 153,510 respondents were asked questions in the Actions to Control Blood Pressure module, which was administered in 21 states. CDC deems this sample representative of individuals with HBP in the U.S. population. Of the individuals who completed the module, 45,024 reported being told on two or more different visits to a doctor or other health professional that they had HBP. These individuals (n=45,024) comprised our final sample and were used for all analyses. We selected these individuals for our final sample because individuals with diagnosed HBP on two or more occasions had a high likelihood of having true HBP.
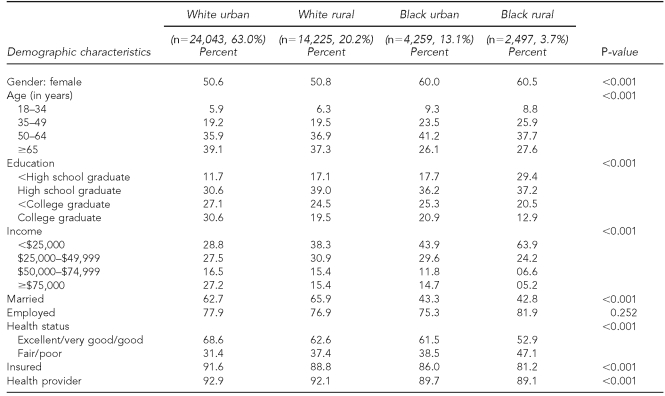
Of our final sample of 45,024 respondents, 63% were categorized as white urban, 20% as white rural, 13% as black urban, and 4% as black rural. Of this sample, 52% were female, 37% were ≥65 years of age, 33% had a high school education, and 34% had a household income <$25,000. Sixty percent were married; 77% were employed; 65% reported that their health was excellent, very good, or good; 90% were insured; and 92% had access to a health-care provider. Table 1 compares the demographic characteristics of adults with HBP by race/residential status (urban white people, rural white people, urban black people, and rural black people). There were significant differences in race/residential status by gender, age, education, income, marital status, perceived health status, insurance, and health provider.
Table 1.
Demographic characteristics of urban/rural black and white U.S. adults with high blood pressure (n=45,024)a
a2007 Behavioral Risk Factor Surveillance System survey: Actions to Control Blood Pressure module
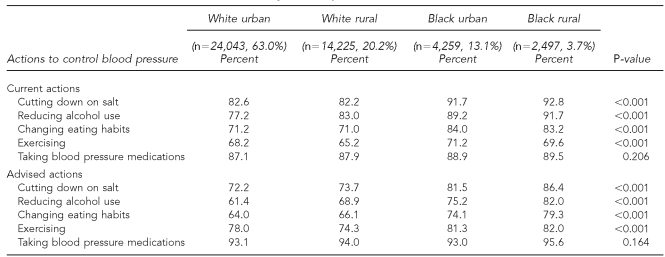
Table 2 compares current and advised actions to control blood pressure by race/residential status. Black rural and black urban adults were more likely to report cutting down on salt, reducing alcohol use, changing eating habits, and exercising as an action to control blood pressure than their white counterparts. Black rural and black urban adults also were more likely to report being advised to cut down on salt, reduce alcohol use, change their eating habits, and exercise than white urban and white rural adults. There were no statistically significant differences in the likelihood of being advised to take blood pressure medications by race/residential status.
Table 2.
Current and advised actions to control blood pressure among urban/rural black and white U.S. adults with high blood pressurea
a2007 Behavioral Risk Factor Surveillance System survey: Actions to Control Blood Pressure module
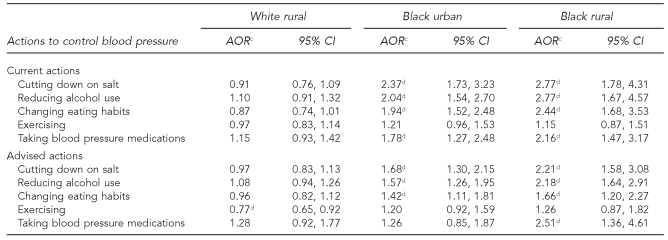
Table 3 presents the adjusted odds of current actions and advised actions to control blood pressure by race and residential status using white urban adults as the reference group and controlling for clinically relevant variables. In comparisons of current actions to control blood pressure, black urban adults were significantly more likely to report cutting down on salt (adjusted OR [AOR] = 2.37, 95% CI 1.73, 3.23), reducing alcohol use (AOR=2.04, 95% CI 1.54, 2.70), changing eating habits (AOR=1.94, 95% CI 1.52, 2.48), and taking medications (AOR=1.78, 95% CI 1.27, 2.48) than white urban adults. Similarly, black rural adults were significantly more likely to report cutting down on salt (AOR=2.77, 95% CI 1.78, 4.31), reducing alcohol use (AOR=2.77, 95% CI 1.67, 4.57), changing eating habits (AOR=2.44, 95% CI 1.68, 3.53), and taking medications (AOR=2.16, 95% CI 1.47, 3.17) than white urban adults.
Table 3.
Adjusted odds ratios of current and advised actions to control blood pressure among urban/rural black and white U.S. adults with high blood pressurea,b
a2007 Behavioral Risk Factor Surveillance System survey: Actions to Control Blood Pressure module
bWhite urban is the reference group.
cAdjusted for age, gender, education, income, marital status, employment status, health status, and insurance
dSignificant at p<0.05
AOR = adjusted odds ratio
CI = confidence interval
Comparisons of advised actions to control HBP by race and residential status indicated that black urban adults were significantly more likely to be advised to cut down on salt (AOR=1.68, 95% CI 1.30, 2.15), reduce alcohol use (AOR=1.57, 95% CI 1.26, 1.95), and change eating habits (AOR=1.42, 95% CI 1.11, 1.81) than white urban adults. Similarly, black rural adults were significantly more likely to report being advised to cut down on salt (AOR=2.21, 95% CI 1.58, 3.08), reduce alcohol use (AOR=2.18, 95% CI 1.64, 2.91), change eating habits (AOR=1.66, 95% CI 1.20, 2.27), and take medications (AOR=2.51, 95% CI 1.36, 4.61) than white urban adults. Finally, white rural adults were significantly less likely to report being advised to exercise (AOR=0.77, 95% CI 0.65, 0.92) than white urban adults.
To determine the independent effect of health provider advice on the odds of changing behavior for those who received advice, we completed additional analyses. We found that those respondents who were advised to cut down on salt were almost four times more likely to do so (OR=3.93, 95% CI 3.36, 4.60) than those who had not received specific advice. Similarly, those who were advised to reduce alcohol use were almost six times more likely to do so (OR=5.85, 95% CI 4.99, 6.86), those who were advised to change their eating habits were more than three times more likely to do so (OR=3.45, 95% CI 2.99, 3.98), those who were advised to exercise were two times more likely to do so (OR=2.07, 95% CI 1.76, 2.44), and those who were advised to take blood pressure medications were 38 times more likely to do so (OR=38.20, 95% CI 27.03, 53.98) than those who were not advised to take blood pressure medications. All values for these analyses were statistically significant at p<0.05 (data not shown).
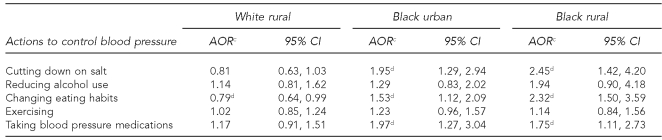
Table 4 presents the adjusted odds of current actions to control blood pressure among a subpopulation of individuals who received advice on actions to control blood pressure by race and residential status using, white urban adults as the reference group and controlling for clinically relevant variables. In comparisons of current actions to control blood pressure, black urban adults were significantly more likely to report cutting down on salt (AOR=1.95, 95% CI 1.29, 2.94), changing eating habits (AOR=1.53, 95% CI 1.12, 2.09), and taking medications (AOR=1.97, 95% CI 1.27, 3.04) than white urban adults. Similarly, black rural adults were significantly more likely to report cutting down on salt (AOR=2.45, 95% CI 1.42, 4.20), changing eating habits (AOR=2.32, 95% CI 1.50, 3.59), and taking medications (AOR=1.75, 95% CI 1.11, 2.73) than white urban adults.
Table 4.
Adjusted odds ratios of actions to control blood pressure among urban/rural black and white U.S. adults with high blood pressure who received advice to control blood pressurea,b
a2007 Behavioral Risk Factor Surveillance System survey: Actions to Control Blood Pressure module
bThe reference group is white urban.
cAdjusted for age, gender, education, income, marital status, employment status, health status, and insurance
dSignificant at p<0.05
AOR = adjusted odds ratio
CI = confidence interval
DISCUSSION
This study shows that a significant proportion of a racially/ethnically diverse national sample of U.S. adults residing in both urban and rural settings reported being currently involved in lifestyle modifications critical to the successful management of HBP. Similarly, the sample reported that they had also been advised by a health-care provider to make appropriate lifestyle modifications to manage HBP. To our knowledge, this is the first study to examine the reported actions of respondents and health-care provider-advised actions to control HBP by both race/ethnicity and residential status among adults with HBP.
This study had three major findings. First, black people were more likely to report current actions to control HBP and to report being advised by a health-care provider of actions to control HBP than their white counterparts. For example, in univariate analyses, both black rural and black urban respondents were more likely to report reducing salt intake and alcohol use, changing their eating habits, and exercising than white urban and white rural groups. Similarly, black rural and black urban respondents were more likely to report being advised to complete actions to control HBP, which included reducing salt and alcohol intake, changing eating habits, and exercising.
Second, provider advice was independently associated with an increased likelihood of actions to control blood pressure. Respondents who had been advised to change actions to control blood pressure were at least two times more likely to exercise and six times more likely to reduce alcohol use when advised to do so. More importantly, when advised to take blood pressure medications, respondents were 38 times more likely to do so compared with those who did not receive advice. Third, in adjusted models controlling for relevant demographic variables, black respondents (urban and rural) were about two to 2.8 times more likely to report three of the four actions to control HBP (cutting down on salt, reducing alcohol intake, and changing eating habits) and about two times more likely to report taking medications to reduce HBP than the reference group (i.e., urban white people). Likewise, black respondents (urban and rural) were about 1.5 to more than two times more likely to be advised of three of four actions to control HBP (cutting down on salt, reducing alcohol intake, and changing eating habits), while black rural respondents were 2.5 times more likely to report being advised to take blood pressure medications than white urban adults. Similar racial differences persisted when considering only those respondents who had received advice on actions to control blood pressure.
Our findings that black people (both rural and urban) were more likely to take preventative risk factor control measures initially suggests that black people should exhibit better control over their blood pressure than their white counterparts. However, studies of HBP traditionally report poor blood pressure control among racial/ethnic minorities relative to white people.6,7,10,13 Consequently, we recognize that reports of higher implementation of actions to control HBP do not equate to improved blood pressure control. That is, there is the possibility that respondents may be more likely to report appropriate risk factor control measures than are actually being completed.
According to the National Heart, Lung, and Blood Institute, cutting down on salt, reducing alcohol use, changing dietary habits, exercising, and taking blood pressure medications are recommended actions to improve blood pressure.14 Therefore, our primary findings of a high percentage of U.S. adults reporting involvement in lifestyle modifications and corresponding receipt of advice from health professionals to make appropriate lifestyle modifications suggest that health-care providers are regularly offering advice to U.S. adults for blood pressure control. The findings of this study agree with a previous report from CDC using 2005 BRFSS data from 20 states and three U.S. territories (Guam, Puerto Rico, and the U.S. Virgin Islands)15 that was designed to examine actions to control HBP. In a survey of 24,447 adults with HBP, 98.1% reported taking at least one action to lower or control their blood pressure, with the majority reporting taking each of the five actions as follows: 70.9% changed eating habits, 79.5% decreased use of salt or did not use salt, 79.2% reduced alcohol intake or did not drink alcohol, 68.6% exercised, and 73.4% took medications.15
Similarly, our results also agree with findings from the Healthstyles 2002 survey16 regarding advice to control HBP. Ayala and colleagues found that adults with HBP were more than five times more likely to have received advice from health-care providers to change eating habits or go on a diet and reduce salt intake (p<0.05) than adults not reporting HBP. In contrast, they were five times less likely to have been advised to exercise. Finally, those respondents with reported HBP were also more likely to take preventative actions to control HBP.16 All analyses were controlled for gender, race/ethnicity, and age. In summary, it appears that health-care providers are advising U.S. adults on the proper measures for blood pressure control.
We also note that in a recent study of advised actions to control HBP among hypertensive adults using 2005 BRFSS data, Viera and colleagues found that the associations between reports of advice given and corresponding actions taken were as follows: 70.1% reported changing eating habits, 78.7% reported reducing salt, 67.1% reported exercising, and 57.9% reported reducing alcohol consumption.17 They found that when compared with those adults who did not recall receiving advice regarding actions to control HBP, those who did recall receiving advice were more likely to change their eating habits (prevalence ratio [PR] = 1.62; 95% CI 1.56, 1.67), reduce salt intake (PR=1.53; 95% CI 1.48, 1.58), exercise (PR=1.41; 95% CI 1.36, 1.47), and reduce alcohol consumption (PR=1.78; 95% CI 1.70, 1.87). However, data regarding racial/ethnic or rural/urban status were not reported in this study.
Our findings of black rural respondents being more likely than white people to report being advised to take medications for their HBP agree with findings by Mainous and colleagues showing that rural African Americans were more likely than white people to be advised to take medications for HBP.10 Surprisingly, however, Mainous et al. found a 24% discrepancy between the proportion of rural African Americans who were advised to take medications for HBP and those currently taking medications for HBP. In our study, we only found a 6% (90% vs. 96%) discrepancy between the proportion of rural African American respondents currently on medications compared with those who reported being advised to take medications to reduce HBP.
Discrepancies between recommendations to take blood pressure medications and the number of individuals who actually take blood pressure medications in rural settings are of concern and have been attributed to a number of factors, including practice patterns associated with costs. Goldstein et al. noted that because rural clinics see a high percentage of indigent patients, they often resort to a high use of sample agents (medications).18 Because samples are limited to one or two months, patients frequently return for subsequent visits, at which time they may receive an alternate medication when the original medication is not available. Unfortunately, they concluded that in the absence of sample medications, many patients would forgo medications completely as a result of the cost, thereby decreasing their likelihood of achieving adequate blood pressure control.18
Limitations
The findings of this study must be interpreted with some degree of caution for a number of reasons. First, comparisons of racial/ethnic differences between rural and urban settings must give consideration to the complexity, diversity, and evolving nature of the two settings. Wallace and colleagues proposed that although rural settings are traditionally viewed as static, there can be significant ethnic heterogeneity among the residents. Additionally, because of vast differences among rural settings in the U.S., cultural, historic, and economic differences must be considered.19
Telephone surveys such as the BRFSS can yield biased estimates because of exclusion of households without telephones. However, studies have established the validity of the BRFSS telephone survey.20,21 Also, the sample of black rural residents was less than 4%; therefore, we must be concerned with this limited sample relative to the study findings. Furthermore, because this was a cross-sectional study, we were limited in our ability to test for and adequately account for causal relationships between race/ethnicity and residence in our analyses. Lastly, because these findings are all based on self-report, we must be concerned with recall bias and social desirability bias (i.e., overreporting or providing a socially desirable response rather than the most accurate response) regarding current and advised actions to control HBP.16 Despite these limitations, however, this study provides new insights into the relationship effects of race/ethnicity and residential status in actions to control HBP.
CONCLUSIONS
Blood pressure control is a major health concern, and effective management requires good advice from health providers and follow-through on recommended preventive strategies. The findings of this study suggest that race/ethnicity may be more important than residential status; however, additional studies are needed to confirm these findings. Our findings also suggest that at a minimum, health professionals should consider race/ethnicity during the development of strategies for effective blood pressure control. Future prospective studies are needed to determine both the relationship among race/ethnicity, residential status, and HBP control and effective strategies for HBP control for adults residing in rural and urban settings, regardless of race/ethnicity.
Footnotes
This article represents work supported by the use of facilities at the Charleston, South Carolina, Veterans Health Administration Health Services Research and Development (HSR&D)-funded Center for Disease Prevention and Health Interventions for Diverse Populations (REA 08-261). Charles Ellis is supported by Career Development Award (CDA) #07-012-3 from HSR&D. Anouk Grubaugh is supported by CDA2 #07-015-2 from HSR&D.
REFERENCES
- 1.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–23. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 2.Hajjar I, Kotchen JM, Kotchen TA. Hypertension: trends in prevalence, incidence, and control. Annu Rev Public Health. 2006;27:465–90. doi: 10.1146/annurev.publhealth.27.021405.102132. [DOI] [PubMed] [Google Scholar]
- 3.Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ, Comparative Risk Assessment Collaborating Group. Selected major risk factors and global and regional burden of disease. Lancet. 2002;360:1347–60. doi: 10.1016/S0140-6736(02)11403-6. [DOI] [PubMed] [Google Scholar]
- 4.Ostchega Y, Yoon SS, Hughes J, Louis T. NCHS Data Brief. Hyattsville (MD): National Center for Health Statistics (US); 2008. Hypertension awareness, treatment, and control—continued disparities in adults: United States, 2005–2006. [PubMed] [Google Scholar]
- 5.Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, et al. Heart disease and stroke statistics—2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee [published erratum appears in Circulation 2009;119:e182] Circulation. 2009;119:480–6. doi: 10.1161/CIRCULATIONAHA.108.191259. [DOI] [PubMed] [Google Scholar]
- 6.Racial/ethnic disparities in prevalence, treatment, and control of hypertension—United States, 1999–2002 MMWR Morb Mortal Wkly Rep. 2005;54(1):7–9. [PubMed] [Google Scholar]
- 7.Kramer H, Han C, Post W, Goff D, Diez-Roux A, Cooper R, et al. Racial/ethnic differences in hypertension and hypertension treatment and control in the multi-ethnic study of atherosclerosis (MESA) Am J Hypertens. 2004;17:963–70. doi: 10.1016/j.amjhyper.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 8.Hertz RP, Unger AN, Cornell JA, Saunders E. Racial disparities in hypertension prevalence, awareness, and management. Arch Intern Med. 2005;165:2098–104. doi: 10.1001/archinte.165.18.2098. [DOI] [PubMed] [Google Scholar]
- 9.King DE, Crisp JR. Rural-urban differences in factors associated with poor blood pressure control among outpatients. South Med J. 2006;99:1221–3. doi: 10.1097/01.smj.0000223736.99072.22. [DOI] [PubMed] [Google Scholar]
- 10.Mainous AG, III, King DE, Garr DR, Pearson WS. Race, rural residence, and control of diabetes and hypertension. Ann Fam Med. 2004;2:563–8. doi: 10.1370/afm.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention (US). The Behavioral Risk Factor Surveillance System operational and user's guide. Atlanta: Department of Health and Human Services (US); 2007. [Google Scholar]
- 12. StataCorp. Stata®: Version 10.0 for Windows. College Station (TX): StataCorp.; 2004. [Google Scholar]
- 13.Bosworth HB, Dudley T, Olsen MK, Voils CI, Powers B, Goldstein MK, et al. Racial differences in blood pressure control: potential explanatory factors. Am J Med. 2006;119:70. doi: 10.1016/j.amjmed.2005.08.019. [DOI] [PubMed] [Google Scholar]
- 14.National Heart, Lung, and Blood Institute (US) The seventh report of the Joint National Committee on Prevention, Detection, Evaluation,and Treatment of High Blood Pressure. Rockville (MD): Department of Health and Human Services (US); 2003. NIH Publication No. 03-5233. [PubMed] [Google Scholar]
- 15.Prevalence of actions to control high blood pressure—20 states,2005. MMWR Morb Mortal Wkly Rep. 2007;56(17):420–3. [PubMed] [Google Scholar]
- 16.Ayala C, Neff LJ, Croft JB, Keenan NL, Malarcher AM, Hyduk A, et al. Prevalence of self-reported high blood pressure awareness, advice received from health professionals, and actions taken to reduce high blood pressure among US adults—Healthstyles 2002. J Clin Hypertens (Greenwich) 2005;7:513–9. doi: 10.1111/j.1524-6175.2005.04286.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Viera AJ, Kshirsagar AV, Hinderliter AL. Lifestyle modifications to lower or control high blood pressure: is advice associated with action?The Behavioral Risk Factor Surveillance Survey. J Clin Hypertens (Greenwich) 2008;10:105–11. doi: 10.1111/j.1751-7176.2008.07577.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goldstein AO, Carey TS, Levis D, Madson S, Bernstein J. Variations in hypertension control in indigent rural primary care clinics in North Carolina. Arch Fam Med. 1994;3:514–9. doi: 10.1001/archfami.3.6.514. [DOI] [PubMed] [Google Scholar]
- 19.Wallace RB, Grindeanu LA, Cirillo DJ. Rural/urban contrasts in population morbidity status. In: Wright L, Johnson NE, Glasgow N, editors. Critical issues in rural health. Danvers (MA): Blackwell Publishing; 2004. pp. 15–26. [Google Scholar]
- 20.Bowlin SJ, Morrill BD, Nafziger AN, Lewis C, Pearson TA. Reliability and changes in validity of self-reported cardiovascular disease risk factors using dual response: the Behavioral Risk Factor Survey. J Clin Epidemiol. 1996;49:511–7. doi: 10.1016/0895-4356(96)00010-8. [DOI] [PubMed] [Google Scholar]
- 21.Shea S, Stein AD, Lantigua R, Basch CE. Reliability of the Behavioral Risk Factor Survey in a triethnic population. Am J Epidemiol. 1991;133:489–500. doi: 10.1093/oxfordjournals.aje.a115916. [DOI] [PubMed] [Google Scholar]