SYNOPSIS
Objective
We investigated the association between a cumulative biological risk or allostatic score and all-cause mortality risk. We used 13,715 records of participants aged 25 years and older from the Third National Health and Nutrition Examination Survey (NHANES III) linked to the National Death Index.
Methods
We specified all-cause mortality using the underlying cause of death in the death certificate. We calculated time to death from interview date through December 31, 2000, as person-years of follow-up using the NHANES III interview month and year. We used Cox proportional hazards regression to estimate hazard ratios (HRs) relating all-cause mortality risk for those with an allostatic score of 2 and ≥3 relative to those with an allostatic score of ≤1.
Results
After controlling for age, gender, race/ethnicity, education, and income, mortality rates were 40% (HR=1.40, 95% confidence interval [CI] 1.11, 1.76) and 88% (HR=1.88, 95% CI 1.56, 2.26) higher for participants with an allostatic score of 2 and ≥3, respectively, compared with those with a score of ≤1. The death rate associated with allostatic score for each racial/ethnic group differed with age.
Conclusions
The allostatic score increased the risk of all-cause mortality. Moreover, this increased risk was observed for adults younger than 65 years of age regardless of their race/ethnicity. Thus, allostatic score may be a contributor to premature death in the U.S.
The black/white mortality gap has been pervasive in the United States since quality data have been collected (i.e., 1960).1,2 In fact, the most recent mortality data suggest that non-Hispanic black people have a higher age-adjusted all-cause death rate than non-Hispanic white people.3 The higher mortality rate among non-Hispanic black people has been attributed in part to their long-lasting exposure to socioeconomic disadvantage and sociopolitical exclusion,4 including racism and/or discrimination.5 However, the pattern observed among non-Hispanic black people does not hold for the Hispanic population, the largest minority group in the U.S.6,7 Hispanic people exhibited an age-adjusted all-cause death rate that was lower (564.0 per 100,000 population) than both non-Hispanic black people (1,001.4 per 100,000 population) and non-Hispanic white people (777.0 per 100,000 population),3 despite the fact that Hispanic people have lower socioeconomic position and access to care than non-Hispanic individuals.8
The cumulative exposure to socioeconomic disadvantage and racism/discrimination could have detrimental effects on health that may lead to premature death (i.e., death for those younger than 65 years of age). This cumulative effect may influence allostatic load, which is defined as the cumulative effect of physiological instability across systems from repeated adaptation to stressors.9,10 This, in turn, may disturb the release of certain biomarker substances in the body (i.e., epinephrine, dehydroepiandrosterone sulfate, and cortisol). These hormones may cause increases in blood pressure, cholesterol levels, glycated hemoglobin, C-reactive protein, and waist-hip ratio, among other health indicators.10,11
Because of the multiple systems affected, previous studies have operationalized an allostatic load score using a sum of selected indicators and have found that a higher score is associated with increased mortality12,13 and older age.14,15 In addition, evidence suggests that non-Hispanic black people not only exhibit a higher allostatic load than non-Hispanic white people, but also mean allostatic load for non-Hispanic black people in each age group is similar to non-Hispanic white people who were 10 years older.15 Consistent with the weathering hypothesis,4 which posits that the health of non-Hispanic black people prematurely deteriorates due to racial inequalities, it is possible that the association between allostatic load and all-cause mortality differs with race/ethnicity and age. Specifically, this association may be stronger for younger non-Hispanic black individuals and possibly Mexican American people than for their non-Hispanic white counterparts.
The release of the Third National Health and Nutrition Examination Survey (NHANES III) linked to the National Death Index data in 2007 affords the unique opportunity to investigate whether (1) there is an association between a cumulative index of biological system deregulation score and all-cause mortality after controlling for selected characteristics including education and income, (2) this association differs by race/ethnicity, and (3) this association differs by race/ethnicity and age simultaneously. Specifically, we hypothesized that mortality risk associated with the cumulative index would be stronger for non-Hispanic black people followed by Mexican American people, relative to the white majority population, and that the racial/ethnic-specific associations would be stronger at younger ages for non-Hispanic black people and Mexican American people than for non-Hispanic white people.
METHODS
NHANES III assessed the health status of a nationally representative sample of the civilian noninstitutionalized U.S. population, selected through a stratified multistage probability sampling design. Full descriptions of the sample design in NHANES III have been reported elsewhere.16 For this analysis, we used NHANES III publicly available datasets (household, adult, examination, and laboratory files) linked to death certificate data from the 2007 National Death Index public release.17 To link these two datasets, the National Center for Health Statistics used a probabilistic matching algorithm based on the following items of identification: social security number, first name, middle initial, last name or surname, date of birth, gender, state of birth, race, state of residence, and marital status. Complete information on the linked dataset can be found at the Centers for Disease Control and Prevention's website.18
The linkage of these datasets resulted in a sample size of 33,994. The following records were excluded from this sample because they were younger than 17 years of age and, thus, ineligible for mortality follow-up (n=13,970); were younger than 25 years of age at the time of the interview (n=3,165); had a sampling weight of zero (n=1,652); were participants responding “other” race (n=587); did not report an education level (n=100); had a follow-up of less than one month (n=3); did not have an underlying cause of death (COD) (n=2); and had records missing for at least five of the individual components of the allostatic score (n=800). These exclusions yielded a final sample of 13,715, including 2,491 deaths and more than approximately 114,755.2 person-years (median = 8.7 years, range: 0.1 to 12.2 years).
All-cause mortality, the outcome, was specified using the underlying COD according to the International Classification of Diseases, Ninth and Tenth Revisions. We calculated time to death from interview date through December 31, 2000, as months of follow-up using the NHANES III interview month and year to the month and year of death for participants who died; and from NHANES III interview month and year to December 31, 2000, for participants assumed to be alive.19 The follow-up time was transformed to years by dividing months by 12.
Our main independent variable was a cumulative biological risk profile of system deregulation or allostatic load.20,21 Consistent with previous studies,22,23 the cumulative biological risk profile included nine health conditions using the following cut points to represent risk for each condition: albumin <3.8 milligrams/deciliter (mg/dl), C-reactive protein ≥0.3 mg/dl, total cholesterol ≥240 mg/dl, high-density lipoprotein <40 mg/dl, hemoglobin A1C ≥6.4%, male waist-to-hip ratio >0.90/female waist-to-hip ratio >0.85, systolic blood pressure ≥140 millimeters of mercury (mmHg), diastolic blood pressure ≥90 mmHg, and pulse rate ≥90 beats/minute. These biomarkers are associated with the organs and tissues affected by allostatic load, cardiovascular disease and atherosclerosis (systolic blood pressure, diastolic blood pressure, triglycerides, protein, homocysteine, and total cholesterol), the metabolic system (body mass index and glycated hemoglobin), inflammation (C-reactive protein and albumin), and the immune system (creatinine clearance).9–11,13,22
Individuals with a factor in the risk range were considered at risk and were assigned a value of 1, while those below these values were assigned a value of 0. We defined the allostatic load score by summing the values corresponding to each risk factor ranging from 0 to 9. Based on tertiles in the total population, we categorized the allostatic load score as ≤1, 2, and ≥3. This allostatic load score distribution was the same for each racial/ethnic group. Although each biomarker may not contribute equally to the allostatic load score, evidence suggests that an equally weighted algorithm may provide a conservative estimate of the true effect of allostatic load on health outcomes.13
We included demographic and socioeconomic variables as covariates. We included age in the analysis as categorical (25–44, 45–64, or ≥65 years of age). Gender was included as collected by NHANES (male/female). Race/ethnicity was included as collected in the survey and was limited to non-Hispanic white, non-Hispanic black, and Mexican American (hereafter, non-Hispanic black and non-Hispanic white will be referred to as black and white, respectively). Education level was recorded as a continuous variable from 0 to 17 years and categorized as less than a high school diploma/general equivalency diploma (GED), high school diploma/GED, and more than a high school diploma/GED. Total family 12-month income during the past year was recorded as continuous and further categorized as ≤$14,999, $15,000−$24,999, and ≥$25,000.
Statistical analysis
Selected characteristics of the population were presented by death status and the total population. To determine significant associations and differences, we used Chi-square statistics of independence and t-tests according to the nature of the variable.
We used Cox proportional hazards regression to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) relating all-cause mortality risk for NHANES III participants with an allostatic load score of 2 and ≥3 to those with an allostatic load score of ≤1 before and after controlling for selected characteristics. Specifically, in addition to the crude association (crude HR), we performed two sets of analyses: (1) HR adjusted for age, gender, and race/ethnicity (Model 1); and (2) HR additionally adjusted for education and income (Model 2). To determine whether this association differed by race/ethnicity, we tested an interaction term between race/ethnicity and the allostatic load score in the fully adjusted model. Moreover, to determine whether the association between allostatic load score and mortality risk differed by race/ethnicity and age simultaneously, we tested interaction terms between age and allostatic load score; between age and race/ethnicity; and among age, race/ethnicity, and allostatic load score. Lastly, because evidence suggests that allostatic load may be associated with socioeconomic position indicators,22,24 we tested interaction terms between education and allostatic load score and between income and allostatic load score.
We conducted all data management procedures using SAS®.25 We conducted statistical analyses using SUDAAN®26 because of its ability to take into account the complex sampling design in calculating unbiased standard error estimates. Sample sizes presented in Table 1 were unweighted, but all other estimates (e.g., proportions, means, standard errors, and HRs with their 95% CIs) were weighted.
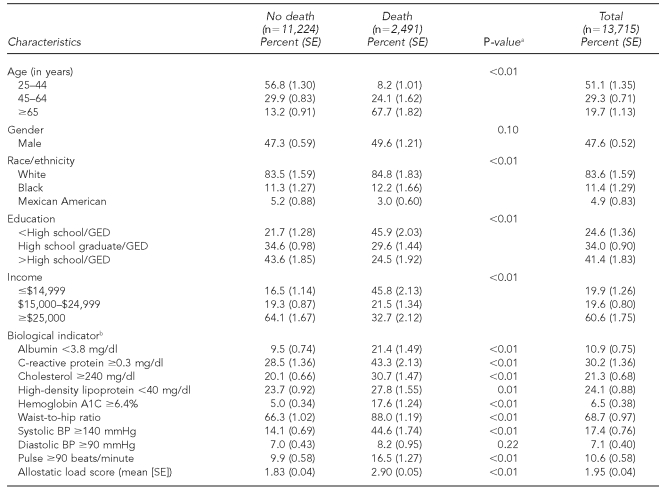
Table 1.
Distribution of selected sociodemographic and health-related characteristics stratified by mortality status among adults aged >25 years, NHANES III linked mortality file
aP-values for Chi-square for proportions and t-tests for mean comparisons
bProportions represent those with values equal or above the ones next to each indicator. For waist-to-hip ratio, the values were >0.90 for male and >0.85 for female
NHANES = National Health and Nutrition Examination Survey
SE = standard error
GED = general equivalency diploma
mg/dl = milligrams per deciliter
BP = blood pressure
mmHg = millimeters of mercury
RESULTS
Table 1 presents the distribution of selected characteristics for NHANES III participants according to death status and for the overall population. Compared with participants who did not die, those who died were more likely to be older, have less than a high school diploma/GED, be in the lower category of poverty-income ratio, or report an income of less than $15,000, and less likely to be Mexican American. With the exception of diastolic blood pressure, respondents who died were more likely to be above the cut points for the biomarkers included in the score (all p≤0.01). The mean allostatic load score was significantly higher for those who died (2.90) than for those who did not die (1.83, p<0.01). Compared with those with an allostatic load score of ≤1 who were younger and less educated, those with an allostatic load score ≥3 were similarly distributed across age and education categories (data not shown).
The death rates for NHANES III participants with an allostatic load score of 2 and ≥3 were 2.55 (95% CI 2.10, 3.10) and 5.29 (95% CI 4.52, 6.20) times greater than participants with an allostatic load score of ≤1 (Table 2), respectively. After controlling for age, gender, race/ethnicity, education, and income, mortality rates were 40% (HR=1.40, 95% CI 1.11, 1.76) and 88% (HR=1.88, 95% CI 1.56, 2.26) higher for participants with an allostatic load score of 2 and ≥3, respectively, compared with those with a score of ≤1.
Table 2.
Crude and adjusted hazard ratiosa of all-cause mortality risk for allostatic load score, NHANES III linked mortality file
aCrude HR for allostatic load score, Model 1 (age, gender, and race/ethnicity), and Model 2 (age, gender, race/ethnicity, education, and income)
NHANES = National Health and Nutrition Examination Survey
HR = hazard ratio
CI = confidence interval
There was no interaction between race/ethnicity and allostatic load score (p=0.28). However, there were interactions between age groups and allostatic load score (p=0.01) and age groups and race/ethnicity (p=0.001). The latter resulted in examination of a three-way interaction among age groups, race/ethnicity, and allostatic load score (p=0.01). Table 3 shows the adjusted HRs and 95% CIs for the association between allostatic load score and all-cause mortality for each racial/ethnic group stratified by age. For white people aged 25–44 years with an allostatic load score of ≥3, the death rate increased by 205% (HR=3.05, 95% CI 1.38, 6.71) relative to their counterparts with an allostatic load score of ≤1. Although lower than the rate of white people, black people with an allostatic load score of ≥3 had a 147% (HR=2.47, 95% CI 1.33, 4.58) increased rate of death compared with black people with a score of ≤1.
Table 3.
Adjusted hazard ratiosa of all-cause mortality risk for allostatic load score for racial/ethnic groups according to age, NHANES III linked mortality file
aAdjusted for gender, education, and income
NHANES = National Health and Nutrition Examination Survey
HR = hazard ratio
CI = confidence interval
Among white and black people aged 45–64 years, we only observed an increased rate of death for those with an allostatic load score of ≥3 (HR=2.83, 95% CI 1.85, 4.32 and HR=2.24, 95% CI 1.38, 3.63, respectively). However, Mexican American people with an allostatic load score of 2 or ≥3 showed a threefold increase in death rates. Finally, for those aged ≥65 years, only white people with an allostatic load score of ≥3 exhibited a 48% (HR=1.48, 95% CI 1.17, 1.86) increase in death rate compared with their peers with a score of ≤1. We observed no interaction between education and allostatic load score tertile nor between income and allostatic load score tertile.
Discussion
Our results suggest that allostatic load score increases the death rate among U.S. adults aged 25 years and older regardless of race/ethnicity, income, and education. Moreover, the death rate for each racial/ethnic group differed with age. For white and black people aged 25–44 years with an allostatic load score of ≥3, there was an increased risk of dying. For individuals 45–64 years of age, the death rate was at least 2.2 times higher for those with an allostatic load score of ≥3 relative to those with a score of ≤1 regardless of their race/ethnicity. It is worth noting that Mexican American people aged 45–64 years with an allostatic load score of 2 exhibited at least a threefold increase of dying relative to their peers with a score of ≤1. Finally, there was an increased death rate for white people aged ≥65 years only.
Previous studies have shown that allostatic load score has been associated with all-cause mortality.12,13 These studies found that among adults aged 70–79 years, an allostatic load score of ≥5 was associated with at least a twofold increase in mortality after controlling for age, gender, ethnicity, and education.12 Using the same data with 4.5 years of follow-up, Karlamangla and colleagues found that baseline allostatic load score and changes in baseline score at 2.5 years were associated with 4.6 and 3.3 greater odds of dying, respectively, after adjusting for age, gender, ethnicity, prevalent cardiovascular disease, and cancer, as well as other chronic diseases.13 Consistent with these studies, our results show that allostatic load score was associated with an increased rate of dying ranging from 40%–88% for those with an allostatic load score of 2 and ≥3, respectively, among U.S. adults ≥25 years of age after controlling for age, gender, race/ethnicity, education, and income after 8.7 years of follow-up.
We propose two main reasons why our associations were weaker than those of previous studies.12,13 First, these studies included an older population (70–79 years of age) than our study, where the conditions included in the score are more common. Second, previous studies used odds ratios as the measures of association while our study used HRs. It is possible that the use of odds ratios has overestimated the true association between allostatic load score and all-cause mortality risk.
Although we found weaker associations than previous studies, our findings of an increased death rate in a younger population suggest that allostatic load is an important contributor to mortality in this population and at least 28.6% and 46.8% of deaths with an allostatic load score of 2 and ≥3, respectively, could be attributed to allostatic load (attributable rate percent = [(HR-1)/HR] *100).
Evidence suggests that non-Hispanic black people <65 years of age exhibited higher death rates than non-Hispanic white people.2,3,27–32 Consistent with this finding, although Hispanic people exhibited similar or lower death rates than non-Hispanic white people,31,33–35 higher death rates have been reported for younger Hispanic people.30,34,35 These findings have been observed regardless of gender. Although we did not find evidence of racial/ethnic variation on the association between allostatic load score and all-cause mortality, our study found that the effect of allostatic load score on all-cause mortality depends jointly on race/ethnicity and age. Specifically, non-Hispanic black and white people <65 years of age with an allostatic load score of ≥3 exhibited higher rates of dying than their counterparts with an allostatic load score of ≤1. Higher rates of death were observed for Mexican American people aged 45–64 years with an allostatic load score of ≥2, while for those aged ≥65 years, only non-Hispanic white people with an allostatic load score of ≥3 exhibited higher death rates. Although these findings suggest that allostatic load score increases the risk of dying regardless of racial/ethnic groups, there are age variations within racial/ethnic groups resulting in an increased rate of premature death for all racial/ethnic groups.
Strengths and limitations
One of the strengths of this study was the use of a nationally representative sample of the two major racial/ethnic groups, non-Hispanic black and white people, and the largest Hispanic subgroup, Mexican American people. Other strengths included the large sample size, which allowed us to control for selected covariates and examine effect measure modification; and the inclusion of biomarkers, which are critical for calculating the allostatic load score.
Important limitations included the use of the public-use version of the NHANES III-linked mortality files. The NHANES III-linked mortality public-use files include limited mortality information compared with the restricted-use files and have small perturbations for a small, selected number of records. However, a comparative analysis of the NHANES III public- and restricted-use linked mortality files conducted by the National Center for Health Statistics suggests that the results obtained from these two datasets were very similar for all-cause and selected cause-specific mortality.19 Thus, it is very unlikely that the public-use files of the NHANES III-linked mortality files affected our study results. Finally, individuals who agreed to participate in NHANES III may be different from those who chose not to participate. However, this refusal may have under- or overestimated our results toward the null depending on whether the decision to participate was based on race/ethnicity.
CONCLUSIONS
Our findings suggest that allostatic load increases the risk of all-cause mortality. Our study demonstrates that younger black, Mexican American, and white people exhibited higher mortality rates with increasing allostatic load scores. However, while it is possible that individuals <65 years of age may be more vulnerable to the effect of the conditions included in the allostatic load than their ≥65 years of age counterparts regardless of their race/ethnicity, the lack of an association for black and Mexican American people aged ≥65 years may represent a survival effect. These findings suggest that allostatic load may be a stronger contributor to premature death in the U.S. regardless of race/ethnicity. Further studies examining the effect of the allostatic load score on specific CODs should be conducted to determine whether there are racial/ethnic and age differences that may contribute to the higher mortality rates observed in black people.
References
- 1.Department of Health and Human Services (US). Report of the Secretary's Task Force on Black and Minority Health. Washington: U.S. Government Printing Office; 1985. [Google Scholar]
- 2.Satcher D, Fryer GE, Jr, McCann J, Troutman A, Woolf SH, Rust G. What if we were equal? A comparison of the black-white mortality gap in 1960 and 2000. Health Aff (Millwood) 2005;24:459–64. doi: 10.1377/hlthaff.24.2.459. [DOI] [PubMed] [Google Scholar]
- 3.Heron M, Hoyert DL, Murphy SL, Xu J, Kochanek KD, Tejada-Vera B. Deaths: final data for 2006. Natl Vital Stat Rep. 2009 Apr 17;57:1–134. [PubMed] [Google Scholar]
- 4.Geronimus AT. The weathering hypothesis and the health of African-American women and infants: evidence and speculations. Ethn Dis. 1992;2:207–21. [PubMed] [Google Scholar]
- 5.Williams DR. Race, socioeconomic status, and health. The added effects of racism and discrimination. Ann N Y Acad Sci. 1999;896:173–88. doi: 10.1111/j.1749-6632.1999.tb08114.x. [DOI] [PubMed] [Google Scholar]
- 6.Grieco EM, Cassidy RC. Overview of race and Hispanic origin. Washington: Census Bureau (US); 2000. [Google Scholar]
- 7.Guzman B. The Hispanic population. Washington: Census Bureau (US); 2001. [Google Scholar]
- 8.Markides KS, Coreil J. The health of Hispanics in the southwestern United States: an epidemiologic paradox. Public Health Rep. 1986;101:253–65. [PMC free article] [PubMed] [Google Scholar]
- 9.McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338:171–9. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- 10.McEwen BS, Seeman T. Protective and damaging effects of mediators of stress. Elaborating and testing the concepts of allostasis and allostatic load. Ann N Y Acad Sci. 1999;896:30–47. doi: 10.1111/j.1749-6632.1999.tb08103.x. [DOI] [PubMed] [Google Scholar]
- 11.Seeman TE, Singer BH, Rowe JW, Horwitz RI, McEwen BS. Price of adaptation—allostatic load and its health consequences. MacArthur studies of successful aging. Arch Intern Med. 1997;157:2259–68. [PubMed] [Google Scholar]
- 12.Seeman TE, Crimmins E, Huang MH, Singer B, Bucur A, Gruenewald T, et al. Cumulative biological risk and socio-economic differences in mortality: MacArthur studies of successful aging. Soc Sci Med. 2004;58:1985–97. doi: 10.1016/S0277-9536(03)00402-7. [DOI] [PubMed] [Google Scholar]
- 13.Karlamangla AS, Singer BH, Seeman TE. Reduction in allostatic load in older adults is associated with lower all-cause mortality risk: MacArthur studies of successful aging. Psychosom Med. 2006;68:500–7. doi: 10.1097/01.psy.0000221270.93985.82. [DOI] [PubMed] [Google Scholar]
- 14.Crimmins EM, Johnston M, Hayward M, Seeman T. Age differences in allostatic load: an index of physiological dysregulation. Exp Gerontol. 2003;38:731–4. doi: 10.1016/s0531-5565(03)00099-8. [DOI] [PubMed] [Google Scholar]
- 15.Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. Am J Public Health. 2006;96:826–33. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Plan and operation of the Third National Health and Nutrition Examination Survey, 1988–1994. Vital Health Stat. 1994;1(32):1–407. [PubMed] [Google Scholar]
- 17.National Center for Health Statistics (US) NHANES III linked mortality file. [cited 2010 Jun 30]. Available from: URL: http://www.cdc.gov/nchs/data_access/data_linkage/mortality/nhanes3_linkage.htm.
- 18.National Center for Health Statistics (US) Hyattsville (MD): NCHS; 2009. [cited 2009 Apr 13]. The Third National Health and Nutrition Examination Survey (NHANES III) linked mortality file: mortality follow-up through 2006: matching methodology. Also available from: URL: http://www.cdc.gov/nchs/data/datalinkage/matching_methodology_nhanes3_final.pdf. [Google Scholar]
- 19.Data Linkage Team. Hyattsville (MD): National Center for Health Statistics (US); 2010. [cited 2010 Jun 30]. Comparative analysis of the NHANES III public-use and restricted-use linked mortality files: 2010 data release. Available from: URL: http://www.cdc.gov/NCHS/data/datalinkage/NH3_mort_compare_2010_final.pdf. [Google Scholar]
- 20.McEwen BS, Stellar E. Stress and the individual. Mechanisms leading to disease. Arch Intern Med. 1993;153:2093–101. [PubMed] [Google Scholar]
- 21.McEwen BS. Stress, adaptation, and disease. Allostasis and allostatic load. Ann N Y Acad Sci. 1998;840:33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- 22.Seeman T, Merkin SS, Crimmins E, Koretz B, Charette S, Karlamangla A. Education, income and ethnic differences in cumulative biological risk profiles in a national sample of US adults: NHANES III (1988–1994) Soc Sci Med. 2008;66:72–87. doi: 10.1016/j.socscimed.2007.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Merkin SS, Basurto-Davila R, Karlamangla A, Bird CE, Lurie N, Escarce J, et al. Neighborhoods and cumulative biological risk profiles by race/ethnicity in a national sample of U.S. adults: NHANES III. Ann Epidemiol. 2009;19:194–201. doi: 10.1016/j.annepidem.2008.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kubzansky LD, Kawachi I, Sparrow D. Socioeconomic status, hostility, and risk factor clustering in the Normative Aging Study: any help from the concept of allostatic load? Ann Behav Med. 1999;21:330–8. doi: 10.1007/BF02895966. [DOI] [PubMed] [Google Scholar]
- 25. SAS Institute, Inc. SAS®: Version 9.2. Cary (NC): SAS Institute, Inc; 2009.
- 26.Research Triangle Institute. SUDAAN®: Release 10.0. Research Triangle Park (NC): Research Triangle Institute; 2008. [Google Scholar]
- 27.McCord C, Freeman HP. Excess mortality in Harlem. N Engl J Med. 1990;322:173–7. doi: 10.1056/NEJM199001183220306. [DOI] [PubMed] [Google Scholar]
- 28.Sorlie PD, Backlund E, Keller JB. US mortality by economic, demographic, and social characteristics: the National Longitudinal Mortality Study. Am J Public Health. 1995;85:949–56. doi: 10.2105/ajph.85.7.949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Geronimus AT, Bound J, Waidmann TA, Hillemeier MM, Burns PB. Excess mortality among blacks and whites in the United States. N Engl J Med. 1996;335:1552–8. doi: 10.1056/NEJM199611213352102. [DOI] [PubMed] [Google Scholar]
- 30.Liao Y, Cooper RS, Cao G, Durazo-Arvizu R, Kaufman JS, Luke A, et al. Mortality patterns among adult Hispanics: findings from the NHIS, 1986 to 1990. Am J Public Health. 1998;88:227–32. doi: 10.2105/ajph.88.2.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.National Center for Health Statistics (US) Health, United States, 2008: with chartbook on trends in the health of Americans, with special feature on the health of young adults. Hyattsville (MD): NCHS; 2009. [PubMed] [Google Scholar]
- 32.Hadden WC, Rockswold PD. Increasing differential mortality by educational attainment in adults in the United States. Int J Health Serv. 2008;38:47–61. doi: 10.2190/HS.38.1.c. [DOI] [PubMed] [Google Scholar]
- 33.Sorlie PD, Backlund E, Johnson NJ, Rogot E. Mortality by Hispanic status in the United States. JAMA. 1993;270:2464–8. [PubMed] [Google Scholar]
- 34.Hummer RA, Rogers RG, Nam CB, LeClere FB. Race/ethnicity, nativity, and US adult mortality. Soc Sci Q. 1999;80:136–53. [Google Scholar]
- 35.Hummer RA. Adult mortality differentials among Hispanic subgroups and non-Hispanic whites. Soc Sci Q. 2000;81:459–76. [PubMed] [Google Scholar]