SYNOPSIS
Objectives
The National Asthma Survey—New York State (NYS), a telephone survey of NYS residents, was conducted in 2002–2003 to further understand the burden of asthma among adults and children and to identify health, socioeconomic, behavioral, and environmental factors associated with asthma.
Methods
A total of 1,412 households with at least one member with current asthma and 2,290 control households answered questions about their home environment (e.g., presence of asthma triggers and practices that promote or reduce common asthma triggers).
Results
For children younger than 18 years of age, we found statistically significant positive associations between current asthma and the presence of mold (adjusted odds ratio [AOR] = 2.1, 95% confidence interval [CI] 1.3, 3.3), air cleaners (AOR=1.5, 95% CI 1.1, 2.1), dehumidifiers (AOR=2.0, 95% CI 1.4, 2.7), and humidifiers (AOR=1.6, 95% CI 1.1, 2.3). For adults, there were statistically significant positive associations with the presence of mold (AOR=2.5, 95% CI 1.8, 3.4), air cleaners (AOR=2.2, 95% CI 1.7, 2.8), and humidifiers (AOR=1.4, 95% CI 1.1, 1.8). There were no statistically significant associations with the presence of cockroaches, pets, or tobacco smoke, while use of a wood-burning stove or fireplace was significantly more prevalent in control homes.
Conclusions
Asthma guidelines emphasize the importance of reducing triggers in the home as part of a multifaceted approach to asthma control. Despite these guidelines, many asthma triggers (specifically, mold) were as prevalent or more so in the homes of New Yorkers with asthma as compared with control households. Public health interventions in NYS should focus on educating households about potential asthma triggers and their sources and teach methods to prevent, reduce, or eliminate them.
The Expert Panel Report 3 (EPR-3) Full Report 2007—Guidelines for the Diagnosis and Management of Asthma—underscores the continued impact of asthma on the health and quality of life of Americans and the economy of the United States.1 In addition, it emphasizes the importance of collecting high-quality data to support progress toward national asthma-control goals. During 2001–2003, annual estimates from the National Health Interview Survey indicated that 20 million American adults and children (7.2% of the population) had asthma. The continued impact of asthma is also evident in the number of people who reported at least one asthma attack during the past year (11.6 million) and the number of emergency department visits (1.8 million), in-patient hospitalizations (504,000), and deaths (4,200) due to asthma each year.2 Loss of productivity due to asthma was estimated at more than 10.1 million work days per year for adults and 12.8 million school days for children.3 In New York State (NYS), 1.1 million adults (7.6%) and 370,000 children (8.4%) were estimated to have asthma in 2005.4
The EPR-3 states that for an individual, the ultimate goal of asthma therapy is control, defined as reducing impairment and risk through four critical components of care: (1) assessment and monitoring, (2) patient education that supports a patient-clinician partnership, (3) control of environmental factors and comorbid conditions, and (4) medications.1 The guidelines also emphasize the importance of controlling asthma-related environmental conditions for patients, regardless of the severity of their asthma. In NYS, comprehensive asthma interventions have been implemented throughout the state, and surveillance efforts continue to monitor intervention progress as well as some of the EPR-3 components. However, because existing large-scale surveys already include questions on many diseases and other risk factors, it is difficult to add more questions for disease-specific environmental conditions and related modifications (i.e., asthma-related environmental factors). Consequently, many studies have assessed the relationship between asthma and the environment by studying specific geographic areas or demographic groups or by focusing on exacerbation of asthma symptoms rather than the presence or absence of disease.
Many of these studies focus only on households with members who have asthma and/or live in urban or low-income areas with a high burden of asthma. However, evidence from a nationally representative sample that included homes of people with and without asthma suggests that some important asthma triggers (e.g., mouse and dust mite allergens) were more common in homes of people with asthma.5,6 Allergen levels in these studies were directly assessed from the analysis of settled dust, but dust sampling is not a practical or feasible method for most large-scale surveys. On the other hand, Wilson and colleagues found that certain allergens measured in dust were associated with observable housing conditions (e.g., cracks in walls and moldy odors). This study suggests that questionnaires and screening tools, which may be critical to the ongoing surveillance of environmental asthma triggers, could be useful in assessing the presence of asthma triggers within a home.7
Statewide and national asthma surveillance generates a wealth of information that is an invaluable tool for the public health and medical communities working to address the problem of asthma. In 2002–2003, the NYS Department of Health, sponsored by the Centers for Disease Control and Prevention, conducted the National Asthma Survey—New York State (NAS-NYS), a random-digit-dialing (RDD) telephone survey of NYS residents.8 The purpose of the NAS-NYS was to further understand the burden of asthma among adults and children and to describe and identify the health, socioeconomic, behavioral, and environmental factors that are associated with asthma.
In an attempt to overcome some of the challenges described previously, this survey included questions about the home environment of participants with asthma and a random subset of participants without asthma. These questions inquired about the presence of asthma triggers (e.g., mold and cigarette smoking) and asthma-related environmental modifications (e.g., the use of air cleaners, humidifiers, and dehumidifiers). We characterized the home environmental conditions and modifications that are related to current asthma among NYS residents.
METHODS
Study design
For this study, we used a nested case-control design within the cross-sectional NAS-NYS and conducted separate analyses for children and adults. The NAS-NYS followed the State and Local Area Integrated Telephone Survey methodology using the same sampling frame as the National Immunization Survey (NIS).9 The NIS uses an RDD telephone survey method to select a random sample of telephone numbers (households) from landline phone banks for the general population. The NAS questionnaire was designed to immediately follow a completed NIS interview. This questionnaire was designed by the National Center for Environmental Health and was further refined based on cognitive testing and results from a series of four pretests.10 Subsequently, the NAS questionnaire was used for a national sample and several state-specific samples, including NYS.
At the beginning of the NAS-NYS interview, one adult participant was asked two screening questions about each household member to determine who, if anyone, had asthma: (1) “Have you (has he/she) ever been told by a doctor or other health professional that you have asthma?” (2) “Do you (does he/she) still have asthma?” A positive response to both questions classified an individual as having current asthma. A positive response to the first question and a negative response to the second question classified an individual as having lifetime asthma only. A negative response to the first question categorized an individual as not having asthma. For individuals with asthma, the NAS questionnaire collected information about asthma symptoms, asthma attacks, asthma medication usage, health-care utilization, missed school and work days due to asthma, quality of life, and knowledge of asthma management. Households with and without individuals with asthma were asked questions about individual- and household-level demographics and home environment conditions.
Selection of cases
In households with only one child with current asthma, that child was selected as the asthma case. In households with more than one child with current asthma, one child was randomly selected as the asthma case. In households with only one adult with current asthma, that adult was selected as the asthma case. In households with more than one adult with current asthma, one adult was randomly selected as the asthma case. Households could contribute one adult and one child to the analysis.
Selection of controls
The NAS study design used by other states did not collect information about home environment conditions from households that had no individuals with current or lifetime asthma (i.e., control households). However, NYS chose to randomly survey a subset of control households to compare home environment conditions among cases and controls. For the child analysis, one control child was randomly selected from the children in these households. Similarly, for the adult analysis, one control adult was randomly selected from these households. Control households were only asked about individual- and household-level demographic information and home environment conditions.
Independent variables
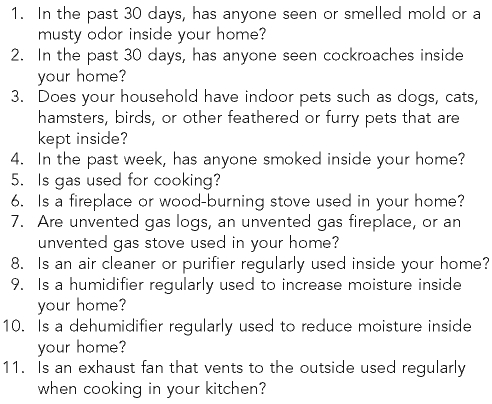
The survey included two groups of environmental questions that were asked of both cases and controls (Figure). The first group assessed environmental triggers potentially related to asthma: presence or absence of mold, cockroaches, indoor pets, and environmental tobacco smoke (ETS) in the home. The second group of questions assessed actions or behaviors that can mitigate and/or exacerbate exposure to triggers in the home environment: use of gas for cooking, wood-burning stoves or fireplaces, unvented stoves or fireplaces, air cleaners or purifiers, humidifiers, dehumidifiers, and kitchen exhaust fans. However, only cases were asked about environmental modifications relating to the use and care of mattress and pillow covers for controlling dust mites and the presence of wall-to-wall carpeting. Therefore, these questions were not included in this analysis.
Figure.
Questions from the 2003 National Asthma Survey—New York State, section 7: modifications to the environment
Demographic information for the surveyed households and each household member was obtained during the interview. At the individual level, we collected age, gender, race/ethnicity, and educational attainment. At the household level, we collected income, residential zip code, and location (New York City or the rest of the state). Children were grouped into four age categories (0–4, 5–9, 10–14, and 15–17 years of age), and adults were grouped into four age categories (18–24, 25–44, 45–64, and ≥65 years of age). Race categories consisted of white, black, Asian, and other races. We aggregated American Indian/Alaska Native and Native Hawaiian/Pacific Islander into the other race category because of the small number of participants in these groups. Ethnicity consisted of Hispanic and non-Hispanic minority groups.
Educational attainment was grouped into less than a high school degree, high school degree, and more than a high school degree. For the child case-control analysis, we used the highest level of educational attainment reported among the adults in the household. To assess poverty, we established household poverty levels based on the combined household income information and the U.S. Census Bureau 2003 federal poverty thresholds.11 To compute the percent of the poverty threshold, we divided the household income by the federal poverty level (FPL) for each family size category. Households were classified into three groups: <100% FPL, 100% to <200% FPL, and ≥200% FPL. Finally, we used the residential zip code to stratify households into categories based on the four tiers of the rural urban commuting area system: urban core areas, suburban areas, large town areas, and small town/isolated rural areas.12
Statistical analysis
We performed statistical analyses using SAS® version 9.1.13 We conducted two analyses: one for children (<18 years of age) and one for adults (≥18 years of age). For each analysis, we generated the distribution of demographic characteristics among cases and controls. We examined the unadjusted association between demographic factors and home environment conditions by case-control status using odds ratios (ORs) and 95% confidence intervals (CIs). We used the OR to estimate the risk ratio because the prevalence of current asthma was less than 10%.8,14 We used multiple logistic regression to examine the relationship between home environment conditions and asthma case-control status, controlling for sociodemographic characteristics (e.g., age, gender, race/ethnicity, geographic region, education, and FPL).
The adjusted ORs (AORs) and 95% CIs from the models show the association between the presence of the home environment factors and having current asthma. We used the likelihood ratio test to evaluate improvement in the models after adding the following interaction terms: FPL and use of a fireplace or wood-burning stove, cockroaches and location, mold and use of a dehumidifier, and mold and use of a humidifier. However, the interaction results are not shown because they were not statistically significant.
RESULTS
Response rates
The overall response rate for the NAS-NYS screening interview (including controls) was 46%. The person-level interview completion rate, which measures the number of detailed interviews completed among sampled adults or children with asthma, was 89%. Of the 11,713 households surveyed for the NAS-NYS, 1,573 households (13.4%) had at least one individual with current asthma, 456 households (3.9%) had at least one individual with lifetime asthma only, and 9,684 households (82.7%) had no individuals with current or lifetime asthma. A total of 1,412 households with at least one member with current asthma and 2,290 control households answered questions about their home environment conditions.
Child case-control analysis
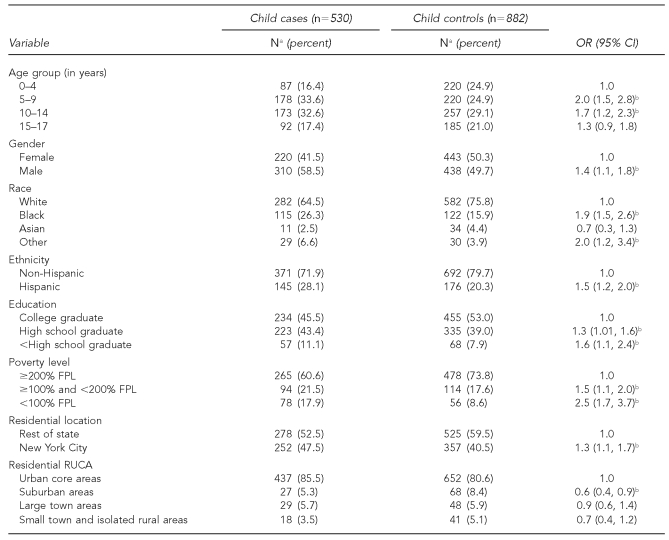
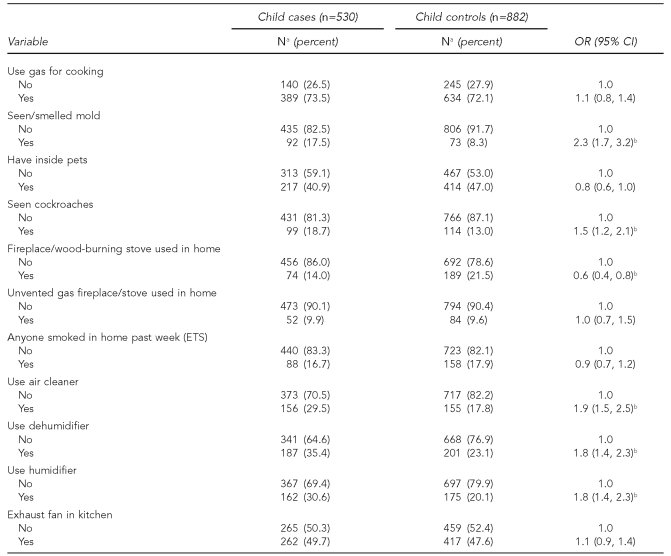
There were 530 cases and 882 controls in the child case-control analysis. Tables 1a and 1b present the unadjusted results of the sociodemographic characteristics and home environment conditions, respectively. The unadjusted ORs reveal that cases were more likely than the controls to be 5–14 years of age, male, black or another race, or Hispanic (Table 1a). In addition, children with current asthma were more likely than the controls to be from households with lower educational attainment and <200% FPL. Child cases were more likely than the controls to reside in New York City, but less likely to reside in suburban areas. The unadjusted ORs for the home environment conditions indicate that the presence of mold and cockroaches and the use of air cleaners, dehumidifiers, and humidifiers inside the home were significantly associated with having current asthma (Table 1b). However, children with current asthma were less likely than controls to live in homes where a wood-burning stove or fireplace was used. There were no statistically significant associations for current asthma and the presence of indoor pets, ETS, the use of gas for cooking, unvented gas fireplace or stove, or kitchen exhaust fans.
Table 1a.
Distribution of selected confounders and unadjusted odds ratios in case vs. control children (n=1,412), 2003 National Asthma Survey—New York State
aDue to missing values, numbers for some variables do not equal the total of cases and controls.
bStatistically significant
OR = odds ratio
CI = confidence interval
FPL = federal poverty level
RUCA = rural urban commuting area
Table 1b.
Distribution of home environment exposures and unadjusted odds ratios in case vs. control children (n=1,412), 2003 National Asthma Survey—New York State
aDue to missing values, numbers for some variables do not equal the total of cases and controls.
bStatistically significant
OR = odds ratio
CI = confidence interval
ETS = environmental tobacco smoke
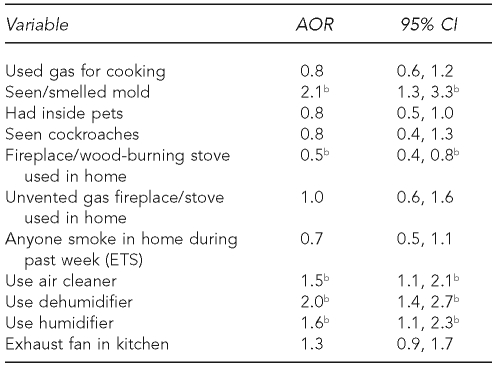
The logistic regression model (Table 2) reveals that children with current asthma were more likely to live in a home with mold (OR=2.1, 95% CI 1.3, 3.3) and a home in which a humidifier was used (OR=1.6, 95% CI 1.1, 2.3). There were no statistically significant associations between current asthma status and the use of gas for cooking, indoor pets, cockroaches, ETS, and kitchen exhaust fans. A wood-burning stove or fireplace was less likely to be used in a household with a child with asthma (OR=0.5, 95% CI 0.4, 0.8). With regard to modifications that mitigate triggers inside the home, children with current asthma were more likely to live in a home in which a dehumidifier (OR=2.0, 95% CI 1.4, 2.7) or an air cleaner (OR=1.5, 95% CI 1.0, 2.1) was used.
Table 2.
Adjusted odds ratiosa for current asthma by home environment exposures in case and control children (n=912), 2003 National Asthma Survey—New York State
aLogistic regression adjusted for age, gender, race/ethnicity, geographic region, education, and percent of the poverty threshold
bStatistically significant
AOR = adjusted odds ratio
CI = confidence interval
ETS = environmental tobacco smoke
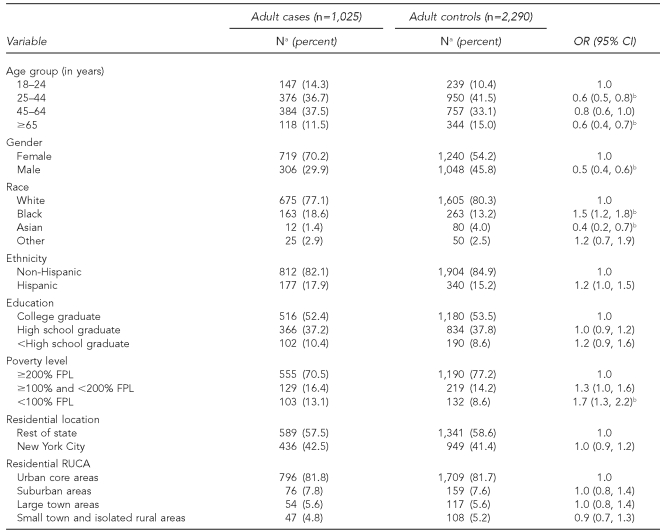
Adult case-control analysis
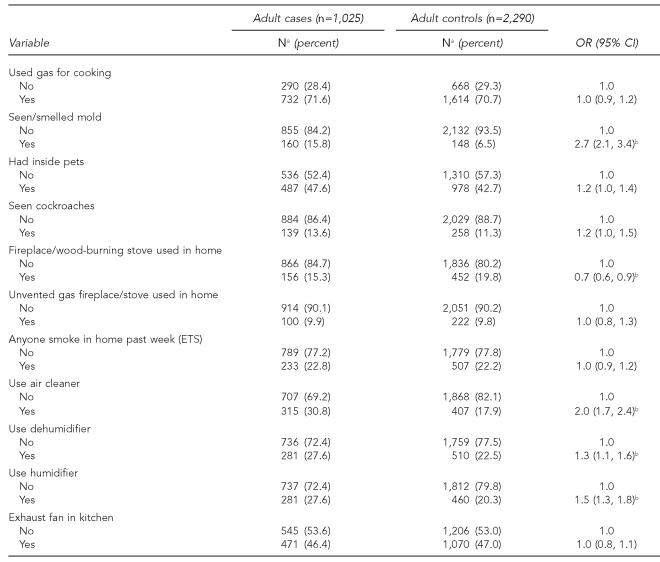
The adult analysis included 1,025 cases and 2,290 controls. The unadjusted ORs of sociodemographic characteristics (Table 3a) show that adults with current asthma were more likely than the controls to be black and to live in households that were <100% FPL. However, cases were less likely to be male, Asian, and 25–44 years or ≥65 years of age compared with the controls. We did not observe statistically significant differences between adult cases and controls with respect to ethnicity, residential location, and level of education. Unadjusted ORs for the home environment conditions (Table 3b) show that the presence of mold and the use of air cleaners, dehumidifiers, and humidifiers were positively associated with current asthma. A wood-burning stove or fireplace was less likely to be used in the homes of adults with current asthma. However, there were no statistically significant differences between cases and controls regarding the use of gas for cooking or the presence of indoor pets, cockroaches, an unvented gas fireplace or stove, or kitchen exhaust fan.
Table 3a.
Distribution of selected confounders and unadjusted odds ratios in case vs. control adults (n=3,315), 2003 National Asthma Survey—New York State
aDue to missing values, numbers for some variables do not equal the total of cases and controls.
bStatistically significant
OR = odds ratio
CI = confidence interval
FPL = federal poverty level
RUCA = rural urban commuting area
Table 3b.
Distribution of home environment exposures and unadjusted odds ratios in case vs. control adults (n=3,315), 2003 National Asthma Survey—New York State
aDue to missing values, numbers for some variables do not equal the total of cases and controls.
bStatistically significant
OR = odds ratio
CI = confidence interval
ETS = environmental tobacco smoke
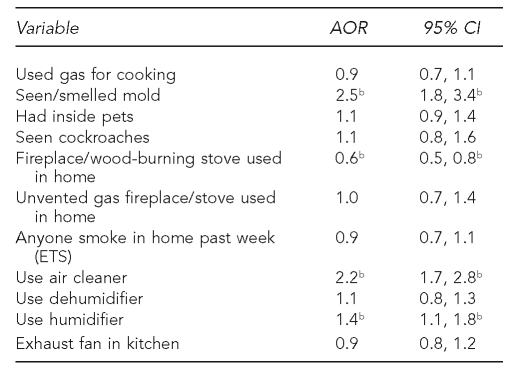
The AORs (Table 4) show that adults with current asthma were more likely than controls to report seeing or smelling mold in their homes (AOR=2.5, 95% CI 1.8, 3.4) and to use a humidifier (AOR=1.4, 95% CI 1.1, 1.8). Wood-burning stoves or fireplaces were less likely to be used in the homes with an adult with asthma (AOR=0.6, 95% CI 0.5, 0.8). Adults with current asthma were more than twice as likely as the controls to use an air cleaner (AOR=2.2, 95% CI 1.7, 2.8). We found no other statistically significant associations for the remaining home environment factors.
Table 4.
Adjusted odds ratiosa for current asthma by home environment exposures in case and control adults (n=2,020), 2003 National Asthma Survey—New York State
aLogistic regression adjusted for age, gender, race/ethnicity, geographic region, education, and percent of the poverty threshold
bStatistically significant
AOR = adjusted odds ratio
CI = confidence interval
ETS = environmental tobacco smoke
DISCUSSION
To our knowledge, this is the largest asthma prevalence study that represents both child and adult populations in NYS. We found that the associations between home environment conditions and current asthma were fairly consistent for children and adults. Households having a member with current asthma were more likely to report the presence of mold and use of air cleaners and humidifiers, which may be used to modify their physical home environment or control asthma. Conversely, a fireplace or wood-burning stove was less likely to be used in the homes of participants with current asthma.
Asthma is a chronic disease that is often exacerbated by exposure to environmental triggers. Our results are consistent with other studies that show a higher prevalence of mold among households having an adult or child with asthma. For example, a cross-sectional community-based study among adults from 18 different countries conducted by Zock et al. found an association between mold exposure in the last 12 months and current asthma (OR=1.28, 95% CI 1.13, 1.46).15 A Taiwanese study conducted by Lee et al. reported that visible mold on walls at home was independently associated with the occurrence of asthma symptoms in adulthood (OR=1.49, 95% CI 1.09, 2.01).16 In a previous study of children, Lee and colleagues found positive associations between reports of visible mold on walls at home and asthma in girls (OR=1.20, 95% CI 1.01, 1.41) and boys (OR=1.27, 95% CI 1.10, 1.47).17 A large, population-based case-control study in China found an association between childhood asthma and having mold or fungi on the ceilings of the house or inside the child's room (OR=1.8, 95% CI 1.1, 2.9).18
The findings also suggest that households with members who have asthma are more likely to use air cleaners and humidifiers. While it is possible that individuals with asthma and their families may selectively make changes in their behavior to avoid certain environmental asthma triggers, these modifications are not easily categorized as positive or negative changes. For example, some air cleaners and purifiers, thought by the public to remove pollutants from indoor air, can produce levels of ozone (a potential asthma trigger) that exceed federal and state health-related standards.19 Likewise, it is a common perception that humidifier use decreases dry air (another asthma trigger). Multiple studies have reported an association between current asthma and the use of a humidifier. However, the interpretation of these findings is complicated. For example, in a cross-sectional study among Canadian children aged 5–8 years, Dekker et al. reported a statistically significant association between current asthma and the use of a humidifier in the home (OR=1.66, 95% CI 1.36, 2.01).20
From a cohort study in California, McConnell et al. found that children with no history of wheezing had an increased risk of developing asthma when a humidifier was used (rate ratio = 1.7, 95% CI 1.2, 2.4).21 In a case-control study, Infante-Rivard found that the presence of a humidifier in the child's room prior to the time of diagnosis was significantly associated with asthma (OR=1.89, 95% CI 1.30, 2.74).22 One theory in the literature that may explain this association is that humidifiers may contribute to mold production in the humidifier itself or by increasing the relative humidity in the home.21–23 There is also evidence that high relative humidity increases the presence of triggers, such as dust mites.24 However, due to the design of our study, we could not test these hypotheses.
This study indicates that the use of a fireplace or wood-burning stove was less prevalent in homes with child and adult cases than in homes of controls, even when adjusted for socioeconomic status and geographic region. While several studies found that having a fireplace or wood-burning stove was associated with higher asthma prevalence,25–27 other studies found no association,20,28–31 and several have mentioned that some households with asthma may decrease or stop their use of a fireplace or wood-burning stove.29,30 It is possible that our finding reflects changes in behavior (i.e., not using fireplaces or wood-burning stoves) in an effort to avoid asthma triggers.
We did not find statistically significant associations between current asthma and the presence of pets, cockroaches, and ETS. Our study assessed the home environment conditions presently associated with the current asthma status of the participants, which could be the result of modification to the homes of people with asthma in response to dissemination of environmental control messages. On the other hand, the prevalence of these triggers in homes of people with asthma was not lower than in control homes.
Strengths and limitations
This study had several strengths that enhanced our understanding of the indoor environment in which many New Yorkers with asthma live. First, this study provided information on both children and adults in NYS. With respect to environmental asthma, the NAS-NYS is unique in the large number of households that were surveyed and the broad geographic and sociodemographic representation of the participants. While many large-scale surveys accommodate only one or two questions about a specific environmental factor, our survey included a wide range of environmental questions. In addition, this survey used standardized questions to assess the home environment. Finally, we presented information on both environmental triggers related to asthma as well as environmental and behavioral modifications among families with asthma.
There were also several limitations associated with this study. First, this survey was conducted in 2003 and it is possible, although unlikely, that behaviors or housing conditions have changed significantly since then. This survey also did not assess whether the exposure to environmental triggers or changes in behavior occurred before the onset or exacerbation of asthma. This study was not designed to establish a causal relationship with exposures (e.g., mold and the onset of asthma) and did not control for some important confounders (e.g., family history of asthma) and other indoor and outdoor triggers. However, the assessment of existing home environment conditions is appropriate in this case because our study objective was to specifically characterize the current home environment conditions and current asthma status. While this survey comprehensively assessed multiple home environment conditions, a different study design would allow for more detailed information about the timing and intensity of exposures and parent/patient knowledge of triggers.
Issues of self-report and sensitivity may also complicate the interpretation of findings regarding environmental conditions. Self-reported or, in the case of children, proxy-reported information is subject to recall and social desirability bias. For instance, people with asthma or parents of children with asthma often have some knowledge of environmental triggers and appropriate environmental modifications; they might be eager to give the “right” answer rather than the true answer, especially to sensitive questions about smoking, the presence of cockroaches, and having pets. If this were the case, the result would be an underestimate of exposure among cases, and the underlying associations might be missed. On the other hand, overreporting of visible mold by cases may result in differential misclassification of exposure and an overestimation of the association with current asthma.
The findings of this study could be subject to some form of selection bias. First, the study sample only represents households with a landline telephone. Secondly, telephone surveys that rely on voluntary participation may be subject to self-selection. The random selection of subjects for this study and the use of vigorous methods to improve the participation rate (e.g., mailing advance letters and using Spanish-language interviews) may have reduced the amount of selection bias. Furthermore, the distribution of sociodemographic characteristics of adults and children in our study were very similar to the NYS population based on the 2000 U.S. Census (data not shown).
The literature has demonstrated the effectiveness of certain environmental interventions to reduce triggers and improve asthma morbidity. An expert panel convened by the National Center for Healthy Housing found compelling evidence of the effectiveness of asthma home interventions that include an indoor environmental assessment, education, smoking cessation, and the control of asthma triggers (including mold, cockroaches, rodents, and dust).32 The type of study we conducted can serve as a bridge between this evidence base and community efforts to help people with asthma reduce exposure to triggers. In addition, this study has increased our understanding of the home conditions of people with asthma and, thus, enhanced our ability to appropriately and effectively direct resources for environmental controls.
Future studies could address some of the limitations of the current survey. These studies should further explore the association with home environment conditions by asthma severity or for households that have multiple individuals with asthma. Moreover, some common triggers, such as dust, were not included in this analysis and may be important additions to future attempts to examine the association with current asthma. Alternatively, future studies should focus on whether people with asthma are engaging in desirable behaviors related to the home environment rather than characterizing the home environment. To achieve a comprehensive understanding of these associations, an in-depth assessment of the amount, frequency, and timing of environmental exposures in relation to specific asthma endpoints is recommended. Finally, although it is unlikely that behaviors or housing conditions may have changed significantly since 2003, another study would provide updated information.
CONCLUSIONS
Asthma guidelines emphasize the importance of reducing triggers in the home as part of a multifaceted approach to asthma control. Despite these guidelines, many asthma triggers (e.g., mold) were as prevalent or more so in the homes of New Yorkers with asthma as compared with control households. Asthma households were more likely to report the presence of mold, less likely to report the use of a fireplace or wood-burning stove, and not significantly different from control households in the presence of other assessed triggers.
Individuals can take actions to reduce their exposure to triggers in the home environment. However, for some people with asthma, these efforts may be hindered by real and perceived barriers, including a lack of accurate information about triggers and trigger control, inadequate resources to address potential environmental issues, and a lack of control over their home environment (e.g., structural changes requiring a landlord's intervention). Public health interventions in NYS should focus on educating people with asthma, their families, and their health-care providers about potential asthma triggers and trigger sources, and teaching methods to prevent, reduce, or eliminate environmental asthma triggers in the home.
REFERENCES
- 1.National Heart, Lung, and Blood Institute (US). Expert Panel Report 3 (EPR-3): guidelines for the diagnosis and management of asthma. Rockville (MD): Department of Health and Human Services, National Institutes of Health (US); 2007. [Google Scholar]
- 2.Moorman JE, Rudd RA, Johnson CA, King M, Minor P, Bailey C, et al. National surveillance for asthma—United States, 1980-2004. MMWR Surveill Summ. 2007;56(SS08)(1-14):18–54. [PubMed] [Google Scholar]
- 3.Akinbami L. Asthma prevalence, health care use and mortality: United States, 2003-05. [cited 2010 Jun 21]. Available from: URL: http://www.cdc.gov/nchs/data/hestat/asthma03-05/asthma03-05.htm.
- 4.New York State Department of Health. New York State asthma surveillance summary report. Albany (NY): NYSDOH; 2007. Oct, [cited 2009 Jul 31]. Also available from: URL: http://www.health.state.ny.us/statistics/ny_asthma/pdf/2007_asthma_surveillance_summary_report.pdf. [Google Scholar]
- 5.Elliott L, Arbes SJ, Harvey ES, Lee RC, Salo PM, Cohn RD, et al. Dust weight and asthma prevalence in the National Survey of Lead and Allergens in Housing (NSLAH) Environ Health Perspect. 2007;115:215–20. doi: 10.1289/ehp.9412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Salo PM, Jaramillo R, Cohn RD, London SJ, Zeldin DC. Exposure to mouse allergen in U.S. homes associated with asthma symptoms. Environ Health Perspect. 2009;117:387–91. doi: 10.1289/ehp.11847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wilson J, Dixon SL, Breysse P, Jacobs D, Adamkiewicz G, Chew GL, et al. Housing and allergens: a pooled analysis of nine US studies. Environ Res. 2010;110:189–98. doi: 10.1016/j.envres.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 8.New York State Department of Health. National Asthma Survey—New York State summary report. Albany (NY): NYSDOH; 2006. [cited 2009 Jul 31]. Also available from: URL: http://www.health.state.ny.us/statistics/ny_asthma/pdf/national_asthma_survey_nys.pdf. [Google Scholar]
- 9.Centers for Disease Control and Prevention (US). National Immunization Survey. [cited 2009 Jul 31]. Available from: URL: http://www.cdc.gov/nis.
- 10.O'Connor KS, Osborn L, Olson L, Blumberg SJ, Frankel MR, Srinath KP, et al. Design and operation of the National Asthma Survey. Vital Health Stat 1. 2008;46 [PubMed] [Google Scholar]
- 11.Census Bureau (US). Poverty thresholds 2003. [cited 2009 Jul 31]. Available from: URL: http://www.census.gov/hhes/www/poverty/threshld/thresh03.html.
- 12.Hall SA, Kaufman JS, Ricketts TC. Defining urban and rural areas in United States epidemiologic studies. J Urban Health. 2006;83:162–75. doi: 10.1007/s11524-005-9016-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.SAS Institute, Inc. SAS®: Version 9.1 for Windows. Cary (NC): SAS Institute, Inc.; 2004. [Google Scholar]
- 14.Rothman KJ. Epidemiology: an introduction. New York: Oxford University Press; 2002. [Google Scholar]
- 15.Zock JP, Jarvis D, Luczynska C, Sunyer J, Burney P. Housing characteristics, reported mold exposure, and asthma in the European Community Respiratory Health Survey. J Allergy Clin Immunol. 2002;110:285–92. doi: 10.1067/mai.2002.126383. [DOI] [PubMed] [Google Scholar]
- 16.Lee YL, Hsiue TR, Lee CH, Su HJ, Guo YL. Home exposures, parental atopy, and occurrence of asthma symptoms in adulthood in southern Taiwan. Chest. 2006;129:300–8. doi: 10.1378/chest.129.2.300. [DOI] [PubMed] [Google Scholar]
- 17.Lee YL, Lin YC, Hsiue TR, Hwang BF, Guo YL. Indoor and outdoor environmental exposures, parental atopy, and physician-diagnosed asthma in Taiwanese schoolchildren. Pediatrics. 2003;112:e389. doi: 10.1542/peds.112.5.e389. [DOI] [PubMed] [Google Scholar]
- 18.Zheng T, Niu S, Lu B, Fan X, Sun F, Wang J, et al. Childhood asthma in Beijing, China: a population-based case-control study. Am J Epidemiol. 2002;156:977–83. doi: 10.1093/aje/kwf127. [DOI] [PubMed] [Google Scholar]
- 19.Britigan N, Alshawa A, Nizkorodov SA. Quantification of ozone levels in indoor environments generated by ionization and ozonolysis air purifiers. J Air Waste Manag Assoc. 2006;56:601–10. doi: 10.1080/10473289.2006.10464467. [DOI] [PubMed] [Google Scholar]
- 20.Dekker C, Dales R, Bartlett S, Brunekreef B, Zwanenburg H. Childhood asthma and the indoor environment. Chest. 1991;100:922–6. doi: 10.1378/chest.100.4.922. [DOI] [PubMed] [Google Scholar]
- 21.McConnell R, Berhane K, Gilliland F, Islam T, Gauderman WJ, London SJ, et al. Indoor risk factors for asthma in a prospective study of adolescents. Epidemiology. 2002;13:288–95. doi: 10.1097/00001648-200205000-00009. [DOI] [PubMed] [Google Scholar]
- 22.Infante-Rivard C. Childhood asthma and indoor environmental risk factors. Am J Epidemiol. 1993;137:834–44. doi: 10.1093/oxfordjournals.aje.a116745. [DOI] [PubMed] [Google Scholar]
- 23.Lwebuga-Mukasa JS, Wojcik R, Dunn-Georgiou E, Johnson C. Home environmental factors associated with asthma prevalence in two Buffalo inner-city neighborhoods. J Health Care Poor Underserved. 2002;13:214–28. doi: 10.1353/hpu.2010.0519. [DOI] [PubMed] [Google Scholar]
- 24.Arlian LG, Morgan MS, Neal JS. Dust mite allergens: ecology and distribution. Curr Allergy Asthma Rep. 2002;2:401–11. doi: 10.1007/s11882-002-0074-2. [DOI] [PubMed] [Google Scholar]
- 25.Honicky RE, Osborne JS, III, Akpom CA. Symptoms of respiratory illness in young children and the use of wood burning stoves for indoor heating. Pediatrics. 1985;75:587–93. [PubMed] [Google Scholar]
- 26.Thorn J, Brisman J, Toren K. Adult-onset asthma is associated with self-reported mold or environmental tobacco smoke exposures in the home. Allergy. 2001;56:287–92. doi: 10.1034/j.1398-9995.2001.00805.x. [DOI] [PubMed] [Google Scholar]
- 27.Sotir M, Yeatts K, Shy C. Presence of asthma risk factors and environmental exposures related to upper respiratory infection-triggered wheezing in middle school-age children. Environ Health Perspect. 2003;111:657–62. doi: 10.1289/ehp.5824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maier WC, Arrighi HM, Morray B, Llewellyn C, Redding GJ. Indoor risk factors for asthma and wheezing among Seattle school children. Environ Health Perspect. 1997;105:208–14. doi: 10.1289/ehp.97105208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Noonan CW, Ward TJ. Environmental tobacco smoke, woodstove heating and risk of asthma symptoms. J Asthma. 2007;44:735–8. doi: 10.1080/02770900701595675. [DOI] [PubMed] [Google Scholar]
- 30.Eisner MD, Yelin EH, Katz PP, Earnest G, Blanc PD. Exposure to indoor combustion and adult asthma outcomes: environmental tobacco smoke, gas stoves, and woodsmoke. Thorax. 2002;57:973–8. doi: 10.1136/thorax.57.11.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tuthill RW. Woodstoves, formaldehyde, and respiratory disease. Am J Epidemiol. 1984;120:952–5. doi: 10.1093/oxfordjournals.aje.a113966. [DOI] [PubMed] [Google Scholar]
- 32.National Center for Healthy Housing. Housing interventions and health: a review of the evidence. Columbia (MD): National Center for Healthy Housing; 2009. [cited 2009 Jul 31]. Also available from: URL: http://www.nchh.org/Portals/0/Contents/Housing%20Interventions%20and%20Health.pdf. [Google Scholar]