The science of epidemiology began largely through the investigation of outbreaks. While the field evolved to encompass other types of health problems, outbreak investigations and the need to respond quickly to health concerns have remained critical services for public health departments. In addition to the traditional roles of health departments in investigating outbreaks, the expansion of activities focused on public health preparedness has increased the need to have well-trained volunteers available to provide surge capacity in the event of an emergency.
There is also an ongoing need in health departments for a well-educated public health workforce. One strategy to help students learn to practice public health has been through curriculum design of practical applications and opportunities for participation in either research projects or field experiences.1,2 Such applications can introduce students to the work of public health departments, provide opportunities for students to practice newly learned classroom skills and tools, and give practical assistance to health departments. While most public health professionals recognize the need for collaboration between schools of public health (SPHs) and health departments, there are often roadblocks due to competing interests and resources. The challenge in making these partnerships work is to find a program that benefits all parties and makes as few extra demands as possible on the partners.
Establishing student teams able to respond to public health incidents benefits the fields of preparedness and epidemiology in two major ways. First, the students can serve as trained surge capacity for the health departments in the case of an outbreak or other public health incident. Second, participation allows public health graduate students to gain real-world experience in a health department, outside of an internship or thesis project. To date, approximately 25% of accredited SPHs have established some form of student response teams.
The Epidemiology Program at the Mel and Enid Zuckerman College of Public Health (MEZCOPH) at the University of Arizona in Tucson, Arizona, identified the need to provide additional opportunities for students to apply what they were learning in a practical setting. An assessment was conducted to determine the needs of local and state health departments and the level of interest for working with public health students. From this assessment and pilot student experiences, the Student Aid for Field Epidemiology Response (SAFER) team was developed to include trainings within health departments and field experiences. These efforts were sustained through funding from health departments and incorporation of experiences into coursework requirements. The following sections describe the development process, the joint health department-university training program, a summary of student experiences, and strategies used for program sustainability.
STRUCTURE AND TRAINING OF THE SAFER TEAM
Needs assessment for a student epidemiologic response team
The goal of SAFER was to create a student response team that could respond quickly to a health department's needs during an outbreak investigation. Interviews conducted with health department leaders and staff, college faculty and administration, and other student response programs (1) determined the level of readiness for health departments to use students and (2) identified types of outbreaks and health problems that could be addressed with students as well as training needs and responsibilities and expectations for both students and health departments.
The health departments raised several issues of concern. First, it was important to the health departments that students be trained before an event occurred. A second issue concerned identification of potential student activities. Other issues included confidentiality and funding.
The issue of training was addressed by having partnering health departments create their own training sessions and offer input regarding student training materials. Potential student activities identified by the health departments included data collection, data analysis, sample transport, questionnaire development, and contact tracing; many of these have since become core activities for SAFER students. Confidentiality issues were addressed by having students attend lectures both at the health departments and within the SAFER course on the importance of maintaining patient information and how laws such as HIPAA apply to public health. Students must also sign confidentiality forms with each health department prior to conducting any interviews. In addition, the program coordinator is trained in departmental procedures pertaining to confidentiality, and students are required to conduct interviews in private locations at the university or health department. Funding issues (specifically travel costs) are an ongoing issue and are discussed later in this article.
Team structure and management
During SAFER's development, other SPHs were also developing and refining their own student response teams.3–5 Team EpiAid at the University of North Carolina published recommendations for a single point of contact being identified at the university with whom partnering agencies could request assistance and coordinate activities.3 The county health department coordinator with Emory University's Student Outreach and Response Team provided further advice on establishing a team and identifying potential student activities in the fall of 2004. These recommendations led to the creation of a coordinator position with responsibilities for organizing trainings and seminars, teaching outbreak principles, maintaining contact with health departments during and between outbreaks, and organizing student response efforts when requested.
Training sessions at health departments
Participating health departments were asked to develop and host at least one training session. These sessions helped the partners gain confidence that students had the proper training prior to assisting the department. The joint sessions also assured investment in the partnership. Ultimately, the Arizona Department of Health Services (ADHS), the Maricopa County Department of Public Health (MCDPH), and the Pima County Health Department (PCHD) each developed training sessions that were incorporated into the overall SAFER course and program. Content in these training sessions ranged from review of surveillance systems used in local health departments, to the specifics of conducting a foodborne outbreak (including mock interviews with health department staff), to working within a call center during a public health emergency. These training sessions also allowed students to become accustomed to the location and layout of the health departments and to meet current public health professionals.
Creation of class for credit
Originally, the program was to be an extracurricular program with a college-sponsored program coordinator facilitating activities. After the program's pilot experiences, it became apparent that the SAFER team could work within the university's structure and serve as an asset for the university in maintaining its partnerships with health departments. The epidemiology academic program created a specific course in which membership on the team was mandatory. Later, this course became a required part of the Master of Public Health curriculum for the epidemiology concentration. The course was designed as a seminar style class that incorporated lectures on infectious disease outbreaks, guest speakers with knowledge in infectious disease investigations, and student presentations.
Students were required to commit two two-hour blocks of time each month to be available for response activities, with the understanding that if a large-scale outbreak occurred, all students would be notified and expected to make a best effort to respond. During time periods when an active outbreak investigation was not ongoing, students worked collectively on projects that were predetermined by the coordinator and health department partners. Examples of projects include literature reviews, revising health department questionnaires, or conducting data analyses on prior investigations.
The decision to create the course for credit was made not only to provide students academic credit for the experience they were gaining, but also to gain consistency in schedules. Due to the fact that outbreaks cannot be predicted, it was difficult to maintain an ongoing relationship with students during an academic year and to keep them engaged if there was a long lag time between outbreak responses.
Responding to an outbreak
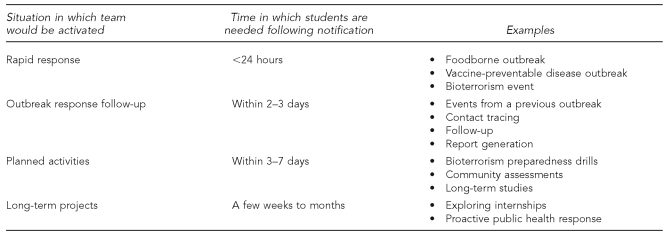
The SAFER program coordinator is informed of an outbreak investigation by contact from a health department epidemiologist. Together, they determine the type of student activities required, the number of students needed, the timeline, and any special skills needed. This communication process and the required course hours per student have created a process whereby the team can typically respond within 24 hours (Figure 1). To address issues of distance and travel time (the distance between Tucson [MEZCOPH] and Phoenix [ADHS and MCDPH] is more than 100 miles), the program coordinator was given access to a secure e-mail account allowing confidential information, such as line lists, to be transmitted.
Figure 1.
Potential student activities with a health department based on the situation and time frame in which the team responds
Due to confidentiality concerns, telephone interviews must always be made from the university in a private location. Students are required to input all interview responses into established health department databases. The interview forms are then either faxed back to the health department or entered into a database. Originals are securely stored until they are no longer needed and then destroyed. All of this is not to imply that students never leave the building. Students have also conducted door-to-door interviews, worked at the county health department's call center, conducted field surveillance, and taken part in points-of-dispensing (POD) activities.
TYPES OF STUDENT RESPONSES
Student response to outbreaks
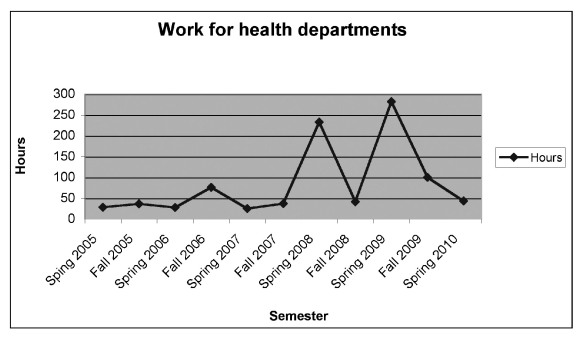
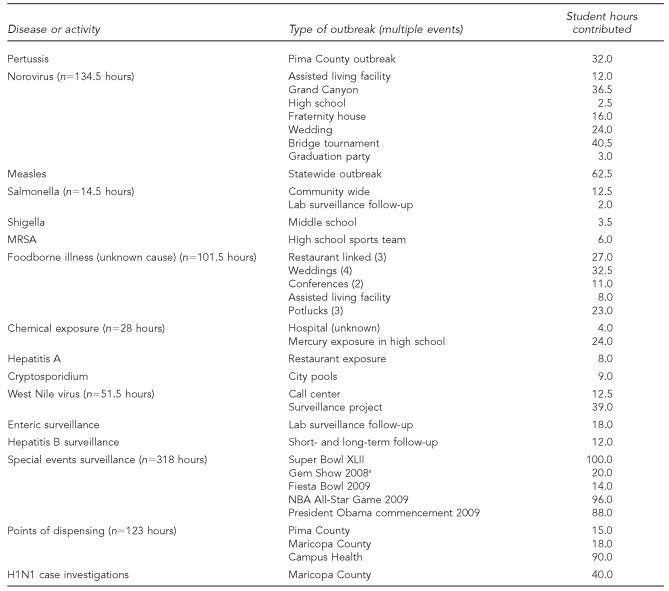
Beginning in the spring semester of 2005 until the spring semester of 2010, 79 students have contributed a total of 962 hours to responding to activities of collaborating health departments. The activities have included 35 outbreak investigations, eight surveillance activities, and two POD activities. As shown in Figure 2, the amount of student hours varied by semester depending on outbreak detection in the community and ongoing team surveillance projects. The Table details the various types of outbreaks that students have been called upon to help investigate. The most common activities are outbreak investigations of gastrointestinal illnesses. SAFER has investigated five laboratory-confirmed norovirus outbreaks, including one involving multiple groups of river rafters on the Colorado River in the Grand Canyon,6 in which cases had to be tracked all over the world. While most of the outbreaks involved foodborne-related diseases (e.g., salmonellosis, shigellosis, and hepatitis A infection), SAFER has also worked on two community-wide outbreaks of pertussis and measles.7
Figure 2.
Number of student hours spent on Student Aid for Field Epidemiology Response health department projects by semester, University of Arizona MEZCOPH, 2005–2009
MEZCOPH = Mel and Enid Zuckerman College of Public Health
Table.
Student time spent on Student Aid for Field Epidemiology Response health department projects by disease or activity, University of Arizona MEZCOPH, 2005–2009
aSurveillance conducted from the health department, not on-site
MEZCOPH = Mel and Enid Zuckerman College of Public Health
MRSA = methicillin-resistant Staphylococcus aureus
NBA = National Basketball Association
Student involvement in surveillance projects and activities
SAFER also trained and participated in various surveillance activities. These have included an assessment of a neighborhood West Nile virus educational campaign, assisting county health departments to complete routine investigations of laboratory-confirmed enteric cases, and participation in real-time syndromic surveillance at several special events. The SAFER coordinator assisted the Epidemiology Division of MCDPH in planning for enhanced surveillance for Super Bowl XLII, which was held in Glendale, Arizona, in February 2008. A plan was developed for students to work with the local fire department, which had responsibility for the on-site first aid stations.
On game day, assessments were made on -individuals seeking medical care at the station as to whether they met the criteria for one of four syndromes (e.g., gastrointestinal, respiratory, neurological, or skin). If they did meet one of these criteria, a SAFER team member completed an additional questionnaire on potential suspect exposures. The student member then immediately entered the data on numbers of illnesses and possible exposures and sent the information to the health department. While no unusual health-related events were detected during this Super Bowl, the other first-responder agencies appreciated having public health personnel present. The county health department representatives also felt it was helpful to have reporting personnel on-site. SAFER students have since worked four large events, including the Fiesta Bowl, the National Basketball Association All-Star Game, the Tucson Gem Show, and President Obama's convocation speech at Arizona State University, for a total of 318 hours.
Preparedness activities
One of the strategies for sustaining the SAFER program was to work in collaboration with the Arizona Center for Public Health Preparedness (AzCPHP). Students were required to complete training on the public health incident command system.8 As a result of these trainings, SAFER students received opportunities to take part in community preparedness activities with county health departments. Two of these opportunities included working a POD exercise in which the PCHD tested its ability to vaccinate large numbers of people quickly by providing seasonal influenza vaccine to children and conducting POD checks (annual checking of equipment) at sites around Maricopa County. The third opportunity was a mass-dispensing drive-through clinic for seasonal flu vaccine with Campus Health at the university.
LESSONS LEARNED
There have been many lessons learned from this process that can be helpful for an SPH or a health department looking to establish a student response team. They are listed and then explained subsequently in greater detail:
Establish a position for a dedicated program coordinator.
Work to integrate the team into the health department system.
Establish protocols including those related to information sharing.
Find ways to fund the program that benefits both sides.
Look for other ways to collaborate to strengthen relationships.
Recognize that student schedules may be different from those of health department employees.
Establish a program coordinator
It is highly recommended that a coordinator position dedicated to managing the team be created. This person can be employed either by the university or the health department (or, in the case of SAFER, can receive funding from both agencies). However, it is important to have consistency from year to year for the students, faculty, and the health department staff. The program coordinator should meet regularly with agency counterparts and could serve as a backup epidemiologist during public health responses. Finally, it is important that the coordinator be integrated into the academic program so that faculty members can assist the coordinator in fielding responses both from the university and the health departments.
Incorporate student teams into the health department
One of the challenges for a new team is to weave itself into the existing infrastructure for an outbreak response. The health department must remember to call the student team early in the investigation. This heightened awareness of the team can be facilitated by having the student team included in the health department's response plans and lists. The students can be considered as surge capacity, which then allows students to be part of general response. One way to promote this practice is to have students register as volunteers with the various health departments. Doing so addresses two important issues: credentialing and liability. Students who are preregistered with departments have already been credentialed and are ready to respond where appropriate. The issue of liability is also resolved because people who are officially registered as volunteers with the health department are covered under the department's liability insurance during a response. Liability is covered by the university during other activities, such as traveling to training sessions.
Establish protocols for student response
While it is important for student teams to be incorporated into health department plans, it is even more important for the team to have its own set of protocols. These protocols should include programmatic issues (e.g., training curricula, travel, or reimbursement procedures) and communication issues (e.g., between the health department and the program coordinator, between the program coordinator and the students, and among students). There should also be protocols for operational and epidemiologic topics such as contact tracing, data collection, data entry, or questionnaire storage and disposal.
Secure funding from all partners
Sustainability of the SAFER teams has been achieved through support from all participating partners: MEZCOPH, AzCPHP, and the health departments. The college provides partial financial support for the program coordinator for teaching the course each semester. The team has received acceptance by the state and county health departments for use of the student teams, demonstrated through increasing paid internships from the infectious disease offices of the health departments and specific financial support. One of the greatest successes SAFER has had toward maintaining its longevity is receipt of funding through an annual contract with MCDPH, which funds 50% of the program's expenses.
Enhance collaborations between the university and health departments
Sustainability is also assisted with enhanced collaborations between the university and the health departments. When the teams began, the state and county health departments noted that few public health students were completing internships with their agencies. Two outcomes of this collaboration have been an increased number of graduate students who complete their internships at either the state or local health departments and the increased number of MEZCOPH graduates who are beginning their careers at state and local health departments. Approximately 25% of SAFER students have either completed an internship or taken jobs with a health department following their participation with the team.
Recognize the need for flexibility when working with students
It is important that health departments recognize that these response teams include graduate students working within a limited time frame. The faculty and coordinator need to remind the health department partners of several realities:
While SAFER team members are all technically students, graduate students can take on substantial responsibility. It is important to reiterate this notion to a health department when selling the concept of a student team. The time taken to train students can be an investment that pays off either in the short term, through additional outbreak assistance, or in the long term, through a workforce more thoroughly trained in the health department's activities.
Schedules will be different from those of a health department employee. However, students are able to make interview calls between classes and do not shy away from responding in the evenings and on weekends.
Students find this work fascinating. For students who have only been able to conduct interviews in a training session, it is exciting, interesting, and offers a practical way for them to learn important skills.
CONCLUSIONS
A student epidemiology response team can be developed that fulfills the need of public health students to gain field experiences and to introduce them to the workings of local and state health departments. Strategies must be developed to sustain the program within the academic institution and build collaborations with health departments. The development and maintenance of this response team enables students to gain important field experiences in public health, while also creating a well-trained group that is capable of serving as surge capacity for Arizona health departments.
Footnotes
Articles for From the Schools of Public Health highlight practice- and academic-based activities at the schools. To submit an article, faculty should send a short abstract (50–100 words) via e-mail to Allison Foster, ASPH Deputy Executive Director, at afoster@asph.org.
REFERENCES
- 1.Lowe CR, Kostrzewski J. London: Churchill Livingstone; 1975. Epidemiology: a guide to teaching methods. [Google Scholar]
- 2.Olsen J, Saracci R, Trichopoulos D, editors. 2nd ed. New York: Oxford University Press; 2003. Teaching epidemiology—a guide for teachers in epidemiology, public health, and clinical medicine. [Google Scholar]
- 3.MacDonald PDM. Team Epi-Aid: graduate student assistance with urgent public health response. Public Health Rep. 2005;120(Suppl 1):35–41. doi: 10.1177/00333549051200S108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oberle MW, Foy HM, Alexander R, Kobayashi J, Hergerson SD. Enhancing student practicum opportunities: the outbreak investigation option. J Public Health Manag Pract. 1995;1:69–73. [PubMed] [Google Scholar]
- 5.Passaro D. School of public health prepares training and tools to combat terrorists: faculty and students form rapid response team. University of Illinois Chicago Newsletter Fall 2003. [cited 2009 Jul 20]. Available from: URL: http://www.uic.edu/depts/spha/about/healthviewsfall03/hv03_p1.pdf.
- 6.Malek M, Barzilay E, Kramer A, Camp B, Jaykus LA, Escudero-Abarca B, et al. Outbreak of norovirus infection among river rafters associated with packaged delicatessen meat, Grand Canyon 2005. Clin Infect Dis. 2009;48:31–7. doi: 10.1086/594118. [DOI] [PubMed] [Google Scholar]
- 7.Daniels S. Measles outbreak 2008. Pima County Health Department. September 2008. [cited 2009 Aug 21]. Available from: URL: http://www.pimahealth.org/disease/MeaslesReport2008.pdf.
- 8.Federal Emergency Management Agency (US) Independent study program. [cited 2009 Aug 22]. Available from: URL: http://training.fema.gov/IS/crslist.asp.