Abstract
Objective
The purpose of this study is to compare the incidence of possible complications of cervical lateral screw fixation and the achievements of bicortical purchase using the Roy-Camille, Magerl and the modified methods.
Methods
Six fresh-frozen cervical spine segments were harvested. The Roy-Camille technique was applied to C3 and C4, and the Magerl technique was applied to C5, C6, and C7 of one side of each cadaver. The modified technique was applied to the other side of each cadaver. The nerve root injury, violation of the facet joint, vertebral artery injury, and the bicortication were examined at each screwing level.
Results
No vertebral artery injury was observed in any of the three methods. One nerve root injury was observed in each cervical spine segment using the Roy-Camille method (8.3%), the Magerl method (5.6%), and the modified method (3.3%). Facet joint injuries were observed in two cervical spinal segments using the Roy-Camille method (16.7%) and three with the Magerl method (16.7%), while five facet joint violations occurred when using the modified method (16.7%). Bicortical purchases were achieved on ten cervical spinal segments with the Roy-Camille method (83.3%) and Magerl method (55.6%), while twenty bicortical purchases were achieved in the modified method (66.7%).
Conclusion
The advantages of the modified method are that it is performed by using given anatomical structures and that the complication rate is as low as those of other known methods. This modified method can be performed easily and safely without fluoroscopic assistance for the treatment of many cervical diseases.
Keywords: Lateral mass screw, Cervical vertebra, Roy-Camille technique, Magerl technique
INTRODUCTION
The cervical lateral mass screw fixation technique is frequently indicated for the stabilization of cervical instabilities caused by trauma, degenerative disease, or tumor2,9,17,24).
Several authors have reported that posterior lateral mass screw fixation provides biomechanical stability equal to those of anterior plating or the posterior wiring technique6,12,22,28). Moreover, the application of posterior lateral screw fixation became easier as a result of the development of the polyaxial screw-rod system7,13,19,21,27).
Since the first description of the technique by Roy-Camille et al. in 1972, several lateral mass screw fixation techniques have been suggested by Louis, Magerl, Anderson and An1,2,17,23). According to previous anatomic and clinical studies, the two most popular types of lateral mass screw techniques are the Roy-Camille technique and the Magerl technique. In the Roy-Camille technique, a screw is inserted perpendicular to the posterior surface of the lateral mass, while in the Magerl technique, the screw is directed 25 degrees laterally, parallel to the superior facet joint. In addition, the Kim's technique : the modification of known other lateral mass screw techniques in which the screw is inserted parallel to the spinous process and its lateral angle is determined by axial angle of spinous process without fluoroscopic assistance was suggested by our senior author (KDH)5).
Though these techniques have unique entrance points for screw insertion and trajectory, avoiding injury to the anatomical structure is still challenging. The anatomic structures at risk during lateral mass screwing of the cervical spine are the nerve roots, the vertebral artery, and the adjacent lateral masses1,9,11,24,29). In addition, achievement of bicortical screw fixation is also an important issue for successful bone fusion16).
The Roy-Camille technique is associated with a higher incidence of facet joint violation, while nerve root injury tends to occur more frequently with the Magerl technique3,15,29). Although our senior author (KDH) had studied optimal angle and screw length used in modified lateral mass screw fixation, the incidences of possible complications of the Kim's technique had not been studied properly.
The purpose of this study is to quantitatively compare the incidences of nerve root or vertebral artery injury and facet joint violation, as well as achievement of bicortical screw fixation, among the Roy-Camille technique, the Magerl technique, and the Kim's technique5).
MATERIALS AND METHODS
Six fresh-frozen cervical spine segments (C3 to C7) were harvested from human donors (M = 4; F = 2; mean age = 70). Three lateral mass screw insertion techniques were performed in this study : the Roy Camille, the Magerl, and the Kim's method. The Roy-Camille technique was applied to C3 and C4 and the Magerl technique to C5, C6, and C7 of one side of each cadaver. The Kim's technique was applied to C3-C7 of the other side of each cadaver. The screw-spinal nerve relationship, the penetrating degree of the ventral bony cortex, the violation of the facet joint surface, and the extent of vertebral artery injury were examined at each screwing level. To determine the-three dimensional safety of the lateral mass screw, we evaluated three-dimensional cervical CT scan results, as well as gross findings.
Surgical anatomy dissection
Each cadaver was placed in a prone position with the neck in the neutral position. After a standard midline incision and dissection, the posterior arches of the cervical vertebrae were exposed. Articular capsules were removed for clear identification of the lateral mass to verify the exact entrance point. All screw holes were drilled with a 2 mm drill bit, and 14 mm-length screws were used for each lateral mass screw fixation.
The entrance point for the Roy-Camille technique was at the center of the posterior surface and the screw was directed 10° lateral and perpendicular to the posterior surface of the lateral mass (Fig. 1A). The entrance point for the Magerl technique was 1 mm medial and cranial from the center of the posterior surface, and the screw was directed 25° lateral and parallel to facet joint, which is approximately 45° cranial to the posterior surface of the lateral mass (Fig. 1A). For the Kim's technique, the entrance point was 1 mm medial from the center of the posterior sur-face (Fig. 2A), and the screw was inserted parallel to the center of the spinous process on its lateral view; by leaning the body of the screw driver on the tip of the spinous process, the screw's lateral angle was determined by the angle of the spinous process (Fig. 1B, 2B).
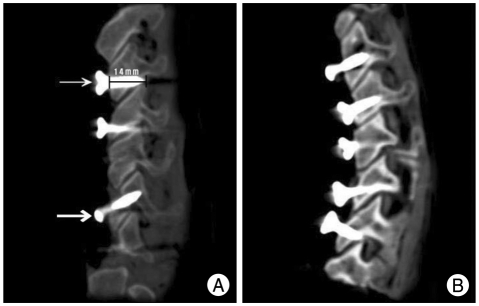
Fig. 1.
Radiologic finding of the cadaveric study. A : The Roy-Camille method (thin arrow) which shows its sagittal angle which is perpendicular to the lateral mass. The screw length was 14 mm and the screw violates facet joint on C3 level. The Magerl method (bold arrow) whose sagittal angle is parallel to the facet joint. B : The Kim's method on each level.
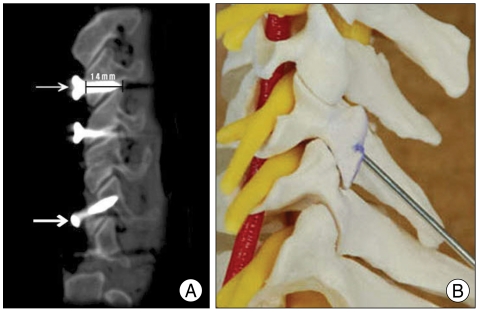
Fig. 2.
A cervical spine model showing the trajectory of the Kim's method. A : Posterior view of the cervical spine model that shows the entrance point and trajectory; the entrance point is 1 mm medial from the center of the posterior surface. The lateral angle is determined by leaning the body of the screw driver on the tip of the spinous process. B : Lateral view of the cervical spine model showing the sagittal plane of the Kim's method that passes through the center of the posterior arch of the spine.
Complication analysis
After screw fixation, we harvested each cervical spine and checked the three-dimensional CT image (Fig. 3) to visualize bicortication and facet joint violation. Then we dissected and grossly observed occurrences of vertebral artery violation and nerve root injury. Nerve root injury was graded by the degree of nerve root violation, as suggested by Xu et al.30) (Grade I : contact with the ventral or dorsal ramus, Grade II : penetration of the ventral or dorsal ramus, Grade III : contact with or penetration of the ventral and dorsal rami) and facet joint violation was measured by the length of the screw that violated the facet joint.
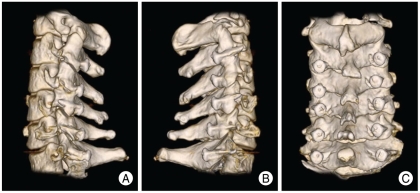
Fig. 3.
Three dimensional image of CT scan. A : Roy-Camille method was performed on C3 and 4 while Magerl method was performed on C5 to C7. B : The Kim's method was performed on C3 to C7 of the lateral mass of the other side. C : Posterior view.
Statistical analysis
Statistical analyses were performed with the Statistical Package for the Social Sciences (SPSS) for Windows, Version 14.0. We performed one-factor analysis in order to determine the difference between two methods (Kim's vs. Roy-Camille, Kim's vs. Magerl) for each factor. Cross-tabulation analysis was used, and the level of statistical significance was considered to be 0.05. When the values of two screwing levels were zero, the factor was excluded from statistical analysis.
RESULTS
Thirty cervical spine segments of six cadavers were used in our statistical analysis. Incidences of nerve root injury, vertebral artery injury, facet joint violation, and achievement of bicortical purchase were analyzed with each method (Table 1).
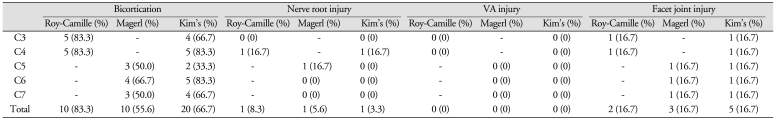
Table 1.
The comparison of the factors among the Roy-Camelle method, the Magerl method, and the Kim's method (percentage)
VA : vertebral artery
In our study, no vertebral artery injury was observed in any of the three methods. There was one nerve root injury for each use of the Roy-Camille method (8.3%) and the Magerl method (5.6%) among twelve and eighteen vertebral segments, respectively, while one nerve root injury occurred with the Kim's method (3.3%) among thirty vertebral segments. All of these nerve root injuries were Grade I. There were no statistically significant differences with the Roy-Camille method versus the Kim's method (p = 1.000) for C3 and C4 or between the Magerl and the Kim's method (p = 0.310) for C5, C6, and C7.
Facet joint injuries were observed on two of twelve vertebral segments using the Roy-Camille method (16.7%) and three of eighteen using the Magerl method (16.7%), while five facet joint violations occurred among thirty vertebral segments with the Kim's method (16.7%). All these violations were less than 2 mm. There were no significant differences between the Roy-Camille method and the Kim's method (p = 1.000) or between the Magerl and the Kim's method (p = 1.000).
Bicortical purchases were achieved in ten of twelve vertebral segments using the Roy-Camille method (83.3%), ten of eighteen using the Magerl method (55.6%), and twenty of thirty vertebral segments using the Kim's method (66.7%). There were also no significant differences between the Roy-Camille method and the Kim's method (p = 0.615) or between the Magerl and the Kim's method (p = 0.735).
DISCUSSION
Posterior cervical lateral mass screw fixation has been widely used for the management of cervical instabilities caused by trauma, neoplasm, degenerative disease or failed anterior fusion2,8,17,23). Several studies of the safety and the biomechanical stability of the posterior cervical lateral mass screw have been published6,12,22,28). Moreover, the application of the posterior lateral screw fixation method became easier as a result of the development of the polyaxial screw-rod system7,15,19,21,27).
Since the first description of the technique by Roy-Camille et al. in 1972, several lateral mass screw fixation techniques have been suggested by Louis, Magerl, Anderson and An1,2,17,23). Our senior author (KDH) suggested the modified lateral mass screw technique to fix the screw using an adjacent anatomical structure5).
Each of these techniques has a unique entrance point for screw insertion and trajectory. In the Roy-Camille method, the sagittal angle is a plane perpendicular to the lateral mass, and the entrance point is a midpoint on the posterior surface of the lateral mass. Using the Magerl method, the sagittal angle is parallel to the facet joint, and the entrance point is 1 mm superior and medial from a midpoint on the posterior surface of the lateral mass. In order to enable the procedure without fluoroscopic guidance, we used a spinous process to determine the sagittal angle. The screw was inserted parallel to the center of the spinous process on its lateral view. The screw's lateral angle was determined by the angle of the spinous process by leaning the body of the screw driver on the tip of the spinous process. The entrance point was 1 mm medial from the center of the lateral mass.
All of these methods have been continually modified to achieve successful fixation without anatomical injuries during screw fixation. According to several reported studies, possible complications which could occur during lateral mass screwing of the cervical spine are nerve root or vertebral artery injury and facet joint violation1,9,11,24,29). Heller et al.15) have suggested that the incidence of nerve root injury was higher with the Magerl technique than with the Roy-Camille technique. Xu et al.29) proposed modification of the traditional Magerl technique, involving a higher entrance point located only 2 mm inferior to the inferior edge of the superior facet so that the trajectory is more cephalad just beneath the articular surface, in order to avoid nerve root injury.
Ebraheim et al.11) evaluated the location of the vertebral artery and found that either Roy-Camille or Magerl technique could damage the vertebral artery with 15° lateral angulation. Cho and kim5) described no significant difference in the safety angles (mean angle less than 8°) for avoiding vertebral artery injury among the Roy-Camille, Magerl and the Kim's method.
Barry et al.3) reported that the Roy-Camille screw easily avoided nerve root injury because it was pointed midway between the nerve bundles. However, the risk of facet joint violation is higher with the Roy-Camille technique in comparison with the Magerl technique, especially at C5 and C6, because the nerve root groove and the facet joint are located close to the transverse plane, reducing the Roy-Camille safety zone. The Roy-Camille technique is, therefore, the best option at C3 or C4 rather than C5 or C6. On the basis of these studies, we used the Roy-Camille technique at the C3 and C4 level whereas the Magerl technique was used on C5, C6, and C7.
In our study, there was only one nerve root injury in each method, considering the entire vertebral segment; 8.3% for the Roy-Camille method, 5.6% in the Magerl method and 3.3% using the Kim's method. There were no significant differences among three values. According to Heller et al.15), nerve roots were placed at higher risk for injury (26.8%) with the Magerl method than with the Roy-Camille method (10.8%). Moreover, considering that all of the nerve root injuries were Grade I, all three methods were successful as the others. Facet joint violations occurred in 16.7% of cases with all three methods and also showed no significant difference between studies.
Heller et al.16) demonstrated that bicortical purchase provided pullout resistance for a lateral mass screw with a gain of approximately 30%, superior to that of unicortical purchase. Berry et al.4) concluded that there was no significant association between pullout resistance and cancellous BMD, consistent with the findings of Heller et al.16) However, screws that are too long will put the spinal nerve at greater risk of injury. Therefore, optimal screw length should be determined for successful screw fixation. Ebraheim et al.10) investigated safe lateral mass screw lengths. The safe screw length was 14-15 mm for the Roy-Camille technique and 15-16 mm with the Magerl technique; using both methods, the mean screw path length decreased from cephalad to caudal. This difference might be due to the relatively straight sagittal angle used with the Roy-Camille method compared to the oblique sagittal angle used with the Magerl method. Cho and Kim5) pre-sumed that the lateral masses in Koreans and East Asians may be shorter, on average, than those of Europeans or Hispanics and, therefore, focused on a Korean population. The mean screw path lengths were 13.5 mm at C3 to C6 and 13.0 mm at C7 for the Roy-Camille technique and 14 mm at C3 to C6 and 13.6 mm at C7 for the Magerl technique, consistent with the result of the study by Yoon et al.31) With the Kim's method, the minimal depth for bicortical screw fixation ranged from 13.7 mm to 13.9 mm at C3, C4, and C5.
We used a 14 mm length screw to optimize bicortical purchase and to avoid certain complications. Bicortical purchases were achieved in ten of twelve vertebral segments using the Roy-Camille method (83.3%), ten of eighteen using the Magerl method (55.6%) and twenty of thirty vertebral segments using the Kim's method (66.7%). There were also no significant differences with the Roy-Camille method vs. the Kim's method (p = 0.615) or the Magerl vs. the Kim's method (p = 0.735).
The use of intraoperative fluoroscopy to guide screw placement was first recommended by Heller et al.15) and is quite tempting, especially to the young spinal surgeons who lack experience performing lateral mass screw fixation. Therefore, it has been tried by many surgeons20). However, exposure to radiation during the operation is related to certain complications such as thyroid malignancy14,18). Therefore, other surgeons, such as Richter et al.25), suggested the use of a computer navigation system in cervical screw operation. Roche et al.26) suggested lateral mass screw fixation without the use of fluoroscopic assistance using a modified method by An et al.10) The entrance point was 1 mm medial to the center of the lateral mass and was aimed 33 degrees lateral and 17 degrees cephalad. Using this method, they described lateral mass screws that were placed safely without complication.
Although the Roy-Camille, Magerl and An methods are known to be safely performable, the determination of the application at the lateral or cephalad angle is often ambiguous in the operative field; therefore less experienced spinal surgeons tend to rely on fluoroscopic guidance. The authors also noted that, before considering the use of these techniques, the surgeon must have received advanced training in spinal surgery.
From this point of view, although the Kim's method has some similarities to those of the method proposed by An et al., the former does have certain advantages. The trajectory of the Kim's method is determined by the adjacent anatomical structures. From 1 mm medial to the center of the lateral mass, the sagittal angle is aimed parallel to the center of the spinous process on its lateral view. The lateral angle is determined by leaning the body of the screw driver on the ipsilateral surface of the spinous process5). Using this method, we expect to reduce the operation time, as well as the time of exposure to radiation.
In our study, we quantitatively compared the incidences of nerve root or vertebral artery injury and facet joint violation, as well as achievement of bicortical screw fixation, among the Roy-Camille technique, the Magerl technique and the Kim's technique. There were no significant differences in the incidences of complications among these three methods. Therefore, we expect that the Kim's method can be applied safely and easily even by less experienced spinal surgeons.
Berry et al.4) compared the pull-out strengths of Roy-Camille and Magerl methods which is debatable. Therefore, future study should be focused on the biomechanical evaluations of these methods. Moreover, clinical study to support this cadaveric study will be necessary.
CONCLUSION
Posterior cervical lateral screw fixation has been developed and modified by many surgeons. In this study, we conclude that the complication rate of the Kim's method is as low as those of other methods. In addition, the rate of bicortical purchase is also as high as that with previous methods. Because of the advantages of this method performed using the given anatomical structure without fluoroscopic assistance, the Kim's method will be an alternative choice that can be performed easily and safely for the treatment of many cervical diseases.
References
- 1.An HS, Gordin R, Renner K. Anatomic considerations for plate-screw fixation of the cervical spine. Spine (Phila Pa 1976) 1991;16:S548–S551. doi: 10.1097/00007632-199110001-00019. [DOI] [PubMed] [Google Scholar]
- 2.Anderson PA, Henley MB, Grady MS, Montesano PX, Winn HR. Posterior cervical arthrodesis with AO reconstruction plates and bone graft. Spine (Phila Pa 1976) 1991;16:S72–S79. doi: 10.1097/00007632-199103001-00012. [DOI] [PubMed] [Google Scholar]
- 3.Barrey C, Mettens P, Jund J, Cotton F, Perrin G. Quantitative anatomic evaluation of cervical lateral mass fixation with a comparison of the Roy-Camille and the Magerl screw techniques. Spine (Phila Pa 1976) 2005;30:E140–E147. doi: 10.1097/01.brs.0000155416.35234.a3. [DOI] [PubMed] [Google Scholar]
- 4.Barrey C, Mettens P, Rumelhart C, Cotton F, Jund J, Perrin G. Biomechanical evaluation of cervical lateral mass fixation : a comparison of the Roy-Camille and Magerl screw techniques. J Neurosurg. 2004;100:268–276. doi: 10.3171/spi.2004.100.3.0268. [DOI] [PubMed] [Google Scholar]
- 5.Cho JI, Kim DH. Comparative analysis of cervical lateral mass screw insertion among three techniques in the Korean population by quantitative measurements with reformatted 2D CT scan images : clinical research. J Korean Neurosurg Soc. 2008;44:124–130. doi: 10.3340/jkns.2008.44.3.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coe JD, Warden KE, Sutterlin CE, 3rd, McAfee PC. Biomechanical evaluation of cervical spinal stabilization methods in a human cadaveric model. Spine (Phila Pa 1976) 1989;14:1122–1131. doi: 10.1097/00007632-198910000-00016. [DOI] [PubMed] [Google Scholar]
- 7.Deen HG, Birch BD, Wharen RE, Reimer R. Lateral mass screw-rod fixation of the cervical spine : a prospective clinical series with 1-year follow-up. Spine J. 2003;3:489–495. [PubMed] [Google Scholar]
- 8.Ebraheim NA, An HS, Jackson WT, Brown JA. Internal fixation of the unstable cervical spine using posterior Roy-Camille plates : preliminary report. J Orthop Trauma. 1989;3:23–28. doi: 10.1097/00005131-198903010-00005. [DOI] [PubMed] [Google Scholar]
- 9.Ebraheim NA, Hoeflinger MJ, Salpietto B, Chung SY, Jackson WT. Anatomic considerations in posterior plating of the cervical spine. J Orthop Trauma. 1991;5:196–199. doi: 10.1097/00005131-199105020-00013. [DOI] [PubMed] [Google Scholar]
- 10.Ebraheim NA, Klausner T, Xu R, Yeasting RA. Safe lateral-mass screw lengths in the Roy-Camille and Magerl techniques. An anatomic study. Spine (Phila Pa 1976) 1998;23:1739–1742. doi: 10.1097/00007632-199808150-00006. [DOI] [PubMed] [Google Scholar]
- 11.Ebraheim NA, Xu R, Yeasting RA. The location of the vertebral artery foramen and its relation to posterior lateral mass screw fixation. Spine (Phila Pa 1976) 1996;21:1291–1295. doi: 10.1097/00007632-199606010-00002. [DOI] [PubMed] [Google Scholar]
- 12.Gill K, Paschal S, Corin J, Ashman R, Bucholz RW. Posterior plating of the cervical spine. A biomechanical comparison of different posterior fusion techniques. Spine (Phila Pa 1976) 1988;13:813–816. doi: 10.1097/00007632-198807000-00018. [DOI] [PubMed] [Google Scholar]
- 13.Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine (Phila Pa 1976) 2001;26:2467–2471. doi: 10.1097/00007632-200111150-00014. [DOI] [PubMed] [Google Scholar]
- 14.Harstall R, Heini PF, Mini RL, Orler R. Radiation exposure to the surgeon during fluoroscopically assisted percutaneous vertebroplasty : a prospective study. Spine (Phila Pa 1976) 2005;30:1893–1898. doi: 10.1097/01.brs.0000174121.48306.16. [DOI] [PubMed] [Google Scholar]
- 15.Heller JG, Carlson GD, Abitbol JJ, Garfin SR. Anatomic comparison of the Roy-Camille and Magerl techniques for screw placement in the lower cervical spine. Spine (Phila Pa 1976) 1991;16:S552–S557. doi: 10.1097/00007632-199110001-00020. [DOI] [PubMed] [Google Scholar]
- 16.Heller JG, Estes BT, Zaouali M, Diop A. Biomechanical study of screws in the lateral masses : variables affecting pull-out resistance. J Bone Joint Surg Am. 1996;78:1315–1321. doi: 10.2106/00004623-199609000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Jeanneret B, Magerl F, Ward EH, Ward JC. Posterior stabilization of the cervical spine with hook plates. Spine (Phila Pa 1976) 1991;16:S56–S63. doi: 10.1097/00007632-199103001-00010. [DOI] [PubMed] [Google Scholar]
- 18.Jones DP, Robertson PA, Lunt B, Jackson SA. Radiation exposure during fluoroscopically assisted pedicle screw insertion in the lumbar spine. Spine (Phila Pa 1976) 2000;25:1538–1541. doi: 10.1097/00007632-200006150-00013. [DOI] [PubMed] [Google Scholar]
- 19.Joseffer SS, Post N, Cooper PR, Frempong-Boadu AK. Minimally invasive atlantoaxial fixation with a polyaxial screw-rod construct : technical case report. Neurosurgery. 2006;58:ONS-E375. doi: 10.1227/01.NEU.0000208955.12461.C7. discussion ONS-E375. [DOI] [PubMed] [Google Scholar]
- 20.Katonis P, Papadopoulos CA, Muffoletto A, Papagelopoulos PJ, Hadjipavlou AG. Factors associated with good outcome using lateral mass plate fixation. Orthopedics. 2004;27:1080–1086. doi: 10.3928/0147-7447-20041001-18. [DOI] [PubMed] [Google Scholar]
- 21.Kim SH, Shin DA, Yi S, Yoon do H, Kim KN, Shin HC. Early results from posterior cervical fusion with a screw-rod system. Yonsei Med J. 2007;48:440–448. doi: 10.3349/ymj.2007.48.3.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kotani Y, Cunningham BW, Abumi K, McAfee PC. Biomechanical analysis of cervical stabilization systems. An assessment of transpedicular screw fixation in the cervical spine. Spine (Phila Pa 1976) 1994;19:2529–2539. doi: 10.1097/00007632-199411001-00007. [DOI] [PubMed] [Google Scholar]
- 23.Nazarian SM, Louis RP. Posterior internal fixation with screw plates in traumatic lesions of the cervical spine. Spine (Phila Pa 1976) 1991;16:S64–S71. doi: 10.1097/00007632-199103001-00011. [DOI] [PubMed] [Google Scholar]
- 24.Pait TG, McAllister PV, Kaufman HH. Quadrant anatomy of the articular pillars (lateral cervical mass) of the cervical spine. J Neurosurg. 1995;82:1011–1014. doi: 10.3171/jns.1995.82.6.1011. [DOI] [PubMed] [Google Scholar]
- 25.Richter M, Amiot LP, Puhl W. [Computer navigation in dorsal instrumentation of the cervical spine--an in vitro study] Orthopade. 2002;31:372–377. doi: 10.1007/s00132-001-0278-5. [DOI] [PubMed] [Google Scholar]
- 26.Roche S, de Freitas DJ, Lenehan B, Street JT, McCabe JP. Posterior cervical screw placement without image guidance : a safe and reliable practice. J Spinal Disord Tech. 2006;19:383–388. doi: 10.1097/00024720-200608000-00001. [DOI] [PubMed] [Google Scholar]
- 27.Stulik J, Vyskocil T, Sebesta P, Kryl J. Atlantoaxial fixation using the polyaxial screw-rod system. Eur Spine J. 2007;16:479–484. doi: 10.1007/s00586-006-0241-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sutterlin CE, 3rd, McAfee PC, Warden KE, Rey RM, Jr, Farey ID. A biomechanical evaluation of cervical spinal stabilization methods in a bovine model. Static and cyclical loading. Spine (Phila Pa 1976) 1988;13:795–802. doi: 10.1097/00007632-198807000-00015. [DOI] [PubMed] [Google Scholar]
- 29.Xu R, Ebraheim NA, Klausner T, Yeasting RA. Modified Magerl technique of lateral mass screw placement in the lower cervical spine : an anatomic study. J Spinal Disord. 1998;11:237–240. [PubMed] [Google Scholar]
- 30.Xu R, Haman SP, Ebraheim NA, Yeasting RA. The anatomic relation of lateral mass screws to the spinal nerves. A comparison of the Magerl, Anderson, and An techniques. Spine (Phila Pa 1976) 1999;24:2057–2061. doi: 10.1097/00007632-199910010-00016. [DOI] [PubMed] [Google Scholar]
- 31.Yoon SH, Park HC, Park HS, Kim EY, Ha Y, Chong CK, et al. Radiological considerations of posterior cervical lateral mass fixation using plate and screw. Yonsei Med J. 2004;45:406–412. doi: 10.3349/ymj.2004.45.3.406. [DOI] [PubMed] [Google Scholar]