Abstract
Objective
A minimally invasive transforaminal lumbar interbody fusion (MIS TLIF) has recently been introduced. However, MIS TLIF is a technically challenging procedure. The authors performed retrospective analysis about MIS TLIF using a single interbody cage.
Methods
Twenty-eight consecutive patients were treated by MIS TLIF. Of these 28 patients, 20 patients were included in this retrospective study. Perioperative, clinical, and radiologic outcomes were assessed. Clinical outcomes were assessed using Oswestry Disability Index (ODI) and Visual Analogue Scores (VAS). Fusion rates and cross-sections of operated spinal canals were assessed by CT.
Results
Twelve patients underwent MIS TLIF at one segment and 8 patients at two segments (L3/4: 4, L4/5: 17, L5/S1: 7). Operation time for a single segment was 131.7 min and for two segment was 201.4 min, and corresponding blood losses were 208.3 mL and 481.2 mL, respectively. ODI and VAS scores were significantly improved at 6 months postop (ODI from 30.32 to 15. 54, VAS from 7.80 to 2.20, p = 0.001). Twenty-two segments (78.6%) achieved grade I fusion, 4 segments (14.3%) achieved grade II, 2 segments (7.1%) achieved grade III and 0 segments achieved grade IV at 12 months. Postoperatively at 12 months, spinal canal cross sectional areas at disc spaces significantly increased from 157.5 to 294.3 mm2 (p = 0.012).
Conclusion
MIS TLIF achieved good clinical outcomes and high fusion rates. Our findings show that MIS TLIF performed with a single interbody cage and a tubular retractor system can be used as a standard MIS TLIF technique.
Keywords: Minimally invasive, Spinal fusion, Lumbar vertebrae
INTRODUCTION
Open transforaminal lumbar interbody fusion (TLIF) has been performed for many years with the aim of improving fusion rates and disc height restoration as compared with the traditional interbody fusion technique1,7,8,15). TLIF procedures can avoid the risks of the anterior lumbar interbody fusion technique (ALIF), such as, vessel injury, sympathetic nerve injury and injury to retroperitoneal and peritoneal structures11,12,15). In addition, TLIF reduces the complications associated with posterior lumbar interbody fusion (PLIF), because it does not require retraction of the dura or nerve roots, eliminates epidural scarring, and reduces intraoperative bleeding5,16,18).
Recently, advances in minimally invasive techniques (MIS) have allowed TLIF to reduce the complications associated with the open technique14,15). Minimally invasive techniques for transforaminal lumbar interbody fusion (MIS TLIF) using the tubular retractor system have been introduced with the aim of reducing blood loss and soft tissue trauma, causing smaller wounds, increasing the speed of recovery, and reducing postoperative pain as compared with the traditional open technique14,15). However, MIS TLIF is challenging technique and requires a learning curve, and furthermore, surgical techniques are different in surgeons14,15,18).
The purposes of this study were to explain technical tips and operative steps, to evaluate the perioperative, radiologic, and clinical outcomes of MIS TLIF using a single interbody cage and a tubular retraction system, and to standardize the MIS TLIF technique.
MATERIALS AND METHODS
Patient populations
Between Jan 2008 and Dec 2008, a total of 28 consecutive patients underwent MIS TLIF using single interbody cage and a tubular retractor system at our hospital. The indications for surgery were grade I spondylolisthesis, a degenerative disc with mechanical low back pain and radicular symptoms, and only one or two involved segments. All patients underwent a retrospective evaluation, involving; static and dynamic plain lumbar spine radiography, magnetic resonance imaging (MRI), and Computed tomography (CT). Conservative management had failed in all before surgery. Of the 28 patients initially enrolled, 20 patients were included this study because of a short follow-up period (less than 12 months). Patient's demographic and operative data were collected.
Perioperative, clinical, and radiologic outcomes
The perioperative outcomes were operation time and blood loss by number of segments treated. Clinical assessments were performed using the Oswestry Disability Index (ODI) and Visual Analogue scores (VAS) for leg and back, before surgery and at 7 days, and 1, 4, 6, and 12 months postop. Radiologic outcomes were reviewed by an independent neurosurgeon and a neuroradiologist, who unaware of treatment details. The radiologic outcomes used were fusion rates and decompression degrees. Fusion rates were assessed using the Bridwell grading system and CT and radiographic findings at 12 months postop (Table 1)2). Fusion site disc height was assessed using CT at 12 months postop. In addition, cross sections at operated spinal canals were determined by CT pre- and postop to evaluate the decompression using the PACS software and a PACS workstation (Centricity 2.0, General Electrics Medical Systems, Milwaukee, WI, USA).
Table 1.
Bridwell interbody fusion grading system
Operative technique
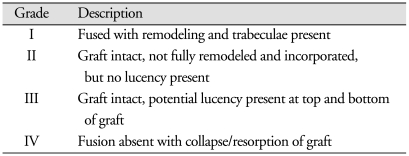
TLIF was performed on more symptomatic sides. Fluoroscopy was used to determine the operative level in all cases. In each case, we checked the disc space and the pedicle and skin marks at the disc space and lateral pedicle line in fluoroscopic AP view (Fig. 1A), and the lateral disc space in lateral view (Fig. 1B). A vertical skin incision (length : 25 mm) is placed at the disc space level cranially 15 mm and caudally 10 mm (Fig. 1). A tubular retractor system (MetRx; Medtronic Sofamor Danek, Memphis, TN, USA) is then introduced under fluoroscopic guidance to the facet joint. The first (smallest) tubular dilator is inserted instead of a K-wire and docked to the facet complex. Dilators of increasing diameter are then sequentially inserted between the paraspinal muscles and used to dissect muscles off the underlying facet complex. A 22 mm diameter working port is then introduced and secured to the operative table with a special arm. The following steps are then performed under a surgical microscope. Monopolar cautery and a pituitary forceps are used to remove remaining soft tissue overlying the facet complex.
Fig. 1.
Using fluoroscopy in AP view (A), the locations of the disc space and pedicle are checked, and a skin mark is made at the disc space and a lateral pedicle line. A vertical skin incision is made at the disc space level 15 mm cranially (black arrow) and 10 mm caudally (white arrow) (A). Fluoroscopy in lateral view is used to confirm the lateral disc space (B).
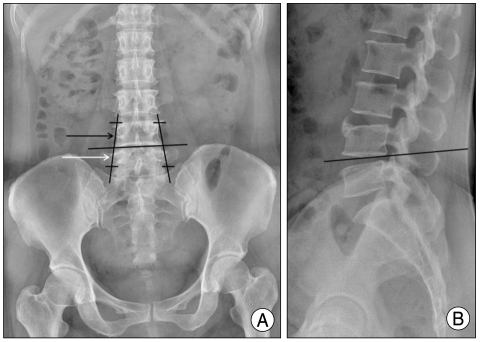
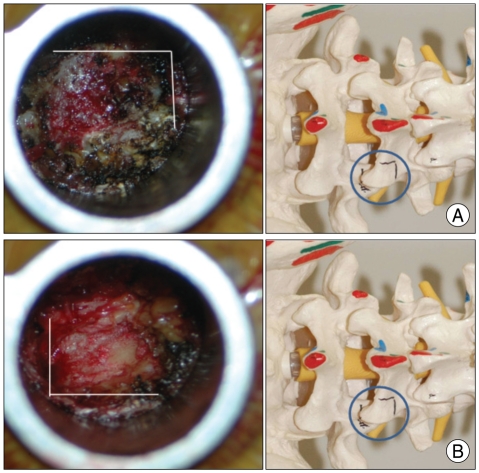
For total facetectomy, a narrow groove is made for an osteotome at the inferior articular process (Fig. 2A), and an osteotome is then used to remove the inferior articular process. The same procedure is used to remove the superior articular process (Fig. 2B). After complete facetectomy, the ligamentum flavum is removed to expose the lateral border of ipilateral nerve root (Fig. 3A). For decompression of contralateral side, the tubular retractor should be angled medially and the patient tilted laterally. Extensive decompression is then carried out, including that of central stenosis and the contralateral side (Fig. 3B).
Fig. 2.
A narrow groove is made using a high speed drill for osteotome at the inferior articular process (A), and at the superior articular process (B).
Fig. 3.
A : After complete facetectomy and ligamentum flavum removal, the lateral border of the nerve root is exposed. B : After tubular retractor angled medially and the patient tilted laterally, extensive decompression is conducted including decompression of the central stenosis and the contralateral side.
Standard discectomy is performed for graft insertion. Before interbody fusion instrument insertion, autologous excised bone, hydroxyapatite, or allobone is inserted at the disc space and then the interbody single long cage (Capstone; Medtronic Sofamor Danek, Memphis, TN, USA, 32 mm length) filled with only autologous bone is introduced.
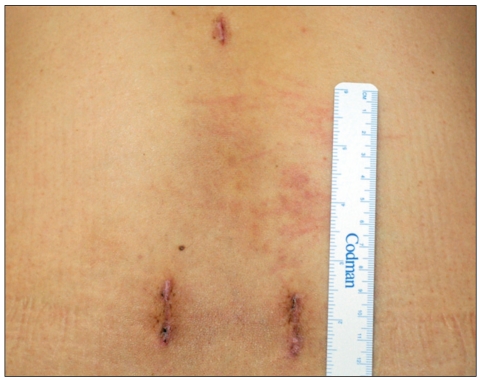
After interbody fusion and adequate decompression are carried out, the tubular retractor system is removed and an ipsilateral percutaneous pedicle screw system (Sextant; Medtronic Sofamor Danek, Memphis, TN) is placed through the same incision. A contralateral percutaneous pedicle screw system is also placed through the mirror incision (Fig. 4) under fluoroscopic guidance.
Fig. 4.
Final skin wound after MIS TLIF using a bilateral percutaneous pedicle screw system. Two wounds were made. Ipsilateral wound for the tubular retractor and ipsilateral percutaneous pedicle screw system and a mirror wound for the contralateral percutaneous pedicle screw system. A single 10 mm wound was needed in the cranial area for rod insertion. MIS TLIF : minimally invasive techniques for transforaminal lumbar interbody fusion.
Statistical analysis
All analyses were carried out using SPSS Ver. 12.00K (SPSS, Inc., Chicago, IL, USA). Clinical and radiological results were analyzed using Wilcoxon's Signed Rank test. p values of less than 0.05 were considered statistically significant.
RESULTS
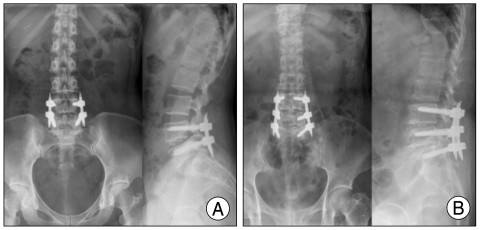
Mean patient age was 53.85 years. There were 14 females and 6 males, and in total 28 segments were included (L3/4 : 4, L4/5 : 17, L5/S1 : 7). The mean follow-up period was 18.08 months (range 14 - 23 months). Twelve patients were treated at one segment (Fig. 5A) and 8 patients at two segments (Fig. 5B). Disease entities were as follows; herniated lumbar discs 12, degenerative spondylolisthesis 4, spondylolytic spondylolisthesis one, and spinal stenosis 11.
Fig. 5.
One segment MIS TLIF using a single interbody cage and a bilateral percutaneous screw system (A) and two segment MIS TLIF using a single interbody cage and a bilateral percutaneous screw system (B). MIS TLIF : Minimally invasive techniques for transforaminal lumbar interbody fusion.
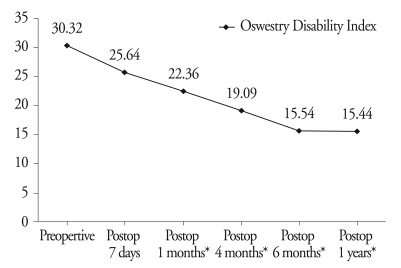
Operation time at one and two segments were 131.7 and 201.4 min, respectively, and mean blood losses were 208.3 mL and 481.2 mL, respectively. Mean ODI scores were significantly improved from 6 months after operation (from 30.32 to 15.54, p = 0.001) (Fig. 6). Mean ODI scores at 12 months were 15.44 and it had no significance with 6 months after operation. VAS scores for leg pain and back pain at 12 months both showed significant improved (leg pain 7.80 to 2.20, p = 0.001, back pain 7.90 to 2.70, p = 0.001).
Fig. 6.
Oswestry Disability Index. *p < 0.05.
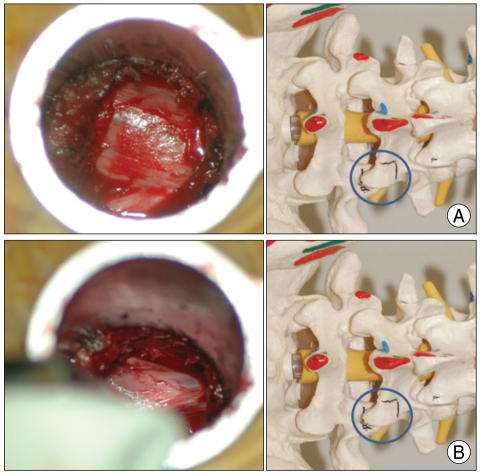
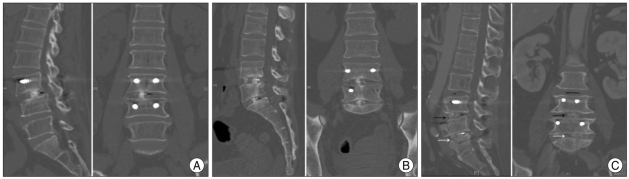
Before interbody fusion instrument insertion, we inserted autologous excised bone, hydroxyapatite, or allobone each disc space then inserted an interbody single long cage filled with only autologous excised bone. Before inserting the interbody cage, autologous bone was inserted into the disc space in 2 segments (7.1%), hydroxyapatite in 23 segments (82.1%) (Mastergraft; Medtronic Sofamor Danek, Memphis, TN, USA), and allograft bone in 3 segments (10.7%). Fusion grades based on the Bridwell grading system were; grade I in 22 segments (78.6%) (Fig. 7A), grade II in 4 segments (14.3%) (Fig. 7B), grade III in 2 segments (7.1%) (Fig. 7C) and grade IV in 0 segment. Fusion was defined as grade 1 or 2 giving a fusion rate of 92.8% (26 segments). Mean spinal canal cross section area at disc spaces was found to have increased significantly at 12 months postoperatively from 157.5 mm2 to 294.3 mm2, (p = 0.012) (Fig. 8). Fusion site disc height was mild increased (9.33 mm to 9.76 mm), but it had no statistical difference. (p = 0.06)
Fig. 7.
Fusion grade as determined using the Bridwell grading system. Grade I (A) represents fusion with remodeling and trabeculae; Grade II (B) graft intact with no lucency, but not fully remodeled and incorporated; Grade III (black arrow) (C) showing potential lucency at the top and bottom of the graft. The white arrow (C) shows Grade I fusion.
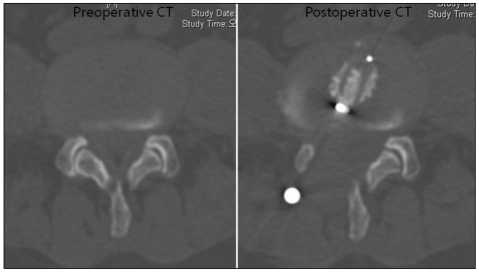
Fig. 8.
Spinal canal cross sectional area at the disc space was significantly increased at 12 months postoperatively. The central canal and contralateral side ligamentum flavum were removed.
Among the 20 patients, there was only one operation related complication. One case of dura tear was seen during operation and using vascular small clip, and it was repaired without CSF leakage. There were no other complications such as hematoma, infection and canal violation of screw.
DISCUSSION
It is well known that MIS TLIF has many advantages as compared with open TLIF in terms of reducing iatrogenic soft tissue and muscle injuries that occur during routine surgical exposure. Furthermore, previous authors have reported that MIS TLIF causes less morbidity than conventional TLIF13-15,17). MIS TLIF preserves the natural posterior tension band and the use of a muscle-splitting, tubular retraction system further limits the injury to the ipsilateral paraspinous musculature, which decreases postoperative pain and preserves healthy muscle tissue15).
However, it is difficult for spine surgeons to attempt MIS TLIF for the following reasons. The first concerns its learning curve, the second is that it take more operation time than conventional lumbar fusion, the third is that it is difficult to treat bilateral symptoms using an unilateral approach, and the forth is that it requires more radiation time than conventional lumbar fusion during the procedure6,9,13-15). Accordingly, the main purpose of this study was present technical tips that allow these difficulties to be overcome.
MIS TLIF is technically complicated, and various techniques have been described in the literature3,10,13-15,17). We have adopted different methods and used different operative steps based on previous reports. Currently, we do not use a K-wire before sequential dilation, because this introduces a risk of neural element damage. Moreover, if the first (smallest) tubular dilator is inserted first, the superficial surface of the facet complex easily felt, which means that fluoroscopy is not needed to check it location.
Furthermore, we did not need to insert a contralateral screw before inserting an interbody cage. Extensive decompression to the contralateral side allows enough space for an interbody distractor, and an interbody distractor can then be inserted into the disc space through an ipsilateral tubular retractor17). Regarding the interbody instrument, only one single long interbody (32 mm long) cage with autologous excised bone is sufficient for fusion, and as was reported by a previous study, a single interbody cage is safe and provides successful fusion4,18). To obtain enough bone for the cage or disc space, we recommend the use an osteotome13,17). In addition, making a narrow groove for the osteotome with a high speed drill is good method of preventing osteotome slippage. Because in many countries, including South Korea, surgeons cannot use BMP yet, it is important to harvest as much autologous bone as possible during the procedure. Based on the present study, a 92.8% fusion rate was achieved using a single long interbody cage, which concurs with previous reports14,15,18).
The problem posed by contralateral side decompression is a major disadvantage of MIS TLIF using an unilateral approach. Initially, we inserted two cages bilaterally for bilateral MIS TLIF. However, it took 4 to 5 hours to conduct the bilateral procedure, which was almost twice that required for conventional lumbar interbody fusion14,15). When a patient has bilateral symptoms or a bilateral radiologic pathology, it is possible to decompress bilaterally with the tubular retractor angled medially and the patient tilted laterally during the unilateral approach15). By using this wanding technique, contralateral side nerve root decompression, including decompression of central canal stenosis, can be confirmed (Fig. 3B). To perform contralateral side nerve root decompression easily, a more medial incision line is needed for the tubular retractor. As mentioned above, a lateral pedicle line was incised (Fig. 1A) 5 to 10 mm medially than previously reported13,15,17). During this process, enough autologous bone can be excised for the cage and disc interspace. Accordingly, bilateral MIS TLIF is not required to treat bilateral symptoms or a bilateral radiologic pathology. During the present study, we found that spinal canal cross section areas at disc levels significantly increased postoperatively. However, spondylolisthesis of more than grade II requires bilateral MIS TLIF and bilateral interbody cages, because decompressing the contralateral exiting root using the wanding technique is difficult. The contralateral traversing root can be decompressed easily using the wanding technique using the unilateral approach, but contralateral exiting root decompression using the unilateral MIS TLIF technique is almost impossible.
If the above technical tips are used, most surgeons can reduce average operative times. In the present study, the mean duration of surgery at one and two segments were 131.7 and 201.4 min, respectively. For one segment, the mean duration of MIS TLIF was 131.7 min, whereas previous studies have reported 216.4 and 191.7 min for MIS TLIF14,15). Park and Ha14) and Peng et al.15) reported open TLIF surgical times of 170.5 min and 148.8 min, respectively. Accordingly, our MIS TLIF operation times are shorter than open TLIF times. In addition, blood loss for one segment MIS TLIF was 208.3 mL, which is less than has been reported for open TLIF. Park and Ha14) and Peng et al.15) reported open TLIF blood losses of 681 and 737.9 mL, respectively14,15). Furthermore, in the present study, blood loss for two segment MIS TLIF was only 481.2 mL, which is less than has been reported for open one segment TLIF14,15). In addition, it should be borne in mind that radiation time increases with surgical duration. However, as with other surgical techniques, an understanding of the underlying three-dimensional anatomy, particularly the neural, bony, and joint anatomies, is critical for MIS TLIF using a single interbody cage and a tubular retractor system.
CONCLUSION
MIS TLIF using single interbody cage and a tubular retractor system with the contralateral decompression technique produces good clinical outcomes, high fusion rates and reduces operative morbidity. By using this wanding technique, contralateral side nerve root decompression, including decompression of central canal stenosis, is possible. Furthermore, our experiences demonstrate that MIS TLIF using a single interbody cage and a tubular retractor system can be used as a standard MIS TLIF technique.
References
- 1.Blume HG, Rojas CH. Unilateral lumbar interbody fusion (posterior approach) utilizing dowel graft. J Neurol Orthop Surg. 1981;2:171–175. [Google Scholar]
- 2.Bridwell KH, Lenke LG, McEnery KW, Baldus C, Blanke K. Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine (Phila Pa 1976) 1995;20:1410–1418. [PubMed] [Google Scholar]
- 3.Cole CD, McCall TD, Schmidt MH, Dailey AT. Comparison of low back fusion techniques transforaminal lumbar interbody fusion (TLIF) or posterior lumbar interbody fusion (PLIF) approaches. Curr Rev Musculoskelet Med. 2009;2:118–126. doi: 10.1007/s12178-009-9053-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cutler AR, Siddiqui S, Mohan AL, Hillard VH, Cerabona F, Das K. Comparison of polyetheretherketone cages with femoral cortical bone allograft as a single-piece interbody spacer in transforaminal lumbar interbody fusion. J Neurosurg Spine. 2006;5:534–539. doi: 10.3171/spi.2006.5.6.534. [DOI] [PubMed] [Google Scholar]
- 5.DiPaola CP, Molinari RW. Posterior lumbar interbody fusion. J Am Acad Orthop Surg. 2008;16:130–139. doi: 10.5435/00124635-200803000-00004. [DOI] [PubMed] [Google Scholar]
- 6.German JW, Foley KT. Minimal access surgical techniques in the management of the painful lumbar motion segment. Spine (Phila Pa 1976) 2005;30:S52–S59. doi: 10.1097/01.brs.0000174501.53285.9d. [DOI] [PubMed] [Google Scholar]
- 7.Harms JG, Jeszensky D. The unilateral transforaminal approach for posterior lumbar interbody fusion. Orthop Traumatol. 1998;6:88–99. [Google Scholar]
- 8.Harris BM, Hilibrand AS, Savas PE, Pellegrino A, Vaccaro AR, Siegler S, et al. Transforaminal lumbar interbody fusion : the effect of various instrumentation techniques on the flexibility of the lumbar spine. Spine (Phila Pa 1976) 2004;29:E65–E70. doi: 10.1097/01.brs.0000113034.74567.86. [DOI] [PubMed] [Google Scholar]
- 9.Khoo LT, Palmer S, Laich DT, Fessler RG. Minimally invasive percutaneous posterior lumbar interbody fusion. Neurosurgery. 2002;51:S166–S161. [PubMed] [Google Scholar]
- 10.Kim JS, Kim DH, Lee SH. Comparison between Instrumented Mini-TLIF and Instrumented Circumferential Fusion in Adult Low-Grade Lytic Spondylolisthesis : Can Mini-TLIF with PPF Replace Circumferential Fusion? J Korean Neurosurg Soc. 2009;45:74–80. doi: 10.3340/jkns.2009.45.2.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McAfee PC, Regan JR, Zdeblick T, Zuckerman J, Picetti GD, 3rd, Heim S, et al. The incidence of complications in endoscopic anterior thoracolumbar spinal reconstructive surgery. A prospective multicenter study comprising the first 100 consecutive cases. Spine (Phila Pa 1976) 1995;20:1624–1632. doi: 10.1097/00007632-199507150-00012. [DOI] [PubMed] [Google Scholar]
- 12.McDonnell MF, Glassman SD, Dimar JR, 2nd, Puno RM, Johnson JR. Perioperative complications of anterior procedures on the spine. J Bone Joint Surg Am. 1996;78:839–847. doi: 10.2106/00004623-199606000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Park P, Foley KT. Minimally invasive transforaminal lumbar interbody fusion with reduction of spondylolisthesis : technique and outcomes after a minimum of 2 years' follow-up. Neurosurg Focus. 2008;25:E16. doi: 10.3171/FOC/2008/25/8/E16. [DOI] [PubMed] [Google Scholar]
- 14.Park Y, Ha JW. Comparison of one-level posterior lumbar interbody fusion performed with a minimally invasive approach or a traditional open approach. Spine (Phila Pa 1976) 2007;32:537–543. doi: 10.1097/01.brs.0000256473.49791.f4. [DOI] [PubMed] [Google Scholar]
- 15.Peng CW, Yue WM, Poh SY, Yeo W, Tan SB. Clinical and radiological outcomes of minimally invasive versus open transforaminal lumbar interbody fusion. Spine (Phila Pa 1976) 2009;34:1385–1389. doi: 10.1097/BRS.0b013e3181a4e3be. [DOI] [PubMed] [Google Scholar]
- 16.Ray CD. Threaded titanium cages for lumbar interbody fusions. Spine (Phila Pa 1976) 1997;22:667–679. doi: 10.1097/00007632-199703150-00019. discussion 679-680. [DOI] [PubMed] [Google Scholar]
- 17.Schwender JD, Holly LT, Rouben DP, Foley KT. Minimally invasive transforaminal lumbar interbody fusion TLIF : technical feasibility and initial results. J Spinal Disord Tech. 2005;18(Suppl):S1–S6. doi: 10.1097/01.bsd.0000132291.50455.d0. [DOI] [PubMed] [Google Scholar]
- 18.Xiao Y, Li F, Chen Q. Transforaminal lumbar interbody fusion with one cage and excised local bone. Arch Orthop Trauma Surg. 2010;130:591–597. doi: 10.1007/s00402-009-0917-6. [DOI] [PubMed] [Google Scholar]